Medicine:Polycythemia vera
| Polycythemia vera | |
|---|---|
| Other names | Polycythaemia vera (PV, PCV), erythremia, primary polycythemia, Vaquez disease, Osler-Vaquez disease, polycythemia rubra vera[1] |
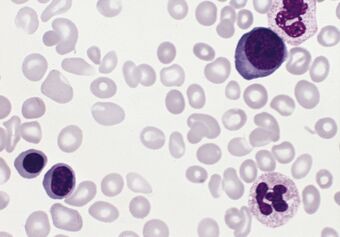 | |
| Blood smear from a patient with polycythemia vera | |
| Specialty | Oncology, hematology |
In oncology, polycythemia vera (PV) is an uncommon myeloproliferative neoplasm (chronic leukemia) in which the bone marrow makes too many red blood cells[1] as well as white blood cells and platelets. The majority of cases[2] are caused by mutations in the JAK2 gene, most commonly resulting in a single amino acid change in its protein product from valine to phenylalanine at position 617.[3]
Most of the health concerns associated with polycythemia vera are caused by the blood being thicker as a result of the increased red blood cells. It is more common in the elderly and may be symptomatic or asymptomatic. Common signs and symptoms include itching (pruritus), and severe burning pain in the hands or feet that is usually accompanied by a reddish or bluish coloration of the skin. Patients with polycythemia vera are more likely to have gouty arthritis. Treatment consists primarily of phlebotomy as well as oral chemotherapy and emerging treatments like long-acting interferon formulations.
Signs and symptoms

People with polycythemia vera can be asymptomatic.[4] Clinical symptoms of polycythemia vera are mostly due to hyperviscosity of blood. A classic symptom of polycythemia vera is pruritus or itching, particularly after exposure to warm water (such as when taking a bath),[5] which may be due to abnormal histamine release[6][7] or prostaglandin production.[8] Such itching is present in approximately 40% of patients with polycythemia vera.[9] Gouty arthritis may be present in up to 20% of patients.[9] Peptic ulcer disease is also common in patients with polycythemia vera; most likely due to increased histamine from mast cells, but may be related to an increased susceptibility to infection with the ulcer-causing bacterium H. pylori.[10]
A classic symptom of polycythemia vera (and the related myeloproliferative disease essential thrombocythemia) is erythromelalgia.[11] This is a burning pain in the hands or feet, usually accompanied by a reddish or bluish coloration of the skin. Erythromelalgia is caused by an increased platelet count or increased platelet "stickiness" (aggregation), resulting in the formation of tiny blood clots in the vessels of the extremity; it responds rapidly to treatment with aspirin.[12][13] Splenomegaly may cause the spleen to be palpable in some patients, which has been reported by Lee et al. (2022) to be associated with both the V617F mutation and the development of myelofibrosis.[14]
Pathophysiology
Polycythemia vera (PV), being a primary polycythemia (increase in the fraction of volume occupied by red cells in the blood), is caused by neoplastic proliferation and maturation of erythroid, megakaryocytic and granulocytic elements to produce what is referred to as panmyelosis. In contrast to secondary polycythemias, PV is associated with a low serum level of the hormone erythropoietin (EPO). Instead, PV cells often carry activating mutation in a tyrosine kinase–encoding gene, JAK2, which acts in signaling pathways of the EPO receptor, making those cells proliferate independently from EPO.[15][page needed]
Diagnosis
Diagnostic criteria for polycythemia vera were modified by the World Health Organisation in 2016.[16] The WHO criteria for polycythemia vera are specifically outlined in Table 4, and emphasis is given to accurate histological observations as proven predictors in the prognosis of the disease.
As summarized by Verstovek following the 2016 European Hematology Association Congress,[17] there are 3 major criteria for PV diagnosis:
- The first is a very high red blood cell count, which is usually identified by elevated levels of hemoglobin or hematocrit;
- A bone marrow biopsy that shows hypercellularity and abnormalities in megakaryocytes; and
- The presence of a mutation in the Janus kinase 2 (JAK2) gene.
Patients usually have a very low level of erythropoietin, a growth factor that increases the production of red blood cells, which may be considered a minor diagnostic feature.
A mutation in the JAK2 kinase (V617F) is strongly associated with polycythemia vera.[18][19] While it is a JAK2 V617F mutation in 95% of patients, JAK2 exon 12 mutations have also been observed.[20] The V617F mutation is not inherited, but develops as a somatic mutation in the erythroid progenitor cells.[21] Some patients may lose the normal allele in the diseased cells entirely together with the short arm of chromosome 9 (9p), likely due to mitotic recombination causing copy-neutral loss of heterozygosity.[22] While the JAK2 V617F mutation is generally sporadic (random), a certain inherited haplotype of JAK2 has been associated with its development.[23][24]
People with untreated polycythemia vera have a substantial risk of Budd-Chiari syndrome (hepatic vein thrombosis).[25]
Treatment
Untreated, polycythemia vera can be fatal, with the median survival in patients being 1.5-3 years.[26][27][28] Data on the effect of life-span of an individual with treated polycythemia vera is inconclusive due to the rarity of the disease. Studies show the median survival rate of controlled Polycythemia Vera ranges from 10 to 20 years; however, most observations are of people diagnosed in their 60s. Patients live close to a normal life expectancy.[29]
Frequent blood withdrawals (phlebotomy) are one form of treatment, which often may be combined with other therapies. The removal of blood from the body induces iron deficiency, thereby decreasing the hemoglobin / hematocrit level, and reducing the risk of blood clots. Phlebotomy is typically performed to bring their hematocrit (red blood cell percentage) down below 45 for men or 42 for women.[30] It has been observed that phlebotomy also reduces cognitive impairment.[31]
Medications are also used which reduce the number of red blood cells. These include hydroxyurea and interferon therapy, among others.[32] The tendency of some practitioners to avoid chemotherapy if possible, especially in young patients, is a result of research indicating possible increased risk of transformation to acute myelogenous leukemia (AML). While hydroxyurea is considered a safer chemotherapy in this aspect, there is still some debate about its long-term safety.[33]
There are indications that the lung cancer drug erlotinib may be an additional treatment option for those with certain genetic markers.[34]
Ruxolitinib (brand name Jakafi), a Janus kinase 2 (JAK2) inhibitor, is also used to treat polycythemia.[35]
Ropeginterferon alfa-2b (Besremi) was approved for medical use in the European Union in February 2019,[36] and in the United States in November 2021.[37][38] Ropeginterferon alfa-2b is the first medication approved by the U.S. Food and Drug Administration (FDA) to treat polycythemia vera that people can take regardless of their treatment history, and the first interferon therapy specifically approved for polycythemia vera.[37] Interferon alfa-2b is also used.[32]
Epidemiology
Polycythemia vera occurs in all age groups,[39] although the incidence increases with age. One study found the median age at diagnosis to be 60 years,[9] while a Mayo Clinic study in Olmsted County, Minnesota found that the highest incidence was in people aged 70–79 years.[40] The overall incidence in the Minnesota population was 1.9 per 100,000 person-years, and the disease was more common in men than women.[40] A cluster around a toxic site was confirmed in northeast Pennsylvania in 2008.[41]
Notable deaths
- Phyllis George (1949–2020), American sportscaster and former First Lady of Kentucky[42]
- Ron Miles (1963–2022), American jazz trumpeter[43]
- Nell Rankin (1924–2005), American mezzo-soprano[44]
References
- ↑ 1.0 1.1 "polycythemia vera." at Encyclopædia Britannica. 2010. Encyclopædia Britannica Online. 21 Sep. 2010
- ↑ "Targeted deep sequencing in polycythemia vera and essential thrombocytopenia". Blood Advances 1 (1): 21-30. 2016. doi:10.1182/bloodadvances.2016000216. PMID 29296692.
- ↑ "Genetic Background of Polycythemia Vera". Genes 13 (4). 2022. doi:10.3390/genes13040637. Art. No. 637. PMID 35456443.
- ↑ [Polycythemia vera EBSCO database] verified by URAC; accessed from Mount Sinai Hospital, New York
- ↑ "Polycythemia vera-associated pruritus and its management". Eur J Clin Invest 40 (9): 828–34. 2010. doi:10.1111/j.1365-2362.2010.02334.x. PMID 20597963.
- ↑ "Polycythaemia rubra vera and water-induced pruritus: blood histamine levels and cutaneous fibrinolytic activity before and after water challenge". Br J Dermatol 116 (3): 329–33. 1987. doi:10.1111/j.1365-2133.1987.tb05846.x. PMID 3567071.
- ↑ "Skin mast cells in polycythaemia vera: relationship to the pathogenesis and treatment of pruritus". Br J Dermatol 116 (1): 21–9. 1987. doi:10.1111/j.1365-2133.1987.tb05787.x. PMID 3814512.
- ↑ "Pruritus in polycythemia vera: treatment with aspirin and possibility of platelet involvement". Acta Derm Venereol 59 (6): 505–12. 1979. doi:10.2340/0001555559505512. PMID 94209.
- ↑ 9.0 9.1 9.2 Berlin NI (1975). "Diagnosis and classification of polycythemias". Semin Hematol 12 (4): 339–51. PMID 1198126.
- ↑ "Gastroduodenal lesions in polycythaemia vera: frequency and role of Helicobacter pylori". Br J Haematol 117 (1): 198–202. 2002. doi:10.1046/j.1365-2141.2002.03380.x. PMID 11918555.
- ↑ "Erythromelalgia: a pathognomonic microvascular thrombotic complication in essential thrombocythemia and polycythemia vera". Semin Thromb Hemost 23 (4): 357–63. 1997. doi:10.1055/s-2007-996109. PMID 9263352.
- ↑ Michiels J (1997). "Erythromelalgia and vascular complications in polycythemia vera". Semin Thromb Hemost 23 (5): 441–54. doi:10.1055/s-2007-996121. PMID 9387203.
- ↑ "Increased thromboxane biosynthesis in patients with polycythemia vera: evidence for aspirin-suppressible platelet activation in vivo". Blood 80 (8): 1965–71. 1992. doi:10.1182/blood.V80.8.1965.1965. PMID 1327286.
- ↑ "Volumetric Splenomegaly in Patients With Polycythemia Vera". Journal of Korean Medical Science 37 (11). 2022. doi:10.3346/jkms.2022.37.e87. Art. No. e87. PMID 35315598.
- ↑ Robbins Basic Pathology (8th ed.). Saunders Elsevier. 2007. ISBN 978-1-4160-2973-1.
- ↑ Daniel A. Arber; Attilio Orazi; Robert Hasserjian; Jürgen Thiele; Michael J. Borowitz; Michelle M. Le Beau; Clara D. Bloomfield; Mario Cazzola et al. (2016). "The 2016 revision to the World Health Organization classification of myeloid neoplasms and acute leukemia". Blood 127 (20): 2391–2405. doi:10.1182/blood-2016-03-643544. PMID 27069254.
- ↑ Verstovsek, S. (2016). "Highlights in polycythemia vera from the 2016 EHA congress". Clin Adv Hematol Oncol 14 (10): 810–813. PMID 27930632. https://www.hematologyandoncology.net/archives/october-2016/highlights-in-polycythemia-vera-from-the-2016-eha-congres/.
- ↑ "Acquired mutation of the tyrosine kinase JAK2 in human myeloproliferative disorders". Lancet 365 (9464): 1054–61. 2005. doi:10.1016/S0140-6736(05)71142-9. PMID 15781101.
- ↑ "Activating mutation in the tyrosine kinase JAK2 in polycythemia vera, essential thrombocythemia, and myeloid metaplasia with myelofibrosis". Cancer Cell 7 (4): 387–97. 2005. doi:10.1016/j.ccr.2005.03.023. PMID 15837627.
- ↑ Verstovsek, S. (2016). "Highlights in polycythemia vera from the 2016 EHA congress". Clin Adv Hematol Oncol 14 (10): 810–813. PMID 27930632. https://www.hematologyandoncology.net/archives/october-2016/highlights-in-polycythemia-vera-from-the-2016-eha-congres/.
- ↑ "Identification of an Acquired JAK2 Mutation in Polycythemia Vera". Journal of Biological Chemistry 280 (24): 22788-22792. 2005. doi:10.1074/jbc.C500138200. PMID 15863514.
- ↑ "A Gain-of-Function Mutation of JAK2 in Myeloproliferative Disorders". The New England Journal of Medicine 352 (17): 1779-1790. 2005. doi:10.1056/NEJMoa051113. PMID 15858187.
- ↑ "JAK2 haplotype is a major risk factor for the development of myeloproliferative neoplasms". Nature Genetics 41 (4): 446-449. 2009. doi:10.1038/ng.334. PMID 19287382.
- ↑ "Whole-exome sequencing identifies novel candidate predisposition genes for familial polycythemia vera". Human Genomics 11 (1). 2017. doi:10.1186/s40246-017-0102-x. Art. No. 6. PMID 28427458.
- ↑ "Elevated serum erythropoietin levels in patients with Budd-Chiari syndrome secondary to polycythemia vera: clinical implications for the role of JAK2 mutation analysis". Eur. J. Haematol. 77 (1): 57–60. July 2006. doi:10.1111/j.1600-0609.2006.00667.x. PMID 16827884.
- ↑ Mayo Clinic staff. "Polycythemia vera - MayoClinic.com". Polycythemia vera: Definition. Mayo Clinic. http://www.mayoclinic.com/health/polycythemia-vera/DS00919.
- ↑ "What Is Polycythemia Vera?". National Heart, Lung and Blood Institute. http://www.nhlbi.nih.gov/health/health-topics/topics/poly/.
- ↑ "Polycythemia Vera Follow-up". http://emedicine.medscape.com/article/205114-followup#showall.
- ↑ Verstovsek, S. (2016). "Highlights in polycythemia vera from the 2016 EHA congress". Clin Adv Hematol Oncol 14 (10): 810–813. PMID 27930632. https://www.hematologyandoncology.net/archives/october-2016/highlights-in-polycythemia-vera-from-the-2016-eha-congres/.
- ↑ "The diagnosis and management of polycythemia vera in the era since the Polycythemia Vera Study Group: a survey of American Society of Hematology members' practice patterns". Blood 99 (4): 1144–9. 2002. doi:10.1182/blood.V99.4.1144. PMID 11830459.
- ↑ "Cognitive impairment in polycythemia vera: partial reversibility upon lowering of the hematocrit". Eur. Neurol. 44 (1): 57–9. 2000. doi:10.1159/000008194. PMID 10894997.
- ↑ 32.0 32.1 "Polycythemia vera - Diagnosis and treatment - Mayo Clinic" (in en). https://www.mayoclinic.org/diseases-conditions/polycythemia-vera/diagnosis-treatment/drc-20355855.
- ↑ Björkholm, M et al. (10 June 2011). "Treatment-related risk factors for transformation to acute myeloid leukemia and myelodysplastic syndromes in myeloproliferative neoplasms.". Journal of Clinical Oncology 29 (17): 2410–5. doi:10.1200/JCO.2011.34.7542. PMID 21537037.
- ↑ "Erlotinib Effectively Inhibits JAK2V617F Activity and Polycythemia Vera Cell Growth". J Biol Chem 282 (6): 3428–32. 2007. doi:10.1074/jbc.C600277200. PMID 17178722.
- ↑ Tefferi, A; Vannucchi, AM; Barbui, T (10 January 2018). "Polycythemia vera treatment algorithm 2018.". Blood Cancer Journal 8 (1): 3. doi:10.1038/s41408-017-0042-7. PMID 29321547.
- ↑ "Besremi EPAR". 12 December 2018. https://www.ema.europa.eu/en/medicines/human/EPAR/besremi.
- ↑ 37.0 37.1 "FDA Approves Treatment for Rare Blood Disease". U.S. Food and Drug Administration (FDA) (Press release). 12 November 2021. Retrieved 12 November 2021.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ "U.S. FDA Approves Besremi (ropeginterferon alfa-2b-njft) as the Only Interferon for Adults With Polycythemia Vera" (Press release). PharmaEssentia. 12 November 2021. Retrieved 14 November 2021 – via Business Wire.
- ↑ "Polycythemia vera in young patients: a study on the long-term risk of thrombosis, myelofibrosis and leukemia". Haematologica 88 (1): 13–8. 2003. PMID 12551821.
- ↑ 40.0 40.1 "Trends in the incidence of polycythemia vera among Olmsted County, Minnesota residents, 1935-1989". Am J Hematol 47 (2): 89–93. 1994. doi:10.1002/ajh.2830470205. PMID 8092146.
- ↑ MICHAEL RUBINKAM (2008). "Cancer cluster confirmed in northeast Pennsylvania". Associated Press. https://news.yahoo.com/s/ap/20080826/ap_on_sc/toxic_dump_fears.
- ↑ Yetter, Deborah (May 16, 2020). "Phyllis George, former Kentucky first lady and Miss America, dies at 70". The Courier-Journal. https://www.courier-journal.com/story/news/local/2020/05/16/former-miss-america-kentucky-first-lady-phyllis-george-dies/3051644001/.
- ↑ Harrington, Jim (March 9, 2022). "'Gifted artist' Ron Miles dies of a rare blood disorder at 58". The Mercury News. https://www.mercurynews.com/2022/03/09/gifted-artist-ron-miles-dies-of-a-rare-blood-disorder-at-58/.
- ↑ Allan Kozinn (January 19, 2005). "Nell Rankin Is Dead at 81; Mezzo-Soprano With Met". The New York Times. https://www.nytimes.com/2005/01/19/arts/music/19rankin.html.
External links
- Polycythemia Vera National Heart, Lung, and Blood Institute
- 11-141d. at Merck Manual of Diagnosis and Therapy Professional Edition
| Classification | |
|---|---|
| External resources |
 |

