Medicine:Delta-beta thalassemia
| Delta-beta thalassemia | |
|---|---|
 | |
| Delta-beta thalassemia | |
| Causes | Produces only gamma-globin and forms HbF(deletes entire delta and beta gene sequence)[1] |
| Diagnostic method | High-performance liquid chromatography |
| Treatment | Blood transfusions[2] |
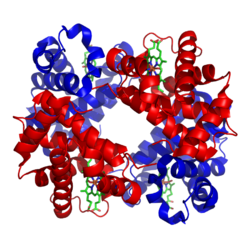
Delta-beta thalassemia is a rare form of thalassemia in which there is a reduced production of hemoglobin subunit delta and hemoglobin subunit beta and raised levels of hemoglobin subunit gamma. It is an autosomal recessive disorder.[1][3]
Signs and symptoms
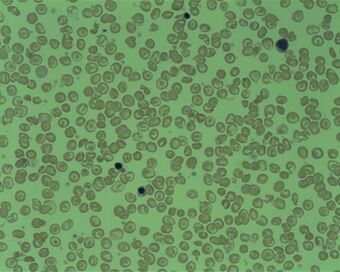
An individual with delta-beta thalassemia is usually asymptomatic, however microcytosis can occur where the red blood cells are abnormally small.[1][4]
Mechanism
Delta-beta thalassemia is autosomal recessive disorder,[1] which means both parents are affected and two copies of the gene must be present.[5] A carrier gets a normal gene to produce hemoglobin A, from one parent and the other parent supplies a gene which makes no hemoglobin A.[6] Delta-beta thalassemia is considered rare.[2]
Delta-beta-thalassemia is caused by deletions of the entire delta and beta genes sequences and only gamma-globin and HbF are formed. Rarely, non-deletional forms have been reported.[7][8]
When two delta0 mutations are inherited, no hemoglobin A2 (alpha2, delta2) are formed. This is innocuous because only 2-3% of normal adult hemoglobin is hemoglobin A2. The individual will have normal hematological parameters (erythrocyte count, total hemoglobin, mean corpuscular volume). The delta-beta thalassemia demonstrates one mutation is at the +69 position.[9]
Relation to beta thalassemia
Delta-beta thalassemia can mask the diagnosis of beta thalassemia trait. In beta thalassemia, an increase in hemoglobin A2 results, but the co-existence of a delta-beta thalassemia mutation will decrease the value of the hemoglobin A2 into the normal range, thereby obscuring the diagnosis of beta thalassemia trait[10]
Diagnosis
Following the detection of hypochromic microcytic red blood cells, delta-beta thalassemia is confirmed by high-performance liquid chromatography.[11]
Treatment
When needed, treatment for anemia, such as blood transfusions are used.[2]
Stem cell transplant is another option, but the donor and the individual who will receive the bone marrow transplant must be compatible, the risks involved should be evaluated.[2][12][13]
See also
- Alpha thalassemia
- Beta-thalassemia
- Hemoglobinopathy
References
- ↑ 1.0 1.1 1.2 1.3 "Delta-beta-thalassemia". http://www.orpha.net/consor/cgi-bin/OC_Exp.php?Lng=EN&Expert=231237. Retrieved 16 September 2016.
- ↑ 2.0 2.1 2.2 2.3 "Thalassaemia | Health | Patient". http://patient.info/health/thalassaemia-leaflet. Retrieved 17 September 2016.
- ↑ "HBD - hemoglobin subunit delta". http://www.orpha.net/consor/cgi-bin/Disease_Genes.php?lng=EN&data_id=20551&MISSING%20CONTENT=hemoglobin-subunit-delta&search=Disease_Genes_Simple&title=hemoglobin-subunit-delta. Retrieved 17 September 2016.
- ↑ Pal, G. K. & (2005) (in en). Textbook Of Practical Physiology - 2Nd Edn.. Orient Blackswan. p. 53. ISBN 9788125029045. https://books.google.com/books?id=XpUAihQ7Ib4C&q=microcytosis+definition&pg=PA53. Retrieved 17 September 2016.
- ↑ "Autosomal recessive: MedlinePlus Medical Encyclopedia". https://medlineplus.gov/ency/article/002052.htm. Retrieved 17 September 2016.
- ↑ "Delta beta thalassemia carrier". https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/540622/1746-delta_beta_thalassaemia-PRINT_250716.pdf. Retrieved 17 September 2016.
- ↑ "Transcription and Translation - National Human Genome Research Institute (NHGRI)". NIH. https://www.genome.gov/27552603/transcription-and-translation/. Retrieved 17 September 2016.
- ↑ (in en) Diagnostic pediatric hematopathology. Cambridge: Cambridge University Press. 2010. p. 61. ISBN 9780521881609. https://books.google.com/books?id=8s8stgvB1kUC&q=delta+beta+thalassemia+symptoms&pg=PA61. Retrieved 17 September 2016.
- ↑ "OMIM Entry - * 142000 - HEMOGLOBIN--DELTA LOCUS; HBD". http://www.omim.org/entry/142000. Retrieved 17 September 2016.
- ↑ Galanello, Renzo; Origa, Raffaella (2010). "Beta-thalassemia". Orphanet Journal of Rare Diseases 5 (1): 11. doi:10.1186/1750-1172-5-11. ISSN 1750-1172. PMID 20492708.
- ↑ "Delta-Beta Thalassaemia in a Pathan Family". Journal of the College of Physicians and Surgeons (Pakistan) 27 (11): 722–724. November 2017. PMID 29132487.
- ↑ Cao, Antonio; Galanello, Renzo (2010-02-01). "Beta-thalassemia" (in en). Genetics in Medicine 12 (2): 61–76. doi:10.1097/GIM.0b013e3181cd68ed. ISSN 1098-3600. PMID 20098328.
- ↑ "Risks" (in en-GB). https://www.nhs.uk/conditions/stem-cell-transplant/risks/.
Further reading
- Verma, S; Bhargava, M; Mittal, SK; Gupta, R (1 January 2013). "Homozygous delta-beta Thalassemia in a Child: a Rare Cause of Elevated Fetal Hemoglobin". Iranian Journal of Pediatric Hematology and Oncology 3 (1): 222–227. ISSN 2008-8892. PMID 24575268.
- Kumar, B. Vinodh; Choccalingam, Chidambharam; Samuel, Premila (1 March 2016). "Incidental Identification of Possible Delta-Beta Thalassemia Trait in a Family: A Rare Cause of Elevated Hb F.". Journal of Clinical and Diagnostic Research 10 (3): BD01–BD02. doi:10.7860/JCDR/2016/16352.7409. ISSN 2249-782X. PMID 27134860.
- "Public Health Information Network Vocabulary Access and Distribution System (PHIN VADS)". Centers for Disease Control. https://phinvads.cdc.gov/vads/http:/phinvads.cdc.gov/vads/ViewCodeSystemConcept.action?oid=2.16.840.1.113883.6.96&code=16360009. Retrieved 17 September 2016.
External links
| Classification | |
|---|---|
| External resources |