Biology:Plasmodium ovale
| Plasmodium ovale | |
|---|---|
| |
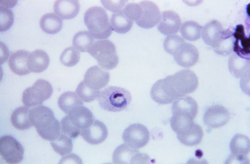
| Plasmodium ovale trophozoite, Giemsa stain. | |
| Scientific classification | |
| Domain: | Eukaryota |
| Clade: | Diaphoretickes |
| Clade: | SAR |
| Clade: | Alveolata |
| Phylum: | Apicomplexa |
| Class: | Aconoidasida |
| Order: | Haemospororida |
| Family: | Plasmodiidae |
| Genus: | Plasmodium |
| Species: | P. ovale
|
| Binomial name | |
| Plasmodium ovale Stephens, 1922
| |
Plasmodium ovale is a species of parasitic protozoon that causes tertian malaria in humans. It is one of several species of Plasmodium parasites that infect humans, including Plasmodium falciparum and Plasmodium vivax which are responsible for most cases of malaria in the world. P. ovale is rare compared to these two parasites, and substantially less dangerous than P. falciparum.
P. ovale has recently been shown by genetic methods to consist of what is considered to be two species (despite having been given subspecies names), namely P. ovale curtisi and P. ovale wallikeri.[1]
History
This species was first described in 1914 by Stephens in a blood sample taken in the autumn of 1913 from a patient in the sanitarium of Pachmari in central India and sent by Major W. H. Kenrick to Stephens (who was working in Liverpool).[2]
Epidemiology
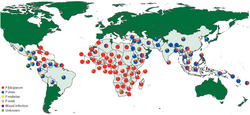
P. ovale is primarily concentrated in sub-Saharan Africa and islands in the western Pacific.[4][5] However P. ovale has also been reported in the Philippines , eastern Indonesia, and Papua New Guinea,[6] as well as in Bangladesh,[7] Cambodia,[8] India ,[9] Myanmar,[10] Thailand[11] and Vietnam[12]
In several studies, the reported prevalence of P. ovale was low relative to other malaria parasites, with fewer than 5% of malaria cases being associated with P. ovale infection. Higher prevalences of P. ovale are possible under certain conditions, as at least one study in Cameroon found the prevalence of P. ovale infection to be greater than 10%.[4]
It has been estimated that there are about 15 million cases of infection each year with this parasite.[1]
While similar to P. vivax, P. ovale is able to infect individuals who are negative for the Duffy blood group, which is the case for many residents of sub-Saharan Africa. This has been said to explain the greater prevalence of P. ovale (versus P. vivax) in most of Africa. [13] However, low-parasitaemia or subpatent P. vivax cases might be more prevalent in Africa than has been thought.[14]
Clinical features
In humans, symptoms generally appear 12 to 20 days after the parasite has entered the blood. In the blood, the parasite's replication cycle lasts approximately 49 hours, causing tertian fever which spikes approximately every 49 hours as newly replicated parasites erupt out of red blood cells. Mean maximum parasite levels have been found to be 6,944/microl for sporozoite-induced infections and 7,310/microl for trophozoite-induced infections.[4]
In some cases, relapse may occur up to 4 years after infection.[4]
Diagnosis
The microscopic appearance of P. ovale is very similar to that of P. vivax and if there are only a small number of parasites seen, it may be impossible to distinguish the two species on morphological grounds alone. There is no difference between the medical treatment of P. ovale and P. vivax, and therefore some laboratory diagnoses report "P. vivax/ovale", which is perfectly acceptable as treatment for the two is very similar. Schüffner's dots are seen on the surface of the parasitised red blood cell, but these are larger and darker than in P. vivax and are sometimes called James' dots or James' stippling. About twenty percent of the parasitised cells are oval in shape (hence the species name) and some of the oval cells also have fimbriated edges (the so-called "comet cell"). The mature schizonts of P. ovale never have more than twelve nuclei within them and this is the only reliable way of distinguishing between the two species.
P. vivax and P. ovale that have been sitting in EDTA for more than half an hour before the blood film is made will look very similar in appearance to P. malariae, which is an important reason to warn the laboratory immediately when the blood sample is drawn so they can process the sample as soon as it arrives.
Molecular tests (tests that detect DNA in blood) must take into account the fact that there are two P. ovale sensu lato taxa. Tests designed for one will not necessarily detect the other.[15]
Treatment
Standard treatment is concurrent treatment with chloroquine and primaquine. The combination atovaquone-proguanil may be used in those patients who are unable to take chloroquine for whatever reason.[16] An overdose on Chloroquine can be very dangerous and can result in death.
Phylogenetics
Among the species infecting the great apes, Plasmodium schwetzi morphologically appears to be the closest relation to P. ovale. (As of 2013) this had not been confirmed by DNA studies.
The original species has been shown to be two morphologically identical forms – Plasmodium ovale curtisi and Plasmodium ovale wallikeri – which can be differentiated only by genetic means.[1] Both species have been identified in Ghana, Myanmar, Nigeria, São Tomé, Sierra Leone and Uganda. The separation of the lineages is estimated to have occurred between 1.0 and 3.5 million years ago in hominid hosts. A second analysis suggests that these species separated 4.5 million years ago (95% confidence interval 0.5 – 7.7 Mya).[17] A third worked sequenced the whole genome of both species, confirmed the differences and dated the split at around million years.[18] Although dating is always difficult, the authors date that split to be 5 times older than the P. falciparum and P. reichenowi split.
These species appear to be more closely related to Plasmodium malariae than to Plasmodium vivax.[17]
The two species appear to differ biologically, with P. ovale wallikeri having a shorter latency period than P. ovale curtisi.[19]
Life cycle

P. ovale is introduced into the human host by the bite of an infected mosquito, in a motile form called a sporozoite. The sporozoites are carried by the blood to the liver, where they replicate asexually by merogony into non-motile merozoites. Several hundred merozoites are produced and released into the bloodstream where they infect erythrocytes. Inside the erythrocyte, the parasite's replication cycle takes approximately 49 hours, after which the erythrocyte ruptures and between 8 and 20 merozoites are released to infect other erythrocytes. Some of these merozoites will instead form gametocytes which remain in the blood and are ingested by a mosquito.[4]
When gametocytes are ingested by a mosquito, the gametocytes enter the mosquito gut where fertilisation occurs forming a zygote known as an ookinete. The ookinete moves to the outer wall of the mosquito midgut where it develops over the course of several weeks. This developing stage is called an oocyst. After the oocyst develops, it ruptures releasing several hundred sporozoites. The sporozoites are carried by the mosquito's circulation to the mosquito salivary glands. When the mosquito feeds again, the sporozoites enter through the salivary duct and are injected into a new host, starting the life cycle again.[4]
There are situations where some of the sporozoites hypothetically do not immediately start to grow and divide after entering the hepatocyte, but remain in a dormant, hypnozoite stage[21] for weeks or months. However, unlike the P. vivax situation, hypnozoites have yet to actually be seen in the life cycle of P. ovale.[22] The duration of latency is variable from one (assumed in the case of P. ovale) hypnozoite to another and the factors that will eventually trigger growth are not known; this could explain how a single infection can be responsible for a series of waves of parasitaemia or "relapses".[23]
Hosts
While humans appear to be the natural mammalian host of P. ovale, chimpanzees and Saimiri monkeys have also been experimentally infected.[4]
Anopheles gambiae and Anopheles funestus are likely the natural mosquito hosts of P. ovale. Experimentally, several other mosquito species have been shown to be capable of transmitting P. ovale to humans, including:
- Anopheles albimanus
- Anopheles atroparvus
- Anopheles dirus
- Anopheles farauti
- Anopheles freeborni
- Anopheles maculatus
- Anopheles quadrimaculatus
- Anopheles stephensi
- Anopheles subpictus[4]
Genomes
The full genomes of the two P. ovale species can be seen on geneDB.org – P. ovali curtisi P. ovale wallikeri and plasmoDB.org, published 2017.[18]
See also
- List of parasites (human)
References
- ↑ 1.0 1.1 1.2 "Two nonrecombining sympatric forms of the human malaria parasite Plasmodium ovale occur globally". The Journal of Infectious Diseases 201 (10): 1544–50. May 2010. doi:10.1086/652240. PMID 20380562.
- ↑ Stephens JWW (8 April 1914). "A new malaria parasite of man". Proc R Soc Lond B 87 (596): 375–377. doi:10.1098/rspb.1914.0024. Bibcode: 1914RSPSB..87..375S.
- ↑ Tatem AJ, Jia P, Ordanovich D, Falkner M, Huang Z, Howes R (2017). "The geography of imported malaria to non-endemic countries: a meta-analysis of nationally reported statistics.". Lancet Infect Dis 17 (1): 98–107. doi:10.1016/S1473-3099(16)30326-7. PMID 27777030.
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 4.6 4.7 "Plasmodium ovale: parasite and disease". Clinical Microbiology Reviews 18 (3): 570–81. July 2005. doi:10.1128/CMR.18.3.570-581.2005. PMID 16020691.
- ↑ "Plasmodium ovale in a highly malaria endemic area of Senegal". Transactions of the Royal Society of Tropical Medicine and Hygiene 92 (5): 522–5. 1998. doi:10.1016/S0035-9203(98)90900-2. PMID 9861368.
- ↑ "Primaquine therapy for malaria". Clinical Infectious Diseases 39 (9): 1336–45. November 2004. doi:10.1086/424663. PMID 15494911.
- ↑ "Indigenous Plasmodium ovale malaria in Bangladesh". The American Journal of Tropical Medicine and Hygiene 83 (1): 75–8. July 2010. doi:10.4269/ajtmh.2010.09-0796. PMID 20595481.
- ↑ "Large sequence heterogeneity of the small subunit ribosomal RNA gene of Plasmodium ovale in Cambodia". The American Journal of Tropical Medicine and Hygiene 72 (6): 719–24. June 2005. doi:10.4269/ajtmh.2005.72.719. PMID 15964956. http://www.ajtmh.org/cgi/pmidlookup?view=long&pmid=15964956.
- ↑ "Identification of the four human malaria parasite species in field samples by the polymerase chain reaction and detection of a high prevalence of mixed infections". Molecular and Biochemical Parasitology 58 (2): 283–92. April 1993. doi:10.1016/0166-6851(93)90050-8. PMID 8479452.
- ↑ Li, Nana; Parker, Daniel M.; Yang, Zhaoqing; Fan, Qi; Zhou, Guofa; Ai, Guoping; Duan, Jianhua; Lee, Ming-chieh et al. (2013-10-10). "Risk factors associated with slide positivity among febrile patients in a conflict zone of north-eastern Myanmar along the China-Myanmar border" (in en). Malaria Journal 12 (1): 361. doi:10.1186/1475-2875-12-361. ISSN 1475-2875. PMID 24112638.
- ↑ "Two cases of Plasmodium ovale malaria from central Thailand". Transactions of the Royal Society of Tropical Medicine and Hygiene 63 (5): 681–2. 1969. doi:10.1016/0035-9203(69)90194-1. PMID 5824291.
- ↑ "Plasmodium ovale malaria acquired in Viet-Nam". Bulletin of the World Health Organization 42 (3): 399–403. 1970. PMID 4392940.
- ↑ "Biology: Malaria (CDC malaria)". https://www.cdc.gov/malaria/biology/parasites/index.htm.
- ↑ Markus, MB (2022). "Theoretical origin of genetically homologous Plasmodium vivax malarial recurrences". Southern African Journal of Infectious Diseases 37 (1): 369. doi:10.4102/sajid.v37i1.369. PMID 35399558.
- ↑ "Recent advances in detection of Plasmodium ovale: implications of separation into the two species Plasmodium ovale wallikeri and Plasmodium ovale curtisi". Journal of Clinical Microbiology 52 (2): 387–91. February 2014. doi:10.1128/JCM.02760-13. PMID 24478466.
- ↑ "Atovaquone plus proguanil is an effective treatment for Plasmodium ovale and P. malariae malaria". Transactions of the Royal Society of Tropical Medicine and Hygiene 90 (6): 682. 1996. doi:10.1016/S0035-9203(96)90435-6. PMID 9015517.
- ↑ 17.0 17.1 "Low level of sequence diversity at merozoite surface protein-1 locus of Plasmodium ovale curtisi and P. ovale wallikeri from Thai isolates". PLOS ONE 8 (3): e58962. 2013. doi:10.1371/journal.pone.0058962. PMID 23536840. Bibcode: 2013PLoSO...858962P.
- ↑ 18.0 18.1 "Plasmodium malariae and P. ovale genomes provide insights into malaria parasite evolution". Nature 542 (7639): 101–104. February 2017. doi:10.1038/nature21038. PMID 28117441. Bibcode: 2017Natur.542..101R.
- ↑ "An observational study of malaria in British travellers: Plasmodium ovale wallikeri and Plasmodium ovale curtisi differ significantly in the duration of latency". BMJ Open 3 (5): e002711. May 2013. doi:10.1136/bmjopen-2013-002711. PMID 23793668.

- ↑ Chavatte JM, Tan SB, Snounou G, Lin RT (2015). "Molecular characterization of misidentified Plasmodium ovale imported cases in Singapore.". Malar J 14: 454. doi:10.1186/s12936-015-0985-8. PMID 26577930.
- ↑ "Malaria: origin of the term "hypnozoite"". Journal of the History of Biology 44 (4): 781–6. 2011. doi:10.1007/s10739-010-9239-3. PMID 20665090.
- ↑ Markus, MB (2021). "Safety and efficacy of tafenoquine for Plasmodium vivax malaria prophylaxis and radical cure: overview and perspectives". Therapeutics and Clinical Risk Management 17: 989–999. doi:10.2147/TCRM.S269336. PMID 34526770.
- ↑ "Malaria eModule – Exo-Erythrocytic Stages". http://www.impact-malaria.com/FR/EPS/Formations_et_cours_internationaux/Formation_de_la_Liverpool_School_LSTMH/cours_liverpool/Unit_1/1_4.html.
External links
- Malaria – TDR: For research on diseases of poverty
Wikidata ☰ Q134445 entry
 |


