Biology:Uterine microbiome
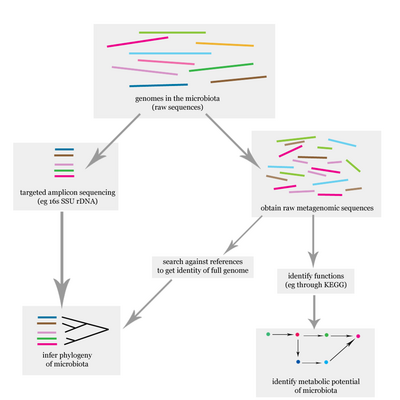
The uterine microbiome is the commensal, nonpathogenic, bacteria, viruses, yeasts/fungi present in a healthy uterus, amniotic fluid and endometrium and the specific environment which they inhabit. It has been only recently confirmed that the uterus and its tissues are not sterile.[1] Due to improved 16S rRNA gene sequencing techniques, detection of bacteria that are present in low numbers is possible.[2] Using this procedure that allows the detection of bacteria that cannot be cultured outside the body, studies of microbiota present in the uterus are expected to increase.[3]
Uterine microbiome and fertility
In the past, the uterine cavity had been traditionally considered to be sterile, but potentially susceptible to be affected by vaginal bacteria. However, this idea has been disproved. Moreover, it's been shown that endometrial and vaginal microbiota can differ in structure and composition in some women.
The microbiome of the innermost layer of the uterus, the endometrium, may influence its capacity to allow an embryo to implant. The existence of more than 10% of non-Lactobacillus bacteria in the endometrium is correlated with negative impacts on reproductive function and should be considered as an emerging cause of implantation failure and pregnancy loss.[4]
Characteristics
Bacteria, viruses and one genus of yeasts are a normal part of the uterus before and during pregnancy.[5] The uterus has been found to possess its own characteristic microbiome that differs significantly from the vaginal microbiome, consisting primarily of lactobacillus species, and at far fewer numbers.[6] In addition, the immune system is able to differentiate between those bacteria normally found in the uterus and those that are pathogenic. Hormonal changes have an effect on the microbiota of the uterus.[7]
Taxa

Commensals


The organisms listed below have been identified as commensals in the healthy uterus. Some also have the potential for growing to the point of causing disease:
Organism Commensal Transient Potential
pathogenReferences Escherichia coli x x [7] Escherichia spp. x x [7] Ureaplasma parvum x x [7] Fusobacterium nucleatum x [8] Prevotella tannerae x [5] Bacteroides spp. x [5] Streptomyces avermitilis x [7] Mycoplasma spp. x x [5] Neisseria lactamica x [7] Neisseria polysaccharea x [7] Epstein–Barr virus x x [5] Respiratory syncytial virus x x [5] Adenovirus x x [5] Candida spp. x x [5]
Pathogens
Other taxa can be present, without causing disease or an immune response. Their presence is associated with negative birth outcomes.[5][7]
Pathogenic organism Increased risk of References Ureaplasma urealyticum Premature, preterm rupture of membranes
Preterm labor
cesarean section
Placental inflammation
Congenital pneumonia
bacteremia
meningitis
fetal lung injury
death of infant[5][9][10] Haemophilus influenzae Premature, preterm rupture of membranes
preterm labor
preterm birth[5] Ureaplasma parvum [5] Fusobacterium nucleatum [5] Prevotella tannerae [5] Bacteroides spp. Streptomyces avermitilis [5] Mycoplasma hominis Congenital pneumonia
bacteremia
meningitis
<pelvic inflammatory disease
postpartum or postabortal fever[5][9] Neisseria lactamica [5] Neisseria polysaccharea [5] Epstein–Barr virus [5] Respiratory syncytial virus [5] Adenovirus [5] Candida spp. [5]
Clinical significance
Prophylactic antibiotics have been injected into the uterus to treat infertility. This has been done before the transfer of embryos with the intent to improve implantation rates. No association exists between successful implantation and antibiotic treatment.[11] Infertility treatments often progress to the point where a microbiological analysis of the uterine microbiota is performed. Preterm birth is associated with certain species of bacteria that are not normally part of the healthy uterine microbiome.[5]
Immune response
The immune response becomes more pronounced when bacteria are found that are not commensal.[5]
History
Investigations into reproductive-associated microbiomes began around 1885 by Theodor Escherich. He wrote that meconium from the newborn was free of bacteria. There was a general consensus at the time and even recently that the uterus was sterile and this was referred to as the sterile womb paradigm. Other investigations used sterile diapers for meconium collection. No bacteria were able to be cultured from the samples. Other studies showed that bacteria were detected and were directly proportional to the time between birth and the passage of meconium.[1]
Research
Investigations into the role of the uterine microbiome in the development of the infant microbiome are ongoing.[1]
See also
- Human microbiome
- Human Microbiome Project
- Human virome
- List of antimicrobial peptides in the female reproductive tract
- List of bacterial vaginosis microbiota
- Placental microbiome
- Vaginal epithelium
- Vaginal flora in pregnancy
References and notes
- ↑ 1.0 1.1 1.2 Perez-Muñoz, Maria Elisa; Arrieta, Marie-Claire; Ramer-Tait, Amanda E.; Walter, Jens (2017). "A critical assessment of the "sterile womb" and "in utero colonization" hypotheses: implications for research on the pioneer infant microbiome". Microbiome 5 (1): 48. doi:10.1186/s40168-017-0268-4. ISSN 2049-2618. PMID 28454555.
- ↑ Verstraelen, Hans; Vilchez-Vargas, Ramiro; Desimpel, Fabian; Jauregui, Ruy; Vankeirsbilck, Nele; Weyers, Steven; Verhelst, Rita; De Sutter, Petra et al. (2016). "Characterisation of the human uterine microbiome in non-pregnant women through deep sequencing of the V1-2 region of the 16S rRNA gene". PeerJ 4: e1602. doi:10.7717/peerj.1602. ISSN 2167-8359. PMID 26823997.
- ↑ Wassenaar, T.M.; Panigrahi, P. (2014). "Is a foetus developing in a sterile environment?". Letters in Applied Microbiology 59 (6): 572–579. doi:10.1111/lam.12334. ISSN 0266-8254. PMID 25273890.
- ↑ Moreno I, Codoñer FM, Vilella F, Valbuena D, Martinez-Blanch JF, Jimenez-Almazán J, Alonso R, Alamá P, Remohí J, Pellicer A, Ramon D, Simon C. Evidence that the endometrial microbiota has an effect on implantation success or failure. Am J Obstet Gynecol. 2016 Dec;215(6):684-703. doi: 10.1016/j.ajog.2016.09.075.
- ↑ 5.00 5.01 5.02 5.03 5.04 5.05 5.06 5.07 5.08 5.09 5.10 5.11 5.12 5.13 5.14 5.15 5.16 5.17 5.18 5.19 5.20 5.21 5.22 5.23 Payne, Matthew S.; Bayatibojakhi, Sara (2014). "Exploring Preterm Birth as a Polymicrobial Disease: An Overview of the Uterine Microbiome". Frontiers in Immunology 5: 595. doi:10.3389/fimmu.2014.00595. ISSN 1664-3224. PMID 25505898.
- ↑ Elnashar, Aboubakr Mohamed (2021-01-13). "Impact of endometrial microbiome on fertility". Middle East Fertility Society Journal 26 (1): 4. doi:10.1186/s43043-020-00050-3. ISSN 2090-3251.
- ↑ 7.0 7.1 7.2 7.3 7.4 7.5 7.6 7.7 Yarbrough, V. L.; Winkle, S.; Herbst-Kralovetz, M. M. (2014). "Antimicrobial peptides in the female reproductive tract: a critical component of the mucosal immune barrier with physiological and clinical implications". Human Reproduction Update 21 (3): 353–377. doi:10.1093/humupd/dmu065. ISSN 1355-4786. PMID 25547201.
- ↑ Prince, Amanda L.; Antony, Kathleen M.; Chu, Derrick M.; Aagaard, Kjersti M. (2014). "The microbiome, parturition, and timing of birth: more questions than answers". Journal of Reproductive Immunology 104–105: 12–19. doi:10.1016/j.jri.2014.03.006. ISSN 0165-0378. PMID 24793619.
- ↑ 9.0 9.1 Ureaplasma Infection: Background, Pathophysiology, Epidemiology. 17 November 2017. https://emedicine.medscape.com/article/231470-overview#a5. Retrieved 7 December 2017.
- ↑ Pryhuber, Gloria S. (2015). "Postnatal Infections and Immunology Affecting Chronic Lung Disease of Prematurity". Clinics in Perinatology 42 (4): 697–718. doi:10.1016/j.clp.2015.08.002. ISSN 0095-5108. PMID 26593074.
- ↑ Franasiak, Jason M.; Scott, Richard T. (2015). "Reproductive tract microbiome in assisted reproductive technologies". Fertility and Sterility 104 (6): 1364–1371. doi:10.1016/j.fertnstert.2015.10.012. ISSN 0015-0282. PMID 26597628.
 |

