Chemistry:Thapsigargin
| |
| Names | |
|---|---|
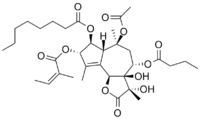
| IUPAC name
(11S)-7,11-Dihydroxy-12-oxo-6β,12-epoxy-1β,7α,10α-guai-4-ene-2β,3α,8α,10-tetrayl 10-acetate 8-butanoate 3-[(2Z)-2-methylbut-2-enoate] 2-octanoate
| |
| Systematic IUPAC name
(3S,3aR,4S,6S,6aR,7S,8S,9bS)-3,3a-Dihydroxy-3,6,9-trimethyl-2-oxo-2,3,3a,4,5,6,6a,7,8,9b-decahydroazuleno[4,5-b]furan-4,6,7,8-tetrayl 6-acetate 4-butanoate 8-[(2Z)-2-methylbut-2-enoate] 7-octanoate | |
| Identifiers | |
3D model (JSmol)
|
|
| ChEBI | |
| ChEMBL | |
| ChemSpider | |
PubChem CID
|
|
| UNII | |
| |
| |
| Properties | |
| C34H50O12 | |
| Molar mass | 650.762 g·mol−1 |
Except where otherwise noted, data are given for materials in their standard state (at 25 °C [77 °F], 100 kPa). | |
| Infobox references | |
Thapsigargin is a non-competitive inhibitor of the sarco/endoplasmic reticulum Ca2+ ATPase (SERCA).[1] Structurally, thapsigargin is classified as a guaianolide, and is extracted from a plant, Thapsia garganica.[2] It is a tumor promoter in mammalian cells.[3]
Thapsigargin raises cytosolic (intracellular) calcium concentration by blocking the ability of the cell to pump calcium into the sarcoplasmic and endoplasmic reticula. Store-depletion can secondarily activate plasma membrane calcium channels, allowing an influx of calcium into the cytosol. Depletion of ER calcium stores leads to ER stress and activation of the unfolded protein response.[4] Non-resolved ER stress can cumulatively lead to cell death.[5][6] Prolonged store depletion can protect against ferroptosis via remodeling of ER-synthesized phospholipids.[7]
Thapsigargin treatment and the resulting ER calcium depletion inhibits autophagy independent of the UPR.[8][9]
Thapsigargin is useful in experimentation examining the impacts of increasing cytosolic calcium concentrations and ER calcium depletion.
A study from the University of Nottingham showed promising results for its use against Covid-19 and other coronavirus.
Biosynthesis
The complete biosynthesis of thapsigargin has yet to be elucidated. A proposed biosynthesis starts with the farnesyl pyrophosphate. The first step is controlled by the enzyme germacrene B synthase. In the second step, the C(8) position is easily activated for an allylic oxidation due to the position of the double bond. The next step is the addition of the acyloxy moiety by a P450 acetyltransferase; which is a well known reaction for the synthesis of the diterpene, taxol. In the third step, the lactone ring is formed by a cytochrome P450 enzyme using NADP+. With the butyloxy group on the C(8), the formation will only generate the 6,12-lactone ring. The fourth step is an epoxidation that initiates the last step of the base guaianolide formation. In the fifth step, a P450 enzyme closes the 5 + 7 guaianolide structure. The ring closing is important, because it will proceed via 1,10 - epoxidation in order to retain the 4,5 - double bond needed in thapsigargin. It is not known whether the secondary modifications to the guaianolide occur before, or after the formation of thapsigargin, but will need to be considered when elucidating the true biosynthesis. It should also be noted, that several of these enzymes are P450s, therefore oxygen and NADPH are likely crucial to this biosynthesis as well as other cofactors such as Mg2+ and Mn2+ may be needed.[10]
Research
Since inhibition of SERCA is a mechanism of action that has been used to target solid tumors, thapsigargin has attracted research interest. A prodrug of thapsigargin, mipsagargin, is currently undergoing clinical trials for the treatment of glioblastoma.[11][12][13][14]
The biological activity has also attracted research into the laboratory synthesis of thapsigargin. To date, three distinct syntheses have been reported: one by Steven V. Ley,[15] one by Phil Baran.,[16] and one by P. Andrew Evans.[17]
Preclinical studies demonstrated that other effects of thapsigargin include suppression of nicotinic acetylcholine receptors activity in neurons of the guinea-pig ileum submucous plexus[18] and rat superior cervical ganglion.[19]
Laboratory studies at the University of Nottingham, using in vitro cell cultures, indicates possible potential as a broad spectrum antiviral, with activity against the COVID-19 virus (SARS-CoV-2), a common cold virus, respiratory syncytial virus (RSV), and the influenza A virus.[20]
See also
- EBC-46
References
- ↑ "Use of thapsigargin to study Ca2+ homeostasis in cardiac cells". Biosci. Rep. 15 (5): 341–9. 1995. doi:10.1007/BF01788366. PMID 8825036.
- ↑ Rasmussen U, Brøogger Christensen S, Sandberg F (1978). "Thapsigargine and thapsigargicine, two new histamine liberators from Thapsia garganica L.". Acta Pharm. Suec. 15 (2): 133–140. PMID 79299.
- ↑ Hakii, H.; Fujiki, H.; Suganuma, M.; Nakayasu, M.; Tahira, T.; Sugimura, T.; Scheuer, P. J.; Christensen, S. B. (1986). "Thapsigargin, a histamine secretagogue, is a non-12-O-tetradecanolphorbol-13-acetate (TPA) type tumor promoter in two-stage mouse skin carcinogenesis". Journal of Cancer Research and Clinical Oncology 111 (3): 177–181. doi:10.1007/BF00389230. PMID 2426275.
- ↑ Malhotra, Jyoti D.; Kaufman, Randal J. (December 2007). "The endoplasmic reticulum and the unfolded protein response". Seminars in Cell & Developmental Biology 18 (6): 716–731. doi:10.1016/j.semcdb.2007.09.003. PMID 18023214.
- ↑ Hetz, Claudio; Papa, Feroz R. (January 2018). "The Unfolded Protein Response and Cell Fate Control". Molecular Cell 69 (2): 169–181. doi:10.1016/j.molcel.2017.06.017. PMID 29107536.
- ↑ Sano, Renata; Reed, John C. (2013-12-01). "ER stress-induced cell death mechanisms". Biochimica et Biophysica Acta (BBA) - Molecular Cell Research 1833 (12): 3460–3470. doi:10.1016/j.bbamcr.2013.06.028. ISSN 0167-4889. PMID 23850759.
- ↑ Xin, Shan; Mueller, Constanze; Pfeiffer, Susanne; Kraft, Vanessa A. N.; Merl-Pham, Juliane; Bao, Xuanwen; Feederle, Regina; Jin, Xiang et al. (2021-10-18). "MS4A15 drives ferroptosis resistance through calcium-restricted lipid remodeling" (in en). Cell Death & Differentiation 29 (3): 670–686. doi:10.1038/s41418-021-00883-z. ISSN 1476-5403. PMID 34663908.
- ↑ Engedal, Nikolai; Torgersen, Maria L; Guldvik, Ingrid J; Barfeld, Stefan J; Bakula, Daniela; Sætre, Frank; Hagen, Linda K; Patterson, John B et al. (2013-10-25). "Modulation of intracellular calcium homeostasis blocks autophagosome formation". Autophagy 9 (10): 1475–1490. doi:10.4161/auto.25900. ISSN 1554-8627. PMID 23970164.
- ↑ Ganley, Ian G.; Wong, Pui-Mun; Gammoh, Noor; Jiang, Xuejun (2011). "Distinct Autophagosomal-Lysosomal Fusion Mechanism Revealed by Thapsigargin-Induced Autophagy Arrest". Molecular Cell 42 (6): 731–743. doi:10.1016/j.molcel.2011.04.024. PMID 21700220. PMC 3124681. https://www.pure.ed.ac.uk/ws/files/9879032/Distinct_autophagosomal_lysosomal_fusion_mechanism_revealed_by_thapsigargin_induced_autophagy_arrest.pdf.
- ↑ Drew, D.P.; Krichau, N.; Reichwald, K.; Simonsen, H.T. (2009). "Guaianolides in apiaceae: perspectives on pharmacology and biosynthesis". Phytochem. Rev. 8 (3): 581–599. doi:10.1007/s11101-009-9130-z.
- ↑ Denmeade, S. R.; Mhaka, A. M.; Rosen, D. M.; Brennen, W. N.; Dalrymple, S; Dach, I; Olesen, C; Gurel, B et al. (2012). "Engineering a Prostate-Specific Membrane Antigen–Activated Tumor Endothelial Cell Prodrug for Cancer Therapy". Science Translational Medicine 4 (140): 140ra86. doi:10.1126/scitranslmed.3003886. PMID 22745436.
- ↑ Andersen, Trine; López, Carmen; Manczak, Tom; Martinez, Karen; Simonsen, Henrik (2015). "Thapsigargin—From Thapsia L. To Mipsagargin". Molecules 20 (4): 6113–27. doi:10.3390/molecules20046113. PMID 25856061.
- ↑ "Mipsagargin". NCI Drug Dictionary. National Cancer Institute. 2011-02-02. https://www.cancer.gov/publications/dictionaries/cancer-drug?cdrid=666090.
- ↑ "Clinical Trials: Mipsagargin". National Cancer Institute. 17 August 2017. https://www.cancer.gov/about-cancer/treatment/clinical-trials/search/results?protocolsearchid=15658898.
- ↑ Ball, Matthew; Andrews, Stephen P.; Wierschem, Frank; Cleator, Ed; Smith, Martin D.; Ley, Steven V. (2007). "Total Synthesis of Thapsigargin, a Potent SERCA Pump Inhibitor". Organic Letters 9 (4): 663–6. doi:10.1021/ol062947x. PMID 17256950.
- ↑ Chu, Hang; Smith, Joel M.; Felding, Jakob; Baran, Phil S. (2017). "Scalable Synthesis of (−)-Thapsigargin". ACS Central Science 3 (1): 47–51. doi:10.1021/acscentsci.6b00313. PMID 28149952.
- ↑ Chen, Dezhi; Evans, P Andrew. (2017). "A Concise, Efficient and Scalable Total Synthesis of Thapsigargin and Nortrilobolide from (R)-(-)-Carvone". J. Am. Chem. Soc. 139 (17): 6046–6049. doi:10.1021/jacs.7b01734. PMID 28422492.
- ↑ Glushakov, A. V.; Glushakova, H. Y.; Skok, V. I. (1999-01-15). "Modulation of nicotinic acetylcholine receptor activity in submucous neurons by intracellular messengers". Journal of the Autonomic Nervous System 75 (1): 16–22. doi:10.1016/S0165-1838(98)00165-9. ISSN 0165-1838. PMID 9935265.
- ↑ Voitenko, S. V.; Bobryshev, A. Yu; Skok, V. I. (2000-01-01). "Intracellular regulation of neuronal nicotinic cholinorceptors". Neuroscience and Behavioral Physiology 30 (1): 19–25. doi:10.1007/BF02461388. ISSN 0097-0549. PMID 10768368.
- ↑ "Powerful Antiviral Treatment for COVID-19 Discovered That Could Change How Epidemics Are Managed". 2 February 2021. https://scitechdaily.com/powerful-antiviral-treatment-for-covid-19-discovered-that-could-change-how-epidemics-are-managed/.
<15.Dey. S.; Bajaj, S. O "Promising anticancer drug thapsigargin: A perspective toward the total synthesis" Synthetic communication 2018, 48(1), 1-13/>
Further reading
- "Thapsigargin-coated intraocular lenses inhibit human lens cell growth". Nat. Med. 3 (9): 1026–8. September 1997. doi:10.1038/nm0997-1026. PMID 9288732.
- Ibaraki N (September 1997). "A brighter future for cataract surgery". Nat. Med. 3 (9): 958–60. doi:10.1038/nm0997-958. PMID 9288718.
 |

