Medicine:Erythema nodosum
| Erythema nodosum | |
|---|---|
| Other names | Subacute migratory panniculitis of Vilanova and Piñol |
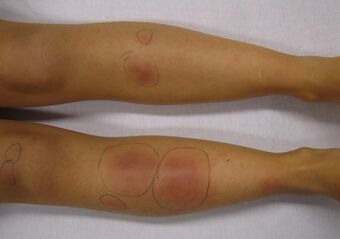 | |
| Erythema nodosum in a person who had recently had streptococcal pharyngitis | |
| Specialty | Dermatology, rheumatology |
Erythema nodosum (EN) is an inflammatory condition characterized by inflammation of the fat cells under the skin, resulting in tender red nodules or lumps that are usually seen on both shins.[1] It can be caused by a variety of conditions, and typically resolves spontaneously within 30 days.[2] It is common in young people aged 12–20 years.
Signs and symptoms
Pre-eruptive phase
The first signs of erythema nodosum are often flu-like symptoms such as a fever, cough, malaise, and aching joints. Some people also experience stiffness or swelling in the joints and weight loss.[3]
Eruptive stage
Erythema nodosum is characterised by 1–2-inch (25–51 mm) nodules (rounded lumps) below the skin surface, usually on the shins. These subcutaneous nodules can appear anywhere on the body, but the most common sites are the shins, arms, thighs, and torso. Each nodule typically disappears after around two weeks, though new ones may continue to form for up to six or eight weeks.[3] A new nodule usually appears red and is hot and firm to the touch. The redness starts to fade and it gradually becomes softer and smaller until it disappears. Each nodule usually heals completely without scarring over the course of about two weeks.[3][4] Joint pain and inflammation sometimes continue for several weeks or months after the nodules appear.[5]
Less common variants of erythema nodosum include:
- Ulcerating forms, seen in Crohn's disease
- Erythema contusiforme, when a subcutaneous hemorrhage (bleeding under the skin) occurs with an erythema nodosum lesion, causing the lesion to look like a contusion (bruise)
- Erythema nodosum migrans (also known as subacute nodular migratory panniculitis), a rare form of chronic erythema nodosum characterized by asymmetrical nodules that are mildly tender and migrate over time.[6][7][8]
-
Erythema nodosum lesion in a person with light skin and tuberculosis
-
A single lesion of erythema nodosum
-
Several lesions of erythema nodosum in an individual with dark skin
Causes
EN is associated with a wide variety of conditions.
Idiopathic
About 30–50% of EN cases are idiopathic (of an unknown cause).[9]
Infection
Infections associated with EN include:[5]
- Streptococcal infection which, in children, is by far the most common precipitant[8]
- Several granulomatous mycobacterial infections including tuberculosis,[10] leprosy,[11] and M. avium complex[12]
- Mycoplasma pneumoniae
- Histoplasma capsulatum
- Yersinia
- Lymphogranuloma venereum (LGV), caused by the bacteria Chlamydia trachomatis
- Epstein-Barr virus
- Coccidioides immitis (Valley fever)
- Cat scratch disease
Autoimmune
Autoimmune disorders associated with EN include:[6]
Immune-mediated/Idiopathic granulomatous diseases
Pregnancy
Pregnancy may be associated with EN.[6]
Medications
Medications associated with EN include:[6][9][15]
- Omeprazole
- Sulfonamides
- Penicillins
- Bromides
- Hepatitis B vaccination[16]
Cancer
Cancers associated with EN include:[6]
- Non-Hodgkin's lymphoma (NHL)
- Carcinoid tumours
- Pancreatic cancer
EN may also be due to excessive antibody production in lepromatous leprosy leading to deposition of immune complexes.[17]
There is an association with the HLA-B27 histocompatibility antigen, which is present in 65% of patients with erythema nodosum.[18]
A useful mnemonic for causes is SORE SHINS (Streptococci, OCP, Rickettsia, Eponymous (Behçet), Sulfonamides, Hansen's Disease (Leprosy), IBD, NHL, Sarcoidosis.[19]
Pathophysiology
Erythema nodosum is probably a delayed hypersensitivity reaction to a variety of antigens. Although circulating immune complexes have been demonstrated in patients with inflammatory bowel disease, they have not been found in idiopathic or uncomplicated cases.[20]
Diagnosis
Erythema nodosum is diagnosed clinically. A biopsy can be taken and examined microscopically to confirm an uncertain diagnosis.[4] Microscopic examination usually reveals a neutrophilic infiltrate surrounding capillaries that results in septal thickening, with fibrotic changes in the fat around blood vessels. A characteristic microscopic finding is radial granulomas, well-defined nodular aggregates of histiocytes surrounding a stellate cleft.[5]
Additional evaluation should be performed to determine the underlying cause of erythema nodosum. This may include a full blood count, erythrocyte sedimentation rate (ESR), antistreptolysin-O (ASO) titer and throat culture, urinalysis, intradermal tuberculin test, and a chest x-ray.[21] The ESR is typically high, the C-reactive protein elevated, and the blood showing an increase in white blood cells.[4]
The ESR is initially very high and falls as the nodules of erythema nodosum. The ASO titer is high in cases associated with a streptococcal throat infection. A chest X-ray should be performed to rule out pulmonary diseases, in particular sarcoidosis and Löfgren syndrome.[4]
Treatment
Erythema nodosum is self-limiting and usually resolves itself within 3–6 weeks. A recurring form does exist, and in children, it is attributed to repeated infections with streptococcus.[17] Treatment should focus on the underlying cause. Symptoms can be treated with bed rest, leg elevation, compressive bandages, wet dressings, and nonsteroidal anti-inflammatory agents (NSAIDs).[5] NSAIDs are usually more effective at the onset of EN versus with chronic disease.[22]
Potassium iodide can be used for persistent lesions whose cause remains unknown. Corticosteroids and colchicine can be used in severe refractory cases.[23][24] Thalidomide has been used successfully in the treatment of Erythema nodosum leprosum,[25] and it was approved by the U.S. FDA for this use in July 1998.[26] According to a 2009 meta-analysis, there is some evidence of benefit for both thalidomide and clofazimine in the treatment of erythema nodosum leprosum.[27]
Epidemiology
Erythema nodosum is the most common form of panniculitis. It is most common in the ages of 20–30, and affects women 3–6 times more than men.[4]
Eponym
The term, Subacute Migratory Panniculitis of Vilanova and Piñol, was named after the two Catalan dermatologists who provided a brief description and explanation of the disease, Xavier Montiu Vilanova (1902–1965) and Joaquin Aguade Piñol (1918–1977), in 1954, and was named in 1956.[28][29]
References
- ↑ "Erythema Nodosum". https://www.hopkinsmedicine.org/health/conditions-and-diseases/erythema-nodosum.
- ↑ Pedro-Pons, Agustín (1968) (in es). Patología y Clínica Médicas. 6 (3rd ed.). Barcelona: Salvat. p. 193. ISBN 978-84-345-1106-4.
- ↑ 3.0 3.1 3.2 "Information for Families Erythema nodosum". GOSH NHS Foundation Trust. April 2012. http://www.gosh.nhs.uk/file/985/download?token=LTc63GqW.
- ↑ 4.0 4.1 4.2 4.3 4.4 Fitzpatrick, Thomas B. (2005). Fitzpatrick's color atlas and synopsis of clinical dermatology (5th ed.). New York: McGraw-Hill. p. 148. ISBN 978-0-07-144019-6.
- ↑ 5.0 5.1 5.2 5.3 Schwartz, R. A.; Nervi, S. J. (2007). "Erythema nodosum: A sign of systemic disease". American Family Physician 75 (5): 695–700. PMID 17375516. https://www.aafp.org/link_out?pmid=17375516.
- ↑ 6.0 6.1 6.2 6.3 6.4 Gilchrist, Heidi; Patterson, James W. (2010). "Erythema nodosum and erythema induratum (nodular vasculitis): Diagnosis and management". Dermatologic Therapy 23 (4): 320–7. doi:10.1111/j.1529-8019.2010.01332.x. PMID 20666819.
- ↑ Rapini, Ronald P.; Bolognia, Jean L.; Jorizzo, Joseph L. (2007). Dermatology: 2-Volume Set. St. Louis: Mosby. ISBN 978-1-4160-2999-1.[page needed]
- ↑ 8.0 8.1 William D. James; Timothy G. Berger; Dirk M. Elston (2011). Andrews' Diseases of the skin : clinical dermatology. (11th ed.). [London]: Saunders/ Elsevier. p. 488. ISBN 978-1-4377-0314-6.
- ↑ 9.0 9.1 Mert, Ali; Ozaras, Resat; Tabak, Fehmi; Pekmezci, Salih; Demirkesen, Cuyan; Ozturk, Recep (2009). "Erythema Nodosum: An Experience of 10 Years". Scandinavian Journal of Infectious Diseases 36 (6–7): 424–7. doi:10.1080/00365540410027184. PMID 15307561.
- ↑ Laborada, Jennifer; Cohen, Philip R (2021). "Tuberculosis-Associated Erythema Nodosum". Cureus 13 (12): e20184. doi:10.7759/cureus.20184. PMID 35004007.
- ↑ Renault, Cybèle A.; Ernst, Joel D. (2015). "Mycobacterium leprae (Leprosy)". Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases. pp. 2819–2831.e2. doi:10.1016/B978-1-4557-4801-3.00252-6. ISBN 978-1-4557-4801-3.
- ↑ Budden, Heidi; Ulloa-Gutierrez, Rolando; Dobson, Simon; Scheifele, David (August 2007). "Erythema Nodosum, Mycobacterium avium Lymphadenitis, and a 15-mm Mantoux Test". Pediatric Infectious Disease Journal 26 (8): 764–765. doi:10.1097/INF.0b013e31807a2fe1. PMID 17848899.
- ↑ Areias, E; García E Silva, L (1984). "[Erythema nodosum and Crohn's disease]". Medicina Cutanea Ibero-latino-americana 12 (6): 489–95. PMID 6152299.
- ↑ Katta, Rajani (15 April 2002). "Cutaneous sarcoidosis: a dermatologic masquerader.". American Family Physician 65 (8): 1581–1584. PMID 11989634. https://www.aafp.org/link_out?pmid=11989634.
- ↑ Bohn, S; Büchner, S; Itin, P (1997). "Erythema nodosum: 112 cases. Epidemiology, clinical aspects and histopathology". Schweizerische Medizinische Wochenschrift 127 (27–28): 1168–76. PMID 9324739.
- ↑ Rogerson, S J; Nye, F J (1990). "Hepatitis B vaccine associated with erythema nodosum and polyarthritis". BMJ 301 (6747): 345. doi:10.1136/bmj.301.6747.345. PMID 2144199.
- ↑ 17.0 17.1 Kumar, Vinay; Abbas, Abul K.; Fausto, Nelson; Aster, Jon C. (2009). Robbins and Coltran Pathological Basis of Disease. Saunders/Elsevier. pp. 372–3. ISBN 978-1-4160-4930-2.
- ↑ Cunha, Burke A. (1999). Infectious disease pearls. Philadelphia: Hanley & Belfus. p. 105. ISBN 978-1-56053-203-3.
- ↑ Dr Kevin McCarthy, Cork, Ireland or DIPOUT: Drugs (e.g. sulfonamides), Infections (e.g. strep), Pregnancy, OCP, Ulcerative colitis, TB[full citation needed]
- ↑ Nguyen, Geoffrey C.; Torres, Esther A.; Regueiro, Miguel; Bromfield, Gillian; Bitton, Alain; Stempak, Joanne; Dassopoulos, Themistocles; Schumm, Philip et al. (2006). "Inflammatory Bowel Disease Characteristics Among African Americans, Hispanics, and Non-Hispanic Whites: Characterization of a Large North American Cohort". The American Journal of Gastroenterology 101 (5): 1012–23. doi:10.1111/j.1572-0241.2006.00504.x. PMID 16696785.
- ↑ García-Porrúa, Carlos; González-Gay, Miguel A.; Vázquez-Caruncho, Manuel; López-Lazaro, Luis; Lueiro, Mercedes; Fernández, Maria L.; Alvarez-Ferreira, Javier; Pujol, Ramón M. (2000). "Erythema nodosum: Etiologic and predictive factors in a defined population". Arthritis & Rheumatism 43 (3): 584–92. doi:10.1002/1529-0131(200003)43:3<584::AID-ANR15>3.0.CO;2-6. PMID 10728752.
- ↑ "Erythema Nodosum". 24 July 2020. https://www.lecturio.com/concepts/erythema-nodosum/.
- ↑ Mat, C.; Yurdakul, S; Uysal, S; Gogus, F; Ozyazgan, Y; Uysal, O; Fresko, I; Yazici, H (2005). "A double-blind trial of depot corticosteroids in Behcet's syndrome". Rheumatology 45 (3): 348–52. doi:10.1093/rheumatology/kei165. PMID 16263779.
- ↑ Yurdakul, Sebahattin; Mat, Cem; Tüzün, Yalçin; Özyazgan, Yilmaz; Hamuryudan, Vedat; Uysal, Ömer; Şenocak, Mustafa; Yazici, Hasan (2001). "A double-blind trial of colchicine in Behçet's syndrome". Arthritis & Rheumatism 44 (11): 2686–92. doi:10.1002/1529-0131(200111)44:11<2686::AID-ART448>3.0.CO;2-H. PMID 11710724.
- ↑ Silverman, W. A. (2002). "The Schizophrenic Career of a 'Monster Drug'". Pediatrics 110 (2): 404–6. doi:10.1542/peds.110.2.404. PMID 12165600.
- ↑ Rouhi, Maureen (20 June 2005). "THALIDOMIDE". Chemical & Engineering News Archive 83 (25): 122. doi:10.1021/cen-v083n025.p122.
- ↑ Van Veen, Natasja HJ; Lockwood, Diana NJ; van Brakel, Wim H; Ramirez Jr, Jose; Richardus, Jan Hendrik (8 July 2009). "Interventions for erythema nodosum leprosum". Cochrane Database of Systematic Reviews (3): CD006949. doi:10.1002/14651858.CD006949.pub2. PMID 19588412.
- ↑ Subacute Nodular Migratory Panniculitis (Vilanova Disease) at eMedicine
- ↑ Mascaró, J. M. (1978). "In memoriam Joaquin Piñol Aguadé, 1918--1977". Der Hautarzt; Zeitschrift für Dermatologie, Venerologie, und Verwandte Gebiete 29 (11): 613–4. PMID 363649.
External links
| Classification | |
|---|---|
| External resources |
 |



