Medicine:Thyroid cancer
| Thyroid cancer | |
|---|---|
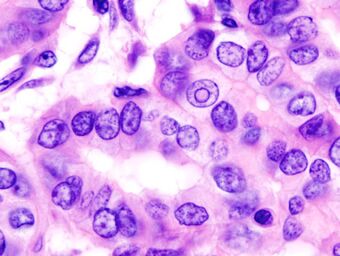 | |
| Micrograph of a papillary thyroid carcinoma demonstrating diagnostic features (nuclear clearing and overlapping nuclei). | |
| Specialty | Oncology |
| Symptoms | Swelling or lump in the neck[1] |
| Risk factors | Radiation exposure, enlarged thyroid, family history,[1][2] obesity[3] |
| Diagnostic method | Ultrasound, fine needle aspiration[1] |
| Differential diagnosis | Thyroid nodule, metastatic disease[1][4] |
| Treatment | Surgery, radiation therapy, chemotherapy, thyroid hormone, targeted therapy, watchful waiting[1] |
| Prognosis | Five year survival rates 98% (US)[5] |
| Frequency | 3.2 million (2015)[6] |
| Deaths | 31,900 (2015)[7] |
Thyroid cancer is cancer that develops from the tissues of the thyroid gland.[1] It is a disease in which cells grow abnormally and have the potential to spread to other parts of the body.[8][9] Symptoms can include swelling or a lump in the neck.[1] Cancer can also occur in the thyroid after spread from other locations, in which case it is not classified as thyroid cancer.[4]
Risk factors include radiation exposure at a young age, having an enlarged thyroid, family history and obesity.[1][2][3] The four main types are papillary thyroid cancer, follicular thyroid cancer, medullary thyroid cancer, and anaplastic thyroid cancer.[4] Diagnosis is often based on ultrasound and fine needle aspiration.[1] Screening people without symptoms and at normal risk for the disease is not recommended as of 2017.[10]
Treatment options may include surgery, radiation therapy including radioactive iodine, chemotherapy, thyroid hormone, targeted therapy, and watchful waiting.[1] Surgery may involve removing part or all of the thyroid.[4] Five-year survival rates are 98% in the United States.[5]
Globally as of 2015, 3.2 million people have thyroid cancer.[6] In 2012, 298,000 new cases occurred.[11] It most commonly is diagnosed between the ages of 35 and 65.[5] Women are affected more often than men.[5] Those of Asian descent are more commonly affected;[4] with a higher rate of mortality among Filipino females.[12] Rates have increased in the last few decades, which is believed to be due to better detection.[11] In 2015, it resulted in 31,900 deaths.[7]
Signs and symptoms
Most often, the first symptom of thyroid cancer is a nodule in the thyroid region of the neck.[13] However, up to 65% of adults have small nodules in their thyroids, but typically under 10% of these nodules are found to be cancerous.[14] Sometimes, the first sign is an enlarged lymph node. Later symptoms that can be present are pain in the anterior region of the neck and changes in voice due to an involvement of the recurrent laryngeal nerve.[15]
Thyroid cancer is usually found in a euthyroid patient, but symptoms of hyperthyroidism or hypothyroidism may be associated with a large or metastatic, well-differentiated tumor. Thyroid nodules are of particular concern when they are found in those under the age of 20. The presentation of benign nodules at this age is less likely, thus the potential for malignancy is far greater.[citation needed]
Causes
Thyroid cancers are thought to be related to a number of environmental and genetic predisposing factors, but significant uncertainty remains regarding their causes.[16]
Environmental exposure to ionizing radiation from both natural background sources and artificial sources is suspected to play a significant role, and significantly increased rates of thyroid cancer occur in those exposed to mantlefield radiation for lymphoma, and those exposed to iodine-131 following the Chernobyl,[17] Fukushima, Kyshtym, and Windscale[18] nuclear disasters.[19] Thyroiditis and other thyroid diseases also predispose to thyroid cancer.[18][20]
Genetic causes include multiple endocrine neoplasia type 2, which markedly increases rates, particularly of the rarer medullary form of the disease.[21]
Diagnosis
After a thyroid nodule is found during a physical examination, a referral to an endocrinologist or a thyroidologist may occur. Most commonly, an ultrasound is performed to confirm the presence of a nodule and assess the status of the whole gland. Some ultrasound results may report a TI-RADS or TIRADS score to categorize the risk of malignancy.[22] Measurement of thyroid stimulating hormone, free and/or total triiodothyronine (T3) and thyroxine (T4) levels, and antithyroid antibodies will help decide if a functional thyroid disease such as Hashimoto's thyroiditis is present, a known cause of a benign nodular goiter.[23] a thyroid scan, performed often in conjunction with a radioactive iodine uptake test may be used to determine whether a nodule is "hot" or "cold"[24] which may help to make a decision whether to perform a biopsy of the nodule.[25] Measurement of calcitonin is necessary to exclude the presence of medullary thyroid cancer. Finally, to achieve a definitive diagnosis before deciding on treatment, a fine needle aspiration cytology test may be performed and reported according to the Bethesda system.[26]
After diagnosis, to understand potential for spread of disease, or for follow up monitoring after surgery, a whole body I-131 or I-123 radioactive iodine scan may be performed.[27]
In adults without symptoms, screening for thyroid cancer is not recommended.[28]
Classification

Thyroid cancers can be classified according to their histopathological characteristics.[30][31] These variants can be distinguished (distribution over various subtypes may show regional variation):
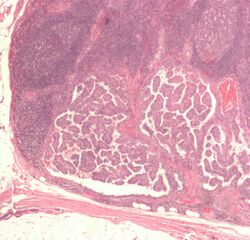
- Papillary thyroid cancer (75 to 85% of cases[32]) – is more often diagnosed in young females compared to other types of thyroid cancer and has an excellent prognosis. It may occur in women with familial adenomatous polyposis and in patients with Cowden syndrome. A follicular variant of papillary thyroid cancer also exists.[33]
- Newly reclassified variant: noninvasive follicular thyroid neoplasm with papillary-like nuclear features is considered an indolent tumor of limited biologic potential.
- Follicular thyroid cancer (10 to 20% of cases[32]) – occasionally seen in people with Cowden syndrome. Some include Hürthle cell carcinoma as a variant and others list it as a separate type.[4][34]
- Medullary thyroid cancer (5[32] to 8% of cases) – cancer of the parafollicular cells, often part of multiple endocrine neoplasia type 2.[35]
- Poorly differentiated thyroid cancer
- Anaplastic thyroid cancer (1 to 2%[36]) is not responsive to treatment and can cause pressure symptoms.
- Others
- Thyroid lymphoma
- Squamous cell thyroid carcinoma
- Sarcoma of thyroid
- Hürthle cell carcinoma
The follicular and papillary types together can be classified as "differentiated thyroid cancer".[37] These types have a more favorable prognosis than the medullary and undifferentiated types.[38]
- Papillary microcarcinoma is a subset of papillary thyroid cancer defined as a nodule measuring less than or equal to 1 cm.[39] 43% of all thyroid cancers and 50% of new cases of papillary thyroid carcinoma are papillary microcarcinoma.[40][41] Management strategies for incidental papillary microcarcinoma on ultrasound (and confirmed on FNAB) range from total thyroidectomy with radioactive iodine ablation to lobectomy or observation alone. Harach et al. suggest using the term "occult papillary tumor" to avoid giving patients distress over having cancer. Woolner et al. first arbitrarily coined the term "occult papillary carcinoma", in 1960, to describe papillary carcinomas ≤ 1.5 cm in diameter.[42]
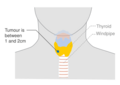
Staging
Cancer staging is the process of determining the extent of the development of a cancer. The TNM staging system is usually used to classify stages of cancers, but not of the brain.[43]
-
Stage M1 thyroid cancer
-
Stage N1a thyroid cancer
-
Stage N1b thyroid cancer
-
Stage T1a thyroid cancer
-
Stage T1b thyroid cancer
-
Stage T2 thyroid cancer
-
Stage T3 thyroid cancer
-
Stage T4a thyroid cancer
-
Stage T4b thyroid cancer
Metastases
Detection of differentiated thyroid cancer metastases may be detected by performing a full-body scintigraphy using iodine-131.[44][45]
Spread
Thyroid cancer can spread directly, via lymphatics or blood. Direct spread occurs through infiltration of the surrounding tissues. The tumor infiltrates into infrahyoid muscles, trachea, oesophagus, recurrent laryngeal nerve, carotid sheath, etc. The tumor then becomes fixed. Anaplastic carcinoma spreads mostly by direct spread, while papillary carcinoma spreads so the least. Lymphatic spread is most common in papillary carcinoma. Cervical lymph nodes become palpable in papillary carcinoma even when the primary tumor is unpalpable. Deep cervical nodes, pretracheal, prelaryngeal, and paratracheal groups of lymph nodes are often affected. The lymph node affected is usually the same side as that of the location of the tumor. Blood spread is also possible in thyroid cancers, especially in follicular and anaplastic carcinoma. The tumor emboli do angioinvasion of lungs; end of long bones, skull, and vertebrae are affected. Pulsating metastases occur because of their increased vascularity.[46]
Treatment
Thyroidectomy and dissection of central neck compartment is the initial step in treatment of thyroid cancer in the majority of cases.[13] Thyroid-preserving operations may be applied in cases, when thyroid cancer exhibits low biological aggressiveness (e.g. well-differentiated cancer, no evidence of lymph-node metastases, low MIB-1 index, no major genetic alterations like BRAF mutations, RET/PTC rearrangements, p53 mutations etc.) in patients younger than 45 years.[47] If the diagnosis of well-differentiated thyroid cancer (e.g. papillary thyroid cancer) is established or suspected by FNA, then surgery is indicated, whereas watchful waiting strategy is not recommended in any evidence-based guidelines.[47][48] Watchful waiting reduces overdiagnosis and overtreatment of thyroid cancer among old patients.[49]
Radioactive iodine-131 is used in people with papillary or follicular thyroid cancer for ablation of residual thyroid tissue after surgery and for the treatment of thyroid cancer.[50] Patients with medullary, anaplastic, and most Hurthle-cell cancers do not benefit from this therapy.[13]
External irradiation may be used when the cancer is unresectable, when it recurs after resection, or to relieve pain from bone metastasis.[13]
Sorafenib and lenvatinib are approved for advanced metastatic thyroid cancer.[51] Numerous agents are in phase II and III clinical trials.[51]
Post surgical monitoring for recurrence or metastasis may include routine ultrasound, CT scans, FDG-PET/CT, radioactive iodine whole body scans, and routine laboratory blood tests for changes in thyrogolubin, thyroglobuilin antibodies, or calcitonin, depending on the variant of thyroid cancer.[52][53][54]
Prognosis
The prognosis of thyroid cancer is related to the type of cancer and the stage at the time of diagnosis. For the most common form of thyroid cancer, papillary, the overall prognosis is excellent. Indeed, the increased incidence of papillary thyroid carcinoma in recent years is likely related to increased and earlier diagnosis. One can look at the trend to earlier diagnosis in two ways. The first is that many of these cancers are small and not likely to develop into aggressive malignancies. A second perspective is that earlier diagnosis removes these cancers at a time when they are not likely to have spread beyond the thyroid gland, thereby improving the long-term outcome for the patient. No consensus exists at present on whether this trend toward earlier diagnosis is beneficial or unnecessary.
The argument against early diagnosis and treatment is based on the logic that many small thyroid cancers (mostly papillary) will not grow or metastasize. This view holds the overwhelming majority of thyroid cancers are overdiagnosed that is, will never cause any symptoms, illness, or death for the patient, even if nothing is ever done about the cancer. Including these overdiagnosed cases skews the statistics by lumping clinically significant cases in with apparently harmless cancers.[55] Thyroid cancer is incredibly common, with autopsy studies of people dying from other causes showing that more than one-third of older adults technically have thyroid cancer, which is causing them no harm.[55] Detecting nodules that might be cancerous is easy, simply by feeling the throat, which contributes to the level of overdiagnosis. Benign (noncancerous) nodules frequently co-exist with thyroid cancer; sometimes, a benign nodule is discovered, but surgery uncovers an incidental small thyroid cancer. Increasingly, small thyroid nodules are discovered as incidental findings on imaging (CT scan, MRI, ultrasound) performed for another purpose; very few of these people with accidentally discovered, symptom-free thyroid cancers will ever have any symptoms, and treatment in such patients has the potential to cause harm to them, not to help them.[55][56]
Thyroid cancer is three times more common in women than in men, but according to European statistics,[57] the overall relative 5-year survival rate for thyroid cancer is 85% for females and 74% for males.[58]
The table below highlights some of the challenges with decision making and prognostication in thyroid cancer. While general agreement exists that stage I or II papillary, follicular, or medullary cancer have good prognoses, when evaluating a small thyroid cancer to determine which ones will grow and metastasize and which will not is not possible. As a result, once a diagnosis of thyroid cancer has been established (most commonly by a fine needle aspiration), a total thyroidectomy likely will be performed.
This drive to earlier diagnosis has also manifested itself on the European continent by the use of serum calcitonin measurements in patients with goiter to identify patients with early abnormalities of the parafollicular or calcitonin-producing cells within the thyroid gland. As multiple studies have demonstrated, the finding of an elevated serum calcitonin is associated with the finding of a medullary thyroid carcinoma in as high as 20% of cases.
In Europe where the threshold for thyroid surgery is lower than in the United States, an elaborate strategy that incorporates serum calcitonin measurements and stimulatory tests for calcitonin has been incorporated into the decision to perform a thyroidectomy; thyroid experts in the United States, looking at the same data, have for the most part not incorporated calcitonin testing as a routine part of their evaluations, thereby eliminating a large number of thyroidectomies and the consequent morbidity. The European thyroid community has focused on prevention of metastasis from small medullary thyroid carcinomas; the North American thyroid community has focused more on prevention of complications associated with thyroidectomy (see American Thyroid Association guidelines below). As demonstrated in the table below, individuals with stage III and IV disease have a significant risk of dying from thyroid cancer. While many present with widely metastatic disease, an equal number evolve over years and decades from stage I or II disease. Physicians who manage thyroid cancer of any stage recognize that a small percentage of patients with low-risk thyroid cancer will progress to metastatic disease.
Improvements have been made in thyroid cancer treatment during recent years. The identification of some of the molecular or DNA abnormalities has led to the development of therapies that target these molecular defects. The first of these agents to negotiate the approval process is vandetanib, a tyrosine kinase inhibitor that targets the RET proto-oncogene, two subtypes of the vascular endothelial growth factor receptor, and the epidermal growth factor receptor.[59] More of these compounds are under investigation and are likely to make it through the approval process. For differentiated thyroid carcinoma, strategies are evolving to use selected types of targeted therapy to increase radioactive iodine uptake in papillary thyroid carcinomas that have lost the ability to concentrate iodide. This strategy would make possible the use of radioactive iodine therapy to treat "resistant" thyroid cancers. Other targeted therapies are being evaluated, making life extension possible over the next 5–10 years for those with stage III and IV thyroid cancer.
Prognosis is better in younger people than older ones.[58]
Prognosis depends mainly on the type of cancer and cancer stage.
| Thyroid cancer type |
5-year survival | 10-year survival | ||||
|---|---|---|---|---|---|---|
| Stage I | Stage II | Stage III | Stage IV | Overall | Overall | |
| Papillary | 100%[60] | 100%[60] | 93%[60] | 51%51%[60] | 96%[61] or 97%[62] | 93%[61] |
| Follicular | 100%[60] | 100%[60] | 71%[60] | 50%[60] | 91%[61] | 85%[61] |
| Medullary | ||||||
| Anaplastic | (always stage IV)[60] | 7%[60] | 7%[60] or 14%[61] | (no data) | ||
Epidemiology
Thyroid cancer, in 2010, resulted in 36,000 deaths globally up from 24,000 in 1990.[63] Obesity may be associated with a higher incidence of thyroid cancer, but this relationship remains the subject of much debate.[64]
Thyroid cancer accounts for less than 1% of cancer cases and deaths in the UK. Around 2,700 people were diagnosed with thyroid cancer in the UK in 2011, and around 370 people died from the disease in 2012.[65]
However, in South Korea, thyroid cancer was the 5th most prevalent cancer, which accounted for 7.7% of new cancer cases in 2020.[66]
Notable cases
- Callum Ainley, English footballer[67]
- Ann-Katrin Berger, German women footballer
- Emre Can, German footballer[68]
- Jerry Dipoto, former Major League Baseball pitcher[69]
- Roger Ebert, American film critic
- Jennifer Grey, American actress
- Uhm Jung-hwa, South Korean singer, actress and dancer [70]
- Lee Moon-sae, South Korean ballad singer[71]
- Danny New, co-host of Daytime for WFLA[72][73] and previous host of Mass Appeal on WWLP.[74]
- Joe Piscopo, American actor
- Vladimir Putin, president of Russia [75]
- William Rehnquist, Chief Justice of the United States (1986–2005) died September 3, 2005, from anaplastic thyroid cancer[76]
- Katee Sackhoff, American actress
- Karen Smyers, American swimmer
- Daniel Snyder, American owner of the Washington Football Team[77]
- Rod Stewart, British singer
- Scott Thompson, American businessman
- Sofía Vergara, American actress
- Julia Volkova, Russian singer
- April Winchell, American actress
References
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 "Thyroid Cancer Treatment" (in en). 27 Apr 2017. https://www.cancer.gov/types/thyroid/patient/thyroid-treatment-pdq#section/all.
- ↑ 2.0 2.1 "Thyroid cancer". Annual Review of Medicine 65: 125–137. 2014. doi:10.1146/annurev-med-061512-105739. PMID 24274180.
- ↑ 3.0 3.1 "Body Mass Index and Thyroid Cancer Risk: A Pooled Analysis of Half a Million Men and Women in the Asia Cohort Consortium". Thyroid 32 (3): 306–314. 2022. doi:10.1089/thy.2021.0445. PMID 34915752.
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 "Thyroid Cancer Treatment" (in en). 12 May 2017. https://www.cancer.gov/types/thyroid/hp/thyroid-treatment-pdq#section/all.
- ↑ 5.0 5.1 5.2 5.3 "Cancer of the Thyroid - Cancer Stat Facts" (in en). https://seer.cancer.gov/statfacts/html/thyro.html.
- ↑ 6.0 6.1 Vos, Theo et al. (October 2016). "Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015". Lancet 388 (10053): 1545–1602. doi:10.1016/S0140-6736(16)31678-6. PMID 27733282.
- ↑ 7.0 7.1 Wang, Haidong et al. (October 2016). "Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980-2015: a systematic analysis for the Global Burden of Disease Study 2015". Lancet 388 (10053): 1459–1544. doi:10.1016/s0140-6736(16)31012-1. PMID 27733281.
- ↑ "Cancer Fact sheet N°297". February 2014. https://www.who.int/mediacentre/factsheets/fs297/en/.
- ↑ "Defining Cancer". 2007-09-17. http://www.cancer.gov/cancertopics/cancerlibrary/what-is-cancer.
- ↑ "Screening for Thyroid Cancer: US Preventive Services Task Force Recommendation Statement". JAMA 317 (18): 1882–1887. May 2017. doi:10.1001/jama.2017.4011. PMID 28492905.
- ↑ 11.0 11.1 World Cancer Report 2014.. World Health Organization. 2014. pp. Chapter 5.15. ISBN 978-9283204299.
- ↑ Paz-Pacheco, Elizabeth; Juan, Mari Des San (2 March 2023). "Incidence, Recurrence and Mortality Among Filipinos With Differentiated Thyroid Cancer: A Systematic Review". Journal of the ASEAN Federation of Endocrine Societies 38 (1): 100–107. doi:10.15605/jafes.038.01.14. PMID 37252408.
Nguyen, Michelle Linh T.; Hu, Jiaqi; Hastings, Kattherine G.; Daza, Eric J; Cullen, Mark R.; Orloff, Lisa A.; Palaniappan, Latha P. (7 September 2017). "Thyroid cancer mortality higher in Filipinos in United States: an analysis using national mortality records from 2003–2012". Cancer 123 (24): 4860–4867. doi:10.1002/cncr.30958. PMID 28881423.
Lee, Alice W.; Mendoza, Roy A.; Aman, Shehla; Jsu, Robert; Liu, Lihua (February 2022). "Thyroid cancer incidence disparities among ethnic Asian American populations, 1990–2014". Annals of Epidemiology 66: 28–36. doi:10.1016/j.annepidem.2021.11.002. PMID 34774744. https://www.sciencedirect.com/science/article/pii/S1047279721003227. Retrieved 24 October 2023. - ↑ 13.0 13.1 13.2 13.3 "Thyroid and Parathyroid Cancers". Cancer Management: A Multidisciplinary Approach (11th ed.). Lawrence, Kansas: CMP Media. 2008. ISBN 978-1-891483-62-2. http://www.cancernetwork.com/cancer-management-11/chapter05/article/10165/1402668.
- ↑ "The Diagnosis and Management of Thyroid Nodules: A Review". JAMA 319 (9): 914–924. March 2018. doi:10.1001/jama.2018.0898. PMID 29509871.
- ↑ "Thyroid Cancer" (in en). 2021-02-01. https://www.cancer.columbia.edu/cancer-types-care/types/thyroid-cancer/about-thyroid-cancer.
- ↑ "Thyroid Cancer Overview - Signaling Pathway. Diagnosis. Targeted Therapy - Creative Biolabs". https://www.creativebiolabs.net/thyroid-cancer-overview-signaling-pathway-diagnosis-targeted-therapy.htm.
- ↑ "Radioactive I-131 from Fallout". National Cancer Institute. http://www.cancer.gov/cancertopics/causes/i131.
- ↑ 18.0 18.1 "Thyroid cancer epidemiology in England and Wales: time trends and geographical distribution". British Journal of Cancer 67 (2): 330–340. February 1993. doi:10.1038/bjc.1993.61. PMID 8431362.
- ↑ "Experts link higher incidence of children's cancer to Fukushima radiation". 12 October 2015. http://www.sciencealert.com/experts-link-higher-incidence-of-children-s-cancer-to-fukushima-radiation.
- ↑ "Thyroid cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up". Annals of Oncology 21 (Suppl 5): v214–v219. May 2010. doi:10.1093/annonc/mdq190. PMID 20555084.
- ↑ "Genetics of Endocrine and Neuroendocrine Neoplasias". National Cancer Institute. 1980-01-01. http://www.cancer.gov/cancertopics/pdq/genetics/medullarythyroid/HealthProfessional.
- ↑ "Ultrasound imaging classifications of thyroid nodules for malignancy risk stratification and clinical management: state of the art". Gland Surgery 8 (Suppl 3): S233–S244. September 2019. doi:10.21037/gs.2019.07.01. PMID 31559190.
- ↑ "Diagnosis and treatment of the solitary thyroid nodule. Results of a European survey". Clinical Endocrinology 50 (3): 357–363. March 1999. doi:10.1046/j.1365-2265.1999.00663.x. PMID 10435062.
- ↑ "Thyroid scan: MedlinePlus Medical Encyclopedia" (in en). https://medlineplus.gov/ency/article/003829.htm.
- ↑ "Vol 7 Issue 6 p.3-4" (in en-US). https://www.thyroid.org/patient-thyroid-information/ct-for-patients/vol-7-issue-6/vol-7-issue-6-p-3-4/.
- ↑ "The bethesda system for reporting thyroid cytopathology: interpretation and guidelines in surgical treatment". Indian Journal of Otolaryngology and Head and Neck Surgery 64 (4): 305–311. December 2012. doi:10.1007/s12070-011-0289-4. PMID 24294568.
- ↑ "I-123 diagnostic thyroid tumor whole-body scanning with imaging at 6, 24, and 48 hours". Clinical Nuclear Medicine 27 (1): 1–8. January 2002. doi:10.1097/00003072-200201000-00001. PMID 11805475.
- ↑ "Screening for Thyroid Cancer: US Preventive Services Task Force Recommendation Statement". JAMA 317 (18): 1882–1887. May 2017. doi:10.1001/jama.2017.4011. PMID 28492905.
- ↑ "Demographic and histological subtypes of Hurthle cell tumours of the thyroid in a South African setting". South African Journal of Surgery. Suid-Afrikaanse Tydskrif vir Chirurgie 56 (3): 20–23. September 2018. doi:10.17159/2078-5151/2018/v56n3a2557. PMID 30264938.
- ↑ "Thyroid Cancer Treatment". National Cancer Institute. 1980-01-01. http://www.cancer.gov/cancertopics/pdq/treatment/thyroid/HealthProfessional/page2.
- ↑ "Thyroid cancer". National Cancer Institute. http://cancerweb.ncl.ac.uk/cancernet/101252.html#2_CELLULARCLASSIFICATION.
- ↑ 32.0 32.1 32.2 Chapter 20 in: Robbins Basic Pathology. Philadelphia: Saunders. 2007. ISBN 978-1-4160-2973-1. 8th edition.
- ↑ "Follicular variant of papillary thyroid carcinoma is a unique clinical entity: a population-based study of 10,740 cases". Thyroid 23 (10): 1263–1268. October 2013. doi:10.1089/thy.2012.0453. PMID 23477346.
- ↑ "Follicular thyroid cancer and Hürthle cell carcinoma: challenges in diagnosis, treatment, and clinical management". The Lancet. Diabetes & Endocrinology 6 (6): 500–514. June 2018. doi:10.1016/S2213-8587(17)30325-X. PMID 29102432.
- ↑ "New therapeutic approaches to treat medullary thyroid carcinoma". Nature Clinical Practice. Endocrinology & Metabolism 4 (1): 22–32. January 2008. doi:10.1038/ncpendmet0717. PMID 18084343.
- ↑ "Anaplastic Thyroid Cancer". https://columbiasurgery.org/conditions-and-treatments/anaplastic-thyroid-cancer.
- ↑ "Thyroid cancer review 2: management of differentiated thyroid cancers". International Journal of Clinical Practice 59 (12): 1459–1463. December 2005. doi:10.1111/j.1368-5031.2005.00672.x. PMID 16351679. http://www.medscape.com/viewarticle/518396.
- ↑ "Thyroid cancer review 3: management of medullary and undifferentiated thyroid cancer". International Journal of Clinical Practice 60 (1): 80–84. January 2006. doi:10.1111/j.1742-1241.2005.00673.x. PMID 16409432.
- ↑ "TNM classification of thyroid carcinoma". World Journal of Surgery 31 (5): 879–887. May 2007. doi:10.1007/s00268-006-0864-0. PMID 17308849.
- ↑ "Thyroid Papillary Microcarcinoma: Etiology, Clinical Manifestations,Diagnosis, Follow-up, Histopathology and Prognosis". Iranian Journal of Pathology 11 (1): 1–19. 2016. PMID 26870138.
- ↑ "The most commonly occurring papillary thyroid cancer in the United States is now a microcarcinoma in a patient older than 45 years". Thyroid 21 (3): 231–236. March 2011. doi:10.1089/thy.2010.0137. PMID 21268762.
- ↑ "Occult papillary carcinoma of the thyroid gland: a study of 140 cases observed in a 30-year period". The Journal of Clinical Endocrinology and Metabolism 20: 89–105. January 1960. doi:10.1210/jcem-20-1-89. PMID 13845950.
- ↑ "Cancer Staging - NCI" (in en). 2015-03-09. https://www.cancer.gov/about-cancer/diagnosis-staging/staging.
- ↑ "Bone metastases of differentiated thyroid cancer: impact of early 131I-based detection on outcome". Endocrine-Related Cancer 14 (3): 799–807. September 2007. doi:10.1677/ERC-07-0120. PMID 17914109.
- ↑ "Detection and treatment of lung metastases of differentiated thyroid carcinoma in patients with normal chest X-rays". Journal of Nuclear Medicine 29 (11): 1790–1794. November 1988. PMID 3183748.
- ↑ A concise textbook of surgery (5th ed.). Calcutta: Dr S. Das. 2008. ISBN 978-8190568128.
- ↑ 47.0 47.1 "Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer". Thyroid 19 (11): 1167–1214. November 2009. doi:10.1089/thy.2009.0110. PMID 19860577.
- ↑ British Thyroid Association, Royal College of Physicians, Perros P (2007). Guidelines for the management of thyroid cancer. 2nd edition. Report of the Thyroid Cancer Guidelines Update Group. Royal College of Physicians. p. 16. ISBN 9781860163098. http://www.british-thyroid-association.org/news/Docs/Thyroid_cancer_guidelines_2007.pdf. Retrieved 12 July 2013.
- ↑ Overdiagnosed: Making People Sick in the Pursuit of Health. Beacon Press. 18 January 2011. pp. 138–43. ISBN 9780807022009. https://archive.org/details/overdiagnosedmak0000welc. Retrieved 7 October 2012.
- ↑ "Guidelines for the management of thyroid cancer". Clinical Endocrinology 81 (Suppl 1): 1–122. July 2014. doi:10.1111/cen.12515. PMID 24989897.
- ↑ 51.0 51.1 "Recent advances in managing differentiated thyroid cancer". F1000Research 7: 86. 2018-01-18. doi:10.12688/f1000research.12811.1. PMID 29399330.
- ↑ "2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer". Thyroid 26 (1): 1–133. January 2016. doi:10.1089/thy.2015.0020. PMID 26462967.
- ↑ "Revised American Thyroid Association guidelines for the management of medullary thyroid carcinoma". Thyroid 25 (6): 567–610. June 2015. doi:10.1089/thy.2014.0335. PMID 25810047.
- ↑ "American Thyroid Association guidelines for management of patients with anaplastic thyroid cancer". Thyroid 22 (11): 1104–1139. November 2012. doi:10.1089/thy.2012.0302. PMID 23130564.
- ↑ 55.0 55.1 55.2 Overdiagnosed: Making People Sick in the Pursuit of Health. [Malaysia?]: Beacon Press. 2011. pp. 61–34. ISBN 978-0-8070-2200-9.
- ↑ "Thyroid nodules: time to stop over-reporting normal findings and update consensus guidelines". BMJ 347: f5742. September 2013. doi:10.1136/bmj.f5742. PMID 24068719.
- ↑ "Thyroid Cancer". MedicineNet.com. http://www.medicinenet.com/thyroid_cancer/article.htm.
- ↑ 58.0 58.1 Numbers from EUROCARE, from Page 10 in: Thyroid cancer. Berlin: Springer. 2005. ISBN 978-3-540-22309-2.
- ↑ "FDA approves new treatment for rare form of thyroid cancer" (Press release). U.S. Food and Drug Administration. 6 April 2011. Archived from the original on 10 April 2011. Retrieved 7 April 2011.
- ↑ 60.00 60.01 60.02 60.03 60.04 60.05 60.06 60.07 60.08 60.09 60.10 cancer.org Thyroid Cancer By the American Cancer Society. In turn citing: AJCC Cancer Staging Manual (7th ed).
- ↑ 61.0 61.1 61.2 61.3 61.4 Numbers from National Cancer Database in the US, from Page 10 in: Thyroid cancer. Berlin: Springer. 2005. ISBN 978-3-540-22309-2. (Note:Book also states that the 14% 10-year survival for anaplastic thyroid cancer was overestimated)
- ↑ Rounded up to nearest natural number from 96.7% as given by "Thyroid, Papillary Carcinoma". eMedicine. 28 September 2010. http://emedicine.medscape.com/article/282276-overview.
- ↑ "Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010". Lancet 380 (9859): 2095–2128. December 2012. doi:10.1016/S0140-6736(12)61728-0. PMID 23245604. http://www.cobiss.si/scripts/cobiss?command=DISPLAY&base=cobib&rid=1537267652&fmt=11.
- ↑ "Mechanisms in endocrinology: the crosstalk between thyroid gland and adipose tissue: signal integration in health and disease". European Journal of Endocrinology 171 (4): R137–R152. October 2014. doi:10.1530/eje-14-0067. PMID 25214234. http://eje-online.org/content/171/4/R137.long.
- ↑ "Thyroid cancer statistics". http://www.cancerresearchuk.org/cancer-info/cancerstats/types/thyroid/.
- ↑ "Republic of Korea Cancer Rates". Global Cancer Observatory (GCO). World Health Organization. 2020. https://gco.iarc.fr/today/data/factsheets/populations/410-korea-republic-of-fact-sheets.pdf.
- ↑ "Callum Ainley: Grimsby Town midfielder diagnosed with thyroid cancer". BBC Sport. 16 January 2024. https://www.bbc.co.uk/sport/football/67987683.
- ↑ Hunsley, James (27 January 2023). "'I am so grateful' - ex-Liverpool midfielder Emre Can opens up on battle with cancer". Goal.com. https://www.goal.com/en/news/ex-liverpool-midfielder-emre-can-battle-thyroid-cancer-juventus/bltafd65cb286ab51.
- ↑ Bamberger, Michael (27 May 2002). "Survivors". Sports Illustrated. http://sportsillustrated.cnn.com/vault/article/magazine/MAG1025858/index.htm. Retrieved 11 August 2013.
- ↑ "Uhm Jung-hwa had Thyroid cancer op". The Korean Herald. 20 October 2010. http://www.koreaherald.com/view.php?ud=20101020000759.
- ↑ "Lee Moon-se risks cancer relapse to keep singing". The Korean Herald. 31 March 2015. http://m.kpopherald.com/view.php?ud=201503311319126591959_2.
- ↑ "Thyroid surgeon Dr. Gary Clayman teaches Danny about his cancer diagnosis" (in en-US). 2021-01-25. https://www.wfla.com/daytime/thyroid-surgeon-dr-gary-clayman-teaches-danny-about-his-cancer-diagnosis/.
- ↑ "Danny shares he has thyroid cancer, advocates for awareness" (in en-US). 2021-01-25. https://www.wfla.com/daytime/danny-shares-he-has-thyroid-cancer-advocates-awareness/.
- ↑ "Danny New is heading back to the Sunshine State" (in en-US). 2019-12-03. https://www.wwlp.com/massappeal/danny-new-is-heading-back-to-the-sunshine-state/.
- ↑ "Putin under care of cancer doctor, bathing in deer antler blood: Report". Washington Examiner. April 3, 2022. https://www.msn.com/en-us/news/world/putin-under-care-of-cancer-doctor-bathing-in-deer-antler-blood-report/ar-AAVNqOd?ocid=winp2oct&cvid=2d2829900baf4421b2c16f94575ecf6b.
- ↑ "Rehnquist Eulogies Look Beyond Bench". The Washington Post. 8 September 2005. https://www.washingtonpost.com/wp-dyn/content/article/2005/09/07/AR2005090701791.html.
- ↑ "Celebrities with Thyroid problems". Alexander Shifrin. http://www.shifrinmd.com/celebrities-with-thyroid-problems-2.html.
External links
- Thyroid cancer at Curlie
- Management Guidelines for Patients with Thyroid Nodules and Differentiated Thyroid Cancer—The American Thyroid Association Guidelines Taskforce (2015)
| Classification | |
|---|---|
| External resources |
 |