Medicine:Knee replacement
| Knee replacement | |
|---|---|
 Knee replacement | |
| Other names | Knee arthroplasty |
| ICD-10-PCS | 0SRD0JZ |
| ICD-9-CM | 81.54 |
| MeSH | D019645 |
| MedlinePlus | 002974 |
| eMedicine | 1250275 |
Knee replacement, also known as knee arthroplasty, is a surgical procedure to replace the weight-bearing surfaces of the knee joint to relieve pain and disability, most commonly offered when joint pain is not diminished by conservative sources.[1][2] It may also be performed for other knee diseases, such as rheumatoid arthritis. In patients with severe deformity from advanced rheumatoid arthritis, trauma, or long-standing osteoarthritis, the surgery may be more complicated and carry higher risk. Osteoporosis does not typically cause knee pain, deformity, or inflammation, and is not a reason to perform knee replacement.
Knee replacement surgery can be performed as a partial or a total knee replacement.[3] In general, the surgery consists of replacing the diseased or damaged joint surfaces of the knee with metal and plastic components shaped to allow continued motion of the knee.
The operation typically involves substantial postoperative pain and includes vigorous physical rehabilitation. The recovery period may be 12 weeks or longer and may involve the use of mobility aids (e.g. walking frames, canes, crutches) to enable the patient's return to preoperative mobility.[4] It is estimated that approximately 82% of total knee replacements will last 25 years.[5]
Medical uses
Knee replacement surgery is most commonly performed in people with advanced osteoarthritis and should be considered when conservative treatments have been exhausted.[6] Total knee replacement is also an option to correct significant knee joint or bone trauma in young patients,[7] treat complex fractures in elderly, either due to previous symptomatic osteoarthritis or situations where internal fixation with plates and screws is deemed too hazardous.[8] Similarly, total knee replacement can be performed to correct mild valgus or varus deformity. Serious valgus or varus deformity should be corrected by osteotomy. Physical therapy has been shown to improve function, and may delay or prevent the need for knee replacement. Pain often is noted when performing physical activities requiring a wide range of motion in the knee joint.[9]
Pre-operative preparation

|
Angles commonly measured before knee replacement surgery: |
To indicate knee replacement in case of osteoarthritis, its radiographic classification and severity of symptoms both should be substantial. Such radiography should consist of weightbearing X-rays of both knees: AP, lateral, and 30 degrees of flexion. AP and lateral views may not show joint space narrowing, but the 30-degree flexion view is most sensitive for narrowing. Full-length projections also are used in order to adjust the prosthesis to provide a neutral angle for the distal lower extremity. Two angles used for this purpose are:
- Hip-knee-shaft angle (HKS),[10] an angle formed between a line through the longitudinal axis of the femoral shaft and its mechanical axis, which is a line from the center of the femoral head to the intercondylar notch of the distal femur.[12]
- Hip-knee-ankle angle (HKA),[11] which is an angle between the femoral mechanical axis and the center of the ankle joint.[12] It is normally between 1.0° and 1.5° of varus in adults.[13]
The patient is to perform range-of-motion exercises, and hip, knee and ankle strengthening as directed daily. Exercises that include strengthening of hip flexors, hip abductors and knee flexors helps to recover faster post operatively. Before the surgery is performed, pre-operative tests are done: usually a complete blood count, electrolytes, APTT and PT to measure blood clotting, chest X-rays, ECG, and blood cross-matching for possible transfusion. About a month before the surgery, the patient may be prescribed supplemental iron to boost the hemoglobin in their blood system. Accurate X-rays of the affected knee are needed to measure the size of components which will be needed. Medications such as warfarin and aspirin will be stopped some days before surgery to reduce the amount of bleeding. Patients may be admitted on the day of surgery if the pre-op work-up is done in the pre-anesthetic clinic or may come into hospital one or more days before surgery. As of 2017, there was insufficient quality evidence to support the use of pre-operative physiotherapy in older adults undergoing total knee arthroplasty.[14] However, as of 2022, there has been renewed interest in improving patient outcomes and "prehab" has become standard practice. [15]
Preoperative education is currently an important part of patient care. There is some evidence that it may slightly reduce anxiety before knee-replacement surgery, with low risk of detrimental effects.[16]
Knee replacement referrals are often blocked if a person is overweight because it is believed they may benefit less from surgery. However, knee replacements have been found to reduce pain and improve function, regardless of people's weight. After 10 years, most people did not need repeat surgery.[17][18] In addition, weight loss surgery before a knee replacement does not appear to change outcomes.[19]
Technique
The surgery involves exposure of the front of the knee, with detachment of part of the quadriceps muscle (vastus medialis) from the patella. The patella is displaced to one side of the joint, allowing exposure of the distal end of the femur and the proximal end of the tibia. The ends of these bones then are cut accurately to shape, using cutting guides oriented to the long axis of the bones. The cartilages and the anterior cruciate ligament are removed; the posterior cruciate ligament also may be removed but the tibial and fibular collateral ligaments are preserved.[20] Whether the posterior cruciate ligament is removed or preserved depends on the type of implant used, although there appears to be no clear difference in knee function or range of motion favoring either approach.[20] Metal components are then impacted onto the bone or fixed using polymethylmethacrylate (PMMA) cement. Alternative techniques exist that affix the implant without cement. These cement-less techniques may involve osseointegration, including porous metal prostheses. Finally, stability and range of motion are checked, followed by irrigation, hemostasis, placement of hemovacs, and closure.[21]
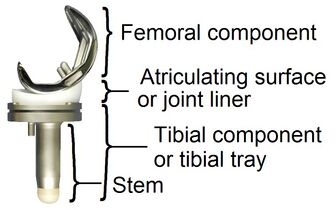
Femoral replacement
A round-ended implant is used for the femur, mimicking the natural shape of the joint. On the tibia the component is flat, although it sometimes has a stem that goes down inside the bone for further stability. A flattened or slightly dished high-density polyethylene surface is then inserted onto the tibial component so the weight is transferred metal to plastic, not metal to metal. During the operation any deformities must be corrected, and the ligaments balanced so the knee has a good range of movement, and is stable and aligned. In some cases the articular surface of the patella also is removed and replaced by a polyethylene button cemented to the posterior surface of the patella. In other cases, the patella is replaced unaltered.[citation needed]
Technology
In recent years, there has been an increase in technology assistance with implantation of total knee replacements. Traditionally, knee replacements were performed using mechanical jigs, not unlike those used in carpentry. These mechanical jigs rely on vision and human judgment. Using computer assistance to provide navigation, navigated knee replacements provide assistance in more accurate placement of implanted knee replacements based on mechanical axis. While these implants are placed more accurately, there has not been much improvement in long-term outcomes.[22] Similarly, sensor-based guidance provides accurate feedback to demonstrate soft-tissue tension to assist in guidance of insertion of knee replacements.[23] Robotic-assisted knee replacements take into account both mechanical axis and soft-tissue balancing in order to assist the surgeon in placement of a knee replacement. Short-term outcomes of robotic-assisted knee replacements are promising.[24]
Post-operative pain control
The regional analgesia techniques (neuraxial anesthesia or continuous femoral nerve block[25] or adductor canal block) are used most commonly.[26] Local anesthesia infiltration in the pericapsular area using liposomal bupivacaine provides good analgesia in the post-operative period without increasing the risk for instability or nerve injury.[27] A combined approach of local infiltration analgesia and femoral nerve block to achieve multimodal analgesia is common.[citation needed]
Modified intervastus approach
Introduced in 2018, a modified intervastus approach to the anterior knee may be used for total knee arthroplasty.[28] The procedure is intended to preserve the quadriceps tendon and vastus medialis.[28]
Tourniquet use
The current body of evidence suggests if a tourniquet is used in knee replacement surgery, it probably increases the risk of severe side effects and postoperative pain.[29] The evidence did not show any clear benefit on patient function, treatment success or quality of life.[citation needed]
Controversies
Cemented or cementless
The femoral, tibial and patellar components of a total knee replacement are fixed to the bone by using either cement or cementless total knee replacement implants. Cemented fixation is performed on the vast majority of total knee replacements. However, short-term trials suggest that there may be relief of pain.[30] There are concerns regarding tibial loosening after implantation, prohibiting widespread adoption of cementless knee replacements at this time.[31]
Denervation of the patella
There is debate regarding denervating the patella. Anterior knee pain is thought to be related to the association of the patella and femoral component. Some surgeons believe that by using electrocautery to denervate the patella, it reduces the chance of anterior knee pain postoperatively.[32][33]
Patella resurfacing
Many surgeons in the USA perform patella resurfacing routinely, while many surgeons in Asia and Europe do not. Patella resurfacing is performed by removing the cartilage from the surface of the knee and replacing it with polyethylene. Surgeons who do not routinely resurface the patella do not believe that it is a significant contribution to pain, when there is no evidence of arthritis to the patellofemoral joint. Some surgeons believe it is not cost-effective routinely to resurface the kneecap and that routine patella resurfacing may lead to increased complications such as patella fracture.[34] Other surgeons are concerned that patients with an unresurfaced patella may have increased pain postoperatively. A meta-analysis evaluating outcomes following patella resurfacing found that routine resurfacing more reliably relieves patient's pain.[35]
Tibia polyethylene component
Polyethylene is the plastic component that is inserted between the femoral and tibial components. There are several different polyethylene component designs that have been published, including posterior stabilized (PS), cruciate retaining (CR), bicruciate retaining (BCR), medial congruent (MC) and mobile bearing.[citation needed]
Ligament retaining or sacrificing
The posterior cruciate ligament (PCL) is important to the stability of the knee by preventing posterior subluxation of the tibia, reducing shear stress, increasing flexion and lever arm of the extensor mechanism by inducing femoral rollback upon flexion, and thus minimizing polyethylene abrasion through reducing stress applied to the articular surface.[36] The PS implant uses a post that is built into the implant to accommodate for the loss of PCL. Proponents of retaining the PCL advise that it is difficult to balance a CR knee and unnatural physiologic loads may increase wear of the polyethylene.[36] Multiple studies have demonstrated minimal to no difference between the two designs.[36][37]
Medial congruent polyethylene and ligament retaining
MC knee replacements attempt to mimic a more natural knee motion by decreasing motion on the medial aspect of the knee and allowing for increased motion on the lateral aspect of the joint. This mimics the external rotation and abduction of the tibia that is seen during normal ambulation. While several studies have shown improved gait profiles, long-term studies are needed to demonstrate improved results.[38][39] Conversely, the BCR knee retains the Anterior and posterior cruciate ligaments to try to mimic the normal tension of the knee's ligaments. Concerns over increased revision frequency have led to some designs being pulled from the market.[40]
Mobile bearing
A mobile bearing design allows for free motion of the polyethylene within the tibial component. Other component designs have the polyethylene member fixed to the tibial component, and only articulate at the femur/polyethylene junction.[41] There is no strong evidence that this approach improves knee function, mortality, adverse events, or amount of pain, compared with a fixed bearing approach for total knee replacement.[41] Mobile bearing designs are important to ensuring decreased wear rates in hinged knee arthroplasty.[42]
Minimally invasive
Minimally invasive procedures have been developed in total knee replacement that do not cut the quadriceps tendon. There are different definitions of minimally invasive knee surgery, which may include a shorter incision length, retraction of the patella without eversion (rotating out), and specialized instruments. There are few randomized trials, with studies finding less postoperative pain, shorter hospital stays, and shorter recovery times. These studies studies have not shown long-term benefits.[4]
Partial knee replacement
Unicompartmental arthroplasty (UKA), also called partial knee replacement, is an option for some people. The knee is generally divided into three "compartments": medial, lateral, and patellofemoral. Most people with arthritis severe enough to consider knee replacement have significant wear in two or more of the above compartments, and are treated with total knee replacement (TKA). A minority of people with osteoarthritis have wear primarily in one compartment, usually the medial, and may be candidates for unicompartmental knee replacement. Advantages of UKA compared to TKA include smaller incision, easier post-op rehabilitation, better postoperative range of motion, shorter hospital stay, less blood loss, lower risk of infection, stiffness, and blood clots, but a harder revision if necessary. Persons with infectious or inflammatory arthritis (rheumatoid arthritis, lupus, psoriasis), or marked deformity are not candidates for this procedure.[43]
Many studies demonstrate higher revision rates associated with partial knee replacements. There is significant variation in revision rates, depending on implant design and implantation technique.[44]
Components and zones
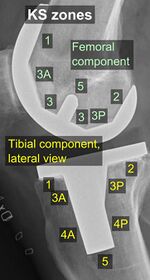
Standardized zones around the components are used for specifying, for example, signs of loosening on radiographic follow-up. There are various classification systems for specifying such zones,[46][47] including by KS (Knee Society) zones published in 2015.[45]
KS zones, anteroposterior (AP) view.[45]
Specific KS zones are as follows, with * meaning that the zone can be specified as "A" (anterior), "P" (posterior), "M" (medial) or "L" (lateral):[45]
- Femoral component (lateral view)
- Zone 1 and 2: Anterior and posterior flange, respectively.
- Zone 3: Central box/distal fixation region, where "A" and "P" designate the respective chamfers if visible*
- Zone 4: Stem extension*
- Zone 5: Stem
- Tibial component:
- Zone 1: Anterior on lateral view, medial on anteroposterior (AP) view.
- Zone 2: Posterior on lateral view, lateral on AP view.
- Zone 3: Central keel/stem/peg fixation region*
- Zone 4: Stem extension*
- Zone 5: Inferior aspect of keel or stem
Risks
Risks and complications in knee replacement[48] are similar to those associated with all joint replacements. The most serious complication is infection of the joint, which occurs in <1% of patients. Risk factors for infection are related to both patient and surgical factors.[49] Deep vein thrombosis occurs in up to 15% of patients, and is symptomatic in 2–3%. Nerve injuries occur in 1–2% of patients. Persistent pain or stiffness occurs in 8–23% of patients. Prosthesis failure occurs in approximately 2% of patients at 5 years.[4]
There is increased risk of complications for obese people going through total knee replacement.[50] The morbidly obese should be advised to lose weight before surgery and, if medically eligible, would probably benefit from bariatric surgery.[51]
Smokers have a higher risk of surgical complications (deep wound infection, superficial wound infection, and wound dehiscence) compared with nonsmokers. They also have a higher risk of pneumonia after surgery.[52]
Fracturing or chipping of the polyethylene platform between the femoral and tibial components may be of concern. These fragments may become lodged in the knee and create pain or may move to other parts of the body. Advancements in implant design have greatly reduced these issues but the potential for such an event is still present over the life span of the knee replacement.[citation needed]
Deep vein thrombosis
According to the American Academy of Orthopedic Surgeons (AAOS), deep vein thrombosis in the leg is "the most common complication of knee replacement surgery... prevention... may include periodic elevation of patient's legs, lower leg exercises to increase circulation, support stockings and medication to thin your blood."[3] Some medications used to thin the blood to prevent thrombotic events include direct oral anticoagulants (i.e. rivaroxaban, dabigatran, and apixaban), low-molecular weight heparins (i.e. dalteparin, enoxaparin), and the antiplatelet agent aspirin. Although it is suggested that aspirin is non-inferior to rivaroxaban, it is unclear if aspirin is appropriate for all patients.[53] This is specifically the case for those people who have additional risk factors for venous thromboembolisms, and those people who are at risk of aspirin resistance.[clarification needed][54]
Fractures
Periprosthetic fractures are becoming more frequent with the aging patient population and can occur intraoperatively or postoperatively. Depending on the location of the fracture and the stability of the prosthesis, these can be treated surgically with open reduction and internal fixation or revision of the prosthesis.[citation needed]
Loss of motion
The knee at times may not recover its normal range of motion (0–135 degrees usually) after total knee replacement. Much of this is dependent on pre-operative function. Most patients can achieve 0–110 degrees, but stiffness of the joint can occur. In some situations, manipulation of the knee under anesthetic is used to reduce post operative stiffness. There are also many implants from manufacturers that are designed to be "high-flex" knees, offering a greater range of motion.[citation needed]
Instability
In some patients, the kneecap dislocates to the outer side of the knee after surgery. This is painful and usually needs to be treated by surgery to realign the kneecap. However, this is quite rare.[citation needed]
Loosening
Loosening of the prosthesis can be indicated on X-ray by thin radiolucent spaces around the implant, or more obviously by implant displacement.[55]
Infection
The current classification of AAOS divides prosthetic infections into four types.[56]
- Type 1 (positive intraoperative culture): Two positive intraoperative cultures
- Type 2 (early postoperative infection): Infection occurring within first month after surgery
- Type 3 (acute hematogenous infection): Hematogenous seeding of site of previously well-functioning prosthesis
- Type 4 (late chronic infection): Chronic indolent clinical course; infection present for more than a month
While it is relatively rare, periprosthetic infection remains one of the most challenging complications of joint arthroplasty. A detailed clinical history and physical examination remain the most reliable tool to recognize a potential periprosthetic infection. In some cases the classic signs of fever, chills, painful joint, and a draining sinus may be present, and diagnostic studies are simply done to confirm the diagnosis. In reality though, most patients do not present with those clinical signs, and in fact the clinical presentation may overlap with other complications such as aseptic loosening and pain. In those cases diagnostic tests can be useful in confirming or excluding infection.[citation needed]
Modern diagnosis of infection around a total knee replacement is based on the Musculoskeletal Infection Society (MSIS) criteria.[57] They are:
1. There is a sinus tract communicating with the prosthesis; or 2. A pathogen is isolated by culture from at least two separate tissue or fluid samples obtained from the affected prosthetic joint; or
Four of the following six criteria exist:
1.Elevated serum erythrocyte sedimentation rate (ESR>30mm/hr) and serum C-reactive protein (CRP>10 mg/L) concentration,
2.Elevated synovial leukocyte count,
3.Elevated synovial neutrophil percentage (PMN%),
4.Presence of purulence in the affected joint,
5.Isolation of a microorganism in one culture of periprosthetic tissue or fluid, or
6. Greater than five neutrophils per high-power field in five high-power fields observed from histologic analysis of periprosthetic tissue at ×400 magnification.
None of the above laboratory tests has 100% sensitivity or specificity for diagnosing infection. Specificity improves when the tests are performed in patients in whom clinical suspicion exists. ESR and CRP remain good 1st line tests for screening (high sensitivity, low specificity). Aspiration of the joint remains the test with the highest specificity for confirming infection.
The choice of treatment depends on the type of prosthetic infection.[58]
- Positive intraoperative cultures: Antibiotic therapy alone
- Early post-operative infections: debridement, antibiotics, and retention of prosthesis.
- Acute hematogenous infections: debridement, antibiotic therapy, retention of prosthesis.
- Late chronic: delayed exchange arthroplasty. Surgical débridement and parenteral antibiotics alone in this group has limited success, and standard of care involves exchange arthroplasty.[59]
Post-operative evaluation

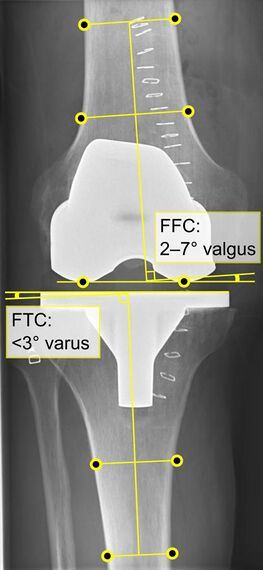
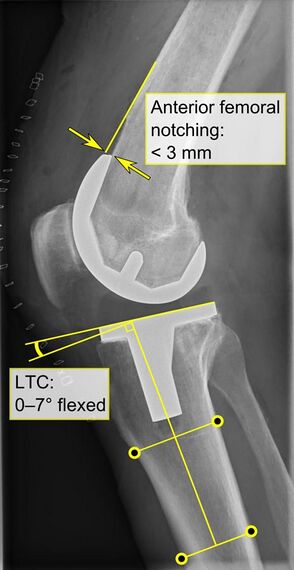
Knee replacement is routinely evaluated by X-ray, including the following measures:
HKA: Hip-knee-ankle angle, which is ideally between 3° varum to 3° valgum from a right angle.[61]
- FFC: frontal femoral component angle. It is typically regarded as optimal when being 2–7° in valgus.[62]
- FTC: frontal tibial component angle, which is regarded as optimal when being at a right angle. A varus position of more than 3° has generally been found to increase the failure rate of the prosthesis.[62]- Anterior femoral notching (the femoral component causing reduced thickness of the distal femur anteriorly), seems to cause an increased risk of fractures when exceeding about 3 mm.[63]
- LTC: lateral (or sagittal) tibial component angle, which is ideally positioned so that the tibia is 0–7° flexed compared to at a right angle with the tibial plate.[62]
Post-operative rehabilitation and follow-up
The length of post-operative hospitalization is five days on average depending on the health status of the patient and the amount of support available outside the hospital setting.[64] Protected weight bearing on crutches or a walker is required until specified by the surgeon[65] because of weakness in the quadriceps muscle.[66]
To increase the likelihood of a good outcome after surgery, multiple weeks of physical therapy are needed to help the patient return to normal activities, as well as prevent blood clots, improve circulation, increase range of motion, and eventually strengthen the surrounding muscles through specific exercises. Range of motion (to the limits of the prosthesis) is recovered over the first two weeks. Over time, patients are able to increase the amount of weight bearing on the operated leg, and eventually are able to tolerate full weight bearing with the guidance of the physical therapist.[65] After about ten months, the patient should be able to return to normal daily activities, although the operated leg may be significantly weaker than the non-operated leg.[66]
For post-operative knee replacement patients, immobility is a factor precipitated by pain and other complications. Physical immobility affects every body system and contributes to functional complications of prolonged illness.[67] In most medical-surgical hospital units that perform knee replacements, ambulation is a key aspect of nursing care that is promoted to patients. Early ambulation can decrease the risk of complications associated with immobilization such as pressure ulcers, deep vein thrombosis (DVT), impaired pulmonary function, and loss of functional mobility.[68] Promotion and execution of early ambulation on patients reduce the complications, as well as decrease length of stay and costs associated with further hospitalization.[68]
Multiple rehabilitation protocols may be used for recovery of total knee arthroplasty.[1] Continuous passive motion (CPM) is a postoperative therapy approach that uses a machine to move the knee continuously through a specific range of motion, with the goal of preventing joint stiffness and improving recovery.[69][70] There is no evidence that CPM therapy leads to a clinically significant improvement in range of motion, pain, knee function, or quality of life.[70] CPM is inexpensive, convenient, and assists patients in therapeutic compliance. However, CPM should be used in conjunction with traditional physical therapy.[69]
Sling therapy is a therapeutic modality used postoperative in order to decrease stiffness and improve range of motion following the procedure. In sling therapy, the patient's leg is placed in a standard tubular bandage that is suspended from a cross brace fixed to the bed while lying on their back . Unlike CPM, the use of sling therapy allows the patient to perform active knee flexion and extension with their leg suspended, minimizing gravity's resistance. By actively mobilizing the joint using their own muscular strength instead of outside forces like in CPM, studies show that there are clinically relevant benefits. The use of this modality is convenient and easy to set up in a hospital setting along with being less expensive than the CPM machine.[71] This treatment should be incorporated with traditional physical therapy in the postoperative acute setting.[71]
Cryotherapy or 'cold therapy' is recommended after surgery for pain relief and to limit swelling of the knee. Knee edema appears in the hours or days following the operation. It reaches its maximum level 3 to 8 days after the surgery. On average, the volume increases by 35% compared to before the operation.[72] Three months after the procedure, it is still increased by 11%. Cryotherapy involves the application of ice bags or cooled water to the skin of the knee joint. Stretching helps to improve range of motion as well during initial rehabilitation. Post surgery the range of motion is limited due to the immobilization, which leads to increased muscle stiffness. Hence, stretching helps to extend the shortened muscle and gradually improving the range of motion.[73] Some physicians and patients may consider having ultrasonography for deep venous thrombosis after knee replacement.[74][75] Neither gabapentin nor pregabalin have been found to be useful for pain following a knee replacement.[76] A Cochrane review concluded that early multidisciplinary rehabilitation programs may produce better results.[77]
Follow-up assessments are conducted to examine the need for revision surgery. This is because there is an increased risk of prosthesis failure over time due to factors such as the material used, infection, and dislocation. However, a UK study showed that only 5% of knee replacements needed a revision. Researchers recommended that routine follow-up may not be needed for up to 10 years. At this point, x-rays should be used to assess the joint, and there should be a clinical assessment of pain and mobility.[78] [79]
After the surgery, 88% of individuals regain their preoperative level of physical activity and sports. Even ten years later, 70% of them continue to engage in sports.[80]
Frequency
With 718,000 hospitalizations, knee arthroplasty accounted for 4.6% of all United States operating room procedures in 2011—making it one of the most common procedures performed during hospital stays.[81][82] The number of knee arthroplasty procedures performed in U.S. hospitals increased 93% between 2001 and 2011.[83] A study of United States community hospitals showed that in 2012, among hospitalizations that involved an OR procedure, knee arthroplasty was the OR procedure performed most frequently during hospital stays paid by Medicare (10.8 percent of stays) and by private insurance (9.1 percent). Knee arthroplasty was not among the top five most frequently performed OR procedures for stays paid by Medicaid or for uninsured stays.[84]
By 2030, the demand for primary total knee arthroplasty is projected to increase to 3.48 million surgeries performed annually in the U.S.[85]
Fall risk after total knee arthroplasty
With osteoarthritis (OA) being the number one reason for total knee arthoplasty (TKA) surgery, it is important to understand that balance deficits significantly impact the quality of daily living in patients with knee OA and are also linked to greater risk of falling and poor mobility. Annually in the US, 40% of all patients with OA report a history of falls. TKA surgery has shown to decrease fall risk and fear of falling in pre-operative fallers with OA versus non-operative fallers by 54% following TKA.[86]
See also
- Autologous chondrocyte implantation
- Microfracture surgery
- Knee osteoarthritis
- Osseointegration
- Meniscus transplant
References
- ↑ 1.0 1.1 "Efficacy of proprioceptive training on the recovery of total joint arthroplasty patients: a meta-analysis". Journal of Orthopaedic Surgery and Research 15 (1): 505. November 2020. doi:10.1186/s13018-020-01970-6. PMID 33143719.
- ↑ "Total Knee Arthroplasty". Medscape Reference. 27 June 2012. http://emedicine.medscape.com/article/1250275-overview#showall.
- ↑ 3.0 3.1 "Total Knee Replacement". American Academy of Orthopedic Surgeons. December 2011. http://orthoinfo.aaos.org/topic.cfm?topic=A00389.
- ↑ 4.0 4.1 4.2 "Minimally invasive total knee arthroplasty for osteoarthritis". The New England Journal of Medicine 360 (17): 1749–58. April 2009. doi:10.1056/NEJMct0806027. PMID 19387017.
- ↑ "How long does a knee replacement last? A systematic review and meta-analysis of case series and national registry reports with more than 15 years of follow-up". Lancet 393 (10172): 655–663. February 2019. doi:10.1016/S0140-6736(18)32531-5. PMID 30782341.
- ↑ "Management of primary knee osteoarthritis and indications for total knee arthroplasty for general practitioners". The Journal of the American Osteopathic Association 112 (11): 709–15. November 2012. PMID 23139341.
- ↑ "3D printing durable patient specific knee implants". Journal of Orthopaedics 14 (1): 182–183. March 2017. doi:10.1016/j.jor.2016.12.015. PMID 28123259.
- ↑ Parratte, S.; Ollivier, M.; Argenson, J. -N. (2018-02-01). "Primary total knee arthroplasty for acute fracture around the knee". Orthopaedics & Traumatology: Surgery & Research. 2017 Instructional Course Lectures (SoFCOT) 104 (1, Supplement): S71–S80. doi:10.1016/j.otsr.2017.05.029. ISSN 1877-0568. https://www.sciencedirect.com/science/article/pii/S1877056817303365.
- ↑ "Effectiveness of manual physical therapy and exercise in osteoarthritis of the knee. A randomized, controlled trial". Annals of Internal Medicine 132 (3): 173–81. February 2000. doi:10.7326/0003-4819-132-3-200002010-00002. PMID 10651597.
- ↑ 10.0 10.1 "Frontal plane knee alignment: a call for standardized measurement". The Journal of Rheumatology 34 (9): 1796–801. September 2007. PMID 17787049.
- ↑ 11.0 11.1 "Association between knee alignment and knee pain in patients surgically treated for medial knee osteoarthritis by high tibial osteotomy. A one year follow-up study". BMC Musculoskeletal Disorders 10 (1): 154. December 2009. doi:10.1186/1471-2474-10-154. PMID 19995425.
- ↑ 12.0 12.1 "Mechanical, Anatomical, and Kinematic Axis in TKA: Concepts and Practical Applications". Current Reviews in Musculoskeletal Medicine 7 (2): 89–95. June 2014. doi:10.1007/s12178-014-9218-y. PMID 24671469.
- ↑ "Does measurement of the anatomic axis consistently predict hip-knee-ankle angle (HKA) for knee alignment studies in osteoarthritis? Analysis of long limb radiographs from the multicenter osteoarthritis (MOST) study". Osteoarthritis and Cartilage 19 (1): 58–64. January 2011. doi:10.1016/j.joca.2010.09.011. PMID 20950695.
- ↑ "Does preoperative physiotherapy improve postoperative, patient-based outcomes in older adults who have undergone total knee arthroplasty? A systematic review". Physiotherapy Theory and Practice 33 (1): 9–30. January 2017. doi:10.1080/09593985.2016.1230660. PMID 27736286.
- ↑ "Prehabilitation Improves Knee Functioning Before and Within the First Year After Total Knee Arthroplasty: A Systematic Review With Meta-analysis". Journal of Orthopaedic & Sports Physical Therapy 52 (11): 709–725. November 2022. doi:10.2519/jospt.2022.11160.
- ↑ "Preoperative education for hip or knee replacement". The Cochrane Database of Systematic Reviews 2014 (5): CD003526. May 2014. doi:10.1002/14651858.CD003526.pub3. PMID 24820247.
- ↑ "Obesity alone should not rule out knee replacement surgery" (in en). NIHR Evidence (National Institute for Health and Care Research). 2022-09-01. doi:10.3310/nihrevidence_53214. https://evidence.nihr.ac.uk/alert/obesity-should-not-rule-out-knee-replacement-surgery/.
- ↑ Jämsen, Esa, ed (July 2021). "Obesity and revision surgery, mortality, and patient-reported outcomes after primary knee replacement surgery in the National Joint Registry: A UK cohort study". PLOS Medicine 18 (7): e1003704. doi:10.1371/journal.pmed.1003704. PMID 34270557.
- ↑ "Does bariatric surgery prior to total hip or knee arthroplasty reduce post-operative complications and improve clinical outcomes for obese patients? Systematic review and meta-analysis". The Bone & Joint Journal 98-B (9): 1160–6. September 2016. doi:10.1302/0301-620x.98b9.38024. PMID 27587514. https://ueaeprints.uea.ac.uk/58880/1/Bariatric_surgery_paper_ACCEPTED_10.05.2016.pdf.
- ↑ 20.0 20.1 "Retention versus sacrifice of the posterior cruciate ligament in total knee arthroplasty for treating osteoarthritis". The Cochrane Database of Systematic Reviews 2013 (10): CD004803. October 2013. doi:10.1002/14651858.CD004803.pub3. PMID 24114343.
- ↑ "Posterior Cruciate-Retaining Total Knee Arthroplasty.". Journal of Medical Insight 3 (8). July 2017. doi:10.24296/jomi/20.
- ↑ "Current state of the art in total knee arthroplasty computer navigation". Knee Surgery, Sports Traumatology, Arthroscopy 24 (11): 3565–3574. November 2016. doi:10.1007/s00167-016-4337-1. PMID 27704159.
- ↑ "Sensor-Based Soft Tissue Balancing in Total Knee Arthroplasty". Intelligent Orthopaedics. Advances in Experimental Medicine and Biology. 1093. 2018. pp. 327–334. doi:10.1007/978-981-13-1396-7_25. ISBN 978-981-13-1395-0.
- ↑ "Robotic Arm-Assisted Total Knee Arthroplasty". The Journal of Arthroplasty 33 (7): 2002–2006. July 2018. doi:10.1016/j.arth.2018.01.060. PMID 29506926.
- ↑ "Comparison of peri- and intraarticular analgesia with femoral nerve block after total knee arthroplasty: a randomized clinical trial". Acta Orthopaedica 78 (2): 172–9. April 2007. doi:10.1080/17453670710013645. PMID 17464603.
- ↑ American Society of Anesthesiologists Task Force on Acute Pain Management (February 2012). "Practice guidelines for acute pain management in the perioperative setting: an updated report by the American Society of Anesthesiologists Task Force on Acute Pain Management". Anesthesiology 116 (2): 248–73. doi:10.1097/ALN.0b013e31823c1030. PMID 22227789.
- ↑ "Local infiltration analgesia versus intrathecal morphine for postoperative pain management after total knee arthroplasty: a randomized controlled trial". Anesthesia and Analgesia 113 (4): 926–33. October 2011. doi:10.1213/ANE.0b013e3182288deb. PMID 21821506.
- ↑ 28.0 28.1 "Modified Intervastus Approach to the Knee". The Journal of Knee Surgery 31 (5): 422–424. May 2018. doi:10.1055/s-0037-1604150. PMID 28701009.
- ↑ "Tourniquet use for knee replacement surgery". The Cochrane Database of Systematic Reviews 2020 (12): CD012874. December 2020. doi:10.1002/14651858.cd012874.pub2. PMID 33316105.
- ↑ "Cemented, cementless or hybrid fixation options in total knee arthroplasty for osteoarthritis and other non-traumatic diseases". The Cochrane Database of Systematic Reviews 10: CD006193. October 2012. doi:10.1002/14651858.cd006193.pub2. PMID 23076921.
- ↑ "Results of Cemented vs Cementless Primary Total Knee Arthroplasty Using the Same Implant Design". The Journal of Arthroplasty 33 (4): 1089–1093. April 2018. doi:10.1016/j.arth.2017.11.048. PMID 29275115.
- ↑ "Patella denervation in primary total knee arthroplasty - a randomized controlled trial with 2 years of follow-up". The Journal of Arthroplasty 29 (5): 977–81. May 2014. doi:10.1016/j.arth.2013.10.017. PMID 24291230.
- ↑ "Effect of Patellar Electrocautery Neurectomy on Postoperative Pain among Patients Referred for Total Knee Arthroplasty". Advanced Biomedical Research 7: 9. 2018. doi:10.4103/abr.abr_154_16. PMID 29456980.
- ↑ "Routine Patellar Resurfacing During Total Knee Arthroplasty Is Not Cost-Effective in Patients Without Patellar Arthritis". The Journal of Arthroplasty 34 (9): 1963–1968. September 2019. doi:10.1016/j.arth.2019.04.040. PMID 31104838. https://jdc.jefferson.edu/orthoposters/1.
- ↑ "Better outcomes with patellar resurfacing during primary total knee arthroplasty: a meta-analysis study". Archives of Orthopaedic and Trauma Surgery 139 (10): 1445–1454. October 2019. doi:10.1007/s00402-019-03246-z. PMID 31367842.
- ↑ 36.0 36.1 36.2 "Functional comparison of posterior cruciate-retaining versus posterior stabilized total knee arthroplasty". The Journal of Arthroplasty 19 (3): 349–53. April 2004. doi:10.1016/j.arth.2003.09.010. PMID 15067650.
- ↑ "Outcomes of Posterior-Stabilized Compared with Cruciate-Retaining Total Knee Arthroplasty". The Journal of Knee Surgery 31 (4): 321–340. April 2018. doi:10.1055/s-0037-1603902. PMID 28666292.
- ↑ "Comparison of posterior-stabilized, cruciate-retaining, and medial-stabilized knee implant motion during gait". Journal of Orthopaedic Research 38 (8): 1753–1768. August 2020. doi:10.1002/jor.24613. PMID 31994751.
- ↑ "A Randomized Controlled Trial Comparing a Medial Stabilized Total Knee Prosthesis to a Cruciate Retaining and Posterior Stabilized Design: A Report of the Clinical and Functional Outcomes Following Total Knee Replacement". The Journal of Arthroplasty 35 (6): 1583–1590.e2. June 2020. doi:10.1016/j.arth.2020.01.085. PMID 32139194.
- ↑ "Mean Three-Year Survivorship of a New Bicruciate-Retaining Total Knee Arthroplasty: Are Revisions Still Higher Than Expected?". The Journal of Arthroplasty 34 (9): 1957–1962. September 2019. doi:10.1016/j.arth.2019.04.030. PMID 31160154.
- ↑ 41.0 41.1 "Mobile bearing vs fixed bearing prostheses for posterior cruciate retaining total knee arthroplasty for postoperative functional status in patients with osteoarthritis and rheumatoid arthritis". The Cochrane Database of Systematic Reviews (2): CD003130. February 2015. doi:10.1002/14651858.CD003130.pub3. PMID 25650566.
- ↑ "Evolution of the rotating hinge for complex total knee arthroplasty" (in en-US). Clinical Orthopaedics and Related Research 392 (392): 292–9. November 2001. doi:10.1097/00003086-200111000-00038. PMID 11716398.
- ↑ (in en) Design of Artificial Human Joints & Organs. Springer Science & Business Media. 2013-08-31. ISBN 978-1-4614-6255-2. https://books.google.com/books?id=U4u9BAAAQBAJ&q=partial+knee+replacement+Persons+with+infectious+or+inflammatory+arthritis+(rheumatoid+arthritis,+lupus,+psoriasis),+or+marked+deformity+are+not+candidates+for+this+procedure&pg=PA203.
- ↑ "Annual revision rates of partial versus total knee arthroplasty: A comparative meta-analysis". The Knee 24 (2): 179–190. March 2017. doi:10.1016/j.knee.2016.11.006. PMID 27916580.
- ↑ 45.0 45.1 45.2 45.3 "Development of a Modern Knee Society Radiographic Evaluation System and Methodology for Total Knee Arthroplasty". The Journal of Arthroplasty 30 (12): 2311–4. December 2015. doi:10.1016/j.arth.2015.05.049. PMID 26122112.
- ↑ "A prospective evaluation of a largely cementless total knee arthroplasty cohort without patellar resurfacing: 10-year outcomes and survivorship". BMC Musculoskeletal Disorders 19 (1): 205. June 2018. doi:10.1186/s12891-018-2128-1. PMID 29945574.
- ↑ "How to interpret postoperative X-rays after total knee arthroplasty". Orthopaedic Surgery 6 (3): 179–86. August 2014. doi:10.1111/os.12123. PMID 25179351.
- ↑ "Knee Replacement Surgery in Bangalore - Vydehi Institute of Medical Sciences". http://www.vims.ac.in/healthcare/joint-replace-recovery-process.html.
- ↑ "The impact of patient and surgical factors on the rate of infection after primary total knee arthroplasty: an analysis of 64,566 joints from the New Zealand Joint Registry". The Bone & Joint Journal 98-B (3): 334–40. March 2016. doi:10.1302/0301-620X.98B3.36775. PMID 26920958.
- ↑ "The influence of obesity on the complication rate and outcome of total knee arthroplasty: a meta-analysis and systematic literature review". The Journal of Bone and Joint Surgery. American Volume 94 (20): 1839–44. October 2012. doi:10.2106/JBJS.K.00820. PMID 23079875.
- ↑ "Total knee replacement in the morbidly obese: a literature review". ANZ Journal of Surgery 80 (9): 595–9. September 2010. doi:10.1111/j.1445-2197.2010.05396.x. PMID 20840400.
- ↑ "Impact of smoking on the incidence and post-operative complications of total knee arthroplasty: A systematic review and meta-analysis of cohort studies". Bosnian Journal of Basic Medical Sciences 22 (3): 353–365. June 2022. doi:10.17305/bjbms.2021.6538. PMID 34923952.
- ↑ "Aspirin or Rivaroxaban for VTE Prophylaxis after Hip or Knee Arthroplasty". The New England Journal of Medicine 378 (8): 699–707. February 2018. doi:10.1056/NEJMoa1712746. PMID 29466159.
- ↑ "A Narrative Review of Aspirin Resistance in VTE Prophylaxis for Orthopaedic Surgery". Drugs 80 (18): 1889–1899. December 2020. doi:10.1007/s40265-020-01413-w. PMID 33037568.
- ↑ "Imaging of knee implants and related complications". Diagnostic and Interventional Imaging 97 (7–8): 809–21. 2016. doi:10.1016/j.diii.2016.02.015. PMID 27423710.
- ↑ "Management of infection at the site of a total knee arthroplasty". Instructional Course Lectures 55: 449–61. 2006. PMID 16958480.
- ↑ "New definition for periprosthetic joint infection: from the Workgroup of the Musculoskeletal Infection Society". Clinical Orthopaedics and Related Research 469 (11): 2992–4. November 2011. doi:10.1007/s11999-011-2102-9. PMID 21938532.
- ↑ "Infection after total knee arthroplasty. A retrospective study of the treatment of eighty-one infections". The Journal of Bone and Joint Surgery. American Volume 81 (10): 1434–45. October 1999. doi:10.2106/00004623-199910000-00008. PMID 10535593.
- ↑ "Surgical débridement and parenteral antibiotics in infected revision total knee arthroplasty". Clinical Orthopaedics and Related Research 461: 130–5. August 2007. doi:10.1097/BLO.0b013e318063e7f3. PMID 17438469.
- ↑ "The Impact Of Tibial Component Overhang On Outcome Scores And Pain In Total Knee Replacement". Orthopaedic Proceedings. 2018-02-21.
- ↑ "Influence of navigation system updates on total knee arthroplasty". BMC Sports Science, Medicine & Rehabilitation 5 (1): 10. 2013. doi:10.1186/2052-1847-5-10. PMID 23638774. (CC-BY-2.0)
- ↑ 62.0 62.1 62.2 "What is the optimal alignment of the tibial and femoral components in knee arthroplasty?". Acta Orthopaedica 85 (5): 480–7. September 2014. doi:10.3109/17453674.2014.940573. PMID 25036719.
- ↑ "Risk of Anterior Femoral Notching in Navigated Total Knee Arthroplasty". Clinics in Orthopedic Surgery 7 (2): 217–24. June 2015. doi:10.4055/cios.2015.7.2.217. PMID 26217469.
- ↑ "Predicting length of stay from an electronic patient record system: a primary total knee replacement example". BMC Medical Informatics and Decision Making 14 (1): 26. April 2014. doi:10.1186/1472-6947-14-26. PMID 24708853.
- ↑ 65.0 65.1 "Rehabilitation". http://www.massgeneral.org/ortho-hip-knee/patient-education/pt-ed-kneerehab.pdf.
- ↑ 66.0 66.1 "Muscle deficits persist after unilateral knee replacement and have implications for rehabilitation". Physical Therapy 89 (10): 1072–9. October 2009. doi:10.2522/ptj.20070295. PMID 19713269.
- ↑ "Mobility: a successful investment for critically ill patients. Foreword". Critical Care Nursing Quarterly 36 (1): 1–2. 2013. doi:10.1097/cnq.0b013e3182750631. PMID 23221435.
- ↑ 68.0 68.1 Teodoro, 2016 [full citation needed]
- ↑ 69.0 69.1 "Five Things Physicians and Patients Should Question". Choosing Wisely: an initiative of the ABIM Foundation. American Physical Therapy Association. 15 September 2014. http://www.choosingwisely.org/doctor-patient-lists/american-physical-therapy-association/.
- ↑ 70.0 70.1 "Continuous passive motion following total knee arthroplasty in people with arthritis". The Cochrane Database of Systematic Reviews (2): CD004260. February 2014. doi:10.1002/14651858.CD004260.pub3. PMID 24500904.
- ↑ 71.0 71.1 "The effect of continuous passive motion and sling exercise training on clinical and functional outcomes following total knee arthroplasty: a randomized active-controlled clinical study". Health and Quality of Life Outcomes 12 (1): 68. May 2014. doi:10.1186/1477-7525-12-68. PMID 24886619.
- ↑ Loyd, Brian J.; Kittelson, Andrew J.; Forster, Jeri; Stackhouse, Scott; Stevens-Lapsley, Jennifer (2020-06-04). "Development of a reference chart to monitor postoperative swelling following total knee arthroplasty" (in en). Disability and Rehabilitation 42 (12): 1767–1774. doi:10.1080/09638288.2018.1534005. ISSN 0963-8288. PMID 30668214. https://www.tandfonline.com/doi/full/10.1080/09638288.2018.1534005.
- ↑ "A way to reduce manipulations under anaesthetic the STAK tool: a stretching device to treat arthrofibrosis following total knee replacement" (in en). Physiotherapy 107: e6. May 2020. doi:10.1016/j.physio.2020.03.011.
- ↑ American Academy of Orthopaedic Surgeons (February 2013), "Five Things Physicians and Patients Should Question", Choosing Wisely: an initiative of the ABIM Foundation (American Academy of Orthopaedic Surgeons), http://www.choosingwisely.org/doctor-patient-lists/american-academy-of-orthopaedic-surgeons/
- ↑ "Preventing venous thromboembolic disease in patients undergoing elective total hip and knee arthroplasty". The Journal of Bone and Joint Surgery. American Volume 94 (8): 673–4. April 2012. doi:10.2106/JBJS.9408edit. PMID 22517384.
- ↑ "A Meta-Analysis on the Use of Gabapentinoids for the Treatment of Acute Postoperative Pain Following Total Knee Arthroplasty". The Journal of Bone and Joint Surgery. American Volume 98 (16): 1340–50. August 2016. doi:10.2106/jbjs.15.01202. PMID 27535436. https://ora.ox.ac.uk/objects/uuid:cbe29197-14a9-47dc-b961-2ad3e24fd1c0. Retrieved 1 September 2020.
- ↑ "Multidisciplinary rehabilitation programmes following joint replacement at the hip and knee in chronic arthropathy". The Cochrane Database of Systematic Reviews 2010 (2): CD004957. April 2008. doi:10.1002/14651858.cd004957.pub3. PMID 18425906.
- ↑ "Joint replacements: many people can safely wait 10 years for follow-up". NIHR Evidence (National Institute for Health and Care Research). 11 January 2023. https://evidence.nihr.ac.uk/alert/joint-replacement-many-people-can-safely-wait-10-years-for-follow-up/.
- ↑ Kingsbury, Sarah R; Smith, Lindsay K; Czoski Murray, Carolyn J; Pinedo-Villanueva, Rafael; Judge, Andrew; West, Robert; Smith, Chris; Wright, Judy M et al. (2022-06-01). "Safety of disinvestment in mid- to late-term follow-up post primary hip and knee replacement: the UK SAFE evidence synthesis and recommendations" (in en). Health and Social Care Delivery Research 10 (16): 1–172. doi:10.3310/KODQ0769. ISSN 2755-0060. PMID 35767667. https://www.journalslibrary.nihr.ac.uk/hsdr/KODQ0769.
- ↑ Oljaca, Ana; Vidakovic, Ivan; Leithner, Andreas; Bergovec, Marko (2018). "Current knowledge in orthopaedic surgery on recommending sport activities after total hip and knee replacement". Acta Orthopaedica Belgica 84 (4): 415–422. ISSN 0001-6462. PMID 30879445. https://pubmed.ncbi.nlm.nih.gov/30879445.
- ↑ Pfuntner A., Wier L.M., Stocks C. Most Frequent Procedures Performed in U.S. Hospitals, 2011. HCUP Statistical Brief #165. October 2013. Agency for Healthcare Research and Quality, Rockville, MD. [1].
- ↑ "Characteristics of Operating Room Procedures in U.S. Hospitals, 2011.". HCUP Statistical Brief #170 (Rockville, MD: Agency for Healthcare Research and Quality). February 2014. PMID 24716251. http://hcup-us.ahrq.gov/reports/statbriefs/sb170-Operating-Room-Procedures-United-States-2011.jsp.
- ↑ "Trends in Operating Room Procedures in U.S. Hospitals, 2001—2011.". HCUP Statistical Brief #171 (Rockville, MD: Agency for Healthcare Research and Quality). March 2014. PMID 24851286. http://hcup-us.ahrq.gov/reports/statbriefs/sb171-Operating-Room-Procedure-Trends.jsp.
- ↑ "Most Frequent Operating Room Procedures Performed in U.S. Hospitals, 2003-2012". HCUP Statistical Brief #186. Rockville, MD: Agency for Healthcare Research and Quality. December 2014. https://www.hcup-us.ahrq.gov/reports/statbriefs/sb186-Operating-Room-Procedures-United-States-2012.jsp.
- ↑ "Essential amino acid supplementation in patients following total knee arthroplasty". The Journal of Clinical Investigation 123 (11): 4654–66. November 2013. doi:10.1172/JCI70160. PMID 24135139.
- ↑ "The effect of total knee arthroplasty on patients' balance and incidence of falls: a systematic review". Knee Surgery, Sports Traumatology, Arthroscopy 25 (11): 3439–3451. November 2017. doi:10.1007/s00167-016-4355-z. PMID 27761627.
Further reading
- "A New Set of Knees Comes at a Price: A Whole Lot of Pain". The New York Times. 8 February 2005. https://www.nytimes.com/2005/02/08/health/08brod.html.
- "When It Comes to Severe Pain, Doctors Still Have Much to Learn". The New York Times. 15 February 2005. https://www.nytimes.com/2005/02/15/health/15brod.html.
- "A Year With My New Knees: Much Pain but Much Gain". The New York Times. 20 December 2005. https://www.nytimes.com/2005/12/20/health/20brod.html.
- "3 Years Later, Knees Made for Dancing"]. The New York Times. 3 June 2008. https://www.nytimes.com/2008/06/03/health/03brod.html.
- "Relief for Joints Besieged by Arthritis". The New York Times. 9 July 2012. http://well.blogs.nytimes.com/2012/07/09/relief-for-joints-besieged-by-arthritis/.
External links
 |