Medicine:Topical drug delivery system
Topical drug delivery system is a route of administration of drugs via the skin to provide topical therapeutic effects. As skin is one of the largest and most superficial organs in the human body, pharmacists utilise it to deliver various drugs. This system usually provides a local effect on certain positions of the body. In ancient times, people used herbs to put on wounds for relieving the inflammatory effect or as pain relievers. The use of topical drug delivery system is much broader now, from smoking cessation to beauty purposes. Nowadays, there are numerous dosage forms that can be used topically, including cream, ointment, lotion, patches, dusting powder and much more.[citation needed] There are many advantages for this drug delivery system - avoiding first pass metabolism which can increase its bioavailability, being convenient and easy to apply to a large area, being easy to terminate the medication and avoiding gastro-intestinal irritations. All these can increase the patient compliance. However, there are several disadvantages for this system - causing skin irritations and symptoms like rashes and itchiness may occur. Also, only small particles can pass through the skin, which limits the choice of drugs. Since skin is the main medium of topical drug delivery system, its conditions determine the rate of skin penetration leading to affecting the pharmacokinetics of the drug. The temperature, pH value and dryness of the skin need to be considered. There are some novel topical drugs in the market which can utilise the system as much as possible.
Topical Drug Delivery
This localized system provides topical therapeutic effects via skin, eyes, nose and vagina[1] to treat [diseases]. The most common usage is for local skin infection problems. Dermatological products have various formulations and range in consistency though the most popular dermal products are semisolid dosage forms[2] to provide topical treatment.
Factor affecting topical drug absorption
Topical drug absorption depends on two major factors - biological and physicochemical properties.
The first factor concerns body structure effects on the drugs. The degradation of drugs can be affected by the site of applications. Some studies discovered different Percutaneous absorption patterns. Apart from the place, age also affects the absorption as the skin structure changes with age. The lowered collagen and broadened blood capillary networks happen with ageing. These features alter the effectiveness of absorption of both hydrophilic and lipophilic substances into stratum corneum underneath the surface of skin.[citation needed] The skin surface integrity can also affect the permeability of drugs such as the density of hair follicles, sweat glands or disintegrated by inflammation or dehydration.
The other factor concerns metabolism of medications on skin. When the percutaneous drug is applied on skin, it will be gradually absorbed down the skin. Normally, when the drugs are absorbed, they will be metabolised by various enzymes in our body and the amount will be lower. The exact amount delivered to the target action site determines the potency and bioavailability of the drugs. If the concentration is too low, the therapeutic effect is impeded; if the concentration is too high, drug toxicity may happen to cause side effects or even do harm to our body. For the topical drug delivery way, degradation of drugs in skin is very low compared to liver. The metabolism of drugs is mainly by metabolic enzyme cytochrome P450, and this enzyme is not active in skin. The CYP450 actively metabolized drugs can then maintain high concentration when being applied on skin. Despite CYP450 enzyme action, the partition coefficient (K) determines the activity of topical drugs. The ability of drug particles to go through the skin layer also affects the absorption of drugs. For transdermal activity, medicines with higher K value are harder to get rid of the lipid layer of skin cells. The trapped molecules then cannot penetrate into the skin. This reduces the efficacy of the transdermal drugs. The drugs target cells underneath the skin or need to diffuse into blood capillary to exert their effect. Meanwhile, the size of particles affects this transdermal process. The smaller the drug molecules, the faster the rate of penetration. Polarity of the drugs can affect this diffusion rate too. If the drug shows lower degree of ionization, it is less polar. Therefore, it can have a faster absorption rate.
Topical Drug Classification System (TCS)
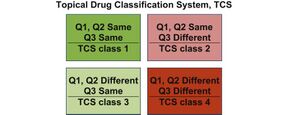
Topical drug classification system (TCS) is proposed by the FDA. It is designed from the Biopharmaceutics Classification System (BCS) for oral immediate release solid drug products which is very successful for decades. There are 3 aspects to assess and 4 classes in total. The 3 aspects include qualitative (Q1), quantitative (Q2) and similarity of in vitro release (IVR) rate (Q3).[3]
Advantages of topical drug delivery systems
In the early 1970s, the Alza Corporation, through their founder Alejandro Zaffaroni, filed the first US patents describing transdermal delivery systems for scopolamine, nitroglycerin and nicotine.[4] People found that applying medicines on the body surfaces is beneficial in many aspects. Skin medicines can give faster onset and local effect on our body as the surface cream can bypass first pass metabolism such as hepatic and intestinal metabolism. Apart from the absorption, dermal drugs effectively prevent oral delivery limitations such as nausea and vomiting and poor appliances due to unpalatable tastes of the drugs . Topical application is an easy way for patients to tackle skin infections in a painless and non-invasive way. From a patient perspective, applying drugs on skin also provides stable dosage in blood so as to give the optimal bioavailability and therapeutic effects. In case of overdose or unwanted side effects, patients can take off or wash out the medicines quickly to eliminate toxicity by simply removing the patch to stop the delivery of drugs.[citation needed]
Disadvantages of topical drug delivery systems
The site of putting the patches for topical drugs may get irritated and have rashes and feel itchy. Hence, some topical drugs including nicotine patches for smoking cessation are advised to change places for each application to avoid continuous irritation of the skin. Also, since the drug needs to penetrate the skin, some drugs may not be able to pass through the skin. Some drugs are then “wasted” and the bioavailability of the drug will decrease.
Challenges for designing topical dosage form
Skin penetration is the main challenge for any topical dosage form. The drug needs to penetrate the skin in order to get into the body to apply its function. The drug follows the Fick’s first law of diffusion.[5] One of the most common versions of Fick’s first law of diffusion is:
- [math]\displaystyle{ J=-D{dc \over dx} }[/math]
where
- J is the diffusion flux.
- D is the diffusion coefficient.
- dc/dx is the concentration gradient.
For D is described by the Stokes–Einstein equation. The equation is:
- [math]\displaystyle{ D=\frac{RT}{6\pi\eta rN_A} }[/math]
where
- R is the gas constant.
- T is the temperature.
- η is the viscosity.
- r is the radius of the solute.
- [math]\displaystyle{ N_A }[/math] is the Avogadro constant.
Assuming concentration gradient is constant for all newly applied topical drugs and the temperature is constant (normal body temperature: 37 °C), the viscosity and radius of the drug determine the flux of diffusion. The higher the viscosity or the larger the radius of the drug is, the lower the diffusion flux of the drug is.[5]
New developments
There are many factors for drug developers to consider in developing new topical formulations.
The first one is the effect of the vehicle. The medium to carry the topical drugs can affect the penetration of the drug active ingredient and efficacy. For example, this carrier can have a cooling, drying, emollient or protective action to suit the required conditions of the application site such as applying gel or lotion for hairy areas. Meanwhile, scientists need to match the type of preparation with the type of lesions. For example, they need to avoid oily ointments for acute weepy dermatitis. Chemists also need to consider the irritation or any sensitization potential to ensure that the topical application can be stable during storage and transport to maintain its efficacy.[4] Another potential material is nanofiber-based dispersion to improve the adhesion of active ingredients on the skin.[6]
In order to enhance drug penetration into the skin, scientists have several ways to achieve their purposes by using chemical, biochemical, physical and super saturation enhancement. Advanced Emulgel technology is a breakthrough of painkilling topical drugs.[citation needed] It helps the gel to enter deeply down the skin layer to strengthen delivery of diclofenac to the point of pain so as to achieve better therapeutic effects by modifying the above properties.[4]
See also
References
- ↑ Singh, D.; Mital, N.; Kaur, G. (2016). "Topical Drug Delivery Systems: A Patent Review". Expert Opinion on Therapeutic Patents 26 (2): 213–228. doi:10.1517/13543776.2016.1131267. PMID 26651499. https://www.tandfonline.com/doi/full/10.1517/13543776.2016.1131267. Retrieved 27 March 2021.
- ↑ Holmgaard, R.; Nielsen, J.B. (2009). "Dermal absorption of pesticides – evaluation of variability and prevention". Pesticides Research (124): 35–376. https://www2.mst.dk/udgiv/publications/2009/978-87-7052-980-8/pdf/978-87-7052-981-5.pdf.
- ↑ 3.0 3.1 Shah, Vinod P.; Yacobi, Avraham; Rădulescu, Flavian Ştefan; Miron, Dalia Simona; Lane, Majella E. (August 2015). "A science based approach to topical drug classification system (TCS)". International Journal of Pharmaceutics 491 (1–2): 21–25. doi:10.1016/j.ijpharm.2015.06.011. PMID 26070249. https://discovery.ucl.ac.uk/id/eprint/1470027/.
- ↑ 4.0 4.1 4.2 Pastore, M. N.; Kalia, Y. N.; Horstmann, M.; Roberts, M. S. (2015). "Transdermal patches: history, development and pharmacology". British Journal of Pharmacology 172 (9): 2179–2209. doi:10.1111/bph.13059. PMID 25560046.
- ↑ 5.0 5.1 Florence, A. T., & Attwood, D. (2016). Physicochemical principles of pharmacy in manufacture, formulation and clinical use. London: (PhP) Pharmaceutical Press.
- ↑ A.E. Benson, Heather; E. Grice, Jeffrey; Mohammed, Yousuf; Namjoshi, Sarika; S. Roberts, Michael (2019). "Topical and Transdermal Drug Delivery: From Simple Potions to Smart Technologies". Current Drug Delivery 16 (5): 440–460. doi:10.2174/1567201816666190201143457. PMID 30714524.




