Medicine:Bifascicular block
| Bifascicular block | |
|---|---|
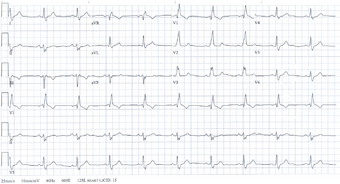 | |
| Bifascicular block on an electrocardiogram. |
Bifascicular block is characterized by right bundle branch block with left anterior fascicular block, left bundle branch block, or right bundle branch block with left posterior fascicular block on electrocardiography. Complete heart block could be the cause of syncope that is otherwise unexplained if bifascicular block is seen on electrocardiography.[1] It is estimated that less than 50% of patients with bifascicular block have high-degree atrioventricular block, although the exact incidence is unknown.[2]
The European Society of Cardiology (ESC) suggests using electrophysiology studies to look into it (EPS). When pharmacologic stress or incremental atrial pacing induces high-degree atrioventricular block, a permanent pacemaker (PPM) is recommended. If EPS is negative, long-term rhythm monitoring with an implantable loop recorder (ILR) is advised.[3]
Most commonly, it refers to a combination of right bundle branch block (RBBB) and either left anterior fascicular block (LAFB) or left posterior fascicular block (LPFB), with the former being more common.[4]
Signs and symptoms
Patients who suffer from bifascicular block are more likely to experience syncope and unexpected death.[5]
Diagnosis
Diagnostic criteria:[citation needed]
Clinically, bifascicular block presents with one of two ECG patterns:
Right bundle branch block (RBBB) with left anterior fascicular block (LAFB), manifested as left axis deviation (LAD).
RBBB and left posterior fascicular block (LPFB), manifested as right axis deviation (RAD) in the absence of other causes.
Treatment
In those with bifascicular block and no symptoms, little with respect to treatment is needed. In those with syncope, a pacemaker is recommended.[6]
See also
References
- ↑ Shabbir, Muhammad Asim; Shaukat, Muhammad Hamza Saad; Ehtesham, Moiz; Murawski, Shannon; Singh, Sukhraj; Alimohammad, Rizwan (2022). "Bifascicular block in unexplained syncope is underrecognized and under-evaluated: A single-center audit of ESC guidelines adherence". PLOS ONE (PLOS) 17 (2): e0263727. doi:10.1371/journal.pone.0263727. PMID 35226666. Bibcode: 2022PLoSO..1763727S.
- ↑ M, Brignole; C, Menozzi; A, Moya; R, Garcia-Civera; L, Mont; M, Alvarez; F, Errazquin; J, Beiras et al. (2001). "Mechanism of syncope in patients with bundle branch block and negative electrophysiological test". Circulation 104 (17): 2045–2050. doi:10.1161/hc4201.097837. ISSN 1524-4539. PMID 11673344. https://pubmed.ncbi.nlm.nih.gov/11673344/. Retrieved December 30, 2023.
- ↑ M, Brignole; A, Moya; FJ, de Lange; JC, Deharo; PM, Elliott; A, Fanciulli; A, Fedorowski; R, Furlan et al. (August 28, 2018). "2018 ESC Guidelines for the diagnosis and management of syncope". European Heart Journal (Eur Heart J) 39 (21): 1883–1948. doi:10.1093/eurheartj/ehy037. ISSN 1522-9645. PMID 29562304. https://pubmed.ncbi.nlm.nih.gov/29562304/. Retrieved December 30, 2023.
- ↑ "Lesson VI — ECG Conduction Abnormalities". http://library.med.utah.edu/kw/ecg/ecg_outline/Lesson6/index.html#bifasc.
- ↑ Ohara, Kuniji; Yamada, Harumoto; Jochheim, David; Mehilli, Julinda; Chandrashekhar, Y.; Narula, Jagat; Lopes, Renato D.; Fanaroff, Alexander C. et al. (October 1, 1983). "Electrophysiologic evaluation of syncope in patients with bifascicular block". American Heart Journal (Mosby) 106 (4): 693–697. doi:10.1016/0002-8703(83)90089-3. ISSN 0002-8703. PMID 6613815. https://www.sciencedirect.com/science/article/abs/pii/0002870383900893. Retrieved December 30, 2023.
- ↑ Epstein, Andrew E.; DiMarco, John P.; Ellenbogen, Kenneth A.; Estes, N.A. Mark; Freedman, Roger A.; Gettes, Leonard S.; Gillinov, A. Marc; Gregoratos, Gabriel et al. (2008-05-27). "ACC/AHA/HRS 2008 Guidelines for Device-Based Therapy of Cardiac Rhythm Abnormalities". Circulation 117 (21): e350-408. doi:10.1161/circualtionaha.108.189742. ISSN 0009-7322. PMID 18483207.
Further reading
- Steinberg, Jonathan S.; Pokushalov, Evgeny; Zeidan-Shwiri, Tawfiq; Crystal, Eugene; Nakamura, Kohki; Naito, Shigeto; Ávila, Pablo; Arenal, Ángel et al. (August 1, 1973). "Bifascicular block: A clinical and electrophysiologic study". American Heart Journal (Mosby) 86 (2): 173–181. doi:10.1016/0002-8703(73)90241-X. ISSN 0002-8703. PMID 4719938. https://www.sciencedirect.com/science/article/abs/pii/000287037390241X. Retrieved December 30, 2023.
- Kiehl, Erich L.; Cantillon, Daniel J.; Heidecker, Bettina; Jr, Leslie T. Cooper; Singh, Gagan D.; Rogers, Jason H.; Wilson, Ryan E.; Ziada, Khaled M. et al. (January 1, 2017). "Bradyarrhythmias—Conduction System Abnormalities". Arrhythmia Essentials. Elsevier. pp. 28–86. doi:10.1016/B978-0-323-39968-5.00002-0. ISBN 9780323399685. https://www.sciencedirect.com/science/article/abs/pii/B9780323399685000020. Retrieved December 30, 2023.
External links
| Classification | |
|---|---|
| External resources |
|
 |

