Biology:Pathophysiology of multiple sclerosis
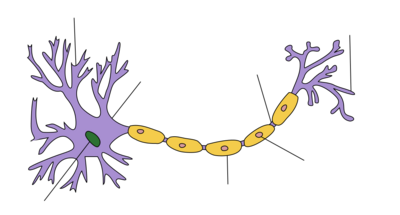
| Myelin sheath of a healthy neuron |
|---|
Multiple sclerosis is an inflammatory demyelinating disease of the CNS in which activated immune cells invade the central nervous system and cause inflammation, neurodegeneration, and tissue damage. The underlying cause is currently unknown. Current research in neuropathology, neuroimmunology, neurobiology, and neuroimaging, together with clinical neurology, provide support for the notion that MS is not a single disease but rather a spectrum.[1]
There are three clinical phenotypes: relapsing-remitting MS (RRMS), characterized by periods of neurological worsening following by remissions; secondary-progressive MS (SPMS), in which there is gradual progression of neurological dysfunction with fewer or no relapses; and primary-progressive MS (MS), in which neurological deterioration is observed from onset.
Pathophysiology is a convergence of pathology with physiology. Pathology is the medical discipline that describes conditions typically observed during a disease state; whereas physiology is the biological discipline that describes processes or mechanisms operating within an organism. Referring to MS, the physiology refers to the different processes that lead to the development of the lesions and the pathology refers to the condition associated with the lesions.
Pathology
Multiple sclerosis can be pathologically defined as the presence of distributed glial scars (or sclerosis) in the central nervous system disseminated in time (DIT) and space (DIS).[2] The gold standard for MS diagnosis is pathological correlation, though given its limited availability, other diagnosis methods are normally used.[3] The scleroses that define the disease are the remainders of previous demyelinating lesions in the CNS white matter of a patient (encephalomyelitis) showing special characteristics, such as confluent instead of perivenous demyelination.[4]
There are three phases for how an unknown underlying condition may cause damage in MS:
- An unknown soluble factor (produced by CD8+ T-cells or CD20+ B-cells), creates a toxic environment that activates microglia.[5][6]
- MRI-abnormal areas with hidden damage appear in the brain and spine (NAWM, NAGM, DAWM). Some clusters of activated microglia, axonal transection and myelin degeneration are present.[7][8][9]
- Leaks in the blood–brain barrier appear and immune cells infiltrate, causing demyelination.[10] and axon destruction.[11]
Multiple sclerosis differs from other idiopathic inflammatory demyelinating diseases in its confluent subpial cortical lesions. These types of lesions are the most specific finding for MS, being exclusively present in MS patients, though currently they can only be detected at autopsy.[12]
Most MS findings take place inside the white matter, and lesions appear mainly in a periventricular distribution (clustered around the ventricles of the brain). Apart from white matter demyelination, the cortex and deep gray matter (GM) nuclei can be affected, together with diffuse injury of the NAWM.[13] GM atrophy is independent of classical MS lesions and is associated with physical disability, fatigue, and cognitive impairment in MS[14]
At least five characteristics are present in CNS tissues of MS patients: Inflammation beyond classical white matter lesions, intrathecal Ig production with oligoclonal bands, an environment fostering immune cell persistence, and a disruption of the blood–brain barrier outside of active lesions.[15] The scars that give the name to the condition are produced by astrocytes healing old lesions.[16] MS is active even during remission periods.[17]
Meningeal tertiary lymphoid-like structures
Follicle-like aggregates in the meninges are formed only in secondary progressive MS.[18] and correlate with the degree of subpial cortical demyelination and brain atrophy, suggesting that they might contribute to cortical pathology in SPMS[18]
These ectopic lymphoid follicles are composed mainly of EBV infected B-cells.[19]
Demyelination patterns
Four different damage patterns have been identified in patient's brain tissues. The original report[citation needed] suggests that there may be several types of MS with different immune causes, and that MS may be a family of several diseases. Though originally a biopsy was required to classify the lesions of a patient, since 2012 it is possible to classify them by a blood test[20] looking for antibodies against 7 lipids, three of which are cholesterol derivatives[21] Cholesterol crystals are believed to both impair myelin repair and aggravate inflammation.[22][23]
It is believed that they may correlate with differences in disease type and prognosis, and perhaps with different responses to treatment. In any case, understanding lesion patterns can provide information about differences in disease between individuals and enable doctors to make more effective treatment decisions.[citation needed]
According to one of the researchers involved in the original research, "Two patterns (I and II) showed close similarities to T-cell-mediated or T-cell plus antibody-mediated autoimmune encephalomyelitis, respectively. The other patterns (III and IV) were highly suggestive of a primary oligodendrocyte dystrophy, reminiscent of virus- or toxin-induced demyelination rather than autoimmunity."
The four identified patterns are:[24]
- Pattern I
- The scar presents T-cells and macrophages around blood vessels, with preservation of oligodendrocytes, but no signs of complement system activation.[25]
- Pattern II
- The scar presents T-cells and macrophages around blood vessels, with preservation of oligodendrocytes, as before, but also signs of complement system activation can be found.[26] This pattern has been considered similar to damage seen in NMO, though AQP4 damage does not appear in pattern II MS lesions[27] Nevertheless, pattern II has been reported to respond to plasmapheresis,[28] which points to something pathogenic into the blood serum.
- The complement system infiltration in these cases convert this pattern into a candidate for research into autoimmune connections like anti-Kir4.1,[29] anti-Anoctamin-2[30] or anti-MOG mediated MS[31] About the last possibility, research has found antiMOG antibodies in some pattern-II MS patients.[32]
- Pattern II pathogenic T cells has been shown to be different from others[33][34] The functional characterization shows that T cells releasing Th2 cytokines and helping B cells dominate the T-cell infiltrate in pattern II brain lesions.[33]
- Pattern III
- The scars are diffuse with inflammation, distal oligodendrogliopathy, microglial activation and loss of myelin-associated glycoprotein (MAG). It is considered atypical and an overlap between MS and Balo concentric sclerosis. The scars do not surround the blood vessels, and a rim of preserved myelin appears around the vessels. There is evidence of partial remyelinization and oligodendrocyte apoptosis. At first, some researchers thought it was an early stage of the evolution of the other patterns.[35][36] Recently, it is thought that it represents ischaemia-like injury with absence of oligoclonal bands in the CSF, related to the pathogenesis of Balo concentric sclerosis.[37]
- Pattern IV
- The scar presents sharp borders and oligodendrocyte degeneration, with a rim of normal-appearing white matter. There is a lack of oligodendrocytes in the center of the scar. There is no complement activation or MAG loss.
These differences are noticeable only in early lesions[38] and the heterogeneity was controversial for some time because some research groups thought that these four patterns could be a consequence of the age of the lesions.[39] Nevertheless, after some debate among research groups, the four patterns model is accepted and the exceptional case found by Prineas has been classified as NMO[40][41]
For some investigation teams this means that MS is an immunopathogenetically heterogeneous disease. The latter hypothesis is further corroborated by a recent study that demonstrated significant differences in routine cerebrospinal fluid findings between patients with pattern I lesions and patients with non-pattern I lesions, including a lack of CSF-restricted oligoclonal bands, in most pattern II and III patients.[42] Finally, some previously diagnosed with pattern II MS were later found to have in fact MOG-IgG-related encephalomyelitis, suggesting that both the current clinicoradiological diagnostic criteria for MS and the histopathological criteria for MS may be insufficiently specific. This was already indicated by previous studies that found a relatively high rate of false diagnoses of MS among patients with AQP4-IgG-positive neuromyelitis optica spectrum disorders or MOG encephalomyelitis. Currently antibodies to lipids and peptides in sera, detected by microarrays, can be used as markers of the pathological subtype given by brain biopsy.[43]
Another development in this area is the finding that some lesions present mitochondrial defects that could distinguish types of lesions.[44]
Physiology of MS
In multiple sclerosis, inflammation, demyelination, and neurodegeneration are observed together. Some clinical trials have shown that the inflammation produces both the relapses and the demyelination, and that neurodegeneration (axonal transection) is independent from inflammation, produces the accumulative disability, and advances even when inflammation and demyelination are delayed.[45] It seems that neurodegeneration is produced by damaged mitochondria, which in turn comes from activated microglia.[46]
Currently it is unknown what the primary cause of MS is; if MS is a heterogeneous disease, the lesion development process would not be unique. In particular, some PPMS patients having a special clinical course named rapidly progressive multiple sclerosis could have a special genetic cause[47] and a different development process.
Several types of damage appear in the brain: normal appearing white matter (NAWM) and characteristic lesions. Changes in NAWM include axonal injury without demyelination, low-grade inflammation, and microglial and astrocytic activation[48]
MS lesion development
MS lesions develop inside NAWM areas. Their shape is influenced by their activity[49]
The most accepted sequence of events is first NAWM appearance, then the so-called pre-active lesions, with activated microglia, and finally the BBB (blood-brain barrier) breakdown, which enables the entry of T-cells to the CNS. This marks the beginning of an autoimmune attack which destroys myelin in active lesions.[50] When the attack is resolved, a characteristic glial scar is formed by astrocytes.
Current models can be divided into two categories: inside-out and outside-in. In the former, it is hypothesized that a problem in CNS cells produces an immune response that destroys myelin and subsequently breaks the BBB. In latter, an external factor produces BBB leaks, enters the CNS, and destroys myelin and axons.[51] Whatever the underlying condition for MS is, it appears that damage is triggered by an unknown soluble factor in the CSF, potentially produced in meningeal areas; this factor can diffuse into the cortical parenchyma and destroy myelin either directly or indirectly through microglia activation.[12]
The evolution of a preactive lesion is related to microglia reactivity. Increased expression of pro-inflammatory cell surface markers have been observed in NAWM and "initial" lesions, corresponding to a so-called loss of homeostatic microglial equilibrium.[52]
Some authors report active lesion formation before BBB breakdown;[53] others point to adipsin as a factor of the breakdown.[54]
MS lesions are driven mainly by T-cells. It has been found recently that B-cells are also involved.[55]
Blood–brain barrier disruption
The blood–brain barrier (BBB) is a protective barrier that denies the entrance of foreign material into the nervous system. BBB disruption is the moment in which penetration of the barrier by lymphocytes occur and has been considered one of the early problems in MS lesions.[56]
The BBB is composed of endothelial cells which line the blood vessel walls of the central nervous system. Compared to normal endothelial cells, the cells lining the BBB are connected by occludin and claudin which form tight junctions in order to create a barrier to keep out larger molecules such as proteins. In order to pass through, molecules must be taken in by transport proteins or an alteration in the BBB permeability must occur, such as interactions with associated adaptor proteins like ZO-1, ZO-2 and ZO-3.[57]
The BBB is compromised due to active recruitment of lymphocytes and monocytes and their migration across the barrier. Release of chemokines allow for the activation of adhesion molecules on the lymphocytes and monocytes, resulting in an interaction with the endothelial cells of the BBB which then activate the expression of matrix metalloproteinases to degrade the barrier.[57] This results in disruption of the BBB, causing an increase in barrier permeability due to the degradation of tight junctions which maintain barrier integrity. Inducing the formation of tight junctions can restore BBB integrity and reduces its permeability, which can be used to reduce the damage caused by lymphocyte and monocyte migration across the barrier as restored integrity would restrict their movement.[58]
After barrier breakdown symptoms may appear, such as swelling. Activation of macrophages and lymphocytes and their migration across the barrier may result in direct attacks on myelin sheaths within the central nervous system, leading to the characteristic demyelination event observed in MS.[59] After demyelination has occurred, the degraded myelin sheath components, such as myelin basic proteins and Myelin oligodendrocyte glycoproteins, are then used as identifying factors to facilitate further immune activity upon myelin sheaths. Further activation of cytokines is also induced by macrophage and lymphocyte activity, promoting inflammatory activity as well continued activation of proteins such as matrix metalloproteinases, which have detrimental effect on BBB integrity.[60]
Recently it has been found that BBB damage happens even in non-enhancing lesions.[61] MS has an important vascular component.[62]
Postmortem BBB study
Postmortem studies of the BBB, especially the vascular endothelium, show immunological abnormalities. Microvessels in periplaque areas coexpressed HLA-DR and VCAM-1, some others HLA-DR and urokinase plasminogen activator receptor, and others HLA-DR and ICAM-1.[63]
In vivo BBB
The damaged white matter is known as "Normal-appearing white matter" (NAWM) and is where lesions appear.[10] These lesions form in NAWM before blood–brain barrier breakdown.[64]
BBB can be broken centripetally (the most normal) or centrifugally.[65] Several possible biochemical disrupters were proposed. Some hypotheses about how the BBB is compromised revolve around the presence of compounds in the blood that could interact with vessels only in the NAWM areas. The permeability of two cytokines, Interleukin 15 and LPS, may be involved in BBB breakdown.[66] Breakdown is responsible for monocyte infiltration and inflammation in the brain.[67] Monocyte migration and LFA-1-mediated attachment to brain microvascular endothelia is regulated by SDF-1alpha through Lyn kinase.[68]
Using iron nanoparticles, involvement of macrophages in BBB breakdown can be detected.[69] A special role is played by Matrix metalloproteinases. These increase BBB T-cell permeability, specially in the case of MMP-9[60] and are supposedly related to the mechanism of action of interferons.[70]
Whether BBB dysfunction is the cause or the consequence of MS[71] is disputed, because activated T-Cells can cross a healthy BBB when they express adhesion proteins.[72] Apart from that, activated T-Cells can cross a healthy BBB when they express adhesion proteins.[72] (Adhesion molecules could also play a role in inflammation[73]) In particular, one of these adhesion proteins involved is ALCAM (Activated Leukocyte Cell Adhesion Molecule, also called CD166), and is under study as therapeutic target.[74] Another protein involved is CXCL12,[75] which is found also in brain biopsies of inflammatory elements,[76] and which could be related to the behavior of CXCL13 under methylprednisolone therapy.[77] Some molecular biochemical models for relapses have been proposed.[78]
Normally, gadolinium enhancement is used to show BBB disruption on MRIs.[79] Abnormal tight junctions are present in both SPMS and PPMS. They appear in active white matter lesions and in gray matter in SPMS. They persist in inactive lesions, particularly in PPMS.[80]
A uric acid deficiency was implicated in this process. Uric acid added in physiological concentrations (i.e. achieving normal concentrations) is therapeutic in MS by preventing BBB breakdown through inactivation of peroxynitrite.[81] The low level of uric acid found in people with MS is manifestedly causative rather than a tissue damage consequence in the white matter lesions,[82] but not in the grey matter lesions.[83] Uric acid levels are lower during relapses.[84]
Proposed causes
It is not known what causes MS. Several problems appear together with the white matter lesions, like cortical lesions and normal-appearing tissues. Several theories have been proposed to explain it.
Some areas that appear normal under normal MRI look abnormal under special MRI, like magnetisation transfer MTR-MRI. These are called Normal Appearing White Matter (NAWM) and Normal Appearing Grey Matter (NAGM). The cause why the normal appearing areas appear in the brain is unknown, but seems clear that they appear mainly in the ventricles and that they predict the course of the disease.[85]
Given that MS lesions begin inside the NAWM areas, these areas are expected to be produced by the same underlying condition that produces the lesions, and therefore the ultimate MS underlying condition, whatever it is.[86] Historically, several theories about how these areas appear have been presented:
Autoimmune theories
The search for an auto-antigen has taken a long time, but at least there is one reported. It is the enzyme GDP-L-fucose synthase.[87][88]
This theory in part could also explain why some patients report amelioration under dietary treatment.
HERVs
Human endogenous retroviruses (HERVs) have been reported in MS for several years. In fact, one of the families, Human Endogenous Retrovirus-W was first discovered while studying MS patients.
Recent research as of 2019 point to one of the HERV-W viruses (pHEV-W), and specifically one of the proteins of the viral capsid that has been found to activate microglia in vitro. Activated microglia in turn produces demyelination.[89] Some interactions between the Epstein-Barr virus and the HERVs could be the trigger of the MS microglia reactions.[90] Supporting this study, a monoclonal antibody against the viral capside (Temelimab) has shown good results in trials in phase IIb.[91]
- Venous pathology has been associated with MS for more than a century. Pathologist Georg Eduard Rindfleisch noted in 1863 that the inflammation-associated lesions were distributed around veins.[92] Some other authors like Tracy Putnam[93] pointed to venous obstructions.
- Mechanical flow: Later the focus moved to softer hemodynamic abnormalities, which were showing precede changes in sub-cortical gray matter[86] and in substantia nigra.[94] However, such reports of a "hemodynamic cause of MS" are not universal, and possibly not even common. At this time the evidence is largely anecdotal and some MS patients have no blood flow issues. Possibly vascular problems may be an aggravating factor, like many others in MS. Indeed, the research, by demonstrating patients with no hemodynamic problems actually prove that this is not the only cause of MS.
- Endothelium: Other theories point to a possible primary endothelial dysfunction.[95] The importance of vascular misbehaviour in MS pathogenesis has also been independently confirmed by seven-tesla MRI.[96] It is reported that a number of studies have provided evidence of vascular occlusion in MS, which suggest the possibility of a primary vascular injury in MS lesions or at least that they are occasionally correlated.[97]
- Venous insufficiency: Some morphologically special medullar lesions (wedge-shaped) have also been linked to venous insufficiency.[98]
- BBB infection: It has also been pointed out that some infectious agents with positive correlation to MS, specially Chlamydia pneumoniae, can cause problems in veins and arteries walls[99]
- CCSVI: The term "chronic cerebrospinal venous insufficiency" was coined in 2008 by Paolo Zamboni, who described it in patients with multiple sclerosis. Instead of intracranial venous problems he described extracranial blockages, and he stated that the location of those obstructions seemed to influence the clinical course of the disease.[100] According to Zamboni, CCSVI had a high sensitivity and specificity differentiating healthy individuals from those with multiple sclerosis.[101] Zamboni's results were criticized as some of his studies were not blinded and they need to be verified by further studies.[100][101] (As of 2010) the theory is considered at least defensible[102]
- A more detailed evidence of a correlation between the place and type of venous malformations imaged and the reported symptoms of multiple sclerosis in the same patients was published in 2010.[103]
- Haemodynamic problems have been found in the blood flow of MS patients using Doppler,[104] initially using transcranial color-coded duplex sonography (TCCS), pointing to a relationship with a vascular disease called chronic cerebro-spinal venous insufficiency (CCSVI).[105][106] In 2010 there were conflicting results when evaluating the relationship between MS and CCSVI.[107][108][109][110] but is important to note that positives have appeared among the blinded studies.
- CSF flow: Other theories focus in the possible role of cerebrospinal fluid flow impairment.[111] This theory could be partially consistent with the previous one.[112] Currently a small trial with 8 participants has been performed[113]
CSF composition: Kir4.1 and Anoctamin-2
Whatever the underlying primary condition is, it is expected to be a soluble factor in the CSF,[12] maybe an unknown cytokine or ceramide, or a combination of them. Also B-cells and microglia could be involved.[114][115] In particular, it is known that B-cells of MS patients secrete an unknown toxin against oligodendrocytes[116]
It has been reported several times that CSF of some MS patients can damage myelin in culture[117][118][119][120][121] and mice[122][123] and ceramides have been recently brought into the stage.[124] Whatever the problem is, it produces apoptosis of neurons respecting astrocytes[125]
In 2012 it was reported that a subset of MS patients have a seropositive anti-Kir4.1 status,[126] which can represent up to a 47% of the MS cases, and the study has been reproduced by at least two other groups.[127][128]
In 2016 a similar association was reported for anti-Anoctamin-2[129]
If the existence of any of these subsets of MS is confirmed, the situation would be similar to what happened for Devic Disease and Aquaporin-4[citation needed]. MS could be considered a heterogeneous condition or a new medical entity will be defined for these cases.
Primary neuro-degeneration theories
Some authors propose a primary neurodegenerative factor. Maybe the strongest argument supporting this theory comes from the comparison with NMO. Though autoimmune demyelination is strong, axons are preserved, showing that the standard model of a primary demyelination cannot be hold.[130] The theory of the trans-synaptic degeneration, is compatible with other models based in the CSF biochemistry.[131]
Others propose an oligodendrocyte stress as primary dysfunction, which activates microglia creating the NAWM areas[132] and others propose a yet-unknown intrinsic CNS trigger induces the microglial activation and clustering, which they point out could be again axonal injury or oligodendrocyte stress.[133]
Finally, other authors point to a cortical pathology which starts in the brain external layer (pial surface) and progresses extending into the brain inner layers[134]
Genetic causes
If as expected MS is an heterogeneous disease and the lesion development process would not be unique. In particular, some PPMS patients have been found to have a special genetic variant named rapidly progressive multiple sclerosis[47] which would behave differently from what here is explained.
It is due to a mutation inside the gene NR1H3, an arginine to glutamine mutation in the position p.Arg415Gln, in an area that codifies the protein LXRA.
Biomarkers
- Main:Multiple sclerosis biomarkers
Several biomarkers for diagnosis, disease evolution and response to medication (current or expected) are under research. While most of them are still under research, there are some of them already well stablished:
- oligoclonal bands: They present proteins that are in the CNS or in blood. Those that are in CNS but not in blood suggest a diagnosis of MS.
- MRZ-Reaction: A polyspecific antiviral immune response against the viruses of measles, rubella and zoster found in 1992.[135] In some reports the MRZR showed a lower sensitivity than OCB (70% vs. 100%), but a higher specificity (69% vs. 92%) for MS.[135]
- free light chains (FLC). Several authors have reported that they are comparable or even better than oligoclonal bands.[136]
See also
- Multiple sclerosis borderline
References
- ↑ Golan, Daniel; Staun-Ram, Elsebeth; Miller, Ariel (2016). "Shifting paradigms in multiple sclerosis". Current Opinion in Neurology 29 (3): 354–361. doi:10.1097/WCO.0000000000000324. PMID 27070218.
- ↑ "Pathology and definition of multiple sclerosis". Rev Prat. 56 (12): 1293–8. Jun 2006. PMID 16948216.
- ↑ "Imaging in multiple sclerosis: A new spin on lesions". J. Med. Imaging Radiat. Oncol. 60 (5): 577–586. 27 July 2016. doi:10.1111/1754-9485.12498. PMID 27464473.
- ↑ "Perivenous demyelination: association with clinically defined acute disseminated encephalomyelitis and comparison with pathologically confirmed multiple sclerosis". Brain 133 (2): 333–348. 2010. doi:10.1093/brain/awp321. PMID 20129932.
- ↑ Lassman H (Mar 2019). "The changing concepts in the neuropathology of acquired demyelinating central nervous system disorders". Curr Opin Neurol 32 (3): 313–319. doi:10.1097/WCO.0000000000000685. PMID 30893100.
- ↑ Lassman H (2019). "Pathogenic Mechanisms Associated With Different Clinical Courses of Multiple Sclerosis". Front Immunol 9: 3116. doi:10.3389/fimmu.2018.03116. PMID 30687321.
- ↑ "Preactive lesions in multiple sclerosis.". Curr Opin Neurol 22 (3): 207–13. 2009. doi:10.1097/WCO.0b013e32832b4c76. PMID 19417567.
- ↑ "Alpha-B-Crystallin Induces an Immune-Regulatory and Antiviral Microglial Response in Preactive Multiple Sclerosis Lesions". J Neuropathol Exp Neurol 72 (10): 970–9. 2013. doi:10.1097/NEN.0b013e3182a776bf. PMID 24042199.
- ↑ Ontaneda (Nov 2014). "Identifying the Start of Multiple Sclerosis Injury: A Serial DTI Study". J Neuroimaging 24 (6): 569–76. doi:10.1111/jon.12082. PMID 25370339.
- ↑ 10.0 10.1 "A serial study of new MS lesions and the white matter from which they arise". Neurology 51 (6): 1689–97. December 1998. doi:10.1212/wnl.51.6.1689. PMID 9855524. http://www.neurology.org/cgi/content/abstract/51/6/1689. Retrieved 2008-09-28.
- ↑ "Clinico-pathological evidence that axonal loss underlies disability in progressive multiple sclerosis". Mult Scler 16 (4): 406–411. April 2010. doi:10.1177/1352458510364992. PMID 20215480.
- ↑ 12.0 12.1 12.2 Lassmann Hans (2014). "Multiple sclerosis: Lessons from molecular neuropathology". Experimental Neurology 262: 2–7. doi:10.1016/j.expneurol.2013.12.003. PMID 24342027.
- ↑ "The immunopathology of multiple sclerosis: an overview". Brain Pathol. 17 (2): 210–8. April 2007. doi:10.1111/j.1750-3639.2007.00064.x. PMID 17388952.
- ↑ "Gray matter involvement in multiple sclerosis". Neurology 68 (9): 634–42. February 2007. doi:10.1212/01.wnl.0000250267.85698.7a. PMID 17325269.
- ↑ "Compartmentalization of inflammation in the CNS: A major mechanism driving progressive multiple sclerosis". J Neurol Sci 274 (1–2): 42–4. November 2008. doi:10.1016/j.jns.2008.06.032. PMID 18715571.
- ↑ "The astrocyte in multiple sclerosis revisited". Glia 61 (4): 453–465. 2013. doi:10.1002/glia.22443. PMID 23322421.
- ↑ "MR Spectroscopy Indicates Diffuse Multiple Sclerosis Activity During Remission". J. Neurol. Neurosurg. Psychiatry 80 (12): 1330–6. June 2009. doi:10.1136/jnnp.2009.176263. PMID 19546105.
- ↑ 18.0 18.1 Shinji Oki (March 2018). "Novel mechanisms of chronic inflammation in secondary progressive multiple sclerosis". Neuroimmunology 9 (S1): 13–19. doi:10.1111/cen3.12437.
- ↑ "Dysregulated Epstein-Barr virus infection in the multiple sclerosis brain". Journal of Experimental Medicine 204 (12): 2899–2912. Nov 2007. doi:10.1084/jem.20071030. PMID 17984305.
- ↑ F. Quintana et al., Specific Serum Antibody Patterns Detected with Antigen Arrays Are Associated to the Development of MS in Pediatric Patients, Neurology, 2012. Freely available at [1]
- ↑ Harnessing the clinical value of biomarkers in MS, International Journal of MS care, June 2012 [2]
- ↑ "Cholesterol crystals impede nerve repair". Science 359 (6376): 635–636. 2018. doi:10.1126/science.aar7369. PMID 29439228. Bibcode: 2018Sci...359..635C.
- ↑ "Defective cholesterol clearance limits remyelination in the aged central nervous system". Science 359 (6376): 684–688. 2018. doi:10.1126/science.aan4183. PMID 29301957. Bibcode: 2018Sci...359..684C.
- ↑ "Distinct patterns of multiple sclerosis pathology indicates heterogeneity on pathogenesis". Brain Pathol 6 (3): 259–74. Jul 1996. doi:10.1111/j.1750-3639.1996.tb00854.x. PMID 8864283.
- ↑ Holmes, Nick (15 November 2001). "Part 1B Pathology: Lecture 11 - The Complement System". http://immserv1.path.cam.ac.uk/~immuno/part1/lec10/lec10_97.html.
- ↑ "A quantitative analysis of oligodendrocytes in multiple sclerosis lesions - A study of 113 cases". Brain 122 (12): 2279–2295. December 1999. doi:10.1093/brain/122.12.2279. PMID 10581222.
- ↑ "Humoral pattern II multiple sclerosis pathology not associated with neuromyelitis Optica IgG". Arch Neurol 66 (10): 1298–9. October 2009. doi:10.1001/archneurol.2009.199. PMID 19822791.
- ↑ "Some MS patients have "Dramatic" responses to Plasma Exchange". Neurology Reviews 8 (3). March 2000. http://www.neurologyreviews.com/mar00/nr_mar00_MSpatients.html. Retrieved 2006-05-05.
- ↑ Srivastava, Rajneesh; Aslam, Muhammad; Kalluri, Sudhakar Reddy; Schirmer, Lucas; Buck, Dorothea; Tackenberg, Björn; Rothhammer, Veit; Chan, Andrew et al. (2012). "Potassium Channel KIR4.1 as an Immune Target in Multiple Sclerosis". New England Journal of Medicine 367 (2): 115–23. doi:10.1056/NEJMoa1110740. PMID 22784115.
- ↑ Ayoglu, Burcu; Mitsios, Nicholas; Kockum, Ingrid; Khademi, Mohsen; Zandian, Arash; Sjöberg, Ronald; Forsström, Björn; Bredenberg, Johan et al. (2016). "Anoctamin 2 identified as an autoimmune target in multiple sclerosis". Proceedings of the National Academy of Sciences 113 (8): 2188–2193. doi:10.1073/pnas.1518553113. PMID 26862169. Bibcode: 2016PNAS..113.2188A.
- ↑ Spadaro Melania (2015). "Histopathology and clinical course of MOG-antibody-associated encephalomyelitis". Annals of Clinical and Translational Neurology 2 (3): 295–301. doi:10.1002/acn3.164. PMID 25815356.
- ↑ "Screening for MOG-IgG and 27 other anti-glial and anti-neuronal autoantibodies in 'pattern II multiple sclerosis' and brain biopsy findings in a MOG-IgG-positive case.". Mult Scler 22 (12): 1541–1549. 11 Feb 2016. doi:10.1177/1352458515622986. PMID 26869529.
- ↑ 33.0 33.1 Planas Raquel (2015). "Central role of Th2/Tc2 lymphocytes in pattern II multiple sclerosis lesions". Annals of Clinical and Translational Neurology 2 (9): 875–893. doi:10.1002/acn3.218. PMID 26401510.
- ↑ "Sequencing the immunopathologic heterogeneity in multiple sclerosis". Annals of Clinical and Translational Neurology 2 (9): 873–874. 2015. doi:10.1002/acn3.230. PMID 26401509.
- ↑ Barnett, MH; Prineas, JW (April 2004). "Relapsing and remitting multiple sclerosis: pathology of the newly forming lesion". Annals of Neurology 55 (4): 458–68. doi:10.1002/ana.20016. PMID 15048884. http://www.direct-ms.org/pdf/ImmunologyMS/Prineas%20new%20lesion.pdf. Retrieved 2009-10-28.
- ↑ Marik, C.; Felts, P. A.; Bauer, J.; Lassmann, H.; Smith, K. J. (2007). "Lesion genesis in a subset of patients with multiple sclerosis: A role for innate immunity?". Brain 130 (11): 2800–2815. doi:10.1093/brain/awm236. PMID 17956913.
- ↑ Hardy TA, Tobin WO, Lucchinetti CF (2016). "Exploring the overlap between multiple sclerosis, tumefactive demyelination and Baló's concentric sclerosis". Multiple Sclerosis Journal 22 (8): 986–992. doi:10.1177/1352458516641776. PMID 27037180.
- ↑ "Homogeneity of active demyelinating lesions in established multiple sclerosis". Annals of Neurology 63 (1): 16–25. 2008. doi:10.1002/ana.21311. PMID 18232012.
- ↑ Michael H. Barnett; John W. Prineas (2004). "Relapsing and Remitting Multiple Sclerosis: Pathology of the Newly Forming Lesion". Annals of Neurology 55 (1): 458–468. doi:10.1002/ana.20016. PMID 15048884. http://www.cpnhelp.org/files/Ref1_Annals04.pdf.
- ↑ "Neuromyelitis optica lesions may inform multiple sclerosis heterogeneity debate". Ann Neurol 72 (3): 385–94. Sep 2012. doi:10.1002/ana.23621. PMID 23034911.
- ↑ "Pathophysiological processes in multiple sclerosis: focus on nuclear factor erythroid-2-related factor 2 and emerging pathways". Clin Pharmacol 6: 35–42. Feb 2014. doi:10.2147/CPAA.S35033. PMID 24591852.
- ↑ "Pattern II and pattern III MS are entities distinct from pattern I MS: evidence from cerebrospinal fluid analysis". J Neuroinflammation 14 (1): 171. 29 Aug 2017. doi:10.1186/s12974-017-0929-z. PMID 28851393.
- ↑ "Antigen microarrays identify unique serum autoantibody signatures in clinical and pathologic subtypes of multiple sclerosis". Proc Natl Acad Sci USA 105 (48): 18889–94. December 2008. doi:10.1073/pnas.0806310105. PMID 19028871. Bibcode: 2008PNAS..10518889Q.
- ↑ "Mitochondrial defects in acute multiple sclerosis lesions". Brain 131 (Pt 7): 1722–35. 2008. doi:10.1093/brain/awn105. PMID 18515320.
- ↑ "Monoclonal antibody treatment exposes three mechanisms underlying the clinical course of multiple sclerosis.". Ann Neurol 46 (3): 296–304. 1999. doi:10.1002/1531-8249(199909)46:3<296::AID-ANA4>3.0.CO;2-#. PMID 10482259.
- ↑ "Mitochondrial dysfunction contributes to neurodegeneration in multiple sclerosis". Trends in Molecular Medicine 20 (3): 179–187. 2014. doi:10.1016/j.molmed.2013.11.007. PMID 24369898.
- ↑ 47.0 47.1 Wang Zhe (2016). "Nuclear Receptor NR1H3 in Familial Multiple Sclerosis". Neuron 90 (5): 948–954. doi:10.1016/j.neuron.2016.04.039. PMID 27253448.
- ↑ "Primary Progressive Multiple Sclerosis: Putting Together the Puzzle". Front. Neurol. 8: 8–234. 2017. doi:10.3389/fneur.2017.00234. PMID 28620346.
- ↑ Sivakolundu, Dinesh K.; Hansen, Madison R.; West, Kathryn L.; Wang, Yeqi; Stanley, Thomas; Wilson, Andrew; McCreary, Morgan; Turner, Monroe P. et al. (January 27, 2019). "Three-Dimensional Lesion Phenotyping and Physiologic Characterization Inform Remyelination Ability in Multiple Sclerosis". Journal of Neuroimaging 29 (5): 605–614. doi:10.1111/jon.12633. PMID 31148298. https://onlinelibrary.wiley.com/doi/abs/10.1111/jon.12633.
- ↑ "Pathological abnormalities in the normal-appearing white matter in multiple sclerosis". Neurological Sciences 22 (2): 141–144. 2001. doi:10.1007/s100720170012. PMID 11603615.
- ↑ "Inside-Out versus Outside-In models for virus induced demyelination: axonal damage triggering demyelination.". Springer Semin Immunopathol 24 (2): 105–25. 2002. doi:10.1007/s00281-002-0105-z. PMID 12503060.
- ↑ "Loss of 'homeostatic' microglia and patterns of their activation in active multiple sclerosis". Brain 140 (7): 1900–1913. 2017. doi:10.1093/brain/awx113. PMID 28541408.
- ↑ "The pathogenesis of lesions and normal-appearing white matter changes in multiple sclerosis: a serial diffusion MRI study". Brain 123 (8): 1667–76. August 2000. doi:10.1093/brain/123.8.1667. PMID 10908196.
- ↑ Schmid, Andreas; Hochberg, Alexandra; Berghoff, Martin; Schlegel, Jutta; Karrasch, Thomas; Kaps, Manfred; Schäffler, Andreas (2016). "Quantification and regulation of adipsin in human cerebrospinal fluid (CSF)". Clinical Endocrinology 84 (2): 194–202. doi:10.1111/cen.12856. PMID 26186410.
- ↑ Ireland, Sara J.; Guzman, Alyssa A.; Frohman, Elliot M.; Monson, Nancy L. (2016). "B cells from relapsing remitting multiple sclerosis patients support neuro-antigen-specific Th17 responses". Journal of Neuroimmunology 291: 46–53. doi:10.1016/j.jneuroim.2015.11.022. PMID 26857494.
- ↑ Alireza Minagar and J Steven Alexander, Blood–brain barrier disruption in multiple sclerosis [3]
- ↑ 57.0 57.1 Correale, Jorge; Andrés Villa (24 July 2006). "The blood–brain-barrier in multiple sclerosis: Functional roles and therapeutic targeting". Autoimmunity 40 (2): 148–160. doi:10.1080/08916930601183522. PMID 17453713.
- ↑ "Identification of an essential endogenous regulator of blood–brain barrier integrity, and its pathological and therapeutic implications". Proceedings of the National Academy of Sciences of the United States of America 110 (3): 832–841. 15 January 2013. doi:10.1073/pnas.1209362110. PMID 23277546. Bibcode: 2013PNAS..110..832C.
- ↑ Prat, Elisabetta; Roland Martin (March–April 2002). "The immunopathogenesis of multiple sclerosis". Journal of Rehabilitation Research and Development 39 (2): 187–99. PMID 12051463.
- ↑ 60.0 60.1 "Elevated matrix metalloproteinase-9 and degradation of perineuronal nets in cerebrocortical multiple sclerosis plaques". J Neuropathol Exp Neurol 67 (9): 888–99. September 2008. doi:10.1097/NEN.0b013e318183d003. PMID 18716555.
- ↑ "Quantification of subtle blood–brain barrier disruption in non-enhancing lesions in multiple sclerosis: a study of disease and lesion subtypes". Multiple Sclerosis 13 (7): 884–94. 2007. doi:10.1177/1352458507076970. PMID 17468443.
- ↑ "Multiple sclerosis as a vascular disease". Neurol. Res. 28 (3): 230–5. 2006. doi:10.1179/016164106X98080. PMID 16687046.
- ↑ "Expression of immunologically relevant endothelial cell activation antigens on isolated central nervous system microvessels from patients with multiple sclerosis". Ann. Neurol. 35 (1): 89–97. Jan 1994. doi:10.1002/ana.410350114. PMID 7506877.
- ↑ Allen et al. (2001). "Pathological abnormalities in the normal-appearing white matter in multiple sclerosis". Neurol Sci 22 (2): 141–4. doi:10.1007/s100720170012. PMID 11603615.
- ↑ "Population-Wide Principal Component-Based Quantification of Blood-Brain-Barrier Dynamics in Multiple Sclerosis". NeuroImage 57 (4): 1430–46. May 2011. doi:10.1016/j.neuroimage.2011.05.038. PMID 21635955.
- ↑ "Permeation of blood-borne IL15 across the blood–brain barrier and the effect of LPS". J. Neurochem. 106 (1): 313–9. 2008. doi:10.1111/j.1471-4159.2008.05390.x. PMID 18384647.
- ↑ "Tissue-type plasminogen activator is a regulator of monocyte diapedesis through the brain endothelial barrier". Journal of Immunology 181 (5): 3567–74. 2008. doi:10.4049/jimmunol.181.5.3567. PMID 18714030.
- ↑ "Monocyte migration and LFA-1 mediated attachment to brain microvascular endothelia is regulated by SDF-1α through Lyn kinase". Journal of Immunology 181 (7): 4632–7. October 2008. doi:10.4049/jimmunol.181.7.4632. PMID 18802065.
- ↑ "Magnetic resonance imaging of human brain macrophage infiltration". Neurotherapeutics 4 (3): 434–42. 2007. doi:10.1016/j.nurt.2007.05.005. PMID 17599709.
- ↑ "Matrix metalloproteinase-9 (MMP-9) and tissue inhibitor of matrix metalloproteinase (TIMP-1) in patients with relapsing-remitting multiple sclerosis treated with interferon beta". Clin Neurol Neurosurg 108 (2): 124–8. February 2006. doi:10.1016/j.clineuro.2005.01.005. PMID 16412833.
- ↑ "Biomarkers indicative of blood–brain barrier disruption in multiple sclerosis". Dis. Markers 22 (4): 235–44. 2006. doi:10.1155/2006/709869. PMID 17124345.
- ↑ 72.0 72.1 /topic228 .htm# Multiple Sclerosis at eMedicine
- ↑ "Adhesion molecules in multiple sclerosis: relation to subtypes of disease and methylprednisolone therapy". Arch. Neurol. 57 (4): 546–51. April 2000. doi:10.1001/archneur.57.4.546. PMID 10768630. http://archneur.ama-assn.org/cgi/pmidlookup?view=long&pmid=10768630.
- ↑ Alexandre Prat, Nicole Beaulieu, Sylvain-Jacques Desjardins, New Therapeutic Target For Treatment Of Multiple Sclerosis, Jan. 2008
- ↑ "Pathological Expression of CXCL12 at the Blood-Brain Barrier Correlates with Severity of Multiple Sclerosis". Am J Pathol 172 (3): 799–808. March 2008. doi:10.2353/ajpath.2008.070918. PMID 18276777.
- ↑ "Imaging correlates of leukocyte accumulation and CXCR4/CXCR12 in multiple sclerosis". Arch. Neurol. 66 (1): 44–53. January 2009. doi:10.1001/archneurol.2008.512. PMID 19139298. PMC 2792736. http://archneur.ama-assn.org/cgi/pmidlookup?view=long&pmid=19139298.
- ↑ "Impact of methylprednisolone treatment on the expression of macrophage inflammatory protein 3alpha and B lymphocyte chemoattractant in serum of multiple sclerosis patients". Pharmacol Rep 60 (4): 549–54. 2008. PMID 18799824. http://www.if-pan.krakow.pl/pjp/pdf/2008/4_549.pdf.
- ↑ "A molecular trio in relapse and remission in multiple sclerosis". Nature Reviews Immunology 9 (6): 440–7. May 2009. doi:10.1038/nri2548. PMID 19444308.
- ↑ "Biomarkers indicative of blood–brain barrier disruption in multiple sclerosis". Disease Markers 22 (4): 235–44. 2006. doi:10.1155/2006/709869. PMID 17124345. PMC 3850823. http://iospress.metapress.com/openurl.asp?genre=article&issn=0278-0240&volume=22&issue=4&spage=235.
- ↑ "Persistent endothelial abnormalities and blood–brain barrier leak in primary and secondary progressive multiple sclerosis". Neuropathol. Appl. Neurobiol. 33 (1): 86–98. 2007. doi:10.1111/j.1365-2990.2006.00781.x. PMID 17239011.
- ↑ "The peroxynitrite scavenger uric acid prevents inflammatory cell invasion into the central nervous system in experimental allergic encephalomyelitis through maintenance of blood-central nervous system barrier integrity". Journal of Immunology 165 (11): 6511–8. 2000. doi:10.4049/jimmunol.165.11.6511. PMID 11086092.
- ↑ "Serum uric acid and multiple sclerosis". Clinical Neurology and Neurosurgery 108 (6): 527–31. 2006. doi:10.1016/j.clineuro.2005.08.004. PMID 16202511.
- ↑ "The blood–brain barrier in cortical multiple sclerosis lesions". J Neuropathol Exp Neurol 66 (4): 321–8. April 2007. doi:10.1097/nen.0b013e318040b2de. PMID 17413323.
- ↑ "Variation of serum uric acid levels in multiple sclerosis during relapses and immunomodulatory treatment". Eur. J. Neurol. 15 (4): 394–7. April 2008. doi:10.1111/j.1468-1331.2008.02087.x. PMID 18312403.
- ↑ J. William Brown et al. An Abnormal Periventricular Gradient in Magnetisation Transfer Ratio Occurs Early in Multiple Sclerosis. Neurology 2016; vol. 86 no. 16 Supplement S41.002
- ↑ 86.0 86.1 "White Matter Hemodynamic Abnormalities precede Sub-cortical Gray Matter Changes in Multiple Sclerosis". J. Neurol. Sci. 282 (1–2): 28–33. July 2009. doi:10.1016/j.jns.2008.12.036. PMID 19181347.
- ↑ University of Zurich(2018, October 11). Link Between Gut Flora and Multiple Sclerosis Discovered. NeuroscienceNews. Retrieved October 11, 2018
- ↑ Planas R, Santos R, Tomas-Ojer P, Cruciani C, Lutterotti A, Faigle W, Schaeren-Wiemers N, Espejo C, Eixarch H, Pinilla C, Martin R, Sospedra M (2018). "GDP-l-fucose synthase is a CD4+ T cell–specific autoantigen in DRB3*02:02 patients with multiple sclerosis". Science Translational Medicine 10 (462): eaat4301. doi:10.1126/scitranslmed.aat4301. PMID 30305453. https://www.zora.uzh.ch/id/eprint/158835/1/2018_Planas_GDP_L-Fucose_Sci_Transl._Med._in_press.pdf.
- ↑ Kremer (2019). "pHERV-W envelope protein fuels microglial cell-dependent damage of myelinated axons in multiple sclerosis". PNAS 116 (30): 15216–15225. doi:10.1073/pnas.1901283116. PMID 31213545. Bibcode: 2019PNAS..11615216K.
- ↑ Lisak RP (2019). "Human retrovirus pHEV-W envelope protein and the pathogenesis of multiple sclerosis". PNAS 116 (30): 14791–14793. doi:10.1073/pnas.1909786116. PMID 31289223. Bibcode: 2019PNAS..11614791L.
- ↑ Hans-Peter Hartung et al, Efficacy and Safety of Temelimab, an Antibody Antagonist of the Human Endogenous Retrovirus Type-W env Protein, in Participants with Relapsing Remitting Multiple Sclerosis: A Double-Blind, Randomised, Placebo-Controlled Phase 2b Clinical Trial, The Lancet 17 May 2019 [4]
- ↑ "Multiple sclerosis pathology: evolution of pathogenetic concepts". Brain Pathology 15 (3): 217–22. July 2005. doi:10.1111/j.1750-3639.2005.tb00523.x. PMID 16196388.[verification needed]
- ↑ Putnam, T.J. (1937) Evidence of vascular occlusion in multiple sclerosis
- ↑ "Transcranial brain sonography findings predict disease progression in multiple sclerosis". Neurology 73 (13): 1010–7. September 2009. doi:10.1212/WNL.0b013e3181b8a9f8. PMID 19657105.
- ↑ "Persistent endothelial abnormalities and blood–brain barrier leak in primary and secondary progressive multiple sclerosis". Neuropathol. Appl. Neurobiol. 33 (1): 86–98. February 2007. doi:10.1111/j.1365-2990.2006.00781.x. PMID 17239011.
- ↑ "7T MRI: New Vision of Microvascular Abnormalities in Multiple Sclerosis". Archives of Neurology 65 (6): 812–6. 2008. doi:10.1001/archneur.65.6.812. PMID 18541803.
- ↑ "Normal-appearing White and Grey Matter Damage in Multiple Sclerosis. Book review". AJNR 27 (4): 945–946. 2004. http://www.ajnr.org/cgi/content/full/27/4/945.
- ↑ Qiu, W; Raven, S; Wu, JS; Carroll, WM; Mastaglia, FL; Kermode, AG (March 2010). "Wedge-shaped medullary lesions in multiple sclerosis". Journal of the Neurological Sciences 290 (1–2): 190–3. doi:10.1016/j.jns.2009.12.017. PMID 20056253.
- ↑ "Chlamydia pneumoniae DNA in the Arterial Wall of Patients with Peripheral Vascular Disease". Infection 29 (4): 196–200. 2001. doi:10.1007/s15010-001-1180-0. PMID 11545479.
- ↑ 100.0 100.1 "Chronic cerebrospinal venous insufficiency in patients with multiple sclerosis". J. Neurol. Neurosurg. Psychiatry 80 (4): 392–9. April 2009. doi:10.1136/jnnp.2008.157164. PMID 19060024.
- ↑ 101.0 101.1 "Chronic cerebrospinal venous insufficiency and multiple sclerosis". Annals of Neurology 67 (3): 286–90. March 2010. doi:10.1002/ana.22001. PMID 20373339. http://www3.interscience.wiley.com/journal/123283159/abstract.
- ↑ Bryce Weir (2010). "MS, A vascular ethiology?". Can. J. Neurol. Sci. 37 (6): 745–757. doi:10.1017/s0317167100051404. PMID 21059535.
- ↑ "Haemodynamic patterns in chronic cereblrospinal venous insufficiency in multiple sclerosis. Correlation of symptoms at onset and clinical course". Int Angiol 29 (2): 183–8. April 2010. PMID 20351667.
- ↑ "Intracranial venous haemodynamics in multiple sclerosis". Curr Neurovasc Res 4 (4): 252–8. November 2007. doi:10.2174/156720207782446298. PMID 18045150. http://www.bentham-direct.org/pages/content.php?CNR/2007/00000004/00000004/004AG.SGM.
- ↑ "Chronic cerebrospinal venous insufficiency in patients with multiple sclerosis". J. Neurol. Neurosurg. Psychiatry 80 (4): 392–9. April 2009. doi:10.1136/jnnp.2008.157164. PMID 19060024.
- ↑ "Embryological background of truncular venous malformation in the extracranial venous pathways as the cause of chronic cerebro spinal venous insufficiency". Int Angiol 29 (2): 95–108. April 2010. PMID 20351665. http://www.fondazionehilarescere.org/pdf/03-2518-ANGY.pdf.
- ↑ "Internal jugular vein morphology and hemodynamics in patients with multiple sclerosis". Int Angiol 29 (2): 115–20. April 2010. PMID 20351667.
- ↑ "["Chronic cerebrospinal venous insufficiency" and multiple sclerosis : Critical analysis and first observation in an unselected cohort of MS patients.]". Nervenarzt 81 (6): 740–6. April 2010. doi:10.1007/s00115-010-2972-1. PMID 20386873.
- ↑ "No cerebrocervical venous congestion in patients with multiple sclerosis". Annals of Neurology 68 (2): 173–83. August 2010. doi:10.1002/ana.22085. PMID 20695010.
- ↑ "Venous and cerebrospinal fluid flow in multiple sclerosis: A case-control study". Annals of Neurology 68 (2): 255–259. 2010. doi:10.1002/ana.22132. PMID 20695018.
- ↑ Damadian RV, Chu D. The possible role of cranio-cervical trauma and abnormal CSF hydrodynamics in the genesis of multiple sclerosis, 2011, [5]
- ↑ Zamboni (2010). "CSF dynamics and brain volume in multiple sclerosis are associated with extracranial venous flow anomalies". Int Angiol 29 (2): 140–8. PMID 20351670.
- ↑ Raymond V. Damadian and David Chu, The Possible Role of Cranio-Cervical Trauma and Abnormal CSF Hydrodynamics in the Genesis of Multiple Sclerosis [6] [7] [8]
- ↑ "Secretory products of multiple sclerosis B cells are cytotoxic to oligodendroglia in vitro". Journal of Neuroimmunology 246 (1–2): 85–95. 2012. doi:10.1016/j.jneuroim.2012.02.015. PMID 22458983.
- ↑ Ilana Katz Sand et al. CSF from MS Patients Induces Mitochondrial Dysfunction in Unmyelinated Neuronal Cultures, Neurology February 12, 2013; 80(Meeting Abstracts 1): P05.179
- ↑ Lassmann H (2019). "Pathogenic Mechanisms Associated With Different Clinical Courses of Multiple Sclerosis". Front Immunol 9: 3116. doi:10.3389/fimmu.2018.03116. PMID 30687321.
- ↑ "Axonal damage induced by cerebrospinal fluid from patients with relapsing-remitting multiple sclerosis". J Neuroimmunol 104 (1): 58–67. Apr 2000. doi:10.1016/s0165-5728(99)00225-8. PMID 10683515.
- ↑ "The effect of cerebrospinal fluid on neurone culture: implications in the pathogenesis of multiple sclerosis". Rev Neurol 35 (10): 994–7. 2002. PMID 12436405.
- ↑ "Antibodies reactive to heat shock protein 90 induce oligodendrocyte precursor cell death in culture. Implications for demyelination in multiple sclerosis". FASEB J. 18 (2): 409–11. Feb 2004. doi:10.1096/fj.03-0606fje. PMID 14688203.
- ↑ Tiwari-Woodruff SK, Myers LW, Bronstein JM (Aug 2004). "Cerebrospinal fluid immunoglobulin G promotes oligodendrocyte progenitor cell migration". J. Neurosci. Res. 77 (3): 363–6. doi:10.1002/jnr.20178. PMID 15248292.
- ↑ "Cerebrospinal fluid derived from progressive multiple sclerosis patients promotes neuronal and oligodendroglial differentiation of human neural precursor cells in vitro". Neuroscience 250: 614–21. Oct 2013. doi:10.1016/j.neuroscience.2013.07.022. PMID 23876320.
- ↑ Cristofanilli, Massimiliano; Rosenthal, Hannah; Cymring, Barbara; Gratch, Daniel; Pagano, Benjamin; Xie, Boxun; Sadiq, Saud A. (2014). "Progressive multiple sclerosis cerebrospinal fluid induces inflammatory demyelination, axonal loss, and astrogliosis in mice". Experimental Neurology 261: 620–32. doi:10.1016/j.expneurol.2014.07.020. PMID 25111532.
- ↑ "Transfer of multiple sclerosis into severe combined immunodeficiency mice by mononuclear cells from cerebrospinal fluid of the patients". PNAS 89 (13): 6157–6161. 1992. doi:10.1073/pnas.89.13.6157. PMID 1631103. Bibcode: 1992PNAS...89.6157S.
- ↑ "Cerebrospinal fluid ceramides from patients with multiple sclerosis impair neuronal bioenergetics". Brain 137 (8): 2271–86. Aug 2014. doi:10.1093/brain/awu139. PMID 24893707.
- ↑ Burgal, Mathur (Jul 2014). "Molecular Shots". Ann Neurosci 21 (3): 123. doi:10.5214/ans.0972.7531.210311. PMID 25206080.
- ↑ "Potassium channel KIR4.1 as an immune target in multiple sclerosis". N Engl J Med 367 (2): 115–23. Jul 2012. doi:10.1056/NEJMoa1110740. PMID 22784115.
- ↑ Schneider, Raphael (2013). "Autoantibodies to Potassium Channel KIR4.1 in Multiple Sclerosis". Frontiers in Neurology 4: 125. doi:10.3389/fneur.2013.00125. PMID 24032025.
- ↑ Marnetto, Fabiana (2017). "Detection of potassium channel KIR4.1 antibodies in Multiple Sclerosis patients". Journal of Immunological Methods 445: 53–58. doi:10.1016/j.jim.2017.03.008. PMID 28300540.
- ↑ Ayoglua Burcu (2016). "Anoctamin 2 identified as an autoimmune target in multiple sclerosis". PNAS 113 (8): 2188–2193. doi:10.1073/pnas.1518553113. PMID 26862169. Bibcode: 2016PNAS..113.2188A.
- ↑ Matthews Lucy (2015). "Imaging Surrogates of Disease Activity in Neuromyelitis Optica Allow Distinction from Multiple Sclerosis". PLOS ONE 10 (9): e0137715. doi:10.1371/journal.pone.0137715. PMID 26381510. Bibcode: 2015PLoSO..1037715M.
- ↑ "Axonal damage induced by cerebrospinal fluid from patients with relapsing-remitting multiple sclerosis". Journal of Neuroimmunology 104 (1): 58–67. 2000. doi:10.1016/S0165-5728(99)00225-8. PMID 10683515.
- ↑ Peferoen, L., D. Vogel, Marjolein Breur, Wouter Gerritsen, C. Dijkstra, and S. Amor. "Do stressed oligodendrocytes trigger microglia activation in pre-active MS lesions?." In GLIA, vol. 61, pp. S164-S164. 111 RIVER ST, HOBOKEN 07030-5774, NJ USA: WILEY-BLACKWELL, 2013.
- ↑ "Clusters of activated microglia in normal-appearing white matter show signs of innate immune activation". Journal of Neuroinflammation 9: 156. 2012. doi:10.1186/1742-2094-9-156. PMID 22747960.
- ↑ "A gradient in cortical pathology in multiple sclerosis by in vivo quantitative 7 T imaging". Brain 138 (Pt 4): 932–45. 2015. doi:10.1093/brain/awv011. PMID 25681411.
- ↑ 135.0 135.1 Hottenrott T, Dersch R, Berger B, Rauer S, Eckenweiler M, Huzly D, Stich O (2015). "The intrathecal, polyspecific antiviral immune response in neurosarcoidosis, acute disseminated encephalomyelitis and autoimmune encephalitis compared to multiple sclerosis in a tertiary hospital cohort". Fluids Barriers CNS 12: 27. doi:10.1186/s12987-015-0024-8. PMID 26652013.
- ↑ Fabio Duranti; Massimo Pieri; Rossella Zenobi; Diego Centonze; Fabio Buttari; Sergio Bernardini; Mariarita Dessi. "kFLC Index: a novel approach in early diagnosis of Multiple Sclerosis". International Journal of Scientific Research 4 (8). http://worldwidejournals.in/ojs/index.php/ijsr/article/download/6571/6613. Retrieved 2018-08-27.
External links
- The lesion project page
- MRI and CT of Multiple Sclerosis[yes|permanent dead link|dead link}}] MedPix Image Database
 |