Medicine:Congenital hyperinsulinism
| Congenital hyperinsulinism | |
|---|---|
| Other names | CHI, familial hyperinsulinism, hyperinsulinemic hypoglycemia of infancy |
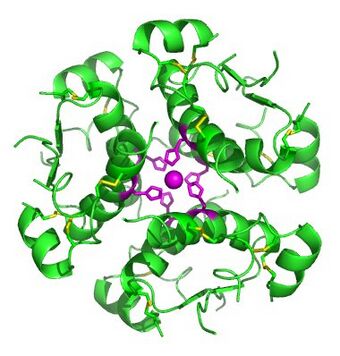 | |
| Insulin (which this condition creates in excess) | |
| Symptoms | Hypoglycemia[1] |
| Causes | ABCC8 gene mutations (most common)[2] |
| Diagnostic method | Blood sample[3] |
| Treatment | Diazoxide, octreotide [4] |
Congenital hyperinsulinism (HI or CHI) is a rare condition causing severe hypoglycemia (low blood sugar) in newborns due to the overproduction of insulin.[5] There are various causes of HI, some of which are known to be the result of a genetic mutation.[6] Sometimes HI occurs on its own (isolated) and more rarely associated with other medical conditions (as a syndrome).[7]
Congenital forms of hyperinsulinism can be transient (short-term) or persistent (long-term) and mild or severe. It can be the result of a defect in the entire pancreas (diffuse HI) or in just part of the pancreas (focal HI).[7] Irrespective of the form, cause, or type, HI is a medical emergency that must be managed from its onset.[8] There is no other hypoglycemic condition in the newborn period as dangerous as HI.[9] Left untreated, hypoglycemia from HI can cause developmental disorders, seizures, permanent brain damage, and even death.[10][11]
For those with focal HI, there is the potential for a cure with surgery.[12] For those with diffuse HI, diazoxide is the only approved medication to treat hypoglycemia. For those who do not respond to diazoxide, the condition is often managed with continuous carbohydrates delivered through a feeding pump and a gastrostomy tube, and off-label use of medications such as octreotide given by injection.[13][14] In the most severe cases, surgery may be necessary to remove most of the pancreas.[12] New and more effective treatments are in development for those who continue to have hypoglycemia on existing therapies and treatments, and for those who experience adverse effects of current treatments.[15]
The incidence of persistent HI has been found to range from 1:2,500 to 1:50,000 births depending on the region or country.[8] The incidence of transient forms of HI has been estimated to be between 1:1200[16] and 1:2000.[17]
Signs and symptoms
As HI is a congenital condition, an infant usually starts to show signs and symptoms within the first few days of life, although very occasionally symptoms may appear later in life. It is often difficult to identify signs and symptoms of HI because they are often confused with typical behaviours of new-borns and infants.[18] About 60% of babies with HI develop hypoglycemia during the first month of life. An additional 30% will be diagnosed later in the first year and some later in life.[5]
HI may present in several ways; common symptoms of hypoglycemia include:
- Irritability[19][20]
- Lethargy (excessive sleepiness)[21][20]
- Jitteriness/tremors[21][22][19][20]
- Tachycardia or bradycardia[23]
- Abnormal breathing patterns/apnoea[19][20]
- Hypothermia[21][19][20]
- Abnormal feeding behaviour (not waking for feeds, not sucking effectively, appearing unsettled and demanding very frequent feeds especially after a period of feeding well)[21][19][20]
- High pitched cry[21]
- Hypotonia (Loose/floppy muscles)[21][19][20]
- Pale/pallor/cyanosis (bluish coloured skin)[19]
- Sweating[22][20]
Older children and adults’ symptoms may also include headaches, confusion and feeling dizzy.[23]
Parents often describe initial concerns or symptoms such as their infants “not feeding well, being sleepy and jittery”.[5]
More severe symptoms, such as seizures (fits or convulsions), can occur with a prolonged or extremely low blood sugar level.[24][22][19][20] If the blood sugar level is not corrected, it can lead to loss of consciousness and potential brain injury.[24]
A simple blood sugar measurement is essential if there are any symptoms of hypoglycaemia.[25]
Cause
Hyperinsulinism or congenital hyperinsulinism can be a genetic or acquired condition. Acquired HI may be secondary to factors around birth, such as growth restriction of the fetus, less oxygen to the baby or maternal diabetes. Together, these are often called perinatal stress induced HI. They are typically present in the first 24 hours of life but often resolve by two weeks of age.[17][26]
In contrast to the resolving perinatal stress induced low blood sugars, HI can also be due to a genetic cause. Therefore, genetic testing should be considered in children in whom acquired HI is unlikely. This typically includes those not responding to first line medication diazoxide. A genetic cause is also possible in children responding to diazoxide but where low sugars persist beyond the first 4 months of life.[6][27]
There are many different genetic forms of HI which can be present in isolation or as part of a wider condition, called a syndrome.[28]
Isolated forms
Isolated hyperinsulinism occurs in the majority of individuals with HI. The most common genetic cause is a change in one or both copies of a gene that instructs the building of the potassium channel (ABCC8 and KCNJ11).[29][30] This channel normally regulates insulin production from the β-cell in the pancreas in response to sugar levels in the blood. A change or fault in the channel leads to uncontrolled and excessive production of insulin. These changes in the ABCC8/KCNJ11 genes can be inherited in a dominant or recessive manner. In the dominant form, a single (monoallelic) change inherited from one parent (or arising spontaneously) causes diffuse HI. In diffuse HI, the whole pancreas is affected. Dominant HI may be mild and respond to diazoxide or severe and diazoxide unresponsive. Some changes in the ABCC8 and KCNJ11 genes are not inherited dominantly but are inherited recessively. In these families each parent carries one copy of a faulty gene, but are themselves unaffected. A child will develop HI if they inherit two copies of the faulty ABCC8/KCNJ11 gene, one from each parent. Recessively-inherited changes in the ABCC8/KCNJ11 genes cause diffuse HI which typically does not respond to diazoxide. In some cases, a paternal copy of the faulty gene is inherited by the child which occurs in combination with a loss of the mother’s normal copy of the gene in the pancreas. This gives rise to focal HI where only one part of the pancreas (called a focal lesion) produces excess insulin.[6][31][7]
If HI is severe and not responsive to medicines, rapid testing of the ABCC8 and KCNJ11 genes is recommended. This helps to identify the possibility of focal HI early in the course of the illness. Following a genetic finding, specialised positron emission tomography (PET) scanning using the radiotracer 18-fluoro-dopa can be used to localise the focal abnormality (lesion) for surgical removal. Genetic testing is also helpful to determine if two copies of faulty ABCC8/KCNJ11 genes are inherited – these indicate a diagnosis of diffuse HI that may not respond to diazoxide. Such cases require treatment with alternative medications such as octreotide and may need surgical removal of most of the pancreas. Therefore, early rapid genetic testing is important to guide the medical and surgical management of children with severe HI. Results from HI genetic testing are preferably analysed by molecular genetics laboratories experienced and specialised in HI.[32][28][7][27]
Another common genetic cause of HI results from changes in the gene for the enzyme glutamate dehydrogenase (GDH). This genetic form of HI is also known as GDH-CHI or GLUD1-CHI. These gene changes are inherited dominantly but may also arise spontaneously. In this condition, ammonia levels in blood are mildly raised. Children and adults with GDH-CHI often respond to diazoxide. An excess of proteins in the diet can bring about low sugars, so a good carbohydrate to protein ratio is advisable. There are many other genetic causes of isolated HI. Examples include changes in the genes that make the enzymes hydroxyacyl-CoA dehydrogenase gene (SCHAD-CHI) and glucokinase (GCK-CHI). More recently, changes in hexokinase 1 (HK1), another enzyme similar to glucokinase has been identified to cause both mild and severe forms of illness.[27][7][33]
Syndromic forms
Syndromic HI is less common than isolated HI. Data from patient registries suggest a prevalence of less than 1% among reported cases.[34] In syndromic HI, genetic causes are common.[35] Beckwith-Wiedemann syndrome (BWS), an overgrowth syndrome is a well-recognized form of syndromic HI. Other syndromes that commonly feature HI include Kabuki syndrome and Turner syndrome. Most individuals with syndromic HI respond to treatment with diazoxide and HI may resolve over time. However, HI with BWS can be severe and be unresponsive to usual therapy.[36][37][38]
Diagnosis

HI is due to dysregulation of secretion of the hormone insulin from beta-cells in the pancreas. Insulin is present in the blood at the time of hypoglycemia rather than being suppressed. This can be difficult to measure due to fluctuation in insulin levels. The diagnosis of HI is made on the basis of increased insulin action and/or inadequate suppression of plasma insulin during a time of hypoglycemia. Increased insulin action can be demonstrated by increased glucose requirement (e.g., > 8 mg/kg/minute in a newborn compared to normal of 4-6 mg/kg/minute.[39] Another sign of excess insulin action is suppressed blood levels of free fatty acids and ketones (beta-hydroxybutyrate) during hypoglycemia. The clinical diagnosis is also supported by a large blood glucose rise after glucagon administration at the time of hypoglycemia.[40][41][42] Glucagon is another hormone secreted from the pancreas that opposes insulin action and stimulates the release of glucose from liver glycogen stores. Measurement of insulin, c-peptide (which is co-secreted with insulin) free fatty acids and ketones together with a glucagon stimulation test can be performed during the spontaneous time of hypoglycemia or during hypoglycemia induced by a period of supervised and monitored fasting. In newborn infants, there is a time of transitional hypoglycaemia due to hyperinsulinism for the first after birth 72 hours. Hence the clinical diagnosis is best established after 72 hours of age.[28] Assessing blood ammonia and acylcarnitine profile, urinary metabolic profiles, in addition to provocative responses to protein and amino acids (leucine) may be helpful in defining the subtype of HI.[43][44][45][46]
Treatment
The goal of treatment in hyperinsulinism is to prevent hypoglycemia-induced brain damage, thus, the goal of therapy is to maintain the blood sugar level in the normal range [>70 mg/dL (3.9 mmol/L)]. The first step is the restoration of blood sugar level to the normal range after acute hypoglycemia, followed by prevention of recurrent episodes of hypoglycemia, which is common in congenital hyperinsulinism. This is best accomplished with intravenous dextrose initially.
Once the diagnosis of HI has been established, including determination of the genotype and phenotype, whenever possible, specific treatment should be initiated. Some of the following measures are often tried:
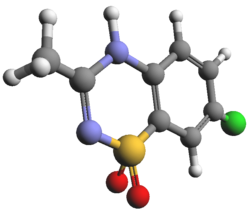
Diazoxide, a KATP channel opener, that inhibits insulin secretion by binding to the sulfonylurea 1 (SUR1) component of the KATP channel, is the only drug with regulatory approval for the treatment of HI and the first line of therapy for this condition.[49] To prevent complications from diazoxide-induced fluid retention, diuretic therapy is typically initiated concomitantly with diazoxide. Dose selection and dose escalation should be carefully considered weighing the response and potential for side effects. Because of its long half-life it may take up to 5 days to achieve a full therapeutic effect. An important next step is the assessment of the responsiveness to diazoxide, which has important diagnostic and therapeutic implications. Responsiveness to diazoxide is defined by the demonstration that the cardinal feature of HI, hypoketotic hypoglycemia, is corrected by treatment. This is best assessed by a fasting test demonstrating that the child can fast for 12-18 hours with plasma glucose ≥ 70 mg/dL (3.9 mmol/L) or that plasma betahydroxybutyrate increases to > 1.8 mmol/L before plasma glucose decreases below 50-60 mg/dL (2.8-3.3 mmol/L) during fasting. Lack of responsiveness to diazoxide suggests the possibility that the HI is due to inactivating mutation(s) in the genes encoding the KATP channels which accounts for up to 90% of cases of diazoxide-unresponsive HI. For these cases, rapid genetic testing of the genes ABCC8 and KCNJ11 is critical to determine the likelihood of focal HI.[50]
Surgery is the treatment of choice for focal HI, but before surgery, it is important to localize the lesion. These lesions are not visible using conventional imaging techniques such as ultrasound, computed tomography (CT) scan, and magnetic resonance imaging (MRI) However, specialized imaging using 18-F-L 3,4 dihydroxyphenylalanine (18F DOPA) positron emission tomography (PET) scan is almost 100% accurate in localizing a focal lesion.[51] Expert assessment of the pancreatic histology during surgery using frozen biopsies and surgical expertise are key for the success of the surgery. The reported cure rate for focal HI is 97%.[12]
For non-focal diazoxide-unresponsive cases, treatment options are limited. Off-label use of the somatostatin analogue octreotide has been the long-standing second line of treatment for HI,[52] but its effectiveness is limited by the development of tachyphylaxis. It is important to note that in countries where diazoxide is not available, octreotide may be the first line of therapy. Because of its association with potentially fatal necrotizing enterocolitis, octreotide use in very young infants should be carefully considered weighting the risk versus the potential benefits.[53] Octreotide is administrated as a subcutaneous injection typically every 6 hours but it can also be administrated continuously through a subcutaneous pump. Long-acting somatostatin analogues, octreotide LAR (administrated intramuscularly) and lanreotide (administered as a deep subcutaneous injection), are a convenient option for older children. An alternative treatment approach for diazoxide-unresponsive cases that are either not eligible or unresponsive to somatostatin analogues is the use of a continuous infusion of dextrose through a gastrostomy tube.[54] Typically, dextrose 20% is used and because of tolerance, the maximal glucose infusion rate administrated through this route is 10 mg/kg/min. Continuous intragastric dextrose is also used in combination with octreotide, an approach that allows for the use of less frequent dosing of octreotide and avoidance of tachyphylaxis. Another option preferred by some centers includes the administration of carbohydrate supplemented formula feedings intermittently or continuously by a gastrostomy tube. A near-total pancreatectomy is indicated when medical therapy fails. [citation needed]
Ongoing monitoring of glycemic control, therapy-associated side effects, and of growth and development are part of the treatment plan. Children who have undergone ≥ 50% pancreatectomy are monitored for diabetes and pancreatic insufficiency.
Multiple new therapies for HI are under development and promise to make possible a personalized approach to treatment of children with HI in an effort to improve their long-term outcome. Therapies currently in clinical trials include: a peptide antagonist of the GLP-1 receptor, a short-acting soluble glucagon analogue, a long-acting glucagon analogue, a selective non-peptide somatostatin receptor 5 agonist, and an allosteric inhibitor of the insulin receptor.
Prognosis
The outcomes of individuals with HI are affected by the disease process itself, including consequences of delayed diagnosis, the side effects of therapy, and the effectiveness of treatment.
Side effects of therapy are common in children treated with diazoxide and somatostatin analogues, affecting up to 50% of treated patients with various degree of severity.[55][56][57][58][52] Surgical outcomes are excellent for children with the focal form of HI with a cure rate of 97%.[12] However, up to 50% of children with the diffuse form of the disease that undergo a near-total pancreatectomy continue to have hypoglycemia after surgery requiring additional therapy.[12][10] Over time, these children developed insulin dependent diabetes and pancreatic insufficiency. Ninety-one percent of children who had undergone a near-total pancreatectomy require insulin by age 14 years.[59]
The frequency of neurodevelopmental and neurobehavioral problems in children with hyperinsulinism is as high as 40-50% across different patient types and countries.[11][10][60][61] Therefore neurodevelopmental assessments should be performed throughout childhood, even in those children who have outgrown or have undergone surgical cure of the disease.
Epidemiology
The incidence of HI is variable. It ranges from 1:2500 in people where cousin marriages are common to 1:50,000 in other people. These numbers may be inaccurate as they are based on small numbers of children with HI admitted to hospitals.[8] The incidence of persistent forms of HI have been reported in the UK to be 1:28,389.[62] In Finland, the incidence has been reported to be 1:13,500.[63] The incidence of transient forms of HI has been reported at 1:7400. However, perinatal stress induced hyperinsulinism is relatively common and so the figure is predicted to be higher.[63][7] The true incidence of HI will not be known until newborn screening services are developed for HI.
The natural history of HI varies with the severity of illness and whether or not HI is transient. Children with severe HI are often unresponsive to medical treatment and may require pancreatic surgery.[64] Although surgery is more likely in those with genetic forms of HI, there appears to be reduction in severity over time, encouraging some clinicians to maintain normal glucose levels by a combination of medications such as octreotide and carbohydrate rich feeds.[12][65] Similarly, some children with changes in genes making up the potassium channel (ABCC8/KCNJ11) showed a reduction in severity.[66]
Changes in single copy of the ABCC8/KCNJ11 genes can be inherited by dominant transmission, i.e., transmission from an affected parent to the child. In such children, remission can happen, although variably.[67][68] In this group, some children and adults may also develop high blood sugar and diabetes in later life.[69] Similarly, a change from low to high blood sugar can also be seen in those with changes in HNF1A and HNF4A genes.[70][71]
The natural history of HI goes beyond the problem of hypoglycemia. An important consequence of early life hypoglycemia is brain injury. Delays in childhood development have been reported in up to 50%, particularly in those with severe HI.[10][11] Feeding problems are also reported commonly by parents.[5][72] Feeding problems appear to be more frequent in children with severe HI and may continue over long periods.[73][74]
The natural history of HI includes the onset and progress of treatment related side effects. In the short term, diazoxide may cause life threatening pulmonary hypertension but this happens only in a minority of cases.[75] More commonly, many on diazoxide develop excess body hair or a change in facial features over a long time.[6][72][76] Children with focal forms of HI treated by limited surgery to the pancreas are usually cured and have no residual pancreas problems. By contrast, those having more extensive surgery, for example subtotal pancreatectomy, invariably develop diabetes requiring insulin by late childhood or adolescence.[77] In the period after pancreatic surgery, they often have a combination of low and high sugars before frank diabetes. About half of such individuals develop the need for pancreatic enzyme supplements.[78]
History
Congenital hyperinsulinism (HI) has been referred to by a variety of names; nesidioblastosis and islet cell adenomatosis were favored in the 1970s, beta cell dysregulation syndrome or dysmaturation syndrome in the 1980s, and persistent hyperinsulinemic hypoglycemia of infancy (PHHI) in the 1990s.[79]
Symptomatic hypoglycemia caused by insulin was first recognized in 1922 when one of the first diabetes patients ever treated with insulin was found “climbing the walls” due to hypoglycemia induced by insulin. The first description of children with congenital hyperinsulinism was made in 1954 by Dr Irvin McQuarrie in his presidential address to the American Pediatric Society. McQuarrie termed the disorder “idiopathic hypoglycemia of infancy” and several of his patients required removal of most of their pancreas to control their hypoglycemia. McQuarrie suggested the disorder might be genetic, since hypoglycemia ran in families of some of his patients; however, he incorrectly believed that insulin was not the cause, since no insulin-producing tumors were found in the pancreas of patients. The following year, Cochrane and colleagues in Toronto reported that hypoglycemia in some, but not all, cases of idiopathic hypoglycemia could be provoked by protein or by certain individual amino acids, especially leucine.[79] “Leucine-sensitive” hypoglycemia provided the first indication that amino acids, as well as glucose, could be important stimulators of insulin release.[80][81][82]
HI is sometimes incorrectly referred to as “nesidioblastosis”, based on the appearance of the pancreatic tissue showing insulin cells arising from ductal structures. However, the term was discarded when it was shown that nesidioblastosis was merely a common feature of the pancreas in early infancy.[79] It is now well recognised that HI is a disorder of beta-cell insulin regulation due to genetic mutations.[28]
In 1964, Drash and colleagues reported that diazoxide, an antihypertensive that suppresses insulin secretion, controlled hypoglycemia in some children with HI; currently, this is the only FDA-approved drug for treatment of hyperinsulinism.[79]
In 1996, mutations causing HI were discovered in the genes (ABCC8, KCNJ11) that encode the K-ATP channel which serves a key role in glucose-stimulated insulin secretion.[83][84] Shortly thereafter, mutations in glucokinase (GCK) and glutamate dehydrogenase (GLUD1) were also identified to cause HI.[85][86][28] The list of HI genes has now grown to over 30.[87] Rapid genetic testing for the most common HI genes has become part of standard diagnosis and can be helpful in identifying infants likely to have a focal form of HI that can be cured by surgical removal.[88][89] In 2003, it was shown that radioactive 18-fluoro-DOPA PET scans could assist surgeons locate and resect focal HI tumors.[90]
Society and culture
Patient advocacy organizations
Patient advocacy organizations dedicated to improving the lives of people born with congenital hyperinsulinism play an important role in supporting people with the disease and their families, participating in and funding research on HI, and raising awareness of the condition.[91][92] For example Congenital Hyperinsulinism International is a globally focused patient advocacy organization dedicated to improving the lives of people born with congenital hyperinsulinism. They are a member of the Chan Zuckerberg Initiative's Rare as One Network, which is a group of patient led organizations that have launched collaborative research networks.[72]
Country specific patient advocacy organizations include:
- Austria: Lobby4kids[93]
- Argentina: Hiperinsulinismo Congénito (HICA)[94]
- Brazil: Associação Hiperinsulinismo Congênito[95]
- France: Association des Hyperinsulinismes[96]
- Germany: Kongenitaler Hyperinsulinismus e.V.[97]
- Italy: Vivere con C.H.I.[98]
- Spain: Hiperinsulinismo Congenito[99]
- Turkey: Konjenital Hiperinsülinizmli Hasta Aileleri Derneği[100]
- United Kingdom: The Children’s Hyperinsulinism Charity[101]
Patient registries
People with congenital hyperinsulinism can participate in a patient reported registry called the HI Global Registry. By submitting a survey on their experiences to the registry, people with HI can help research on the condition.[72][102]
Centers of Excellence
Since 2021, centers that provide the highest quality of care for people with congenital hyperinsulinism (HI) are designated as Centers of Excellence (COE) by the Congenital Hyperinsulinism International (CHI). Being a COE also involves a commitment to research and collaboration.[91][103][104]
The CHI Center of Excellence are:[105]
- Congenital Hyperinsulinism Center at the Children’s Hospital of Philadelphia, PA, United States[106]
- The Hyperinsulinism Center at Cook Children’s Medical Center in Fort Worth, TX, United States[107]
- Congenital Hyperinsulinism Service at the Great Ormond Street Hospital in London, United Kingdom[108]
- Charite-Universitatsmedizin Berlin and the University Children’s Hospital Duesseldorf partnership in Germany[109]
- Collaborative Alliance on Congenital Hyperinsulinism (COACH) headquartered in Magdeburg, Germany[110]
- Northern Congenital Hyperinsulinism Service (NORCHI) in Manchester and Liverpool, in the United Kingdom[111]
See also
References
- ↑ "Familial hyperinsulinism | Genetic and Rare Diseases Information Center(GARD) – an NCATS Program". https://rarediseases.info.nih.gov/diseases/3947/familial-hyperinsulinism. Retrieved 28 November 2016.
- ↑ Reference, Genetics Home. "congenital hyperinsulinism". https://ghr.nlm.nih.gov/condition/congenital-hyperinsulinism.
- ↑ Hussain, K. (August 2005). "Congenital hyperinsulinism". Seminars in Fetal and Neonatal Medicine 10 (4): 369–376. doi:10.1016/j.siny.2005.03.001. PMID 15916932. – via ScienceDirect (Subscription may be required or content may be available in libraries.)
- ↑ Congenital Hyperinsulinism: Background, Pathophysiology, Etiology. 2016-07-01. http://emedicine.medscape.com/article/923538-overview.
- ↑ 5.0 5.1 5.2 5.3 Banerjee, Indraneel; Raskin, Julie; Arnoux, Jean-Baptiste; De Leon, Diva D.; Weinzimer, Stuart A.; Hammer, Mette; Kendall, David M.; Thornton, Paul S. (2022-02-19). "Congenital hyperinsulinism in infancy and childhood: challenges, unmet needs and the perspective of patients and families" (in en). Orphanet Journal of Rare Diseases 17 (1): 61. doi:10.1186/s13023-022-02214-y. ISSN 1750-1172. PMID 35183224.
- ↑ 6.0 6.1 6.2 6.3 Banerjee, I.; Salomon-Estebanez, M.; Shah, P.; Nicholson, J.; Cosgrove, K. E.; Dunne, M. J. (23 September 2018). "Therapies and outcomes of congenital hyperinsulinism-induced hypoglycaemia". Diabetic Medicine 36 (1): 9–21. doi:10.1111/dme.13823. ISSN 1464-5491. PMID 30246418.
- ↑ 7.0 7.1 7.2 7.3 7.4 7.5 Rosenfeld, Elizabeth; Ganguly, Arupa; De Leon, Diva D. (14 August 2019). "Congenital hyperinsulinism disorders: Genetic and clinical characteristics" (in en). American Journal of Medical Genetics Part C: Seminars in Medical Genetics 181 (4): 682–692. doi:10.1002/ajmg.c.31737. ISSN 1552-4868. PMID 31414570.
- ↑ 8.0 8.1 8.2 Arnoux, Jean-Baptiste; Verkarre, Virginie; Saint-Martin, Cécile; Montravers, Françoise; Brassier, Anaïs; Valayannopoulos, Vassili; Brunelle, Francis; Fournet, Jean-Christophe et al. (3 October 2011). "Congenital hyperinsulinism: current trends in diagnosis and therapy" (in en). Orphanet Journal of Rare Diseases 6 (1): 63. doi:10.1186/1750-1172-6-63. ISSN 1750-1172. PMID 21967988.
- ↑ Thornton, Paul S. (2021-08-01). "Recent updates in the management of infants and children with hyperinsulinism" (in en). Current Opinion in Pediatrics 33 (4): 424–429. doi:10.1097/MOP.0000000000001022. ISSN 1040-8703. PMID 34001718. https://journals.lww.com/10.1097/MOP.0000000000001022.
- ↑ 10.0 10.1 10.2 10.3 Lord, Katherine; Radcliffe, Jerilynn; Gallagher, Paul R.; Adzick, N. Scott; Stanley, Charles A.; De León, Diva D. (1 September 2015). "High Risk of Diabetes and Neurobehavioral Deficits in Individuals With Surgically Treated Hyperinsulinism" (in en). The Journal of Clinical Endocrinology & Metabolism 100 (11): 4133–4139. doi:10.1210/jc.2015-2539. ISSN 0021-972X. PMID 26327482.
- ↑ 11.0 11.1 11.2 Avatapalle, Hima Bindu; Banerjee, Indraneel; Shah, Sajni; Pryce, Megan; Nicholson, Jacqueline; Rigby, Lindsey; Caine, Louise; Didi, Mohammed et al. (2013). "Abnormal Neurodevelopmental Outcomes are Common in Children with Transient Congenital Hyperinsulinism". Frontiers in Endocrinology 4: 60. doi:10.3389/fendo.2013.00060. ISSN 1664-2392. PMID 23730298.
- ↑ 12.0 12.1 12.2 12.3 12.4 12.5 Adzick, N. Scott; De Leon, Diva D.; States, Lisa J.; Lord, Katherine; Bhatti, Tricia R.; Becker, Susan A.; Stanley, Charles A. (18 October 2018). "Surgical treatment of congenital hyperinsulinism: Results from 500 pancreatectomies in neonates and children" (in en). Journal of Pediatric Surgery 54 (1): 27–32. doi:10.1016/j.jpedsurg.2018.10.030. PMID 30343978.
- ↑ Yorifuji, Tohru (2014). "Congenital hyperinsulinism: current status and future perspectives" (in en). Annals of Pediatric Endocrinology & Metabolism 19 (2): 57–68. doi:10.6065/apem.2014.19.2.57. ISSN 2287-1012. PMID 25077087.
- ↑ Yorifuji, Tohru; Horikawa, Reiko; Hasegawa, Tomonobu; Adachi, Masanori; Soneda, Shun; Minagawa, Masanori; Ida, Shinobu; Yonekura, Takeo et al. (2017). "Clinical practice guidelines for congenital hyperinsulinism" (in en). Clinical Pediatric Endocrinology 26 (3): 127–152. doi:10.1297/cpe.26.127. ISSN 0918-5739. PMID 28804205. PMC 5537210. https://www.jstage.jst.go.jp/article/cpe/26/3/26_2017-0008/_article.
- ↑ De Cosio, Ana Paola; Thornton, Paul (20 June 2019). "Current and Emerging Agents for the Treatment of Hypoglycemia in Patients with Congenital Hyperinsulinism" (in en). Pediatric Drugs 21 (3): 123–136. doi:10.1007/s40272-019-00334-w. ISSN 1174-5878. PMID 31218604. http://link.springer.com/10.1007/s40272-019-00334-w.
- ↑ on behalf of the Best Pharmaceuticals for Children Act–Pediatric Trials Network Steering Committee; Gray, Keyaria D.; Dudash, Kathryn; Escobar, Carla; Freel, Colman; Harrison, Tylah; McMillan, Chandler; Puia-Dumitrescu, Mihai et al. (11 September 2018). "Prevalence and safety of diazoxide in the neonatal intensive care unit" (in en). Journal of Perinatology 38 (11): 1496–1502. doi:10.1038/s41372-018-0218-4. ISSN 0743-8346. PMID 30206345.
- ↑ 17.0 17.1 Bailey, Miranda J.; Rout, Allie; Harding, Jane E.; Alsweiler, Jane M.; Cutfield, Wayne S.; McKinlay, Christopher J. D. (5 December 2020). "Prolonged transitional neonatal hypoglycaemia: characterisation of a clinical syndrome" (in en). Journal of Perinatology 41 (5): 1149–1157. doi:10.1038/s41372-020-00891-w. ISSN 0743-8346. PMID 33279942. http://www.nature.com/articles/s41372-020-00891-w.
- ↑ Hussain, K. (2005-08-24). "Congenital hyperinsulinism" (in en). Seminars in Fetal and Neonatal Medicine 10 (4): 369–376. doi:10.1016/j.siny.2005.03.001. PMID 15916932. https://linkinghub.elsevier.com/retrieve/pii/S1744165X05000168.
- ↑ 19.0 19.1 19.2 19.3 19.4 19.5 19.6 19.7 Pagliara, Anthony S.; Karl, Irne E.; Haymond, Morey; Kipnis, David M. (April 1973). "Hypoglycemia in infancy and childhood. Part II" (in en). The Journal of Pediatrics 82 (4): 558–577. doi:10.1016/S0022-3476(73)80581-5. PMID 4349061. https://linkinghub.elsevier.com/retrieve/pii/S0022347673805815.
- ↑ 20.0 20.1 20.2 20.3 20.4 20.5 20.6 20.7 20.8 Kane, Charlotte; Shepherd, Ruth M.; Squires, Paul E.; Johnson, Paul R.V.; James, Roger F.L.; Milla, Peter J.; Aynsley-Green, Albert; Lindley, Keith J. et al. (1 December 1996). "Loss of functional KATP channels in pancreatic β–cells causes persistent hyperinsulinemic hypoglycemia of infancy" (in en). Nature Medicine 2 (12): 1344–1347. doi:10.1038/nm1296-1344. ISSN 1078-8956. PMID 8946833. http://www.nature.com/articles/nm1296-1344.
- ↑ 21.0 21.1 21.2 21.3 21.4 21.5 Stanley, Charles A.; Lieu, Yen K.; Hsu, Betty Y.L.; Burlina, Alberto B.; Greenberg, Cheryl R.; Hopwood, Nancy J.; Perlman, Kusiel; Rich, Barry H. et al. (1998-05-07). "Hyperinsulinism and Hyperammonemia in Infants with Regulatory Mutations of the Glutamate Dehydrogenase Gene" (in en). New England Journal of Medicine 338 (19): 1352–1357. doi:10.1056/NEJM199805073381904. ISSN 0028-4793. PMID 9571255.
- ↑ 22.0 22.1 22.2 Rosenfeld, Elizabeth; De León, Diva D. (2023-03-28). "Bridging the gaps: recent advances in diagnosis, care, and outcomes in congenital hyperinsulinism" (in en). Current Opinion in Pediatrics Publish Ahead of Print (4): 486–493. doi:10.1097/MOP.0000000000001243. ISSN 1040-8703. PMID 36974442. PMC 10330427. https://journals.lww.com/10.1097/MOP.0000000000001243.
- ↑ 23.0 23.1 Verkarre, V; Fournet, J C; de Lonlay, P; Gross-Morand, M S; Devillers, M; Rahier, J; Brunelle, F; Robert, J J et al. (1998-10-01). "Paternal mutation of the sulfonylurea receptor (SUR1) gene and maternal loss of 11p15 imprinted genes lead to persistent hyperinsulinism in focal adenomatous hyperplasia." (in en). Journal of Clinical Investigation 102 (7): 1286–1291. doi:10.1172/JCI4495. ISSN 0021-9738. PMID 9769320. PMC 508975. http://www.jci.org/articles/view/4495.
- ↑ 24.0 24.1 Otonkoski, Timo; Näntö-Salonen, Kirsti; Seppänen, Marko; Veijola, Riitta; Huopio, Hanna; Hussain, Khalid; Tapanainen, Päivi; Eskola, Olli et al. (January 2006). "Noninvasive diagnosis of focal hyperinsulinism of infancy with [18F]-DOPA positron emission tomography". Diabetes 55 (1): 13–18. doi:10.2337/diabetes.55.01.06.db05-1128. ISSN 0012-1797. PMID 16380471.
- ↑ Williams, A. F. (1997). "Hypoglycaemia of the newborn: a review". Bulletin of the World Health Organization 75 (3): 261–290. ISSN 0042-9686. PMID 9277014.
- ↑ Hoe, Francis M.; Thornton, Paul S.; Wanner, Laura A.; Steinkrauss, Linda; Simmons, Rebecca A.; Stanley, Charles A. (20 February 2006). "Clinical features and insulin regulation in infants with a syndrome of prolonged neonatal hyperinsulinism" (in en). The Journal of Pediatrics 148 (2): 207–212. doi:10.1016/j.jpeds.2005.10.002. PMID 16492430. https://linkinghub.elsevier.com/retrieve/pii/S0022347605009832.
- ↑ 27.0 27.1 27.2 Hewat, Thomas I.; Johnson, Matthew B.; Flanagan, Sarah E. (7 July 2022). "Congenital Hyperinsulinism: Current Laboratory-Based Approaches to the Genetic Diagnosis of a Heterogeneous Disease". Frontiers in Endocrinology 13: 873254. doi:10.3389/fendo.2022.873254. ISSN 1664-2392. PMID 35872984.
- ↑ 28.0 28.1 28.2 28.3 28.4 Stanley, Charles A. (1 March 2016). "Perspective on the Genetics and Diagnosis of Congenital Hyperinsulinism Disorders" (in en). The Journal of Clinical Endocrinology & Metabolism 101 (3): 815–826. doi:10.1210/jc.2015-3651. ISSN 0021-972X. PMID 26908106.
- ↑ Kapoor, Ritika R; Flanagan, Sarah E; Arya, Ved Bhushan; Shield, Julian P; Ellard, Sian; Hussain, Khalid (1 April 2013). "Clinical and molecular characterisation of 300 patients with congenital hyperinsulinism". European Journal of Endocrinology 168 (4): 557–564. doi:10.1530/EJE-12-0673. ISSN 0804-4643. PMID 23345197.
- ↑ Snider, K. E.; Becker, S.; Boyajian, L.; Shyng, S.-L.; MacMullen, C.; Hughes, N.; Ganapathy, K.; Bhatti, T. et al. (1 February 2013). "Genotype and Phenotype Correlations in 417 Children With Congenital Hyperinsulinism" (in en). The Journal of Clinical Endocrinology & Metabolism 98 (2): E355–E363. doi:10.1210/jc.2012-2169. ISSN 0021-972X. PMID 23275527.
- ↑ de Lonlay, P; Fournet, J C; Rahier, J; Gross-Morand, M S; Poggi-Travert, F; Foussier, V; Bonnefont, J P; Brusset, M C et al. (1997-08-15). "Somatic deletion of the imprinted 11p15 region in sporadic persistent hyperinsulinemic hypoglycemia of infancy is specific of focal adenomatous hyperplasia and endorses partial pancreatectomy." (in en). Journal of Clinical Investigation 100 (4): 802–807. doi:10.1172/JCI119594. ISSN 0021-9738. PMID 9259578. PMC 508251. http://www.jci.org/articles/view/119594.
- ↑ Banerjee, I; Skae, M; Flanagan, S E; Rigby, L; Patel, L; Didi, M; Blair, J; Ehtisham, S et al. (1 May 2011). "The contribution of rapid KATP channel gene mutation analysis to the clinical management of children with congenital hyperinsulinism". European Journal of Endocrinology 164 (5): 733–740. doi:10.1530/EJE-10-1136. ISSN 0804-4643. PMID 21378087. https://academic.oup.com/ejendo/article/164/5/733/6676807.
- ↑ Maiorana, Arianna; Lepri, Francesca Romana; Novelli, Antonio; Dionisi-Vici, Carlo (2022-03-29). "Hypoglycaemia Metabolic Gene Panel Testing". Frontiers in Endocrinology 13: 826167. doi:10.3389/fendo.2022.826167. ISSN 1664-2392. PMID 35422763.
- ↑ Pasquini, Tai L. S.; Mesfin, Mahlet; Schmitt, Jennifer; Raskin, Julie (2022-06-02). "Global Registries in Congenital Hyperinsulinism". Frontiers in Endocrinology 13: 876903. doi:10.3389/fendo.2022.876903. ISSN 1664-2392. PMID 35721728.
- ↑ Zenker, Martin; Mohnike, Klaus; Palm, Katja (2023-03-30). "Syndromic forms of congenital hyperinsulinism". Frontiers in Endocrinology 14: 1013874. doi:10.3389/fendo.2023.1013874. ISSN 1664-2392. PMID 37065762.
- ↑ Brioude, Frédéric; Kalish, Jennifer M.; Mussa, Alessandro; Foster, Alison C.; Bliek, Jet; Ferrero, Giovanni Battista; Boonen, Susanne E.; Cole, Trevor et al. (29 January 2018). "Clinical and molecular diagnosis, screening and management of Beckwith–Wiedemann syndrome: an international consensus statement" (in en). Nature Reviews Endocrinology 14 (4): 229–249. doi:10.1038/nrendo.2017.166. ISSN 1759-5029. PMID 29377879.
- ↑ Wang, Kathleen H.; Kupa, Jonida; Duffy, Kelly A.; Kalish, Jennifer M. (2020-01-21). "Diagnosis and Management of Beckwith-Wiedemann Syndrome". Frontiers in Pediatrics 7: 562. doi:10.3389/fped.2019.00562. ISSN 2296-2360. PMID 32039119.
- ↑ Kalish, Jennifer M.; Arnoux, Jean-Baptiste (2019), De León-Crutchlow, Diva D.; Stanley, Charles A., eds., "Syndromic Causes of Congenital Hyperinsulinism", Congenital Hyperinsulinism, Contemporary Endocrinology (Cham: Springer International Publishing): pp. 49–59, doi:10.1007/978-3-030-02961-6_4, ISBN 978-3-030-02960-9, http://link.springer.com/10.1007/978-3-030-02961-6_4, retrieved 2023-05-08
- ↑ Bier, Dennis M; Leake, Rosemary D; Haymond, Morey W; Arnold, Kenneth J; Gruenke, Larry D; Sperling, Mark A; Kipnis, David M (1977-11-01). "Measurement of "True" Glucose Production Rates in Infancy and Childhood with 6,6-Dideuteroglucose" (in en). Diabetes 26 (11): 1016–1023. doi:10.2337/diab.26.11.1016. ISSN 0012-1797. PMID 913891. https://diabetesjournals.org/diabetes/article/26/11/1016/4344/Measurement-of-True-Glucose-Production-Rates-in.
- ↑ Palladino, Andrew A; Bennett, Michael J; Stanley, Charles A (2008-02-01). "Hyperinsulinism in Infancy and Childhood: When an Insulin Level Is Not Always Enough" (in en). Clinical Chemistry 54 (2): 256–263. doi:10.1373/clinchem.2007.098988. ISSN 0009-9147. PMID 18156285.
- ↑ Ferrara, Christine; Patel, Payal; Becker, Susan; Stanley, Charles A.; Kelly, Andrea (17 October 2015). "Biomarkers of Insulin for the Diagnosis of Hyperinsulinemic Hypoglycemia in Infants and Children" (in en). The Journal of Pediatrics 168: 212–219. doi:10.1016/j.jpeds.2015.09.045. PMID 26490124. https://linkinghub.elsevier.com/retrieve/pii/S0022347615010586.
- ↑ Sakakibara, Azumi; Hashimoto, Yukiko; Kawakita, Rie; Hosokawa, Yuki; Nagahara, Keiko; Hasegawa, Yukihiro; Hoshino, Shin; Nagasaka, Hironori et al. (9 June 2017). "Diagnosis of congenital hyperinsulinism: Biochemical profiles during hypoglycemia" (in en). Pediatric Diabetes 19 (2): 259–264. doi:10.1111/pedi.12548. PMID 28597971.
- ↑ Palladino, Andrew A.; Stanley, Charles A. (9 October 2010). "The hyperinsulinism/hyperammonemia syndrome" (in en). Reviews in Endocrine and Metabolic Disorders 11 (3): 171–178. doi:10.1007/s11154-010-9146-0. ISSN 1389-9155. PMID 20936362. http://link.springer.com/10.1007/s11154-010-9146-0.
- ↑ Zhang, Wei; Sang, Yan-Mei (4 November 2021). "Genetic pathogenesis, diagnosis, and treatment of short-chain 3-hydroxyacyl-coenzyme A dehydrogenase hyperinsulinism" (in en). Orphanet Journal of Rare Diseases 16 (1): 467. doi:10.1186/s13023-021-02088-6. ISSN 1750-1172. PMID 34736508.
- ↑ Kelly, Andrea; Ng, Diva; Ferry, Robert J.; Grimberg, Adda; Koo-McCoy, Samantha; Thornton, Paul S.; Stanley, Charles A. (2001-08-01). "Acute Insulin Responses to Leucine in Children with the Hyperinsulinism/Hyperammonemia Syndrome" (in en). The Journal of Clinical Endocrinology & Metabolism 86 (8): 3724–3728. doi:10.1210/jcem.86.8.7755. ISSN 0021-972X. PMID 11502802.
- ↑ Fourtner, Shannon H.; Stanley, Charles A.; Kelly, Andrea (July 2006). "Protein-sensitive hypoglycemia without leucine sensitivity in hyperinsulinism caused by KATP channel mutations" (in en). The Journal of Pediatrics 149 (1): 47–52. doi:10.1016/j.jpeds.2006.02.033. PMID 16860127. https://linkinghub.elsevier.com/retrieve/pii/S0022347606001296.
- ↑ Glaser, Benjamin (1 January 1993). "Familial Hyperinsulinism". GeneReviews. PMID 20301549. https://www.ncbi.nlm.nih.gov/books/NBK1375/. Retrieved 9 October 2016.update 2013
- ↑ 48.0 48.1 48.2 48.3 Yorifuji, Tohru (28 November 2016). "Congenital hyperinsulinism: current status and future perspectives". Annals of Pediatric Endocrinology & Metabolism 19 (2): 57–68. doi:10.6065/apem.2014.19.2.57. ISSN 2287-1012. PMID 25077087.
- ↑ Brar, Preneet Cheema; Heksch, Ryan; Cossen, Kristina; De Leon, Diva D; Kamboj, Manmohan K; Marks, Seth D; Marshall, Bess A; Miller, Ryan et al. (2020-12-01). "Management and Appropriate Use of Diazoxide in Infants and Children with Hyperinsulinism" (in en). The Journal of Clinical Endocrinology & Metabolism 105 (12): 3750–3761. doi:10.1210/clinem/dgaa543. ISSN 0021-972X. PMID 32810255.
- ↑ Snider, K. E.; Becker, S.; Boyajian, L.; Shyng, S.-L.; MacMullen, C.; Hughes, N.; Ganapathy, K.; Bhatti, T. et al. (1 February 2013). "Genotype and Phenotype Correlations in 417 Children With Congenital Hyperinsulinism" (in en). The Journal of Clinical Endocrinology & Metabolism 98 (2): E355–E363. doi:10.1210/jc.2012-2169. ISSN 0021-972X. PMID 23275527.
- ↑ States, Lisa J.; Saade-Lemus, Sandra; De Leon, Diva D. (July 2020). "18-F-L 3,4-Dihydroxyphenylalanine PET/Computed Tomography in the Management of Congenital Hyperinsulinism" (in en). PET Clinics 15 (3): 349–359. doi:10.1016/j.cpet.2020.03.004. PMID 32498990. https://linkinghub.elsevier.com/retrieve/pii/S155685982030016X.
- ↑ 52.0 52.1 Welters, Alena; Lerch, Christian; Kummer, Sebastian; Marquard, Jan; Salgin, Burak; Mayatepek, Ertan; Meissner, Thomas (25 November 2015). "Long-term medical treatment in congenital hyperinsulinism: a descriptive analysis in a large cohort of patients from different clinical centers" (in en). Orphanet Journal of Rare Diseases 10 (1): 150. doi:10.1186/s13023-015-0367-x. ISSN 1750-1172. PMID 26608306.
- ↑ McMahon, Ann W.; Wharton, Gerold T.; Thornton, Paul; De Leon, Diva D. (2 December 2016). "Octreotide use and safety in infants with hyperinsulinism: Octreotide Use and Safety" (in en). Pharmacoepidemiology and Drug Safety 26 (1): 26–31. doi:10.1002/pds.4144. PMID 27910218.
- ↑ Vajravelu, Mary Ellen; Congdon, Morgan; Mitteer, Lauren; Koh, Jamie; Givler, Stephanie; Shults, Justine; De León, Diva D. (7 August 2018). "Continuous Intragastric Dextrose: A Therapeutic Option for Refractory Hypoglycemia in Congenital Hyperinsulinism" (in en). Hormone Research in Paediatrics 91 (1): 62–68. doi:10.1159/000491105. ISSN 1663-2818. PMID 30086540. PMC 6661174. https://www.karger.com/Article/FullText/491105.
- ↑ Avatapalle, B.; Padidela, R.; Randell, T.; Banerjee, I. (2012-07-30). "Drug-induced hepatitis following use of octreotide for long-term treatment of congenital hyperinsulinism" (in en). Case Reports 2012 (jul30 1): bcr2012006271. doi:10.1136/bcr-2012-006271. ISSN 1757-790X. PMID 22850563.
- ↑ Cuff, Heather; Lord, Katherine; Ballester, Lance; Scully, Tryce; Stewart, Nicole; De Leon, Diva D (2022-07-14). "The Use of Lanreotide in the Treatment of Congenital Hyperinsulinism" (in en). The Journal of Clinical Endocrinology & Metabolism 107 (8): e3115–e3120. doi:10.1210/clinem/dgac322. ISSN 0021-972X. PMID 35587448. https://academic.oup.com/jcem/article/107/8/e3115/6589462.
- ↑ Herrera, Adriana; Vajravelu, Mary Ellen; Givler, Stephanie; Mitteer, Lauren; Avitabile, Catherine M; Lord, Katherine; De León, Diva D (2018-12-01). "Prevalence of Adverse Events in Children With Congenital Hyperinsulinism Treated With Diazoxide" (in en). The Journal of Clinical Endocrinology & Metabolism 103 (12): 4365–4372. doi:10.1210/jc.2018-01613. ISSN 0021-972X. PMID 30247666.
- ↑ Thornton, Paul; Truong, Lisa; Reynolds, Courtney; Hamby, Tyler; Nedrelow, Jonathan (19 March 2019). "Rate of Serious Adverse Events Associated with Diazoxide Treatment of Patients with Hyperinsulinism" (in en). Hormone Research in Paediatrics 91 (1): 25–32. doi:10.1159/000497458. ISSN 1663-2818. PMID 30889588. https://www.karger.com/Article/FullText/497458.
- ↑ Beltrand, Jacques; Caquard, Marylène; Arnoux, Jean-Baptiste; Laborde, Kathleen; Velho, Gilberto; Verkarre, Virginie; Rahier, Jacques; Brunelle, Francis et al. (2012-02-01). "Glucose Metabolism in 105 Children and Adolescents After Pancreatectomy for Congenital Hyperinsulinism" (in en). Diabetes Care 35 (2): 198–203. doi:10.2337/dc11-1296. ISSN 0149-5992. PMID 22190679. PMC 3263917. https://diabetesjournals.org/care/article/35/2/198/38450/Glucose-Metabolism-in-105-Children-and-Adolescents.
- ↑ Meissner, T; Wendel, U; Burgard, P; Schaetzle, S; Mayatepek, E (2003-07-01). "Long-term follow-up of 114 patients with congenital hyperinsulinism". European Journal of Endocrinology 149 (1): 43–51. doi:10.1530/eje.0.1490043. ISSN 0804-4643. PMID 12824865.
- ↑ Menni, Francesca; de Lonlay, Pascale; Sevin, Caroline; Touati, Guy; Peigné, Catherine; Barbier, Valérie; Nihoul-Fékété, Claire; Saudubray, Jean-Marie et al. (2001-03-01). "Neurologic Outcomes of 90 Neonates and Infants With Persistent Hyperinsulinemic Hypoglycemia" (in en). Pediatrics 107 (3): 476–479. doi:10.1542/peds.107.3.476. ISSN 1098-4275. PMID 11230585. https://publications.aap.org/pediatrics/article/107/3/476/66041/Neurologic-Outcomes-of-90-Neonates-and-Infants.
- ↑ Yau, Daphne; Laver, Thomas W.; Dastamani, Antonia; Senniappan, Senthil; Houghton, Jayne A. L.; Shaikh, Guftar; Cheetham, Tim; Mushtaq, Talat et al. (2020-02-06). Brusgaard, Klaus. ed. "Using referral rates for genetic testing to determine the incidence of a rare disease: The minimal incidence of congenital hyperinsulinism in the UK is 1 in 28,389" (in en). PLOS ONE 15 (2): e0228417. doi:10.1371/journal.pone.0228417. ISSN 1932-6203. PMID 32027664. Bibcode: 2020PLoSO..1528417Y.
- ↑ 63.0 63.1 Männistö, Jonna M E; Jääskeläinen, Jarmo; Otonkoski, Timo; Huopio, Hanna (2021-03-25). "Long-Term Outcome and Treatment in Persistent and Transient Congenital Hyperinsulinism: A Finnish Population-Based Study" (in en). The Journal of Clinical Endocrinology & Metabolism 106 (4): 1542–1551. doi:10.1210/clinem/dgab024. ISSN 0021-972X. PMID 33475139.
- ↑ Banerjee, I; Skae, M; Flanagan, S E; Rigby, L; Patel, L; Didi, M; Blair, J; Ehtisham, S et al. (1 May 2011). "The contribution of rapid KATP channel gene mutation analysis to the clinical management of children with congenital hyperinsulinism". European Journal of Endocrinology 164 (5): 733–740. doi:10.1530/EJE-10-1136. ISSN 0804-4643. PMID 21378087. https://academic.oup.com/ejendo/article/164/5/733/6676807.
- ↑ Mazor-Aronovitch, K; Gillis, D; Lobel, D; Hirsch, H J; Pinhas-Hamiel, O; Modan-Moses, D; Glaser, B; Landau, H (1 October 2007). "Long-term neurodevelopmental outcome in conservatively treated congenital hyperinsulinism". European Journal of Endocrinology 157 (4): 491–497. doi:10.1530/EJE-07-0445. ISSN 0804-4643. PMID 17893264.
- ↑ Salomon-Estebanez, Maria; Flanagan, Sarah E.; Ellard, Sian; Rigby, Lindsey; Bowden, Louise; Mohamed, Zainab; Nicholson, Jacqueline; Skae, Mars et al. (1 December 2016). "Conservatively treated Congenital Hyperinsulinism (CHI) due to K-ATP channel gene mutations: reducing severity over time" (in en). Orphanet Journal of Rare Diseases 11 (1): 163. doi:10.1186/s13023-016-0547-3. ISSN 1750-1172. PMID 27908292.
- ↑ Flanagan, Se; Kapoor, Rr; Banerjee, I; Hall, C; Smith, Vv; Hussain, K; Ellard, S (5 May 2011). "Dominantly acting ABCC8 mutations in patients with medically unresponsive hyperinsulinaemic hypoglycaemia" (in en). Clinical Genetics 79 (6): 582–587. doi:10.1111/j.1399-0004.2010.01476.x. ISSN 0009-9163. PMID 20573158.
- ↑ Pinney, Sara E.; MacMullen, Courtney; Becker, Susan; Lin, Yu-Wen; Hanna, Cheryl; Thornton, Paul; Ganguly, Arupa; Shyng, Show-Ling et al. (2008-08-01). "Clinical characteristics and biochemical mechanisms of congenital hyperinsulinism associated with dominant KATP channel mutations" (in en). Journal of Clinical Investigation 118 (8): 2877–2886. doi:10.1172/JCI35414. ISSN 0021-9738. PMID 18596924. PMC 2441858. http://www.jci.org/articles/view/35414.
- ↑ Kapoor, R. R.; Flanagan, S. E.; James, C. T.; McKiernan, J.; Thomas, A. M.; Harmer, S. C.; Shield, J. P.; Tinker, A. et al. (15 June 2011). "Hyperinsulinaemic hypoglycaemia and diabetes mellitus due to dominant ABCC8/KCNJ11 mutations" (in en). Diabetologia 54 (10): 2575–2583. doi:10.1007/s00125-011-2207-4. ISSN 0012-186X. PMID 21674179.
- ↑ McGlacken-Byrne, Sinéad M; Mohammad, Jasmina Kallefullah; Conlon, Niamh; Gubaeva, Diliara; Siersbæk, Julie; Schou, Anders Jørgen; Demirbilek, Huseyin; Dastamani, Antonia et al. (2022-04-01). "Clinical and genetic heterogeneity of HNF4A/HNF1A mutations in a multicentre paediatric cohort with hyperinsulinaemic hypoglycaemia". European Journal of Endocrinology 186 (4): 417–427. doi:10.1530/EJE-21-0897. ISSN 0804-4643. PMID 35089870. https://academic.oup.com/ejendo/article/186/4/417/6852977.
- ↑ Yau, Daphne; Colclough, Kevin; Natarajan, Anuja; Parikh, Ruchi; Canham, Natalie; Didi, Mohammed; Senniappan, Senthil; Banerjee, Indraneel (20 April 2020). "Congenital hyperinsulinism due to mutations in HNF1A" (in en). European Journal of Medical Genetics 63 (6): 103928. doi:10.1016/j.ejmg.2020.103928. PMID 32325224. https://linkinghub.elsevier.com/retrieve/pii/S1769721219305038.
- ↑ 72.0 72.1 72.2 72.3 Pasquini, Tai L. S.; Mesfin, Mahlet; Schmitt, Jennifer; Raskin, Julie (2022-06-02). "Global Registries in Congenital Hyperinsulinism". Frontiers in Endocrinology 13: 876903. doi:10.3389/fendo.2022.876903. ISSN 1664-2392. PMID 35721728.
- ↑ Banerjee, Indraneel; Forsythe, Lynette; Skae, Mars; Avatapalle, Hima Bindu; Rigby, Lindsey; Bowden, Louise E.; Craigie, Ross; Padidela, Raja et al. (2016-02-09). "Feeding Problems Are Persistent in Children with Severe Congenital Hyperinsulinism". Frontiers in Endocrinology 7: 8. doi:10.3389/fendo.2016.00008. ISSN 1664-2392. PMID 26903946.
- ↑ Worth, Chris; Hall, Caroline; Wilson, Sarah; Gilligan, Niamh; O'Shea, Elaine; Salomon-Estebanez, Maria; Dunne, Mark; Banerjee, Indraneel (2020-03-18). "Delayed Resolution of Feeding Problems in Patients With Congenital Hyperinsulinism". Frontiers in Endocrinology 11: 143. doi:10.3389/fendo.2020.00143. ISSN 1664-2392. PMID 32256453.
- ↑ Chen, Suet Ching; Dastamani, Antonia; Pintus, Donatella; Yau, Daphne; Aftab, Sommayya; Bath, Louise; Swinburne, Craig; Hunter, Lindsey et al. (14 September 2019). "Diazoxide‐induced pulmonary hypertension in hyperinsulinaemic hypoglycaemia: Recommendations from a multicentre study in the United Kingdom" (in en). Clinical Endocrinology 91 (6): 770–775. doi:10.1111/cen.14096. ISSN 0300-0664. PMID 31520536. https://onlinelibrary.wiley.com/doi/10.1111/cen.14096.
- ↑ Herrera, Adriana; Vajravelu, Mary Ellen; Givler, Stephanie; Mitteer, Lauren; Avitabile, Catherine M; Lord, Katherine; De León, Diva D (2018-12-01). "Prevalence of Adverse Events in Children With Congenital Hyperinsulinism Treated With Diazoxide" (in en). The Journal of Clinical Endocrinology & Metabolism 103 (12): 4365–4372. doi:10.1210/jc.2018-01613. ISSN 0021-972X. PMID 30247666.
- ↑ Beltrand, Jacques; Caquard, Marylène; Arnoux, Jean-Baptiste; Laborde, Kathleen; Velho, Gilberto; Verkarre, Virginie; Rahier, Jacques; Brunelle, Francis et al. (2012-02-01). "Glucose Metabolism in 105 Children and Adolescents After Pancreatectomy for Congenital Hyperinsulinism" (in en). Diabetes Care 35 (2): 198–203. doi:10.2337/dc11-1296. ISSN 0149-5992. PMID 22190679. PMC 3263917. https://diabetesjournals.org/care/article/35/2/198/38450/Glucose-Metabolism-in-105-Children-and-Adolescents.
- ↑ Arya, Ved Bhushan; Senniappan, Senthil; Demirbilek, Huseyin; Alam, Syeda; Flanagan, Sarah E.; Ellard, Sian; Hussain, Khalid (2014-05-19). Brusgaard, Klaus. ed. "Pancreatic Endocrine and Exocrine Function in Children following Near-Total Pancreatectomy for Diffuse Congenital Hyperinsulinism" (in en). PLOS ONE 9 (5): e98054. doi:10.1371/journal.pone.0098054. ISSN 1932-6203. PMID 24840042. Bibcode: 2014PLoSO...998054A.
- ↑ 79.0 79.1 79.2 79.3 Thornton, Paul S.; Stanley, Charles A.; De Leon, Diva D. (2022). "Congenital Hyperinsulinism: An Historical Perspective" (in en). Hormone Research in Paediatrics 95 (6): 631–637. doi:10.1159/000526442. ISSN 1663-2818. PMID 36446321. https://www.karger.com/Article/FullText/526442.
- ↑ Stanley, C. A.; Baker, L. (1976). "Hyperinsulinism in infants and children: diagnosis and therapy". Advances in Pediatrics 23: 315–355. doi:10.1016/S0065-3101(22)00724-1. ISSN 0065-3101. PMID 795282. https://pubmed.ncbi.nlm.nih.gov/795282.
- ↑ Pagliara, Anthony S.; Karl, Irene E.; Haymond, Morey; Kipnis, David M. (March 1973). "Hypoglycemia in infancy and childhood. Part I" (in en). The Journal of Pediatrics 82 (3): 365–379. doi:10.1016/S0022-3476(73)80109-X. PMID 4572931. https://linkinghub.elsevier.com/retrieve/pii/S002234767380109X.
- ↑ Pagliara, Anthony S.; Karl, Irne E.; Haymond, Morey; Kipnis, David M. (April 1973). "Hypoglycemia in infancy and childhood. Part II" (in en). The Journal of Pediatrics 82 (4): 558–577. doi:10.1016/S0022-3476(73)80581-5. PMID 4349061. https://linkinghub.elsevier.com/retrieve/pii/S0022347673805815.
- ↑ Kane, Charlotte; Shepherd, Ruth M.; Squires, Paul E.; Johnson, Paul R.V.; James, Roger F.L.; Milla, Peter J.; Aynsley-Green, Albert; Lindley, Keith J. et al. (1 December 1996). "Loss of functional KATP channels in pancreatic β–cells causes persistent hyperinsulinemic hypoglycemia of infancy" (in en). Nature Medicine 2 (12): 1344–1347. doi:10.1038/nm1296-1344. ISSN 1078-8956. PMID 8946833. http://www.nature.com/articles/nm1296-1344.
- ↑ Dunne, Mark J.; Kane, Charlotte; Shepherd, Ruth M.; Sanchez, Jorge A.; James, Roger F.L.; Johnson, Paul R.V.; Aynsley-Green, Albert; Lu, Shan et al. (1997-03-06). "Familial Persistent Hyperinsulinemic Hypoglycemia of Infancy and Mutations in the Sulfonylurea Receptor" (in en). New England Journal of Medicine 336 (10): 703–706. doi:10.1056/NEJM199703063361005. ISSN 0028-4793. PMID 9041101. http://www.nejm.org/doi/abs/10.1056/NEJM199703063361005.
- ↑ Glaser, Benjamin; Kesavan, Prebakaran; Heyman, Mozhgan; Davis, Elizabeth; Cuesta, Antonio; Buchs, Andreas; Stanley, Charles A.; Thornton, Paul S. et al. (1998-01-22). "Familial Hyperinsulinism Caused by an Activating Glucokinase Mutation" (in en). New England Journal of Medicine 338 (4): 226–230. doi:10.1056/NEJM199801223380404. ISSN 0028-4793. PMID 9435328.
- ↑ Stanley, Charles A.; Lieu, Yen K.; Hsu, Betty Y.L.; Burlina, Alberto B.; Greenberg, Cheryl R.; Hopwood, Nancy J.; Perlman, Kusiel; Rich, Barry H. et al. (1998-05-07). "Hyperinsulinism and Hyperammonemia in Infants with Regulatory Mutations of the Glutamate Dehydrogenase Gene" (in en). New England Journal of Medicine 338 (19): 1352–1357. doi:10.1056/NEJM199805073381904. ISSN 0028-4793. PMID 9571255.
- ↑ Rosenfeld, Elizabeth; De León, Diva D. (2023-03-28). "Bridging the gaps: recent advances in diagnosis, care, and outcomes in congenital hyperinsulinism" (in en). Current Opinion in Pediatrics Publish Ahead of Print (4): 486–493. doi:10.1097/MOP.0000000000001243. ISSN 1040-8703. PMID 36974442. PMC 10330427. https://journals.lww.com/10.1097/MOP.0000000000001243.
- ↑ Hewat, Thomas I.; Johnson, Matthew B.; Flanagan, Sarah E. (7 July 2022). "Congenital Hyperinsulinism: Current Laboratory-Based Approaches to the Genetic Diagnosis of a Heterogeneous Disease". Frontiers in Endocrinology 13: 873254. doi:10.3389/fendo.2022.873254. ISSN 1664-2392. PMID 35872984.
- ↑ Verkarre, V; Fournet, J C; de Lonlay, P; Gross-Morand, M S; Devillers, M; Rahier, J; Brunelle, F; Robert, J J et al. (1998-10-01). "Paternal mutation of the sulfonylurea receptor (SUR1) gene and maternal loss of 11p15 imprinted genes lead to persistent hyperinsulinism in focal adenomatous hyperplasia." (in en). Journal of Clinical Investigation 102 (7): 1286–1291. doi:10.1172/JCI4495. ISSN 0021-9738. PMID 9769320. PMC 508975. http://www.jci.org/articles/view/4495.
- ↑ Otonkoski, Timo; Näntö-Salonen, Kirsti; Seppänen, Marko; Veijola, Riitta; Huopio, Hanna; Hussain, Khalid; Tapanainen, Päivi; Eskola, Olli et al. (January 2006). "Noninvasive diagnosis of focal hyperinsulinism of infancy with [18F]-DOPA positron emission tomography". Diabetes 55 (1): 13–18. doi:10.2337/diabetes.55.01.06.db05-1128. ISSN 0012-1797. PMID 16380471.
- ↑ 91.0 91.1 Raskin, Julie; Pasquini, Tai L. S.; Bose, Sheila; Tallis, Dina; Schmitt, Jennifer (2022). "Congenital Hyperinsulinism International: A Community Focused on Improving the Lives of People Living With Congenital Hyperinsulinism". Frontiers in Endocrinology 13: 886552. doi:10.3389/fendo.2022.886552. ISSN 1664-2392. PMID 35573986.
- ↑ Ng, Sze May; Dearman, Sarah; Fisher, Mark; Mushtaq, Talat; Randell, Tabitha (2023-02-09). "Paediatric Society and Hyperinsulinism Charity National Surveys on CGM Access for Patients With Recurrent Hypoglycaemia". Journal of the Endocrine Society 7 (4): bvad021. doi:10.1210/jendso/bvad021. ISSN 2472-1972. PMID 36824585.
- ↑ "Lobby4kids". https://lobby4kids.at/.
- ↑ "Hiperinsulismo Congénito Hicongenito". http://www.hicongenito.com.ar/.
- ↑ "HiC - Hiperinsulinismo Congênito" (in en). https://www.facebook.com/hiperinsulinismocongenito.hic/.
- ↑ "Association des Hyperinsulinismes" (in fr). http://www.hyperinsulinisme.com/.
- ↑ "Kongenitaler Hyperinsulinismus e.V.". https://hyperinsulinismus.de/.
- ↑ "Vivere con C.H.I. - Vivere con C.H.I. Iperinsulinismo congenito" (in it-IT). https://www.iperinsulinismo.org/.
- ↑ "Hiperinsulinismo Congénito". https://hiperinsulinismocongenito.org/.
- ↑ "KoHHA-DER – Konjenital Hiperinsülinizmli Hasta Aileleri Derneği" (in tr). https://kohhader.org/.
- ↑ "Children's Hyperinsulinism Charity". https://www.hyperinsulinism.co.uk/.
- ↑ "HI Global Registry". https://www.higlobalregistry.org/.
- ↑ "The CHI Centers of Excellence (COE) Program" (in en-US). https://congenitalhi.org/the-chi-centers-of-excellence-coe-program/.
- ↑ "Cook Children's Hyperinsulinism Center Named a Center of Excellence" (in en-us). https://www.checkupnewsroom.com/cook-childrens-hyperinsulinism-center-named-a-center-of-excellence/.
- ↑ "The CHI Centers of Excellence (COE) Program" (in en-US). https://congenitalhi.org/the-chi-centers-of-excellence-coe-program/.
- ↑ "Congenital Hyperinsulinism Center". 2014-05-05. https://www.chop.edu/centers-programs/congenital-hyperinsulinism-center.
- ↑ "Hyperinsulinism Center" (in en). https://www.cookchildrens.org/services/endocrinology/specialty-programs/hyperinsulinism-center/.
- ↑ "Congenital Hyperinsulinism" (in en-GB). https://www.gosh.nhs.uk/wards-and-departments/departments/clinical-specialties/endocrinology-information/conditions-we-treat/congenital-hyperinsulinism-chi/.
- ↑ "Zentrum für kongenitalen Hyperinsulinismus, angeborene Hypoglykämieerkrankungen und seltene Diabetesformen (ZHHD)" (in de). https://www.uniklinik-duesseldorf.de/patienten-besucher/klinikeninstitutezentren/zentrum-fuer-seltene-erkrankungen/behandlungszentren/zentrum-fuer-kongenitalen-hyperinsulinismus-angeborene-hypoglykaemieerkrankungen-und-seltene-diabetesformen-zhhd.
- ↑ "Zentrum für Congenitalen Hyperinsulinismus (COACH)". http://www.mkse.ovgu.de/COACH.html.
- ↑ "Northern Congenital Hyperinsulinism (NORCHI)". https://norchi.nhs.uk/.
Further reading
- Hoyme, Louanne Hudgins; Toriello, Helga V.; Enns, Gregory M.; Hoyme, H. Eugene (2014) (in en). Signs and symptoms of genetic disease : a handbook. Oxford: Oxford University Press. ISBN 9780199930975. https://books.google.com/books?id=h-J_AwAAQBAJ&q=Congenital+hyperinsulinism+signs&pg=PA260.
- (in en) Care of the newborn a handbook for primary care. Philadelphia: Lippincott Williams & Wilkins. 2005. ISBN 9780781755856. https://books.google.com/books?id=bjdK9__HCV4C&q=Congenital+hyperinsulinism+signs&pg=PA56.
External links
- Hyperinsulinism Genes. Information on the genetic mechanisms of CHI.
- Congenital Hyperinsulinism International. Nonprofit providing information and resources.
| Classification | |
|---|---|
| External resources |
| Scholia has a topic profile for Congenital hyperinsulinism. |
Template:Disease of the pancreas and glucose metabolism
 |

