Medicine:Grandiose delusions
| Grandiose delusions | |
|---|---|
| Other names | Expansive delusions, delusions of grandeur |
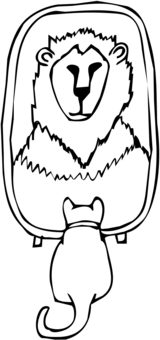 | |
| People with grandiose delusions wrongly hold themselves at an extraordinarily high status in their mind. | |
| Specialty | Psychiatry |
Grandiose delusions (GD), also known as delusions of grandeur or expansive delusions, and also informally known in Japan as eighth-grade syndrome or chūnibyō,[1] are a subtype of delusion that occur in patients with a wide range of psychiatric disorders, including two-thirds of patients in a manic state of bipolar disorder, half of those with schizophrenia, patients with the grandiose subtype of delusional disorder, frequently as a comorbid condition in narcissistic personality disorder, and a substantial portion of those with substance abuse disorders.[2][3] GDs are characterized by fantastical beliefs that one is famous, omnipotent, wealthy, or otherwise very powerful. The delusions are generally fantastic and typically have a religious, science fictional, or supernatural theme. There is a relative lack of research into GD, in contrast to persecutory delusions and auditory hallucinations. Around 10% of healthy people experience grandiose thoughts at some point in their lives but do not meet full criteria for a diagnosis of GD.[3]
While similarly named and sharing some features in common, grandiose delusions are distinct from grandiosity. While GDs refer to beliefs about nonexistent fame, wealth, powers, or religious and historical relevance, grandiosity refers to feelings of superiority, uniqueness, importance or invulnerability, and is best understood as a form of self-regard.
Signs and symptoms
According to the DSM-IV-TR diagnostic criteria for delusional disorders, grandiose-type symptoms include exaggerated beliefs of:
For example, a patient who has fictitious beliefs about their power or authority may believe themselves to be a ruling monarch who deserves to be treated like royalty.[6] There are substantial differences in the degree of grandiosity linked with grandiose delusions in different patients. Some patients believe they are God, the Queen of the United Kingdom, a president's son, a famous rock star, and some other examples. Others are not as expansive and think they are skilled athletes or great inventors.[7]
Expansive delusions may be maintained by auditory hallucinations, which advise the patient that they are significant, or confabulations, when, for example, the patient gives a thorough description of their coronation or marriage to the king. Grandiose and expansive delusions may also be part of fantastic hallucinosis in which all forms of hallucinations occur.[7]
Positive functions
Grandiose delusions frequently serve a very positive function by sustaining or increasing the patient's self-esteem. As a result, it is essential to consider the consequences of removing the grandiose delusion on self-esteem when trying to modify the grandiose delusion in therapy.[4] In many instances of grandiosity, it is suitable to go for a fractional rather than a total modification, which permits those elements of the delusion that are central for self-esteem to be preserved. For example, a person who believes they are a senior secret service agent gains a great sense of self-esteem and purpose from this belief, thus until this sense of self-esteem can be provided from elsewhere, it is best not to attempt modification.[4]
In a case study of more than 13,000 non-clinical and almost 3000 clinical participants, Isham et al.[8] found that the primary sources of meaning derived from grandiose delusions were:[8]
- Confidence in the self
- Overcoming adversity
- The "greater good"
- Happiness
- Supporting loved ones
- Positive social perception
- Spirituality
Comorbidity
Schizophrenia
Schizophrenia is a mental disorder distinguished by a loss of contact with reality and the occurrence of psychotic behaviors, including hallucinations and delusions (unreal beliefs which endure even when there is contrary evidence).[9] Delusions may include the false and constant idea that the person is being followed or poisoned, or that the person’s thoughts are being broadcast for others to listen to. Delusions in schizophrenia often develop as a response to the individual attempting to explain their hallucinations.[9] Patients who experience recurrent auditory hallucinations can develop the delusion that other people are scheming against them and are dishonest when they say they do not hear the voices that the delusional person believes that he or she hears.[9]
Specifically, grandiose delusions are frequently found in paranoid schizophrenia, in which a person has an extremely exaggerated sense of their significance, personality, knowledge, or authority. For example, the person may declare to own a major corporation and kindly offer to write a hospital staff member a check for $5 million if only help them escape from the hospital.[10] Other common grandiose delusions in schizophrenia include religious delusions such as the belief that one is Jesus Christ,[11] or the Mahdi of End time in Muslim societies.[12]
Bipolar disorder
Bipolar 1 disorder can lead to severe affective dysregulation, or mood states that sway from exceedingly low (depression) to exceptionally high (mania).[13] In hypomania or mania, some bipolar patients can have grandiose delusions. In its most severe manifestation, days without sleep, auditory and other hallucinations, or uncontrollable racing thoughts can reinforce these delusions. In mania, this illness affects emotions and can also lead to impulsivity and disorganized thinking, which can be harnessed to increase their sense of grandiosity. Protecting this delusion can also lead to extreme irritability, paranoia, and fear. Sometimes their anxiety can be so over-blown that they believe others are jealous of them and, thus, undermine their "extraordinary abilities," persecuting them or even scheming to seize what they already have.[14]
The vast majority of bipolar patients rarely experience delusions. Typically, when experiencing or displaying a stage of heightened excitability called mania, they can experience joy, rage, and other intense emotions that can cycle out of control, along with thoughts or beliefs that are grandiose. Some of these grandiose thoughts can be expressed as strong beliefs that the patient is very rich or famous or has super-human abilities, or can even lead to severe suicidal ideations.[15] In the most severe form, in what was formerly labeled as megalomania, the bipolar patient may hear voices that support these grandiose beliefs. In their delusions, they can believe that they are, for example, a king, a creative genius, or can even exterminate the world's poverty because of their extreme generosity.[16]
Theories and mechanisms
Psychologists and psychiatrists have proposed multiple theoretical accounts of GDs:[17]
- Delusion-as-defense: defense of the mind against lower self-esteem and depression.
- Emotion-consistent: result of exaggerated positive emotions.
Empirical evidence largely supports emotion-consistent models, but also suggests additional factors like reasoning biases.[18] Grandiose delusions are usually associated with high self-esteem and self-serving attributional style and low levels of depression, anxiety and negative self-evaluation.[8][17][19][20] Moreover, there is evidence from neurotypical persons that repetitive positive self-thinking can confer temporary increases in (non-delusional) grandiose ideas of own superiority, importance or uniqueness.[21] A functional magnetic resonance imaging (fMRI) study of patients with bipolar disorder found that such thinking is associated with exaggerated connectivity between the medial prefrontal cortex and anterior cingulate cortex (brain regions involved in self-relevant information-processing).[22]
Qualitative research likewise indicates that grandiose delusions, far from occurring against a backdrop of negative self-evaluation, conferred a sense of uniqueness, purpose, and belonging, and added meaning to adverse events.[23]
The defensive hypothesis bears a strong similarity to the psychodynamic mask model of non-delusional narcissistic grandiosity,[24] which is also unsupported by the evidence.[25][26]
Neurobiology
Grandiose delusions may be related to lesions of the frontal lobe.[27] Temporal lobe lesions have been mainly reported in patients with delusions of persecution and of guilt, while frontal and frontotemporal involvement have been described in patients with grandiose delusions, Cotard’s syndrome, and delusional misidentification syndrome.[28]
Some studies indicate that GDs are associated with abnormalities in dopaminergic reward pathways and other limbic structures associated with reward and emotion processing.[29][30] GDs seem to be related to impaired connectivity between the left middle temporal gyrus and more dorsal regions of the left temporal lobe, regions forming a central hub of the default mode network and mediating a variety of cognitive functions (namely social and linguistic ones).[31]
Diagnosis
Patients with a wide range of mental disorders which disturb brain function experience different kinds of delusions, including grandiose delusions.[32] Grandiose delusions usually occur in patients with syndromes associated with secondary mania, such as Huntington's disease,[33] Parkinson's disease,[34] and Wilson's disease.[35] Secondary mania has also been caused by substances such as L-DOPA and isoniazid which modify the monoaminergic neurotransmitter function.[36] Vitamin B12 deficiency,[37] uremia,[38] hyperthyroidism[39] as well as the carcinoid syndrome[40] have been found to cause secondary mania, and thus grandiose delusions.
In diagnosing delusions, the MacArthur-Maudsley Assessment of Delusions Schedule is used to assess the patient.[41]
Treatment
In patients with schizophrenia, grandiose and religious delusions are found to be the least susceptible to cognitive behavioral interventions.[41] Cognitive behavioral intervention is a form of psychological therapy, initially used for depression,[42] but currently used for a variety of different mental disorders, in hope of providing relief from distress and disability.[43] During therapy, grandiose delusions were linked to patients' underlying beliefs by using inference chaining.[jargon][42][44] Some examples of interventions performed to improve the patient's state were focus on specific themes, clarification of patient's neologisms, and thought linkage.[44] During thought linkage, the patient is asked repeatedly by the therapist to explain his/her jumps in thought from one subject to a completely different one.[44]
Patients with mental disorders that experience grandiose delusions have been found to have a lower risk of having suicidal thoughts and attempts.[45]
Epidemiology
In researching over 1000 individuals of a vast range of backgrounds, Stompe and colleagues (2006) found that grandiosity remains as the second most common delusion after persecutory delusions.[3] A variation in the occurrence of grandiosity delusions in schizophrenic patients across cultures has also been observed.[46][47] In research done by Appelbaum et al. it has been found that GDs appeared more commonly in patients with bipolar disorder (59%) than in patients with schizophrenia (49%), followed by presence in substance misuse disorder patients (30%) and depressed patients (21%).[48]
A relationship has been claimed between the age of onset of bipolar disorder and the occurrence of GDs. According to Carlson et al. (2000), grandiose delusions appeared in 74% of the patients who were 21 or younger at the time of the onset, while they occurred only in 40% of individuals 30 years or older at the time of the onset.[49]
Prevalence
Research suggests that the severity of the delusions of grandeur is directly related to a higher self-esteem in individuals and inversely related to any individual’s severity of depression and negative self-evaluations.[50] Lucas et al. found that there is no significant gender difference in the establishment of grandiose delusion.[51] However, there is a claim that ‘the particular content of Grandiose delusions’ may be variable across both genders.[52] Also, it has been noted that the presence of GDs in people with at least grammar or high school education was greater than lesser educated persons. Similarly, the presence of grandiose delusions in individuals who are the eldest is greater than in individuals who are the youngest of their siblings.[51]
See also
- God complex
- Illusory superiority
- Messiah complex
- Organic personality disorder
- Persecutory delusions
- Put on airs
- Confidence
- Dunning–Kruger effect
- Haughtiness
- Hubris
- Icarus complex
- Overconfidence effect
- Self-serving bias
- Vanity
- Chūnibyō
References
- ↑ Ray Corsini (2016). The Dictionary of Psychology. Taylor & Francis. pp. 985. ISBN 978-1-317-70570-3. https://books.google.com/books?id=3oyoDQAAQBAJ&pg=PT985.
- ↑ Diagnostic and Statistical Manual of Mental Disorders Fourth edition Text Revision (DSM-IV-TR) American Psychiatric Association (2000)
- ↑ 3.0 3.1 3.2 Knowles, R; McCarthy-Jones, S; Rowse, G (2011). "Grandiose delusions: A review and theoretical integration of cognitive and affective perspectives". Clinical Psychology Review 31 (4): 684–696. doi:10.1016/j.cpr.2011.02.009. PMID 21482326. cites Stompe, TExpression error: Unrecognized word "etal". (2006). "The pathoplastic effect of culture on psychotic symptoms in schizophrenia". World Cultural Psychiatry Research Review: 157–163.
- ↑ 4.0 4.1 4.2 Nelson, H.E. (2005). Cognitive-Behavioural Therapy with Delusions and Hallucinations: A Practice Manual. Nelson Thornes. p. 339. ISBN 9780748792566. https://books.google.com/books?id=VfF6Qq4yxEMC. Retrieved 5 August 2012.
- ↑ Sadock, B. J.; Sadock, VA (2008). "11.3 Delusional Disorder and Shared Psychotic Disorder". Kaplan and Sadock's Concise Textbook of Clinical Psychiatry. Lippincott Williams & Wilkins. DIAGNOSIS AND CLINICAL FEATURES, Mental Status, Table 11.3–1 DSM-IV-TR Diagnostic Criteria for Delusional Disorder, p. 184. ISBN 9780781787468. "Grandiose type: delusions of inflated worth, power, knowledge, identity, or special relationship to a deity or famous person"
- ↑ Davies, J.L.; Janosik E.H. (1991). Mental Health and Psychiatric Nursing: A Caring Approach. Boston, MA: Jones & Bartlett Learning. p. 760. ISBN 9780867204421. https://books.google.com/books?id=ShKgSO8U3-QC&q=grandeur+delusions.
- ↑ 7.0 7.1 Casey, P.R.; Brendan K. (2007). Fish's Clinical Psychopathology: Signs and Symptoms in Psychiatry. UK: RCPsych Publications. p. 138. ISBN 9781904671329. https://books.google.com/books?id=gHdQTZNkA9YC&q=grandiose+delusions..
- ↑ 8.0 8.1 8.2 Isham, Louise; Sheng Loe, Bao; Hicks, Alice; Wilson, Natalie; Bird, Jessica C; Bentall, Richard P; Freeman, Daniel (2022-10-01). "The meaning in grandiose delusions: measure development and cohort studies in clinical psychosis and non-clinical general population groups in the UK and Ireland" (in en). The Lancet Psychiatry 9 (10): 792–803. doi:10.1016/S2215-0366(22)00236-X. ISSN 2215-0366. PMID 36049491. https://www.sciencedirect.com/science/article/pii/S221503662200236X.
- ↑ 9.0 9.1 9.2 Magill's Encyclopedia of Social Science: Psychology. California: Salem Press, Inc. 2003. pp. 718–719.
- ↑ Noll, R. (2009). The Encyclopedia of Schizophrenia and Other Psychotic Disorders. New York: Facts on File, Inc. p. 122. ISBN 9780816075089. https://books.google.com/books?id=jzoJxps189IC&q=grandiose+delusions+and+schizophrenia&pg=PA122.
- ↑ Hunsley, J.; Mash E.J. (2008). A Guide to Assessment that Work. Oxford University Press. p. 676. ISBN 9780198042457. https://books.google.com/books?id=bmilrEoRSf0C.
- ↑ Bernama (2016-04-28). "Man who claimed to be 'Imam Mahdi' gets 24 months' jail". https://www.malaysiakini.com/news/339572.
- ↑ Barlow, D.H. (2007). Clinical Handbook of Psychological Disorders: A Step by Step Treatment Manual. New York: Guilford. p. 722. ISBN 9781606237656. https://books.google.com/books?id=JSfnCPlEFygC.
- ↑ Kantor, M. (2004). Understanding Paranoia: A Guide for Professionals, Families, and Sufferers. West Port: Greenwoord. p. 252. ISBN 9780275981525. https://books.google.com/books?id=9ia6zITbOnMC&q=grandiose+delusions+and+bipolar.
- ↑ Isaac, G. (2001). Bipolar Not Adhd: Unrecognized Epidemic of Manic Depressive Illness in Children. Lincoln: Writers Club Press. p. 184. ISBN 9781475906493. https://books.google.com/books?id=3Qt6vKFA3DcC&q=grandiose+delusions+and+bipolar.
- ↑ Fieve, R. R. (2009). Bipolar Breakthrough: The Essential Guide to Going Beyond Moodswings to Harness Your Highs, Escape the Cycles of Recurrent Depression, and Thrive with Bipolar II. Rodale. p. 288. ISBN 9781605296456. https://books.google.com/books?id=PkixwbQsJrQC&q=grandiose+delusions+and+bipolar.
- ↑ 17.0 17.1 Smith, N.; Freeman D.; Kuipers E. (2005). "Grandiose Delusions: An Experimental Investigation of the Delusion as Defense". Journal of Nervous and Mental Disease 193 (7): 480–487. doi:10.1097/01.nmd.0000168235.60469.cc. PMID 15985843.
- ↑ Knowles, Rebecca; McCarthy-Jones, Simon; Rowse, Georgina (2011-06-01). "Grandiose delusions: A review and theoretical integration of cognitive and affective perspectives" (in en). Clinical Psychology Review 31 (4): 684–696. doi:10.1016/j.cpr.2011.02.009. ISSN 0272-7358. PMID 21482326. https://www.sciencedirect.com/science/article/pii/S0272735811000481.
- ↑ Garety, P. A., Gittins, M., Jolley, S., Bebbington, P., Dunn, G., Kuipers, E., ... & Freeman, D. (2013). Differences in cognitive and emotional processes between persecutory and grandiose delusions. Schizophrenia bulletin, 39(3), 629-639.
- ↑ Jolley, Suzanne; Garety, Philippa; Bebbington, Paul; Dunn, Graham; Freeman, Daniel; Kuipers, Elizabeth; Fowler, David; Hemsley, David (2006-11-01). "Attributional style in psychosis—The role of affect and belief type" (in en). Behaviour Research and Therapy 44 (11): 1597–1607. doi:10.1016/j.brat.2005.12.002. ISSN 0005-7967. PMID 16436270. https://www.sciencedirect.com/science/article/pii/S0005796705002512.
- ↑ Bortolon, C., & Raffard, S. (2021). Pondering on how great I am: Does rumination play a role in grandiose ideas?. Journal of behavior therapy and experimental psychiatry, 70, 101596.
- ↑ Ghaznavi, S., Chou, T., Dougherty, D. D., & Nierenberg, A. A. (2023). Differential patterns of default mode network activity associated with negative and positive rumination in bipolar disorder. Journal of Affective Disorders, 323, 607-616.
- ↑ Isham, Louise; Griffith, Laura; Boylan, Anne‐Marie; Hicks, Alice; Wilson, Natalie; Byrne, Rory; Sheaves, Bryony; Bentall, Richard P. et al. (2019-11-29). "Understanding, treating, and renaming grandiose delusions: A qualitative study" (in en). Psychology and Psychotherapy: Theory, Research and Practice 94 (1): 119–140. doi:10.1111/papt.12260. ISSN 1476-0835. PMID 31785077.
- ↑ Beck, A. T., & Rector, N. A. (2002). Delusions: A cognitive perspective. Journal of Cognitive Psychotherapy, 16(4), 455-468.
- ↑ Bosson, J. K., Lakey, C. E., Campbell, W. K., Zeigler-Hill, V., Jordan, C. H., & Kernis, M. H. (2008). Untangling the links between narcissism and self-esteem: A theoretical and empirical review. Social & Personality Psychology Compass, 2, 1415–1439. doi:10.1111/j.1751-9004.2008.00089.x
- ↑ Campbell, W. K., & Foster, J. D. (2007). The narcissistic self: Background, an extended agency model, and ongoing controversies. The self, 115, 138.
- ↑ Omar, Rohani; Sampson, Elizabeth L.; Loy, Clement T.; Mummery, Catherine J.; Fox, Nick C.; Rossor, Martin N.; Warren, Jason D. (April 2009). "Delusions in frontotemporal lobar degeneration". Journal of Neurology 256 (4): 600–607. doi:10.1007/s00415-009-0128-7. ISSN 0340-5354. PMID 19365594.
- ↑ Tonkonogy, Joseph M; Tonkonogiĭ, TM; Puente, AE (2009). "5 Disturbances in the Recognition of the Social World". Localization of Clinical Syndromes in Neuropsychology and Neuroscience. New York, NY: Springer Publishing Company. Conclusion, p. 288. ISBN 9780826119681. https://books.google.com/books?id=t2Y4gv9d3l0C&q=frontal+lobe+lesion+grandiose+delusions. "2. Temporal lobe lesions have been primarily reported in patients with delusions of persecution and of guilt, while frontal and frontotemporal involvement have described [sic] in patients with grandiose delusions, Cotard’s syndrome, and delusional misidentification syndrome."
- ↑ Bracht, T., Viher, P. V., Stegmayer, K., Strik, W., Federspiel, A., Wiest, R., & Walther, S. (2019). Increased structural connectivity of the medial forebrain bundle in schizophrenia spectrum disorders is associated with delusions of paranoid threat and grandiosity. NeuroImage: Clinical, 24, 102044.
- ↑ Stegmayer, K., Horn, H., Federspiel, A., Razavi, N., Bracht, T., Laimböck, K., ... & Walther, S. (2014). Ventral striatum gray matter density reduction in patients with schizophrenia and psychotic emotional dysregulation. NeuroImage: Clinical, 4, 232-239.
- ↑ Ping, L., Zhou, C., Sun, S., Wang, W., Zheng, Q., & You, Z. (2022). Alterations in resting‐state whole‐brain functional connectivity pattern similarity in bipolar disorder patients. Brain and Behavior, 12(5), e2580.
- ↑ Cummings, Jeffrey L. (1985). "Organic delusions: phenomenology, anatomical correlations and review". The British Journal of Psychiatry 146 (2): 184–197. doi:10.1192/bjp.146.2.184. PMID 3156653.
- ↑ McHugh, P.R; Folstein, M.F (1975). "Psychiatric syndromes in Huntington's chorea". Psychiatric Aspectes of Neurological Disease.
- ↑ Bromberg, W. (1930). "Mental states in chronic encephalitis". Psychiatric Quarterly 4 (4): 537–566. doi:10.1007/bf01563408.
- ↑ Pandy, R.S.; Sreenivas, K.N.; Paith N.M.; Swamy H.S. (1981). "Dopamine beta-hydroxylase in a patient with Wilson's disease and mania". The American Journal of Psychiatry 138 (12): 1628–1629. doi:10.1176/ajp.138.12.1628. PMID 7304799.
- ↑ Lin, J-T Y.; Ziegler, D. (1976). "Psychiatric symptoms with initiation of carbidopa-levodopa treatment.". Neurology 26 (7): 679–700. doi:10.1212/wnl.26.7.699. PMID 945518.
- ↑ Goggans, F.C. (1983). "A case of mania secondary to vitamin B12 deficiency.". The American Journal of Psychiatry 141 (2): 300–301. doi:10.1176/ajp.141.2.300. PMID 6691503.
- ↑ Cooper, A.T. (1967). "Hypomanic psychosis precipitated by hemodialysis.". Comprehensive Psychiatry 8 (3): 168–172. doi:10.1016/s0010-440x(67)80020-8. PMID 6046067.
- ↑ Jefferson, J.W.; Marshall J.R. Neuropsychiatric Features of Medical Disorders. New York: Plenum/Medical Book Company.
- ↑ Lehmann, J. (1966). "Mental disturbances followed by stupor in a patient with carcinoidosis.". Acta Psychiatrica Scandinavica 42 (2): 153–161. doi:10.1111/j.1600-0447.1966.tb01921.x. PMID 5958539.
- ↑ 41.0 41.1 Appelbaum, P.S.; Clark Robbins, P.; Roth, L. H. (1999). "Dimensional approach to delusions: Comparison across types and diagnoses". The American Journal of Psychiatry 156 (12): 1938–1943. doi:10.1176/ajp.156.12.1938. PMID 10588408.
- ↑ 42.0 42.1 Beck, A.T.; Rush A.J.; Shaw B.F.; Emergy G (1979). "Cognitive Therapy of Depression". New York, NY. Guilford Press.
- ↑ Salkovskis, P.M. (1996). Frontiers of Cognitive Therapy. New York: Guillford.
- ↑ 44.0 44.1 44.2 Sensky, T. (2000). "A randomized controlled trial of Cognitive-Behavioral Therapy for Persistent Symptoms in Schizophrenia resistant to medication". Archives of General Psychiatry 57 (2): 165–172. doi:10.1001/archpsyc.57.2.165. PMID 10665619.
- ↑ Oquendo, M.A. (2000). "Suicidal behavior in bipolar mood disorder: clinical characteristics of attempters and nonattempters". Journal of Affective Disorders 59 (2): 107–117. doi:10.1016/s0165-0327(99)00129-9. PMID 10837879.
- ↑ Stompe, T. (2007). "Paranoid-hallucinatory syndromes in schizophrenia results of the international study on psychotic symptoms". World Cultural Psychiatry Review: 63–68.
- ↑ Suhail, K. (2003). "Phenomenology of delusions in Pakistani patients: effect of gender and social class". Psychopathology 36 (4): 195–199. doi:10.1159/000072789. PMID 14504453.
- ↑ Knowles et al. (2011) cites Appelbaum, P.S.; Clark Robbins, P.; Roth, L. H. (1999). "Dimensional approach to delusions: Comparison across types and diagnoses". The American Journal of Psychiatry 156 (12): 1938–1943. doi:10.1176/ajp.156.12.1938. PMID 10588408.
- ↑ Knowles et al. (2011) cites Carlson, GA; Bromet, EJ; Sievers, S (2000). "Phenomenology and outcome of subjects with early- and adult-onset psychotic mania". American Journal of Psychiatry 157 (2): 213–219. doi:10.1176/appi.ajp.157.2.213. PMID 10671389.
- ↑ Smith, N. (2006). "Emotion and psychosis: Links between depression, self-esteem, negative schematic beliefs and delusions and hallucinations". Schizophrenia Research 86 (1): 181–188. doi:10.1016/j.schres.2006.06.018. PMID 16857346. http://discovery.ucl.ac.uk/2182/.
- ↑ 51.0 51.1 Lucas, C.J. (1962). "A social and clinical study of delusions in schizophrenia". The Journal of Mental Science 108 (457): 747–758. doi:10.1192/bjp.108.457.747. PMID 13931397.
- ↑ Knowles et al. (2011) cites Rudalevičienė, P; Stompe, T; Narbekovas, A; Raškauskienė, N; Bunevičius, R (2008). "Are religious delusions related to religiosity in schizophrenia?". Medicina (Kaunas) 44 (7): 529–535. doi:10.3390/medicina44070068. PMID 18695349.
 |

