Medicine:Hyper-IgM syndrome type 4
| Hyper IgM syndrome type 4 | |
|---|---|
 | |
| Immunoglobulin M | |
| Types | Hyper-IgM syndrome type 1,2,3,4 and 5[1][2][3][4][5] |
| Diagnostic method | MRI, Chest radiography and genetic testing[6] |
| Treatment | Allogeneic hematopoietic cell transplantation[7] |
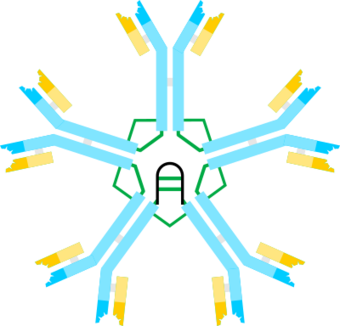
Hyper-IgM syndrome type 4 is a form of Hyper IgM syndrome which is a defect in class switch recombination downstream of the AICDA gene that does not impair somatic hypermutation.[8]
Hyper IgM syndromes
Hyper IgM syndromes is a group of primary immune deficiency disorders characterized by defective CD40 signaling; via B cells affecting class switch recombination (CSR) and somatic hypermutation. Immunoglobulin (Ig) class switch recombination deficiencies are characterized by elevated serum IgM levels and a considerable deficiency in Immunoglobulins G (IgG), A (IgA) and E (IgE). As a consequence, people with HIGM have an increased susceptibility to infections.[9][7][10]
Signs and symptoms
Hyper IgM syndrome can have the following syndromes:[6][11]
- Infection/Pneumocystis pneumonia (PCP), which is common in infants with hyper IgM syndrome, is a serious illness.[9] PCP is one of the most frequent and severe opportunistic infections in people with weakened immune systems.
- Hepatitis (Hepatitis C)
- Chronic diarrhea
- Hypothyroidism
- Neutropenia
- Arthritis
- Encephalopathy (degenerative)
Cause
Different genetic defects cause HIgM syndrome, the vast majority are inherited as an X-linked recessive genetic trait and most sufferers are male.[7][1][2][3][12][4]
IgM is the form of antibody that all B cells produce initially before they undergo class switching. Healthy B cells efficiently switch to other types of antibodies as needed to attack invading bacteria, viruses, and other pathogens. In people with hyper IgM syndromes, the B cells keep making IgM antibodies because can not switch to a different antibody. This results in an overproduction of IgM antibodies and an underproduction of IgA, IgG, and IgE.[13][7]
Pathophysiology
CD40 is a costimulatory receptor on B cells that, when bound to CD40 ligand (CD40L), sends a signal to the B-cell receptor.[14] When there is a defect in CD40, this leads to defective T-cell interaction with B cells. Consequently, humoral immune response is affected. Patients are more susceptible to infection.[6]
Diagnosis
The diagnosis of hyper IgM syndrome can be done via the following methods and tests:[6]
- MRI
- Chest radiography
- Pulmonary function test
- Lymph node test
- Laboratory test (to measure CD40)
Treatment
In terms of treatment for hyper IgM syndrome, there is the use of allogeneic hematopoietic cell transplantation. Additionally, anti-microbial therapy, use of granulocyte colony-stimulating factor, immunosuppressants, as well as other treatments, may be needed.[7]
References
- ↑ 1.0 1.1 "OMIM Entry – # 308230 – IMMUNODEFICIENCY WITH HYPER-IgM, TYPE 1; HIGM1". http://www.omim.org/entry/308230.
- ↑ 2.0 2.1 "OMIM Entry – # 605258 – IMMUNODEFICIENCY WITH HYPER-IgM, TYPE 2; HIGM2". http://omim.org/entry/605258.
- ↑ 3.0 3.1 "OMIM Entry – # 606843 – IMMUNODEFICIENCY WITH HYPER-IgM, TYPE 3; HIGM3". http://www.omim.org/entry/606843.
- ↑ 4.0 4.1 "OMIM Entry – # 608106 – IMMUNODEFICIENCY WITH HYPER-IgM, TYPE 5; HIGM5". http://omim.org/entry/608106.
- ↑ "OMIM Entry – 608184 – IMMUNODEFICIENCY WITH HYPER-IgM, TYPE 4; HIGM4" (in en-us). https://www.omim.org/entry/608184.
- ↑ 6.0 6.1 6.2 6.3 "X-linked Immunodeficiency With Hyper IgM Clinical Presentation: History, Physical, Causes". http://emedicine.medscape.com/article/889104-clinical.
- ↑ 7.0 7.1 7.2 7.3 7.4 Johnson, Judith; Filipovich, Alexandra H.; Zhang, Kejian (1 January 1993). "X-Linked Hyper IgM Syndrome". GeneReviews. PMID 20301576. https://www.ncbi.nlm.nih.gov/books/NBK1402/. Retrieved 12 November 2016.update 2013
- ↑ "Hyper immunoglobulin M syndrome due to CD40 deficiency: clinical, molecular, and immunological features". Immunol. Rev. 203: 48–66. 2005. doi:10.1111/j.0105-2896.2005.00229.x. PMID 15661021.
- ↑ 9.0 9.1 Etzioni, Amos; Ochs, Hans D. (1 October 2004). "The Hyper IgM Syndrome—An Evolving Story" (in en). Pediatric Research 56 (4): 519–525. doi:10.1203/01.PDR.0000139318.65842.4A. ISSN 0031-3998. PMID 15319456.
- ↑ "Hyper-Immunoglobulin M (Hyper-IgM) Syndromes | NIH: National Institute of Allergy and Infectious Diseases". https://www.niaid.nih.gov/diseases-conditions/hyper-immunoglobulin-m-hyper-igm-syndromes.
- ↑ Davies, E Graham; Thrasher, Adrian J (27 November 2016). "Update on the hyper immunoglobulin M syndromes". British Journal of Haematology 149 (2): 167–180. doi:10.1111/j.1365-2141.2010.08077.x. ISSN 0007-1048. PMID 20180797.
- ↑ "Hyper immunoglobulin M syndrome due to CD40 deficiency: clinical, molecular, and immunological features". Immunol. Rev. 203: 48–66. 2005. doi:10.1111/j.0105-2896.2005.00229.x. PMID 15661021.subscription needed
- ↑ Reference, Genetics Home. "X-linked hyper IgM syndrome". https://ghr.nlm.nih.gov/condition/x-linked-hyper-igm-syndrome#.
- ↑ Reference, Genetics Home. "CD40 gene". https://ghr.nlm.nih.gov/gene/CD40.
| Classification | |
|---|---|
| External resources |
 |


