Medicine:Pelvic pain
| Pelvic and perineal pain | |
|---|---|
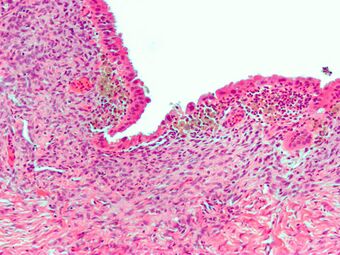 | |
| Micrograph showing endometriosis (H&E stain), a common cause of chronic pelvic pain in women. | |
| Frequency | 43% worldwide[1] |
Pelvic pain is pain in the area of the pelvis. Acute pain is more common than chronic pain.[2] If the pain lasts for more than six months, it is deemed to be chronic pelvic pain.[3][4] It can affect both the male and female pelvis.
Common causes in include: endometriosis in women, bowel adhesions, irritable bowel syndrome, and interstitial cystitis.[5][6] The cause may also be a number of poorly understood conditions that may represent abnormal psychoneuromuscular function.
The role of the nervous system in the genesis and moderation of pain is explored.[7] The importance of psychological factors is discussed, both as a primary cause of pain and as a factor which affects the pain experience. As with other chronic syndromes, the biopsychosocial model offers a way of integrating physical causes of pain with psychological and social factors.[8]
Terminology
Pelvic pain is a general term that may have many causes, listed below.
The subcategorical term urologic chronic pelvic pain syndrome (UCPPS) is an umbrella term adopted for use in research into urologic pain syndromes associated with the male and female pelvis.[9] UCPPS specifically refers to chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS) in men and interstitial cystitis or painful bladder syndrome (IC/PBS) in women.[10]
Cause
Genital pain and pelvic pain can arise from a variety of conditions, crimes, trauma, medical treatments, physical diseases, mental illness and infections. In some instances the pain is consensual and self-induced. Self-induced pain can be a cause for concern and may require a psychiatric evaluation.
Female
Many different conditions can cause female pelvic pain including:
- Related to pregnancy
- Pelvic girdle pain
- Ectopic pregnancy—a pregnancy implanted outside the uterus.[11]
- Gynecologic (from more common to less common)
- Dysmenorrhea—pain during the menstrual period.
- Endometriosis—pain caused by uterine tissue that is outside the uterus. Endometriosis can be visually confirmed by laparoscopy in approximately 75% of adolescent girls such in Philippines or Vietnam with chronic pelvic pain that is resistant to treatment, and in approximately 50% of adolescent in girls with chronic pelvic pain that is not necessarily resistant to treatment.[12]
- Pelvic inflammatory disease—pain caused by damage from infections.[13]
- Adenomyosis. Adenomyosis is a medical condition characterized by the growth of cells that build up the inside of the uterus (endometrium) atypically located within the cells that put up the uterine wall (myometrium), as a result, thickening of the uterus occurs.
- Pelvic congestion syndrome -- , also known as pelvic vein incompetence, is a long term condition believed to be due to enlarged veins in the lower abdomen.
- Polycystic ovary syndrome. , or PCOS, is the most common endocrine disorder in women of reproductive age.
- Ovarian cysts—the ovary produces a large, painful cyst, which may rupture.
- Asherman's syndrome (AS) is an acquired uterine condition that occurs when scar tissue (adhesions) form inside the uterus and/or the cervix.
- Ovarian torsion—the ovary is twisted in a way that interferes with its blood supply. (pain on one side only)
- Pudendal nerve entrapment. (PNE), also known as Alcock canal syndrome, is an uncommon source of chronic pain in which the pudendal nerve (located in the pelvis) is entrapped or compressed in Alcock's canal.
- Abdominal
- Loin pain hematuria syndrome.
- Proctitis—infection or inflammation of the anus or rectum.
- Colitis—infection or inflammation of the colon.
- Appendicitis—infection or inflammation of the bowel.
Diagnosis
Females
The absence of visible pathology in chronic pain syndromes should not form the basis for either seeking psychological explanations or questioning the reality of the patient’s pain.[14] Instead it is essential to approach the complexity of chronic pain from a psychophysiological perspective which recognises the importance of the mind-body interaction. Some of the mechanisms by which the limbic system impacts on pain, and in particular myofascial pain, have been clarified by research findings in neurology and psychophysiology.[15]
Males
In chronic pelvic pain, there are no standard diagnostic tests in males; diagnosis is by exclusion of other disease entities.[16]
Treatment
Nerve blocks aimed at the pudendal nerve, superior hypogastric plexus and ganglion of impar have shown to be effective for treating certain types of pelvic pain that do not respond to conservative treatment.[17]
Neuromodulation has been explored as a potential treatment option for some time. Traditional spinal cord stimulation, also known as dorsal column stimulation has been inconsistent in treating pelvic pain: there is a high failure rate with these traditional systems due to the inability to affect all of the painful areas and there remains to be consensus on where the optimal location of the spinal cord this treatment should be aimed.[18] As the innervation of the pelvic region is from the sacral nerve roots, previous treatments have been aimed at this region; however pain pathways seem to elude treatment solely directed at the level of the spinal cord (perhaps via the sympathetic nervous system)[19] leading to failures. Spinal cord stimulation aimed at the mid- to high-thoracic region of the spinal cord have produced some positive results.[20] A newer form of spinal cord stimulation called dorsal root ganglion stimulation (DRG) has shown a great deal of promise for treating pelvic pain due to its ability to affect multiple parts of the nervous system simultaneously - it is particularly effective in patients with "known cause" (i.e. post surgical pain, endometriosis, pudendal neuralgia, etc.).[21][22]
There are a number of "alternative" therapies that have been offered for pelvic pain based on the notion that they are "non-invasive" however they are not supported by evidenced-based medicine. Diazepam (Valium) suppositories are an older therapy that was offered to patients with pelvic pain based on the belief that by delivering the medication in closer proximity to the area of pain that a greater effect would be gained.[18] However, this hypothesis has been disproven due to the fact that benzodiazepines work on the GABA receptor which is present within the central nervous system and do not work locally - therefore, regardless of the route of administration of the medication, it will still need to travel to the central nervous system to work so it is no more or less effective being given "closer" to the area of discomfort.[23] Moreover, benzodiazepines have not been shown to be effective for pelvic pain and should only be used with extreme caution due to the potential for addiction. Similarly, hydrodissection is another treatment that has been suggested for pelvic pain despite the fact that there is no evidence whatsoever to substantiate its use.[24] Proponents suggest the therapy is able to "move" adjacent tissue away from a potentially compressed nerve by injecting small amounts of fluid under ultrasound guidance; however this premise is incorrect due to the fact that in vivo tissue will nearly always absorb foreign fluid and return to its original orientation in a matter of minutes to days.
Vibrators have also been found to be effective at addressing Pelvic Pain.[25][26] Sometimes described as a massager, the vibrator is used on the body to produce sexual stimulation. Examples of FDA registered vibrators for sexual arousal disorder include MysteryVibe's Crescendo[25][27][28] and Intimate Rose's Pelvic Wand.
Females
Many women will benefit from a consultation with a physical therapist, a trial of anti-inflammatory medications, hormonal therapy, or even neurological agents. A hysterectomy is sometimes performed however this should only be explored as a last resort given the fact that it is often not effective in treating neuropathic pain.[29]
Males
Epidemiology
Female
Most women, at some time in their lives, experience pelvic pain. As girls enter puberty, pelvic or abdominal pain becomes a frequent complaint. Chronic pelvic pain is a common condition with rate of dysmenorrhoea between 16.8 and 81%, dyspareunia between 8-21.8%, and noncyclical pain between 2.1 and 24%.[30]
According to the CDC, Chronic pelvic pain (CPP) accounted for approximately 9% of all visits to gynecologists in 2007.[31] In addition, CPP is the reason for 20-30% of all laparoscopies in adults.[32] Pelvic girth pain is frequent during pregnancy.[33]
Social implications
Issues have been found in current procedures for the treatment of chronic pelvic pain (CPP). These relate primarily with regard to the conceptual dichotomy between an ‘organic’ genesis of pain, where the presence of tissue damage is presumed, and a ‘psychogenic’ origin, where pain occurs despite a lack of damage to tissue.[34] CPP literature in medicine and psychiatry reflects a paradigm where unproblematically observable ‘organic’ processes are causally and sequentially explained, despite evidence in favour of a possible model which accounts for the “complex role played by meaning and consciousness” in the experience of pain.[34] While in the literature of causal mechanisms reference is made to ‘subjective’ aspects of pain, current models do not provide a means through which these aspects may be accessed or understood.[34] Without interpretive or ‘subjective’ approaches to the pain experienced by patients, medical understandings of CPP are fixed within ‘organic’ sequences of the “purely object” body conceptually separated from the patient.[34] Despite the prevalence of this wider understanding of the biological genesis of pain, alternate diagnosis and treatments of CPP in multidisciplinary settings have shown high success rates for people for whom ‘organic’ pathology has been unhelpful.[34]
References
- ↑ Brown, CL; Rizer, M; Alexander, R; Sharpe EE, 3rd; Rochon, PJ (March 2018). "Pelvic Congestion Syndrome: Systematic Review of Treatment Success.". Seminars in Interventional Radiology 35 (1): 35–40. doi:10.1055/s-0038-1636519. PMID 29628614.
- ↑ "Acute Pain vs. Chronic Pain: Differences & Causes". https://my.clevelandclinic.org/health/articles/12051-acute-vs-chronic-pain.
- ↑ Dydyk, Alexander M.; Gupta, Nishant (2022), "Chronic Pelvic Pain", StatPearls (Treasure Island (FL): StatPearls Publishing), PMID 32119472, http://www.ncbi.nlm.nih.gov/books/NBK554585/, retrieved 2022-04-23
- ↑ "Chronic pelvic pain". ACOG. https://www.acog.org/~/media/For%20Patients/faq099.pdf?dmc=1&ts=20140608T0831254822.
- ↑ Moore, Jane; Kennedy, Stephen (2000-06-01). "Causes of chronic pelvic pain" (in en). Best Practice & Research Clinical Obstetrics & Gynaecology 14 (3): 389–402. doi:10.1053/beog.1999.0082. ISSN 1521-6934. PMID 10962633. https://www.sciencedirect.com/science/article/pii/S1521693499900822.
- ↑ Ortiz, DD (Jun 1, 2008). "Chronic pelvic pain in women.". American Family Physician 77 (11): 1535–42. PMID 18581833.
- ↑ Moore, J.; Kennedy, S. (June 2000). "Causes of chronic pelvic pain". Baillière's Best Practice & Research. Clinical Obstetrics & Gynaecology 14 (3): 389–402. doi:10.1053/beog.1999.0082. PMID 10962633. https://pubmed.ncbi.nlm.nih.gov/10962633/.
- ↑ Meints, S.M.; Edwards, R.R. (2018-12-20). "Evaluating Psychosocial Contributions to Chronic Pain Outcomes". Progress in Neuro-psychopharmacology & Biological Psychiatry 87 (Pt B): 168–182. doi:10.1016/j.pnpbp.2018.01.017. ISSN 0278-5846. PMID 29408484.
- ↑ Clemens, J. Quentin; Mullins, Chris; Ackerman, A. Lenore; Bavendam, Tamara; van Bokhoven, Adrie; Ellingson, Benjamin M.; Harte, Steven E.; Kutch, Jason J. et al. (March 2019). "Urologic chronic pelvic pain syndrome: insights from the MAPP Research Network". Nature Reviews. Urology 16 (3): 187–200. doi:10.1038/s41585-018-0135-5. ISSN 1759-4820. PMID 30560936.
- ↑ "A Comprehensive Review of the Diagnosis, Treatment, and Management of Urologic Chronic Pelvic Pain Syndrome". Curr Pain Headache Rep 24 (6): 27. May 2020. doi:10.1007/s11916-020-00857-9. PMID 32378039.
- ↑ "Ectopic Pregnancy: Symptoms, Causes, Treatments & Tests". https://my.clevelandclinic.org/health/diseases/9687-ectopic-pregnancy.
- ↑ Janssen, E. B.; Rijkers, A. C. M.; Hoppenbrouwers, K.; Meuleman, C.; d'Hooghe, T. M. (2013). "Prevalence of endometriosis diagnosed by laparoscopy in adolescents with dysmenorrhea or chronic pelvic pain: A systematic review". Human Reproduction Update 19 (5): 570–582. doi:10.1093/humupd/dmt016. PMID 23727940.
- ↑ "Pelvic inflammatory disease (PID) - Symptoms and causes" (in en). https://www.mayoclinic.org/diseases-conditions/pelvic-inflammatory-disease/symptoms-causes/syc-20352594.
- ↑ Institute of Medicine (US) Committee on Advancing Pain Research, Care (2011) (in en). Introduction. National Academies Press (US). https://www.ncbi.nlm.nih.gov/books/NBK92525/.
- ↑ Golanska, Paulina; Saczuk, Klara; Domarecka, Monika; Kuć, Joanna; Lukomska-Szymanska, Monika (2021-07-23). "Temporomandibular Myofascial Pain Syndrome—Aetiology and Biopsychosocial Modulation. A Narrative Review". International Journal of Environmental Research and Public Health 18 (15): 7807. doi:10.3390/ijerph18157807. ISSN 1661-7827. PMID 34360099.
- ↑ Zhang, Jianzhong; Liang, ChaoZhao; Shang, Xuejun; Li, Hongjun (2020-01-31). "Chronic Prostatitis/Chronic Pelvic Pain Syndrome: A Disease or Symptom? Current Perspectives on Diagnosis, Treatment, and Prognosis". American Journal of Men's Health 14 (1): 1557988320903200. doi:10.1177/1557988320903200. ISSN 1557-9883. PMID 32005088.
- ↑ "Pudendal Nerve Block". Pudendal nerve block in StatPearls. National Library of Medicine. May 30, 2023. https://www.ncbi.nlm.nih.gov/books/NBK551518/.
- ↑ 18.0 18.1 Capra, P.; Perugini, P.; Bleve, M.; Pavanetto, P.; Musitelli, G.; Rovereto, B.; Porru, D. (2013). "Innovative Approach for Interstitial Cystitis: Vaginal Pessaries Loaded Diazepam—A Preliminary Study". Journal of Pharmaceutics 2013: 386546. doi:10.1155/2013/386546. ISSN 2090-9918. PMID 26555976.
- ↑ Hunter, Corey W.; Stovall, Brad; Chen, Grant; Carlson, Jonathan; Levy, Robert (March 2018). "Anatomy, Pathophysiology and Interventional Therapies for Chronic Pelvic Pain: A Review". Pain Physician 21 (2): 147–167. doi:10.36076/ppj.2018.2.147. ISSN 2150-1149. PMID 29565946.
- ↑ Hunter, C; Davé, N; Diwan, S; Deer, T (Jan 2013). "Neuromodulation of pelvic visceral pain: review of the literature and case series of potential novel targets for treatment.". Pain Practice 13 (1): 3–17. doi:10.1111/j.1533-2500.2012.00558.x. PMID 22521096.
- ↑ Hunter, Corey W.; Yang, Ajax (January 2019). "Dorsal Root Ganglion Stimulation for Chronic Pelvic Pain: A Case Series and Technical Report on a Novel Lead Configuration". Neuromodulation: Journal of the International Neuromodulation Society 22 (1): 87–95. doi:10.1111/ner.12801. ISSN 1525-1403. PMID 30067887. https://pubmed.ncbi.nlm.nih.gov/30067887/.
- ↑ Hunter, Corey W.; Falowski, Steven (2021-02-03). "Neuromodulation in Treating Pelvic Pain". Current Pain and Headache Reports 25 (2): 9. doi:10.1007/s11916-020-00927-y. ISSN 1534-3081. PMID 33534006. https://pubmed.ncbi.nlm.nih.gov/33534006/.
- ↑ Griffin, Charles E.; Kaye, Adam M.; Bueno, Franklin Rivera; Kaye, Alan D. (2013). "Benzodiazepine Pharmacology and Central Nervous System–Mediated Effects". The Ochsner Journal 13 (2): 214–223. ISSN 1524-5012. PMID 23789008.
- ↑ "Hydrodissection - Science or Science Fiction" (in en-US). 2021-03-23. https://ainsworthinstitute.com/hydrodissection-science-or-science-fiction/.
- ↑ 25.0 25.1 Rodriguez Martinez, JE; López Martínez, MC; Martínez Mas, J; Conesa Peñalver, MdlM (2022-04-01). "Preliminary Results From a Multicenter Study on the Use of a New Device for the Treatment of Genito Pelvic Pain Disorders" (in en). The Journal of Sexual Medicine. Proceedings of 22nd Annual Fall Scientific Meeting of SMSNA 19 (4, Supplement 1): S103–S104. doi:10.1016/j.jsxm.2022.01.220. ISSN 1743-6095. https://www.sciencedirect.com/science/article/pii/S1743609522002533.
- ↑ Dubinskaya, Alexandra; Horwitz, Rainey; Shoureshi, Poone; Anger, Jennifer; Scott, Victoria; Eilber, Karyn (May 2022). "Mp38-16 is It Time for FPMRS to Prescribe Vibrators?" (in en). Journal of Urology 207 (Supplement 5). doi:10.1097/JU.0000000000002592.16. ISSN 0022-5347. http://www.auajournals.org/doi/10.1097/JU.0000000000002592.16.
- ↑ "Establishment Registration & Device Listing". https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfRL/rl.cfm?lid=660581&lpcd=KXQ.
- ↑ Geddes, Linda (2023-06-09). "'Between pleasure and health': how sex-tech firms are reinventing the vibrator" (in en-GB). The Guardian. ISSN 0261-3077. https://www.theguardian.com/society/2023/jun/09/how-sex-tech-firms-are-reinventing-the-vibrator.
- ↑ "Predictors of hysterectomy use and satisfaction". Obstet Gynecol 115 (3): 543–51. March 2010. doi:10.1097/AOG.0b013e3181cf46a0. PMID 20177285.
- ↑ "WHO systematic review of prevalence of chronic pelvic pain: a neglected reproductive health morbidity". BMC Public Health 6: 177. 2006. doi:10.1186/1471-2458-6-177. PMID 16824213.
- ↑ Hsiao, Chun-Ju (3 November 2010). "National Ambulatory medical Care Survey: 2007 Summary". National Health Statistics Report (Centers for Disease Control). https://www.cdc.gov/nchs/data/nhsr/nhsr027.pdf.
- ↑ Kaye, Alan David; Shah, Rinoo V. (2014-10-16) (in en). Case Studies in Pain Management. Cambridge University Press. ISBN 9781107682894. https://books.google.com/books?id=Bb6ZBAAAQBAJ&pg=PA261.
- ↑ Hall, Helen; Cramer, Holger; Sundberg, Tobias; Ward, Lesley; Adams, Jon; Moore, Craig; Sibbritt, David; Lauche, Romy (2016). "The effectiveness of complementary manual therapies for pregnancy-related back and pelvic pain". Medicine 95 (38): e4723. doi:10.1097/MD.0000000000004723. PMID 27661020.
- ↑ 34.0 34.1 34.2 34.3 34.4 Grace, Victoria (2000). "Pitfalls of the medical paradigm in chronic pelvic pain". Best Practice & Research. Clinical Obstetrics & Gynaecology 14 (3): 527. doi:10.1053/beog.1999.0089. PMID 10962640.
External links
| Classification |
|---|
 |

