Medicine:Polycystic ovary syndrome
| Polycystic ovary syndrome | |
|---|---|
| Other names | Hyperandrogenic anovulation (HA),[1] Stein-Leventhal syndrome[2] |
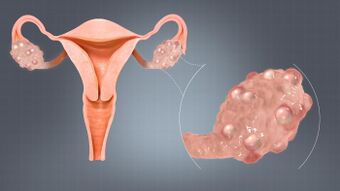 | |
| A polycystic ovary | |
| Specialty | Gynecology, endocrinology |
| Symptoms | Irregular menstrual periods, heavy periods, excess hair, acne, pelvic pain, difficulty getting pregnant, patches of thick, darker, velvety skin[3] |
| Complications | Type 2 diabetes, obesity, obstructive sleep apnea, heart disease, mood disorders, endometrial cancer[4] |
| Duration | Long term[5] |
| Causes | Genetic and environmental factors[6][7] |
| Risk factors | Obesity, not enough exercise, family history[8] |
| Diagnostic method | Based on anovulation, high androgen levels, ovarian cysts[4] |
| Differential diagnosis | Adrenal hyperplasia, hypothyroidism, high blood levels of prolactin[9] |
| Treatment | Weight loss, exercise[10][11] |
| Medication | Birth control pills, metformin, anti-androgens[12] |
| Frequency | 2% to 20% of women of childbearing age[8][13] |
Polycystic ovary syndrome, or polycystic ovarian syndrome (PCOS), is the most common endocrine disorder in women of reproductive age.[14] The syndrome is named after cysts which form on the ovaries of some people with this condition, though this is not a universal symptom, and not the underlying cause of the disorder.[15][16]
Women with PCOS may experience irregular menstrual periods, heavy periods, excess hair, acne, pelvic pain, difficulty getting pregnant, and patches of thick, darker, velvety skin.[3] The primary characteristics of this syndrome include: hyperandrogenism, anovulation, insulin resistance, and neuroendocrine disruption.[17]
A review of international evidence found that the prevalence of PCOS could be as high as 26% among some populations, though ranges between 4% and 18% are reported for general populations.[18][19][20]
The exact cause of PCOS remains uncertain, and treatment involves management of symptoms using medication.[19]
Definition
Two definitions are commonly used:
- NIH
- In 1990, a consensus workshop sponsored by the NIH/NICHD suggested that a person has PCOS if they have all of the following:[21]
- oligoovulation
- signs of androgen excess (clinical or biochemical)
- exclusion of other disorders that can result in menstrual irregularity and hyperandrogenism (e.g.: Congenital Suprarrenal Hyperplasia, androgen producer tumors, hyperprolactinemia).
- Rotterdam
In 2003, a consensus workshop sponsored by ESHRE/ASRM in Rotterdam indicated PCOS to be present if any two out of three criteria are met, in the absence of other entities that might cause these findings:[22][23][24]
- oligoovulation and/or anovulation
- excess androgen activity
- polycystic ovaries (by gynecologic ultrasound)
The Rotterdam definition is wider, including many more women, the most notable ones being women without androgen excess. Critics say that findings obtained from the study of women with androgen excess cannot necessarily be extrapolated to women without androgen excess.[25][26]
- Androgen Excess PCOS Society
- In 2006, the Androgen Excess PCOS Society suggested a tightening of the diagnostic criteria to all of the following:[22]
- excess androgen activity
- oligoovulation/anovulation and/or polycystic ovaries
- exclusion of other entities that would cause excess androgen activity
Signs and symptoms
Signs and symptoms of PCOS include irregular or no menstrual periods, heavy periods, excess body and facial hair, acne, pelvic pain, difficulty getting pregnant, and patches of thick, darker, velvety skin,[3] ovarian cysts, enlarged ovaries, excess androgen, and weight gain.[27][28]
Associated conditions include type 2 diabetes, obesity, obstructive sleep apnea, heart disease, mood disorders, and endometrial cancer.[4]
Common signs and symptoms of PCOS include the following:
- Menstrual disorders: PCOS mostly produces oligomenorrhea (fewer than nine menstrual periods in a year) or amenorrhea (no menstrual periods for three or more consecutive months), but other types of menstrual disorders may also occur.[22]
- Infertility: This generally results directly from chronic anovulation (lack of ovulation).[22]
- High levels of masculinizing hormones: Known as hyperandrogenism, the most common signs are acne and hirsutism (male pattern of hair growth, such as on the chin or chest), but it may produce hypermenorrhea (heavy and prolonged menstrual periods), androgenic alopecia (increased hair thinning or diffuse hair loss), or other symptoms.[22][29] Approximately three-quarters of women with PCOS (by the diagnostic criteria of NIH/NICHD 1990) have evidence of hyperandrogenemia.[30]
- Metabolic syndrome: This appears as a tendency towards central obesity and other symptoms associated with insulin resistance, including low energy levels and food cravings.[22] Serum insulin, insulin resistance, and homocysteine levels are higher in women with PCOS.[31]
- Acne: A rise in testosterone levels, increases the oil production within the sebaceous glands and clogs pores.[32] For many people, the emotional impact is great and quality of life can be significantly reduced.[33]
- Androgenic Alopecia: Estimates suggest that androgenic alopecia affects 22% of PCOS sufferers.[32] This is a result of high testosterone levels that are converted into the dihydrotestosterone (DHT) hormone. Hair follicles become clogged, making hair fall out and preventing further growth.[34]
- Acanthosis Nigricans (AN): A skin condition where dark, thick and "velvety" patches can form. (p. 141)[35]
- Polycystic ovaries: PCOS is a complicated disorder characterized by high androgen levels, irregular menstruation, and/or small cysts on one or both ovaries. Ovaries might get enlarged and comprise follicles surrounding the eggs. As result, ovaries might fail to function regularly. This disease is related to the number of follicles per ovary each month growing from the average range of 6-8 to double, triple or more[citation needed]. Women with PCOS have higher risk of multiple diseases including Infertility, type 2 diabetes mellitus (DM-2), cardiovascular risk, metabolic syndrome, obesity, impaired glucose tolerance, depression, obstructive sleep apnea (OSA), endometrial cancer, and nonalcoholic fatty liver disease/nonalcoholic steatohepatitis (NAFLD/NASH).[36]
Women with PCOS tend to have central obesity, but studies are conflicting as to whether visceral and subcutaneous abdominal fat is increased, unchanged, or decreased in women with PCOS relative to non-PCOS women with the same body mass index.[37] In any case, androgens, such as testosterone, androstanolone (dihydrotestosterone), and nandrolone decanoate have been found to increase visceral fat deposition in both female animals and women.[38]
Although 80% of PCOS presents in women with obesity, 20% of women diagnosed with the disease are non-obese or "lean" women.[39] However, obese women that have PCOS have a higher risk of adverse outcomes, such as hypertension, insulin resistance, metabolic syndrome, and endometrial hyperplasia.[40]
Even though most women with PCOS are overweight or obese, it is important to acknowledge that non-overweight women can also be diagnosed with PCOS. Up to 30% of women diagnosed with PCOS maintain a normal weight before and after diagnosis. "Lean" women still face the various symptoms of PCOS with the added challenges of having their symptoms properly addressed and recognized. Lean women often go undiagnosed for years, and usually are diagnosed after struggles to conceive.[41] Lean women are likely to have a missed diagnosis of diabetes and cardiovascular disease. These women also have an increased risk of developing insulin resistance, despite not being overweight. Lean women are often taken less seriously with their diagnosis of PCOS, and also face challenges finding appropriate treatment options. This is because most treatment options are limited to approaches of losing weight and healthy dieting.[42]
Hormone levels
Testosterone levels are usually elevated in women with PCOS.[43][44] In a 2020 systematic review and meta-analysis of sexual dysfunction related to PCOS which included 5,366 women with PCOS from 21 studies, testosterone levels were analyzed and were found to be 2.34 nmol/L (67 ng/dL) in women with PCOS and 1.57 nmol/L (45 ng/dL) in women without PCOS.[44] In a 1995 study of 1,741 women with PCOS, mean testosterone levels were 2.6 (1.1–4.8) nmol/L (75 (32–140) ng/dL).[45] In a 1998 study which reviewed many studies and subjected them to meta-analysis, testosterone levels in women with PCOS were 62 to 71 ng/dL (2.2–2.5 nmol/L) and testosterone levels in women without PCOS were about 32 ng/dL (1.1 nmol/L).[46] In a 2010 study of 596 women with PCOS which used liquid chromatography–mass spectrometry (LC–MS) to quantify testosterone, median levels of testosterone were 41 and 47 ng/dL (with 25th–75th percentiles of 34–65 ng/dL and 27–58 ng/dL and ranges of 12–184 ng/dL and 1–205 ng/dL) via two different labs.[47] If testosterone levels are above 100 to 200 ng/dL, per different sources, other possible causes of hyperandrogenism, such as congenital adrenal hyperplasia or an androgen-secreting tumor, may be present and should be excluded.[45][48][43] In women with PCOS, the ratio of Luteinizing Hormone (LH) to Follicle-Stimulating Hormone (FSH) is typically elevated, ranging from 2 to 3, whereas in healthy women, it typically stays within the range of 1 to 2. This imbalance is driven by an increase in luteinizing hormone levels and a decrease in follicle-stimulating hormone levels.[49]
Associated conditions
Warning signs may include a change in appearance. But there are also manifestations of mental health problems, such as anxiety, depression, and eating disorders.[27]
A diagnosis of PCOS suggests an increased risk of the following:
- Endometrial hyperplasia and endometrial cancer (cancer of the uterine lining) are possible, due to overaccumulation of uterine lining, and also lack of progesterone, resulting in prolonged stimulation of uterine cells by estrogen.[21][50] It is not clear whether this risk is directly due to the syndrome or from the associated obesity, hyperinsulinemia, and hyperandrogenism.[51][52][53]
- Insulin resistance/type 2 diabetes. A review published in 2010 concluded that women with PCOS have an elevated prevalence of insulin resistance and type 2 diabetes, even when controlling for body mass index (BMI).[21][54] PCOS is also associated with higher risk for diabetes.[55]
- High blood pressure, in particular if obese or during pregnancy[56]
- Depression and anxiety[22][57]
- Dyslipidemia – disorders of lipid metabolism – cholesterol and triglycerides. Women with PCOS show a decreased removal of atherosclerosis-inducing remnants, seemingly independent of insulin resistance/type 2 diabetes.[58]
- Cardiovascular disease,[21] with a meta-analysis estimating a 2-fold risk of arterial disease for women with PCOS relative to women without PCOS, independent of BMI.[59]
- Strokes[21]
- Weight gain
- Miscarriage[60][61]
- Sleep apnea, particularly if obesity is present
- Non-alcoholic fatty liver disease, particularly if obesity is present
- Acanthosis nigricans (patches of darkened skin under the arms, in the groin area, on the back of the neck)[21]
- Autoimmune thyroiditis[citation needed]
- Iron deficiency[62]
The risk of ovarian cancer and breast cancer is not significantly increased overall.[50]
Cause
PCOS is a heterogeneous disorder of uncertain cause.[63][64] There is some evidence that it is a genetic disease. Such evidence includes the familial clustering of cases, greater concordance in monozygotic compared with dizygotic twins and heritability of endocrine and metabolic features of PCOS.[7][63][64] There is some evidence that exposure to higher than typical levels of androgens and the anti-Müllerian hormone (AMH) in utero increases the risk of developing PCOS in later life.[65]
It may be caused by a combination of genetic and environmental factors.[6][7][66] Risk factors include obesity, a lack of physical exercise, and a family history of someone with the condition.[8] Diagnosis is based on two of the following three findings: anovulation, high androgen levels, and ovarian cysts.[4] Cysts may be detectable by ultrasound.[9] Other conditions that produce similar symptoms include adrenal hyperplasia, hypothyroidism, and high blood levels of prolactin.[9]
Genetics
The genetic component appears to be inherited in an autosomal dominant fashion with high genetic penetrance but variable expressivity in females; this means that each child has a 50% chance of inheriting the predisposing genetic variant(s) from a parent, and, if a daughter receives the variant(s), the daughter will have the disease to some extent.[64][67][68][69] The genetic variant(s) can be inherited from either the father or the mother, and can be passed along to both sons (who may be asymptomatic carriers or may have symptoms such as early baldness and/or excessive hair) and daughters, who will show signs of PCOS.[67][69] The phenotype appears to manifest itself at least partially via heightened androgen levels secreted by ovarian follicle theca cells from women with the allele.[68] The exact gene affected has not yet been identified.[7][64][70] In rare instances, single-gene mutations can give rise to the phenotype of the syndrome.[71] Current understanding of the pathogenesis of the syndrome suggests, however, that it is a complex multigenic disorder.[72]
Due to the scarcity of large-scale screening studies, the prevalence of endometrial abnormalities in PCOS remains unknown, though women with the condition may be at increased risk for endometrial hyperplasia and carcinoma as well as menstrual dysfunction and infertility.
The severity of PCOS symptoms appears to be largely determined by factors such as obesity.[7][22][73] PCOS has some aspects of a metabolic disorder, since its symptoms are partly reversible. Even though considered as a gynecological problem, PCOS consists of 28 clinical symptoms.[74]
Even though the name suggests that the ovaries are central to disease pathology, cysts are a symptom instead of the cause of the disease. Some symptoms of PCOS will persist even if both ovaries are removed; the disease can appear even if cysts are absent. Since its first description by Stein and Leventhal in 1935, the criteria of diagnosis, symptoms, and causative factors are subject to debate. Gynecologists often see it as a gynecological problem, with the ovaries being the primary organ affected. However, recent insights show a multisystem disorder, with the primary problem lies in hormonal regulation in the hypothalamus, with the involvement of many organs. The term PCOS is used due to the fact that there is a wide spectrum of symptoms possible. It is common to have polycystic ovaries without having PCOS; approximately 20% of European women have polycystic ovaries, but most of those women do not have PCOS.[15]
Environment
PCOS may be related to or worsened by exposures[clarification needed] during the prenatal period,[75][76][77] epigenetic factors, environmental impacts (especially industrial endocrine disruptors, such as bisphenol A and certain drugs)[78][79][80] and the increasing rates of obesity.[79]
Endocrine disruptors are defined as chemicals that can interfere with the endocrine system by mimicking hormones such as estrogen. According to the NIH (National Institute of Health), examples of endocrine disruptors can include dioxins and triclosan. Endocrine disruptors can cause adverse health impacts in animals.[81] Additional research is needed to assess the role that endocrine disruptors may play in disrupting reproductive health in women and possibly triggering or exacerbating PCOS and its related symptoms.[82]
Pathogenesis
Polycystic ovaries develop when the ovaries are stimulated to produce excessive amounts of androgenic hormones, in particular testosterone, by either one or a combination of the following (almost certainly combined with genetic susceptibility):[68]
- the release of excessive luteinizing hormone (LH) by the anterior pituitary gland
- through high levels of insulin in the blood (hyperinsulinaemia) in women whose ovaries are sensitive to this stimulus
A majority of women with PCOS have insulin resistance and/or are obese, which is a strong risk factor for insulin resistance, although insulin resistance is a common finding among women with PCOS in normal-weight women as well.[10][22][31] Elevated insulin levels contribute to or cause the abnormalities seen in the hypothalamic–pituitary–ovarian axis that lead to PCOS. Hyperinsulinemia increases GnRH pulse frequency,[83] which in turn results in an increase in the LH/FSH ratio[83][84] increased ovarian androgen production; decreased follicular maturation; and decreased SHBG binding.[83] Furthermore, excessive insulin increases the activity of 17α-hydroxylase, which catalyzes the conversion of progesterone to androstenedione, which is in turn converted to testosterone. The combined effects of hyperinsulinemia contribute to an increased risk of PCOS.[83]
Adipose (fat) tissue possesses aromatase, an enzyme that converts androstenedione to estrone and testosterone to estradiol. The excess of adipose tissue in obese women creates the paradox of having both excess androgens (which are responsible for hirsutism and virilization) and excess estrogens (which inhibit FSH via negative feedback).[85]
The syndrome acquired its most widely used name due to the common sign on ultrasound examination of multiple (poly) ovarian cysts. These "cysts" are in fact immature ovarian follicles. The follicles have developed from primordial follicles, but this development has stopped ("arrested") at an early stage, due to the disturbed ovarian function. The follicles may be oriented along the ovarian periphery, appearing as a 'string of pearls' on ultrasound examination.[86]
PCOS may be associated with chronic inflammation,[87] with several investigators correlating inflammatory mediators with anovulation and other PCOS symptoms.[88][89] Similarly, there seems to be a relation between PCOS and an increased level of oxidative stress.[90]
Diagnosis
Not every person with PCOS has polycystic ovaries (PCO), nor does everyone with ovarian cysts have PCOS; although a pelvic ultrasound is a major diagnostic tool, it is not the only one.[91] The diagnosis is fairly straightforward using the Rotterdam criteria, even when the syndrome is associated with a wide range of symptoms.[92]
-
Transvaginal ultrasound scan of polycystic ovary
-
Polycystic ovary as seen on sonography
Differential diagnosis
Other causes of irregular or absent menstruation and hirsutism, such as hypothyroidism, congenital adrenal hyperplasia (21-hydroxylase deficiency) (which may cause excessive body hair, deep tone voice and others symptoms similar to hyperandrogenism), Cushing's syndrome, hyperprolactinemia (leading to anovulation), androgen-secreting neoplasms, and other pituitary or adrenal disorders, should be investigated.[22][24][93]
Assessment and testing
Standard assessment
- History-taking, specifically for menstrual pattern, obesity, hirsutism and acne. A clinical prediction rule found that these four questions can diagnose PCOS with a sensitivity of 77.1% (95% confidence interval [CI] 62.7%–88.0%) and a specificity of 93.8% (95% CI 82.8%–98.7%).[94]
- Gynecologic ultrasonography, specifically looking for small ovarian follicles. These are believed to be the result of disturbed ovarian function with failed ovulation, reflected by the infrequent or absent menstruation that is typical of the condition. In a normal menstrual cycle, one egg is released from a dominant follicle – in essence, a cyst that bursts to release the egg. After ovulation, the follicle remnant is transformed into a progesterone-producing corpus luteum, which shrinks and disappears after approximately 12–14 days. In PCOS, there is a so-called "follicular arrest"; i.e., several follicles develop to a size of 5–7 mm, but not further. No single follicle reaches the preovulatory size (16 mm or more). According to the Rotterdam criteria, which are widely used for diagnosis of PCOS,[10] 12 or more small follicles should be seen in a suspect ovary on ultrasound examination.[21] More recent research suggests that there should be at least 25 follicles in an ovary to designate it as having polycystic ovarian morphology (PCOM) in women aged 18–35 years.[95] The follicles may be oriented in the periphery, giving the appearance of a 'string of pearls'.[96] If a high-resolution transvaginal ultrasonography machine is not available, an ovarian volume of at least 10 ml is regarded as an acceptable definition of having polycystic ovarian morphology. rather than follicle count.[95]
- Laparoscopic examination may reveal a thickened, smooth, pearl-white outer surface of the ovary. (This would usually be an incidental finding if laparoscopy were performed for some other reason, as it would not be routine to examine the ovaries in this way to confirm a diagnosis of PCOS.)[97]
- Serum (blood) levels of androgens, including androstenedione and testosterone may be elevated.[22] Dehydroepiandrosterone sulfate (DHEA-S) levels above 700–800 µg/dL are highly suggestive of adrenal dysfunction because DHEA-S is made exclusively by the adrenal glands.[98][93] The free testosterone level is thought to be the best measure,[93][99] with approximately 60 per cent of PCOS patients demonstrating supranormal levels.[30]
Some other blood tests are suggestive but not diagnostic. The ratio of LH (luteinizing hormone) to FSH (follicle-stimulating hormone), when measured in international units, is elevated in women with PCOS. Common cut-offs to designate abnormally high LH/FSH ratios are 2:1[100] or 3:1[93] as tested on day 3 of the menstrual cycle. The pattern is not very sensitive; a ratio of 2:1 or higher was present in less than 50% of women with PCOS in one study.[100] There are often low levels of sex hormone-binding globulin,[93] in particular among obese or overweight women.[101] Anti-Müllerian hormone (AMH) is increased in PCOS, and may become part of its diagnostic criteria.[102][103][104]
Glucose tolerance testing
- Two-hour oral glucose tolerance test (GTT) in women with risk factors (obesity, family history, history of gestational diabetes)[22] may indicate impaired glucose tolerance (insulin resistance) in 15–33% of women with PCOS.[93] Frank diabetes can be seen in 65–68% of women with this condition.[105] Insulin resistance can be observed in both normal weight and overweight people, although it is more common in the latter (and in those matching the stricter NIH criteria for diagnosis); 50–80% of people with PCOS may have insulin resistance at some level.[22]
- Fasting insulin level or GTT with insulin levels (also called IGTT). Elevated insulin levels have been helpful to predict response to medication and may indicate women needing higher doses of metformin or the use of a second medication to significantly lower insulin levels. Elevated blood sugar and insulin values do not predict who responds to an insulin-lowering medication, low-glycemic diet, and exercise. Many women with normal levels may benefit from combination therapy. A hypoglycemic response in which the two-hour insulin level is higher and the blood sugar lower than fasting is consistent with insulin resistance. A mathematical derivation known as the HOMAI, calculated from the fasting values in glucose and insulin concentrations, allows a direct and moderately accurate measure of insulin sensitivity (glucose-level x insulin-level/22.5).[106]
Management
PCOS has no cure.[5] Treatment may involve lifestyle changes such as weight loss and exercise.[10][11]
Recent research suggests that daily exercise including both aerobic and strength activities can improve hormone imbalances.[107]
Birth control pills may help with improving the regularity of periods, excess hair growth, and acne.[12] Combined oral contraceptives are especially effective, and used as the first-line of treatment to reduce acne and hirsutism, and regulate menstrual cycle. This is especially the case of adolescents.[107]
Metformin and anti-androgens may also help.[12] Other typical acne treatments and hair removal techniques may be used.[12] Efforts to improve fertility include weight loss, metformin, and ovulation induction using clomiphene or letrozole.[108] In vitro fertilization is used by some in whom other measures are not effective.[108]
Certain cosmetic procedures may also help alleviate symptoms in some cases. For example, the use of laser hair removal, electrolysis, or general waxing, plucking and shaving are all effective methods for reducing hirsutism.[35] The primary treatments for PCOS include lifestyle changes and use of medications.[109]
Goals of treatment may be considered under four categories:[citation needed]
- Lowering of insulin resistance
- Reducing Androgen and Testosterone levels
- Restoration of fertility
- Treatment of hirsutism or acne
- Restoration of regular menstruation, and prevention of endometrial hyperplasia and endometrial cancer
In each of these areas, there is considerable debate as to the optimal treatment. One of the major factors underlying the debate is the lack of large-scale clinical trials comparing different treatments. Smaller trials tend to be less reliable and hence may produce conflicting results. General interventions that help to reduce weight or insulin resistance can be beneficial for all these aims, because they address what is believed to be the underlying cause.[110] As PCOS appears to cause significant emotional distress, appropriate support may be useful.[111]
Diet
Where PCOS is associated with overweight or obesity, successful weight loss is the most effective method of restoring normal ovulation/menstruation. The American Association of Clinical Endocrinologists guidelines recommend a goal of achieving 10–15% weight loss or more, which improves insulin resistance and all[clarification needed] hormonal disorders.[112] Still, many women find it very difficult to achieve and sustain significant weight loss. Insulin resistance itself can cause increased food cravings and lower energy levels, which can make it difficult to lose weight on a regular weight-loss diet. A scientific review in 2013 found similar improvements in weight, body composition and pregnancy rate, menstrual regularity, ovulation, hyperandrogenism, insulin resistance, lipids, and quality of life to occur with weight loss, independent of diet composition.[113] Still, a low GI diet, in which a significant portion of total carbohydrates is obtained from fruit, vegetables, and whole-grain sources, has resulted in greater menstrual regularity than a macronutrient-matched healthy diet.[113]
Reducing intake of food groups that cause inflammation, such as dairy, sugars and simple carbohydrates, can be beneficial.[35]
A mediterranean diet is often very effective due to its anti-inflammatory and anti-oxidative properties.[107]
Vitamin D deficiency may play some role in the development of the metabolic syndrome, and treatment of any such deficiency is indicated.[114][115] However, a systematic review of 2015 found no evidence that vitamin D supplementation reduced or mitigated metabolic and hormonal dysregulations in PCOS.[116] As of 2012, interventions using dietary supplements to correct metabolic deficiencies in people with PCOS had been tested in small, uncontrolled and nonrandomized clinical trials; the resulting data are insufficient to recommend their use.[117]
Medications
Medications for PCOS include oral contraceptives and metformin. The oral contraceptives increase sex hormone binding globulin production, which increases binding of free testosterone. This reduces the symptoms of hirsutism caused by high testosterone and regulates return to normal menstrual periods.[114] Anti-androgens such as finasteride, flutamide, spironolactone, and bicalutamide do not show advantages over oral contraceptives, but could be an option for people who do not tolerate them.[118] Finasteride is the only oral medication for the treatment of androgenic alopecia, that is FDA approved.[35]
Metformin is a medication commonly used in type 2 diabetes mellitus to reduce insulin resistance, and is used off label (in the UK, US, AU and EU) to treat insulin resistance seen in PCOS. In many cases, metformin also supports ovarian function and return to normal ovulation.[114][119] A newer insulin resistance medication class, the thiazolidinediones (glitazones), have shown equivalent efficacy to metformin, but metformin has a more favorable side effect profile.[120][121] The United Kingdom's National Institute for Health and Clinical Excellence recommended in 2004 that women with PCOS and a body mass index above 25 be given metformin when other therapy has failed to produce results.[122][123] Metformin may not be effective in every type of PCOS, and therefore there is some disagreement about whether it should be used as a general first line therapy.[124] In addition to this, metformin is associated with several unpleasant side effects: including abdominal pain, metallic taste in the mouth, diarrhoea and vomiting.[125] Metformin is thought to be safe to use during pregnancy (pregnancy category B in the US).[126] A review in 2014 concluded that the use of metformin does not increase the risk of major birth defects in women treated with metformin during the first trimester.[127] Liraglutide may reduce weight and waist circumference in people with PCOS more than other medications.[128] The use of statins in the management of underlying metabolic syndrome remains unclear.[109]
It can be difficult to become pregnant with PCOS because it causes irregular ovulation. Medications to induce fertility when trying to conceive include the ovulation inducer clomiphene or pulsatile leuprorelin. Evidence from randomised controlled trials suggests that in terms of live birth, metformin may be better than placebo, and metform plus clomiphene may be better than clomiphene alone, but that in both cases women may be more likely to experience gastrointestinal side effects with metformin.[129]
Infertility
Not all women with PCOS have difficulty becoming pregnant. But some women with PCOS may have difficulty getting pregnant since their body does not produce the hormones necessary for regular ovulation.[130] PCOS might also increase the risk of miscarriage or premature delivery. However, it is possible to have a normal pregnancy. Including medical care and a healthy lifestyle to follow.[citation needed]
For those that do, anovulation or infrequent ovulation is a common cause and PCOS is the main cause of anovulatory infertility.[131] Other factors include changed levels of gonadotropins, hyperandrogenemia, and hyperinsulinemia.[132] Like women without PCOS, women with PCOS that are ovulating may be infertile due to other causes, such as tubal blockages due to a history of sexually transmitted diseases.[133]
For overweight anovulatory women with PCOS, weight loss and diet adjustments, especially to reduce the intake of simple carbohydrates, are associated with resumption of natural ovulation.[134] Digital health interventions have been shown to be particularly effective in providing combined therapy to manage PCOS through both lifestyle changes and medication.[135]
Femara is an alternative medicine that raises FSH levels and promote the development of the follicle.[35]
For those women that after weight loss still are anovulatory or for anovulatory lean women, then ovulation induction using the medications letrozole or clomiphene citrate are the principal treatments used to promote ovulation.[136][137][138] Clomiphene can cause mood swings and abdominal cramping for some.[35]
Previously, the anti-diabetes medication metformin was recommended treatment for anovulation, but it appears less effective than letrozole or clomiphene.[139][140]
For women not responsive to letrozole or clomiphene and diet and lifestyle modification, there are options available including assisted reproductive technology procedures such as controlled ovarian hyperstimulation with follicle-stimulating hormone (FSH) injections followed by in vitro fertilisation (IVF).[141]
Though surgery is not commonly performed, the polycystic ovaries can be treated with a laparoscopic procedure called "ovarian drilling" (puncture of 4–10 small follicles with electrocautery, laser, or biopsy needles), which often results in either resumption of spontaneous ovulations[114] or ovulations after adjuvant treatment with clomiphene or FSH.[142] (Ovarian wedge resection is no longer used as much due to complications such as adhesions and the presence of frequently effective medications.) There are, however, concerns about the long-term effects of ovarian drilling on ovarian function.[114]
Mental Health
Although women with PCOS are far more likely to have depression than women without, the evidence for anti-depressant use in women with PCOS remains inconclusive.[143] However, the pathophysiology of depression and mental stress during PCOS is linked to various changes including psychological changes such as high activity of pro-inflammatory markers and immune system during stress.[144]
PCOS is associated with other mental health related conditions besides depression such as anxiety, bipolar disorder, and obsessive–compulsive disorder.[33]
Hirsutism and acne
When appropriate (e.g., in women of child-bearing age who require contraception), a standard contraceptive pill is frequently effective in reducing hirsutism.[114] Progestogens such as norgestrel and levonorgestrel should be avoided due to their androgenic effects.[114] Metformin combined with an oral contraceptive may be more effective than either metformin or the oral contraceptive on its own.[145]
In the case of taking medication for acne, Kelly Morrow-Baez PHD, in her exposition titled Thriving with PCOS, informs that it "takes time for medications to adjust hormone levels, and once those hormone levels are adjusted, it takes more time still for pores to be unclogged of overproduced oil and for any bacterial infections under the skin to clear up before you will see discernible results." (p. 138) [35]
Other medications with anti-androgen effects include flutamide,[146] and spironolactone,[114] which can give some improvement in hirsutism. Metformin can reduce hirsutism, perhaps by reducing insulin resistance, and is often used if there are other features such as insulin resistance, diabetes, or obesity that should also benefit from metformin. Eflornithine (Vaniqa) is a medication that is applied to the skin in cream form, and acts directly on the hair follicles to inhibit hair growth. It is usually applied to the face.[114] 5-alpha reductase inhibitors (such as finasteride and dutasteride) may also be used;[147] they work by blocking the conversion of testosterone to dihydrotestosterone (the latter of which responsible for most hair growth alterations and androgenic acne).
Although these agents have shown significant efficacy in clinical trials (for oral contraceptives, in 60–100% of individuals[114]), the reduction in hair growth may not be enough to eliminate the social embarrassment of hirsutism, or the inconvenience of plucking or shaving. Individuals vary in their response to different therapies. It is usually worth trying other medications if one does not work, but medications do not work well for all individuals.[148]
Menstrual irregularity
If fertility is not the primary aim, then menstruation can usually be regulated with a contraceptive pill.[114] The purpose of regulating menstruation, in essence, is for the woman's convenience, and perhaps her sense of well-being; there is no medical requirement for regular periods, as long as they occur sufficiently often.[149]
If a regular menstrual cycle is not desired, then therapy for an irregular cycle is not necessarily required. Most experts say that, if a menstrual bleed occurs at least every three months, then the endometrium (womb lining) is being shed sufficiently often to prevent an increased risk of endometrial abnormalities or cancer.[150] If menstruation occurs less often or not at all, some form of progestogen replacement is recommended.[147]
Alternative medicine
A 2017 review concluded that while both myo-inositol and D-chiro-inositols may regulate menstrual cycles and improve ovulation, there is a lack of evidence regarding effects on the probability of pregnancy.[151][152] A 2012 and 2017 review have found myo-inositol supplementation appears to be effective in improving several of the hormonal disturbances of PCOS.[153][154] Myo-inositol reduces the amount of gonadotropins and the length of controlled ovarian hyperstimulation in women undergoing in vitro fertilization.[155] A 2011 review found not enough evidence to conclude any beneficial effect from D-chiro-inositol.[156] There is insufficient evidence to support the use of acupuncture, current studies are inconclusive and there's a need for additional randomized controlled trials.[157][158]
Epidemiology
PCOS is the most common endocrine disorder among women between the ages of 18 and 44.[22] It affects approximately 2% to 20% of this age group depending on how it is defined.[8][13] When someone is infertile due to lack of ovulation, PCOS is the most common cause and could guide to patients' diagnosis.[4] The earliest known description of what is now recognized as PCOS dates from 1721 in Italy.[159]
The prevalence of PCOS depends on the choice of diagnostic criteria. The World Health Organization estimates that it affects 116 million women worldwide as of 2010 (3.4% of women).[160] Another estimate indicates that 7% of women of reproductive age are affected.[161] Another study using the Rotterdam criteria found that about 18% of women had PCOS, and that 70% of them were previously undiagnosed.[22] Prevalence also varies across countries due to lack of large-scale scientific studies; India, for example, has a purported rate of 1 in 5 women having PCOS.[162]
There are few studies that have investigated the racial differences in cardiometabolic factors in women with PCOS. There is also limited data on the racial differences in the risk of metabolic syndrome and cardiovascular disease in adolescents and young adults with PCOS.[163] The first study to comprehensively examine racial differences discovered notable racial differences in risk factors for cardiovascular disease. African American women were found to be significantly more obese, with a significantly higher prevalence of metabolic syndrome compared to white adult women with PCOS.[164] It is important for the further research of racial differences among women with PCOS, to ensure that every woman that is affected by PCOS has the available resources for management.[165][166]
Ultrasonographic findings of polycystic ovaries are found in 8–25% of women non-affected by the syndrome.[167][168][169][170] 14% women on oral contraceptives are found to have polycystic ovaries.[168] Ovarian cysts are also a common side effect of levonorgestrel-releasing intrauterine devices (IUDs).[171]
There are few studies that have investigated the racial differences in cardiometabolic factors in women with PCOS.[172]
History
The condition was first described in 1935 by American gynecologists Irving F. Stein, Sr. and Michael L. Leventhal, from whom its original name of Stein–Leventhal syndrome is taken.[91][21] Stein and Leventhal first described PCOS as an endocrine disorder in the United States, and since then, it has become recognized as one of the most common causes of oligo ovulatory infertility among women.[50]
The earliest published description of a person with what is now recognized as PCOS was in 1721 in Italy.[159] Cyst-related changes to the ovaries were described in 1844.[159]
Etymology
Other names for this syndrome include polycystic ovarian syndrome, polycystic ovary disease, functional ovarian hyperandrogenism, ovarian hyperthecosis, sclerocystic ovary syndrome, and Stein–Leventhal syndrome. The eponymous last option is the original name; it is now used, if at all, only for the subset of women with all the symptoms of amenorrhea with infertility, hirsutism, and enlarged polycystic ovaries.[91]
Most common names for this disease derive from a typical finding on medical images, called a polycystic ovary. A polycystic ovary has an abnormally large number of developing eggs visible near its surface, looking like many small cysts.[91]
Society and culture
In 2005, 4 million cases of PCOS were reported in the US, costing $4.36 billion in healthcare costs.[173] In 2016 out of the National Institute Health's research budget of $32.3 billion for that year, 0.1% was spent on PCOS research.[174] Among those aged between 14 and 44, PCOS is conservatively estimated to cost $4.37 billion per year.[23]
As opposed to women in the general population, women with PCOS experience higher rates of depression and anxiety. International guidelines and Indian guidelines suggest psychosocial factors should be considered in women with PCOS, as well as screenings for depression and anxiety.[175] Globally, this aspect has been increasingly focused on because it reflects the true impact of PCOS on the lives of patients. Research shows that PCOS adversely impacts a patient's quality of life.[175]
Public figures
A number of celebrities and public figures have spoken about their experiences with PCOS, including:
- Victoria Beckham[176]
- Maci Bookout[177]
- Frankie Bridge[178]
- Harnaam Kaur[179]
- Jaime King[180]
- Chrisette Michele[181]
- Lea Michele[182]
- Keke Palmer[183]
- Sasha Pieterse[184][185]
- Daisy Ridley[186]
- Romee Strijd[187]
- Lee Tilghman[188]
See also
- Androgen-dependent syndromes
References
- ↑ "Terms and thresholds for the ultrasound evaluation of the ovaries in women with hyperandrogenic anovulation". Human Reproduction Update 20 (3): 463–464. 2014. doi:10.1093/humupd/dmu005. PMID 24516084.
- ↑ "Stein-Leventhal syndrome.". Encyclopedia Britannica. 2017. https://www.britannica.com/science/Stein-Leventhal-syndrome.[better source needed]
- ↑ 3.0 3.1 3.2 "What are the symptoms of PCOS?". 29 September 2022. https://www.nichd.nih.gov/health/topics/pcos/conditioninfo/symptoms.
- ↑ 4.0 4.1 4.2 4.3 4.4 "Polycystic Ovary Syndrome (PCOS): Condition Information". National Institute of Child Health and Human Development. January 31, 2017. https://www.nichd.nih.gov/health/topics/pcos/conditioninfo.
- ↑ 5.0 5.1 "Is there a cure for PCOS?". 31 January 2017. https://www.nichd.nih.gov/health/topics/pcos/conditioninfo/cure.
- ↑ 6.0 6.1 "Genetic, hormonal and metabolic aspects of PCOS: an update". Reproductive Biology and Endocrinology 14 (1): 38. July 2016. doi:10.1186/s12958-016-0173-x. PMID 27423183.
- ↑ 7.0 7.1 7.2 7.3 7.4 "The role of genes and environment in the etiology of PCOS". Endocrine 30 (1): 19–26. August 2006. doi:10.1385/ENDO:30:1:19. PMID 17185788.
- ↑ 8.0 8.1 8.2 8.3 "What causes PCOS?". 29 September 2022. https://www.nichd.nih.gov/health/topics/pcos/conditioninfo/causes.
- ↑ 9.0 9.1 9.2 "How do health care providers diagnose PCOS?". 29 September 2022. https://www.nichd.nih.gov/health/topics/pcos/conditioninfo/diagnose.
- ↑ 10.0 10.1 10.2 10.3 "Metabolic Syndrome: Polycystic Ovary Syndrome". FP Essentials 435: 30–42. August 2015. PMID 26280343.
- ↑ 11.0 11.1 "Androgens in polycystic ovary syndrome: the role of exercise and diet". Seminars in Reproductive Medicine 27 (4): 306–315. July 2009. doi:10.1055/s-0029-1225258. PMID 19530064.
- ↑ 12.0 12.1 12.2 12.3 National Institutes of Health (NIH) (2014-07-14). "Treatments to Relieve Symptoms of PCOS". http://www.nichd.nih.gov/health/topics/PCOS/conditioninfo/Pages/relieve.aspx.
- ↑ 13.0 13.1 "Diagnostic Criteria and Epidemiology of PCOS". Polycystic Ovary Syndrome Current and Emerging Concepts. Dordrecht: Springer. 2013. p. 7. ISBN 9781461483946. https://books.google.com/books?id=DTUnAQAAQBAJ&q=Polycystic%20Ovary%20Syndrome%3B%20Subtitle%3A%20Current%20and%20Emerging%20Concepts%3B%20Part%20I&pg=PA7.
- ↑ "American Association of Clinical Endocrinologists, American College of Endocrinology, and androgen excess and PCOS society disease state clinical review: guide to the best practices in the evaluation and treatment of polycystic ovary syndrome-part 1.". Endocrine Practice 21 (11): 1291–1300. November 2015. doi:10.4158/EP15748.DSC. PMID 26509855.
- ↑ 15.0 15.1 "Renaming PCOS--a two-state solution". The Journal of Clinical Endocrinology and Metabolism 98 (11): 4325–4328. November 2013. doi:10.1210/jc.2013-2040. PMID 24009134. "Around 20% of European women have polycystic ovaries (the prevalence is even higher in some other populations) but approximately two-thirds of these women do not have PCOS".
- ↑ Khan MJ, Ullah A, Basit S. Genetic Basis of Polycystic Ovary Syndrome (PCOS): Current Perspectives. Appl Clin Genet. 2019 Dec 24;12:249-260. doi: 10.2147/TACG.S200341. PMID 31920361; PMCID: PMC6935309.
- ↑ "An update of genetic basis of PCOS pathogenesis". Archives of Endocrinology and Metabolism 62 (3): 352–361. June 2018. doi:10.20945/2359-3997000000049. PMID 29972435.
- ↑ "Shedding new light on female fertility: The role of vitamin D". Reviews in Endocrine & Metabolic Disorders 18 (3): 273–283. September 2017. doi:10.1007/s11154-017-9407-2. PMID 28102491.
- ↑ 19.0 19.1 "Polycystic Ovarian Syndrome and Fertility". Clinical Obstetrics and Gynecology 64 (1): 65–75. March 2021. doi:10.1097/GRF.0000000000000595. PMID 33337743.
- ↑ "Geographical Prevalence of Polycystic Ovary Syndrome as Determined by Region and Race/Ethnicity". International Journal of Environmental Research and Public Health 15 (11): 2589. November 2018. doi:10.3390/ijerph15112589. PMID 30463276. "indigenous Australian women could have a prevalence as high as 26%".
- ↑ 21.0 21.1 21.2 21.3 21.4 21.5 21.6 21.7 Polycystic Ovarian Syndrome at eMedicine
- ↑ 22.00 22.01 22.02 22.03 22.04 22.05 22.06 22.07 22.08 22.09 22.10 22.11 22.12 22.13 22.14 "Polycystic ovary syndrome: a complex condition with psychological, reproductive and metabolic manifestations that impacts on health across the lifespan". BMC Medicine 8 (1): 41. June 2010. doi:10.1186/1741-7015-8-41. PMID 20591140.
- ↑ 23.0 23.1 "Controversy in clinical endocrinology: diagnosis of polycystic ovarian syndrome: the Rotterdam criteria are premature". The Journal of Clinical Endocrinology and Metabolism 91 (3): 781–785. March 2006. doi:10.1210/jc.2005-2153. PMID 16418211.
- ↑ 24.0 24.1 Rotterdam ESHRE/ASRM-Sponsored PCOS consensus workshop group (January 2004). "Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome (PCOS)". Human Reproduction 19 (1): 41–47. doi:10.1093/humrep/deh098. PMID 14688154.
- ↑ "Diagnosis of polycystic ovary syndrome: from NIH criteria to ESHRE-ASRM guidelines". Minerva Ginecologica 56 (1): 1–6. February 2004. NAID 10025610607. PMID 14973405. https://www.minervamedica.it/en/journals/minerva-obstetrics-gynecology/article.php?cod=R09Y2004N01A0001.
- ↑ "Definitions, prevalence and symptoms of polycystic ovaries and polycystic ovary syndrome". Best Practice & Research. Clinical Obstetrics & Gynaecology 18 (5): 671–683. October 2004. doi:10.1016/j.bpobgyn.2004.05.001. PMID 15380140.
- ↑ 27.0 27.1 "What We Talk About When We Talk About PCOS" (in en). 23 January 2019. https://www.vice.com/en/article/zmae5j/what-we-talk-about-when-we-talk-about-pcos.
- ↑ "Polycystic Ovary Syndrome (PCOS)" (in en). 2022-02-28. https://www.hopkinsmedicine.org/health/conditions-and-diseases/polycystic-ovary-syndrome-pcos.
- ↑ "Diagnosis of Hyperandrogenism in Female Adolescents". Armenian Health Network, Health.am. Sep 21, 2006. http://www.health.am/gyneco/more/diagnosis-of-hyperandrogenism-in-female/.
- ↑ 30.0 30.1 "Prevalence of hyperandrogenemia in the polycystic ovary syndrome diagnosed by the National Institutes of Health 1990 criteria". Fertility and Sterility 93 (6): 1938–1941. April 2010. doi:10.1016/j.fertnstert.2008.12.138. PMID 19249030.
- ↑ 31.0 31.1 "The effect of serum and intrafollicular insulin resistance parameters and homocysteine levels of nonobese, nonhyperandrogenemic polycystic ovary syndrome patients on in vitro fertilization outcome". Fertility and Sterility 93 (6): 1864–1869. April 2010. doi:10.1016/j.fertnstert.2008.12.024. PMID 19171332.
- ↑ 32.0 32.1 "Lifestyle Interventions and Natural and Assisted Reproduction in Patients with PCOS". Infertility in Women with Polycystic Ovary Syndrome. Cham: Springer International Publishing. 2018. pp. 169–180. doi:10.1007/978-3-319-45534-1_13. ISBN 978-3-319-45533-4.
- ↑ 33.0 33.1 "Psychiatric disorders in women with polycystic ovary syndrome: a systematic review and meta-analysis". Endocrine 62 (2): 318–325. November 2018. doi:10.1007/s12020-018-1692-3. PMID 30066285.
- ↑ "Lifestyle Modifications in Polycystic Ovarian Syndrome". Decoding Polycystic Ovarian Syndrome (PCOS). Jaypee Brothers Medical Publishers (P) Ltd.. 2018. pp. 195. doi:10.5005/jp/books/13089_17. ISBN 9789386322852.
- ↑ 35.0 35.1 35.2 35.3 35.4 35.5 35.6 Thriving with PCOS: Lifestyle Strategies to Successfully Manage Polycystic Ovary Syndrome. Rowman & Littlefield Publishers. 2018.
- ↑ "Polycystic Ovarian Disease". StatPearls. StatPearls Publishing. 2023. https://www.ncbi.nlm.nih.gov/books/NBK459251/.
- ↑ "Adiposity and metabolic dysfunction in polycystic ovary syndrome". Hormone Molecular Biology and Clinical Investigation 21 (2): 107–116. February 2015. doi:10.1515/hmbci-2015-0008. PMID 25781555.
- ↑ "Effects of androgens on insulin action in women: is androgen excess a component of female metabolic syndrome?". Diabetes/Metabolism Research and Reviews 24 (7): 520–532. October 2008. doi:10.1002/dmrr.872. PMID 18615851.
- ↑ "Debates Regarding Lean Patients with Polycystic Ovary Syndrome: A Narrative Review". Journal of Human Reproductive Sciences 10 (3): 154–161. 2017. doi:10.4103/jhrs.JHRS_77_17. PMID 29142442.
- ↑ "Obese and Non-obese Polycystic Ovarian Syndrome: Comparison of Clinical, Metabolic, Hormonal Parameters, and their Differential Response to Clomiphene". Indian Journal of Endocrinology and Metabolism 23 (2): 257–262. 2019. doi:10.4103/ijem.IJEM_637_18. PMID 31161114.
- ↑ "Lean PCOS may be a genetically distinct from obese PCOS: lean women with polycystic ovary syndrome and their relatives have no increased risk of T2DM". Human Reproduction (Oxford, England: Oxford Univ Press) 33: 454. July 2018. doi:10.26226/morressier.5af300b3738ab10027aa99cd.
- ↑ "Debates Regarding Lean Patients with Polycystic Ovary Syndrome: A Narrative Review". Journal of Human Reproductive Sciences 10 (3): 154–161. 2017. doi:10.4103/jhrs.jhrs_77_17. PMID 29142442.
- ↑ 43.0 43.1 "Type 2 Diabetes and Metabolic Syndrome in Children and Adolescents". Staged Diabetes Management: A Systematic Approach (2nd ed.). John Wiley & Sons. 11 January 2007. pp. 213–. ISBN 978-0-470-06171-8. OCLC 1039172275. https://books.google.com/books?id=dQVfgd71NWEC&pg=PA213. "Diagnosis and treatment. The first diagnostic test [of PCOS] is measurement of total testosterone and free testosterone by radioimmunoassay. If total testosterone is between 50 ng/dL and 200 ng/dL above normal (<2.5 ng/dL) PCOS is present. If >200 ng/dL then serum DHEA-S should be measured. If total testosterone or DHEA-S >700 μg/dL then rule out an ovarian or adrenal tumor. These tests should be followed by tests for hypothyroidism, hyperprolactinemia, and adrenal hyperplasia."
- ↑ 44.0 44.1 "Sexual dysfunction in polycystic ovary syndrome: a systematic review and meta-analysis". Hormones (Athens) 19 (3): 413–423. September 2020. doi:10.1007/s42000-020-00210-0. PMID 32462512. "A total of 5366 women with PCOS from 21 studies were included. [...] Women with PCOS [...] [had higher] serum total testosterone level (2.34 ± 0.58 nmol/L vs 1.57 ± 0.60 nmol/L, p < 0.001) compared with women without PCOS. [...] PCOS is characterized by high levels of androgens (dehydroepiandrosterone, androstenedione, and testosterone) and luteinizing hormone (LH), and increased LH/follicle stimulating hormone (FSH) ratio [52].".
- ↑ 45.0 45.1 "Polycystic ovary syndrome: the spectrum of the disorder in 1741 patients". Hum Reprod 10 (8): 2107–11. August 1995. doi:10.1093/oxfordjournals.humrep.a136243. PMID 8567849. "The criteria for the diagnosis of the polycystic ovary syndrome (PCOS) have still not been agreed universally. A population of 1741 women with PCOS were studied, all of whom had polycystic ovaries seen by ultrasound scan. The frequency distributions of the serum concentrations of [...] testosterone [...] were determined and compared with the symptoms and signs of PCOS. [...] A rising serum concentration of testosterone [mean and 95th percentiles 2.6 (1.1-4.8) nmol/1] was associated with an increased risk of hirsutism, infertility and cycle disturbance. [...] If the serum testosterone concentration is >4.8 nmol/1, other causes of hyperandrogenism should be excluded.".
- ↑ "Utilization of commercial laboratory results in management of hyperandrogenism in women". Endocr Pract 4 (1): 1–10. 1998. doi:10.4158/EP.4.1.1. PMID 15251757.
- ↑ "Total testosterone assays in women with polycystic ovary syndrome: precision and correlation with hirsutism". J Clin Endocrinol Metab 95 (12): 5305–13. December 2010. doi:10.1210/jc.2010-1123. PMID 20826578. "Design and Setting: We conducted a blinded laboratory study including masked duplicate samples at three laboratories—two academic (University of Virginia, RIA; and Mayo Clinic, LC/MS) and one commercial (Quest, LC/MS). Participants and Interventions: Baseline testosterone levels from 596 women with PCOS who participated in a large, multicenter, randomized controlled infertility trial performed at academic health centers in the United States were run by varying assays, and results were compared. [...] The median testosterone level by RIA was 50 ng/dl (25th–75th percentile, 34–71 ng/dl); by LC/MS at Mayo, 47 ng/dl (25th–75th percentile, 34–65 ng/dl); and by LC/MS at Quest, 41 ng/dl (25th–75th percentile, 27–58 ng/dl) (Fig. 1). The minimum and maximum values detected by RIA were 8 and 189 ng/dl, respectively; by LC/MS at Mayo, 12 and 184 ng/dl, respectively; and by LC/MS at Quest, 1 and 205 ng/dl, respectively. [...] Our sample size was robust and the largest study to date examining quality control of total testosterone serum levels in women.".
- ↑ "Evaluation of Hormonal Status". Yen and Jaffe's Reproductive Endocrinology: Physiology, Pathophysiology, and Clinical Management (8th ed.). Elsevier. 2019. pp. 887–915.e4. doi:10.1016/B978-0-323-47912-7.00034-2. ISBN 9780323479127.
- ↑ Saadia, Z. (2020, August). Follicle stimulating hormone (LH: FSH) ratio in polycystic ovary syndrome (PCOS) - obese vs. non- obese women. Medical archives (Sarajevo, Bosnia and Herzegovina). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7520057/
- ↑ 50.0 50.1 50.2 "Risk of endometrial, ovarian and breast cancer in women with polycystic ovary syndrome: a systematic review and meta-analysis". Human Reproduction Update 20 (5): 748–758. 1 September 2014. doi:10.1093/humupd/dmu012. PMID 24688118.
- ↑ "Nonclassical congenital adrenal hyperplasia and the polycystic ovarian syndrome". Annals of the New York Academy of Sciences 687 (1): 193–205. May 1993. doi:10.1111/j.1749-6632.1993.tb43866.x. PMID 8323173. Bibcode: 1993NYASA.687..193N.
- ↑ "Polycystic ovary syndrome and endometrial carcinoma". Lancet 361 (9371): 1810–1812. May 2003. doi:10.1016/S0140-6736(03)13409-5. PMID 12781553.
- ↑ "Hyperinsulinemia in polycystic ovary syndrome correlates with increased cardiovascular risk independent of obesity". Fertility and Sterility 73 (1): 150–156. January 2000. doi:10.1016/S0015-0282(99)00468-9. PMID 10632431.
- ↑ "Impaired glucose tolerance, type 2 diabetes and metabolic syndrome in polycystic ovary syndrome: a systematic review and meta-analysis". Human Reproduction Update 16 (4): 347–363. 2010. doi:10.1093/humupd/dmq001. PMID 20159883.
- ↑ (in en) Clinical Reproductive Medicine and Surgery. Elsevier Health Sciences. 2007. p. 223. ISBN 978-0-323-03309-1. https://books.google.com/books?id=fOPtaEIKvcIC&pg=PA223.
- ↑ "Polycystic ovary syndrome (PCOS) - Symptoms and causes". https://www.mayoclinic.org/diseases-conditions/pcos/symptoms-causes/syc-20353439.
- ↑ "Anxiety and depression in polycystic ovary syndrome: a systematic review and meta-analysis". Human Reproduction 26 (9): 2442–2451. September 2011. doi:10.1093/humrep/der197. PMID 21725075.
- ↑ "Insulin resistance, polycystic ovary syndrome, and type 2 diabetes mellitus". Fertility and Sterility 77 (6): 1095–1105. June 2002. doi:10.1016/s0015-0282(02)03111-4. PMID 12057712.
- ↑ "PCOS, coronary heart disease, stroke and the influence of obesity: a systematic review and meta-analysis". Human Reproduction Update 17 (4): 495–500. 1 July 2011. doi:10.1093/humupd/dmr001. PMID 21335359.
- ↑ "Medical therapy in women with polycystic ovarian syndrome before and during pregnancy and lactation". Minerva Ginecologica 60 (1): 63–75. February 2008. PMID 18277353. https://www.minervamedica.it/en/journals/minerva-obstetrics-gynecology/article.php?cod=R09Y2008N01A0063.
- ↑ "Pregnancy complications in women with polycystic ovary syndrome". Seminars in Reproductive Medicine 26 (1): 72–84. January 2008. doi:10.1055/s-2007-992927. PMID 18181085.
- ↑ "Iron Deficiency Injectables Market: Global Industry Trends, Share, Size, Growth, Opportunity and Forecast 2020-2025". https://www.imarcgroup.com/iron-deficiency-injectables-market.
- ↑ 63.0 63.1 Page 836 (Section:Polycystic ovary syndrome) in: "Contemporary genetic technologies and female reproduction". Human Reproduction Update 17 (6): 829–847. 2011. doi:10.1093/humupd/dmr033. PMID 21896560.
- ↑ 64.0 64.1 64.2 64.3 "Molecular progress in infertility: polycystic ovary syndrome". Fertility and Sterility 78 (3): 569–576. September 2002. doi:10.1016/S0015-0282(02)03275-2. PMID 12215335.
- ↑ "Is foetal hyperexposure to androgens a cause of PCOS?". Human Reproduction Update 23 (4): 421–432. July 2017. doi:10.1093/humupd/dmx013. PMID 28531286.
- ↑ "Scientific Statement on the Diagnostic Criteria, Epidemiology, Pathophysiology, and Molecular Genetics of Polycystic Ovary Syndrome". Endocrine Reviews 36 (5): 487–525. October 2015. doi:10.1210/er.2015-1018. PMID 26426951.
- ↑ 67.0 67.1 "Polycystic ovarian disease: heritability and heterogeneity". Human Reproduction Update 7 (1): 3–7. 2001. doi:10.1093/humupd/7.1.3. PMID 11212071.
- ↑ 68.0 68.1 68.2 "Some new thoughts on the pathophysiology and genetics of polycystic ovary syndrome". Annals of the New York Academy of Sciences 997 (1): 42–48. November 2003. doi:10.1196/annals.1290.005. PMID 14644808. Bibcode: 2003NYASA.997...42S.
- ↑ 69.0 69.1 "POLYCYSTIC OVARY SYNDROME 1; PCOS1". McKusick-Nathans Institute of Genetic Medicine, Johns Hopkins University School of Medicine. 12 September 2011. http://omim.org/entry/184700.
- ↑ "The genetics of polycystic ovary syndrome". Best Practice & Research. Clinical Obstetrics & Gynaecology 18 (5): 707–718. October 2004. doi:10.1016/j.bpobgyn.2004.05.002. PMID 15380142.
- ↑ "Mutations in the genes encoding 11beta-hydroxysteroid dehydrogenase type 1 and hexose-6-phosphate dehydrogenase interact to cause cortisone reductase deficiency". Nature Genetics 34 (4): 434–439. August 2003. doi:10.1038/ng1214. PMID 12858176.
- ↑ "Polycystic ovary syndrome". The New England Journal of Medicine 352 (12): 1223–1236. March 2005. doi:10.1056/NEJMra041536. PMID 15788499.
- ↑ "Nutritional management in women with polycystic ovary syndrome: A review study". Diabetes & Metabolic Syndrome 11 (Suppl 1): S429–S432. November 2017. doi:10.1016/j.dsx.2017.03.030. PMID 28416368.
- ↑ "Polycystic Ovary Syndrome: Pathophysiology, Presentation, and Treatment With Emphasis on Adolescent Girls". Journal of the Endocrine Society 3 (8): 1545–1573. August 2019. doi:10.1210/js.2019-00078. PMID 31384717.
- ↑ "Developmental origins and future fate in PCOS". Seminars in Reproductive Medicine 32 (3): 157–158. May 2014. doi:10.1055/s-0034-1371086. PMID 24715509.
- ↑ "Androgen excess fetal programming of female reproduction: a developmental aetiology for polycystic ovary syndrome?". Human Reproduction Update 11 (4): 357–374. 2005. doi:10.1093/humupd/dmi013. PMID 15941725.
- ↑ "The relationship between polycystic ovary syndrome and antiepileptic drugs: a review of the evidence". Journal of Clinical Psychopharmacology 24 (3): 322–334. June 2004. doi:10.1097/01.jcp.0000125745.60149.c6. PMID 15118487.
- ↑ "Bisphenol A (BPA) and its potential role in the pathogenesis of the polycystic ovary syndrome (PCOS)". Gynecological Endocrinology 30 (4): 260–265. April 2014. doi:10.3109/09513590.2013.871517. PMID 24397396.
- ↑ 79.0 79.1 "Industrial endocrine disruptors and polycystic ovary syndrome". Journal of Endocrinological Investigation 36 (11): 1105–1111. December 2013. doi:10.1007/bf03346762. PMID 24445124.
- ↑ "A meta-analysis of polycystic ovary syndrome in women taking valproate for epilepsy". Epilepsy Research 97 (1–2): 73–82. November 2011. doi:10.1016/j.eplepsyres.2011.07.006. PMID 21820873.
- ↑ "Endocrine Disruptors" (in en). https://www.niehs.nih.gov/health/topics/agents/endocrine/index.cfm.
- ↑ "Environmental determinants of polycystic ovary syndrome". Fertility and Sterility 106 (1): 16–24. July 2016. doi:10.1016/j.fertnstert.2016.05.011. PMID 27240194.
- ↑ 83.0 83.1 83.2 83.3 "Insulin resistance and the polycystic ovary syndrome revisited: an update on mechanisms and implications". Endocrine Reviews 33 (6): 981–1030. December 2012. doi:10.1210/er.2011-1034. PMID 23065822.
- ↑ "The utility of the gonadotrophin releasing hormone (GnRH) test in the diagnosis of polycystic ovary syndrome (PCOS)". Endokrynologia Polska 62 (2): 120–128. 2011. ProQuest 2464206947. PMID 21528473. https://journals.viamedica.pl/endokrynologia_polska/article/view/25282.
- ↑ "Polycystic ovary syndrome, insulin resistance, and obesity: navigating the pathophysiologic labyrinth". Int J Reprod Med 2014: 71905. 2014. doi:10.1155/2014/719050. PMID 25763405.
- ↑ "Ultrasound assessment of polycystic ovaries: Ovarian volume and morphology; which is more accurate in making the diagnosis?!" (in en). The Egyptian Journal of Radiology and Nuclear Medicine 47 (1): 347–350. March 2016. doi:10.1016/j.ejrnm.2015.10.002. ISSN 0378-603X.
- ↑ "Mediators of inflammation in polycystic ovary syndrome in relation to adiposity". Mediators of Inflammation 2010: 758656. 2010. doi:10.1155/2010/758656. PMID 20396393.
- ↑ "Interactions between interferon gamma, tumour necrosis factor alpha, and interleukin-1 in modulating progesterone and oestradiol production by human luteinized granulosa cells in culture". Human Reproduction 7 (10): 1361–1364. November 1992. doi:10.1093/oxfordjournals.humrep.a137574. PMID 1291559.
- ↑ "Reactive oxygen species-induced oxidative stress in the development of insulin resistance and hyperandrogenism in polycystic ovary syndrome". The Journal of Clinical Endocrinology and Metabolism 91 (1): 336–340. January 2006. doi:10.1210/jc.2005-1696. PMID 16249279.
- ↑ "Circulating markers of oxidative stress and polycystic ovary syndrome (PCOS): a systematic review and meta-analysis". Human Reproduction Update 19 (3): 268–288. 2013. doi:10.1093/humupd/dms059. PMID 23303572.
- ↑ 91.0 91.1 91.2 91.3 Imaging in Polycystic Ovary Disease at eMedicine
- ↑ "Diagnostic criteria for polycystic ovary syndrome: pitfalls and controversies". Journal of Obstetrics and Gynaecology Canada 30 (8): 671–679. August 2008. doi:10.1016/S1701-2163(16)32915-2. PMID 18786289.
- ↑ 93.0 93.1 93.2 93.3 93.4 93.5 Polycystic Ovarian Syndrome~workup at eMedicine
- ↑ "Polycystic ovary syndrome: validated questionnaire for use in diagnosis". Canadian Family Physician 53 (6): 1042–7, 1041. June 2007. PMID 17872783.
- ↑ 95.0 95.1 "Definition and significance of polycystic ovarian morphology: a task force report from the Androgen Excess and Polycystic Ovary Syndrome Society". Human Reproduction Update 20 (3): 334–352. 2013. doi:10.1093/humupd/dmt061. PMID 24345633.
- ↑ Top 3 Differentials in Radiology. Thieme. 1 January 2011. p. 369. ISBN 978-1-60406-228-1. https://books.google.com/books?id=l9BmkWhvcXYC&pg=PA369. Retrieved 30 August 2014. "Ultrasound findings in PCOS include enlarged ovaries with peripheral follicles in a "string of pearls" configuration."
- ↑ "Laparoscopic ovarian drilling for ovulation induction in women with anovulatory polycystic ovary syndrome". The Cochrane Database of Systematic Reviews 2 (2): CD001122. February 2020. doi:10.1002/14651858.CD001122.pub5. PMID 32048270.
- ↑ "The clinical evaluation of hirsutism". Dermatologic Therapy 21 (5): 376–391. 2008. doi:10.1111/j.1529-8019.2008.00219.x. PMID 18844715.
- ↑ "Free testosterone, luteinizing hormone/follicle stimulating hormone ratio and pelvic sonography in relation to skin manifestations in patients with polycystic ovary syndrome". Saudi Medical Journal 28 (7): 1039–1043. July 2007. INIST:18933286. OCLC 151296412. PMID 17603706.
- ↑ 100.0 100.1 "Incidence of elevated LH/FSH ratio in polycystic ovary syndrome women with normo- and hyperinsulinemia". Roczniki Akademii Medycznej W Bialymstoku 48: 131–134. 2003. PMID 14737959.
- ↑ Black's Medical Dictionary (40 ed.). Lanham, MD: Scarecrow Press. 2002. p. 496. ISBN 0810849844.
- ↑ "Role of Anti-Müllerian Hormone in pathophysiology, diagnosis and treatment of Polycystic Ovary Syndrome: a review". Reproductive Biology and Endocrinology 13: 137. December 2015. doi:10.1186/s12958-015-0134-9. PMID 26691645.
- ↑ "The physiology and clinical utility of anti-Mullerian hormone in women". Human Reproduction Update 20 (3): 370–385. 2014. doi:10.1093/humupd/dmt062. PMID 24430863.
- ↑ "Anti-Müllerian hormone: ovarian reserve testing and its potential clinical implications". Human Reproduction Update 20 (5): 688–701. 2014. doi:10.1093/humupd/dmu020. PMID 24821925.
- ↑ "Diagnosis and follow-up of type 2 diabetes in women with PCOS: a role for OGTT?". European Journal of Endocrinology 179 (3): D1–D14. September 2018. doi:10.1530/EJE-18-0237. PMID 29921567.
- ↑ "Assessing Insulin Sensitivity and Resistance in Humans". Endotext. South Dartmouth (MA): MDText.com, Inc.. 2000. http://www.ncbi.nlm.nih.gov/books/NBK278954/. Retrieved 2022-10-19.
- ↑ 107.0 107.1 107.2 Polycystic Ovary Syndrome. 2022. doi:10.1016/c2018-0-03276-4. ISBN 9780128230459. https://doi.org/10.1016/C2018-0-03276-4.
- ↑ 108.0 108.1 National Institutes of Health (NIH) (2014-07-14). "Treatments for Infertility Resulting from PCOS". http://www.nichd.nih.gov/health/topics/PCOS/conditioninfo/Pages/infertility.aspx.
- ↑ 109.0 109.1 "Diagnosis and treatment of polycystic ovary syndrome: an Endocrine Society clinical practice guideline". The Journal of Clinical Endocrinology and Metabolism 98 (12): 4565–4592. December 2013. doi:10.1210/jc.2013-2350. PMID 24151290.
- ↑ "Management of the metabolic syndrome and type 2 diabetes through lifestyle modification". Annual Review of Nutrition 29: 223–256. 2009. doi:10.1146/annurev-nutr-080508-141200. PMID 19400751.
- ↑ "Emotional distress is a common risk in women with polycystic ovary syndrome: a systematic review and meta-analysis of 28 studies". Human Reproduction Update 18 (6): 638–651. 2012. doi:10.1093/humupd/dms029. PMID 22824735.
- ↑ "American association of clinical endocrinologists and American college of endocrinology comprehensive clinical practice guidelines for medical care of patients with obesity.". Endocrine Practice 22 (Suppl 3): 1–203. July 2016. doi:10.4158/EP161365.GL. PMID 27219496.
- ↑ 113.0 113.1 "Dietary composition in the treatment of polycystic ovary syndrome: a systematic review to inform evidence-based guidelines". Human Reproduction Update 19 (5): 432. 2013. doi:10.1093/humupd/dmt015. PMID 23727939.
- ↑ 114.00 114.01 114.02 114.03 114.04 114.05 114.06 114.07 114.08 114.09 114.10 Polycystic Ovarian Syndrome~treatment at eMedicine
- ↑ "The role of vitamin D in metabolic disturbances in polycystic ovary syndrome: a systematic review". European Journal of Endocrinology 169 (6): 853–865. December 2013. doi:10.1530/EJE-13-0617. PMID 24044903.
- ↑ "Serum Vitamin D Levels and Polycystic Ovary syndrome: A Systematic Review and Meta-Analysis". Nutrients 7 (6): 4555–4577. 2015. doi:10.3390/nu7064555. PMID 26061015.
- ↑ "Clinical update on screening, diagnosis and management of metabolic disorders and cardiovascular risk factors associated with polycystic ovary syndrome". Current Opinion in Endocrinology, Diabetes and Obesity 19 (6): 512–519. December 2012. doi:10.1097/med.0b013e32835a000e. PMID 23108199.
- ↑ "Efficacy and safety of anti-androgens in the management of polycystic ovary syndrome: a systematic review and meta-analysis of randomised controlled trials". eClinicalMedicine 63: 102162. September 2023. doi:10.1016/j.eclinm.2023.102162. PMID 37583655.
- ↑ "Metformin in polycystic ovary syndrome: systematic review and meta-analysis". BMJ 327 (7421): 951–953. October 2003. doi:10.1136/bmj.327.7421.951. PMID 14576245.
- ↑ "Metformin vs thiazolidinediones for treatment of clinical, hormonal and metabolic characteristics of polycystic ovary syndrome: a meta-analysis". Clinical Endocrinology 74 (3): 332–339. March 2011. doi:10.1111/j.1365-2265.2010.03917.x. PMID 21050251.
- ↑ "Metformin or thiazolidinedione therapy in PCOS?". Nature Reviews. Endocrinology 7 (3): 128–129. March 2011. doi:10.1038/nrendo.2011.16. Gale A250471047. PMID 21283123.
- ↑ National Institute for Health and Clinical Excellence. 11 Clinical guideline 11 : Fertility: assessment and treatment for people with fertility problems . London, 2004.
- ↑ "Metformin therapy for the management of infertility in women with polycystic ovary syndrome". Royal College of Obstetricians and Gynaecologists. December 2008. http://www.rcog.org.uk/files/rcog-corp/uploaded-files/SAC13metformin-minorrevision.pdf.
- ↑ "The use of metformin in the management of polycystic ovary syndrome and associated anovulatory infertility: the current evidence". Journal of Obstetrics and Gynaecology 29 (6): 467–472. August 2009. doi:10.1080/01443610902829414. PMID 19697191.
- ↑ NICE (December 2018). "Metformin Hydrochloride". NICE. https://bnf.nice.org.uk/drug/metformin-hydrochloride.html#sideEffects.
- ↑ "Metformin therapy during pregnancy: good for the goose and good for the gosling too?". Diabetes Care 34 (10): 2329–2330. October 2011. doi:10.2337/dc11-1153. PMID 21949224.
- ↑ "First-trimester exposure to metformin and risk of birth defects: a systematic review and meta-analysis". Human Reproduction Update 20 (5): 656–669. 1 September 2014. doi:10.1093/humupd/dmu022. PMID 24861556.
- ↑ "Pharmacologic therapy to induce weight loss in women who have obesity/overweight with polycystic ovary syndrome: a systematic review and network meta-analysis". Obesity Reviews 19 (10): 1424–1445. October 2018. doi:10.1111/obr.12720. PMID 30066361. https://discovery.ucl.ac.uk/id/eprint/10050648/1/Hardiman_revised%20MS%5B23061%5D.pdf.
- ↑ "Metformin for ovulation induction (excluding gonadotrophins) in women with polycystic ovary syndrome". The Cochrane Database of Systematic Reviews 12 (12): CD013505. December 2019. doi:10.1002/14651858.CD013505. PMID 31845767.
- ↑ "Erase the Dread and Stigma of PCOD" (in en). https://www.matria.in/blog/erase-the-dread-and-stigma-of-pcod/.
- ↑ "The management of anovulatory infertility in women with polycystic ovary syndrome: an analysis of the evidence to support the development of global WHO guidance". Human Reproduction Update 22 (6): 687–708. November 2016. doi:10.1093/humupd/dmw025. PMID 27511809.
- ↑ "Extra- and intra-ovarian factors in polycystic ovary syndrome: impact on oocyte maturation and embryo developmental competence". Human Reproduction Update 17 (1): 17–33. 2010. doi:10.1093/humupd/dmq032. PMID 20639519.
- ↑ "What are some causes of female infertility?". 31 January 2017. https://www.nichd.nih.gov/health/topics/infertility/conditioninfo/causes/causes-female.
- ↑ "The Influence of Diet on Ovulation Disorders in Women-A Narrative Review". Nutrients 14 (8): 1556. April 2022. doi:10.3390/nu14081556. PMID 35458118.
- ↑ "Transtheoretical model-based mobile health application for PCOS". Reproductive Health 19 (1): 117. May 2022. doi:10.1186/s12978-022-01422-w. PMID 35549736.
- ↑ "Aromatase inhibitors (letrozole) for ovulation induction in infertile women with polycystic ovary syndrome". The Cochrane Database of Systematic Reviews 2022 (9): CD010287. September 2022. doi:10.1002/14651858.CD010287.pub4. PMID 36165742.
- ↑ "Ovulation induction in polycystic ovary syndrome". Acta Obstetricia et Gynecologica Scandinavica 97 (10): 1162–1167. October 2018. doi:10.1111/aogs.13395. PMID 29889977.
- ↑ "Letrozole versus clomiphene citrate in polycystic ovary syndrome: a meta-analysis of randomized controlled trials". Archives of Gynecology and Obstetrics 297 (5): 1081–1088. May 2018. doi:10.1007/s00404-018-4688-6. PMID 29392438.
- ↑ "Role of metformin for ovulation induction in infertile patients with polycystic ovary syndrome (PCOS): a guideline". Fertility and Sterility 108 (3): 426–441. September 2017. doi:10.1016/j.fertnstert.2017.06.026. PMID 28865539.
- ↑ "Clomiphene, metformin, or both for infertility in the polycystic ovary syndrome". The New England Journal of Medicine 356 (6): 551–566. February 2007. doi:10.1056/NEJMoa063971. PMID 17287476.[non-primary source needed]
- ↑ "Management of infertility and prevention of ovarian hyperstimulation in women with polycystic ovary syndrome". Best Practice & Research. Clinical Obstetrics & Gynaecology 18 (5): 773–788. October 2004. doi:10.1016/j.bpobgyn.2004.05.006. PMID 15380146.
- ↑ "Clomiphene citrate co-treatment with low dose urinary FSH versus urinary FSH for clomiphene resistant PCOS: randomized controlled trial". Journal of Assisted Reproduction and Genetics 30 (11): 1477–1485. November 2013. doi:10.1007/s10815-013-0090-2. PMID 24014214.
- ↑ "Antidepressants for polycystic ovary syndrome". The Cochrane Database of Systematic Reviews 2013 (5): CD008575. May 2013. doi:10.1002/14651858.CD008575.pub2. PMID 23728677.
- ↑ "Does polycystic ovary syndrome start in childhood?". Pediatric Endocrinology Reviews 5 (4): 904–911. June 2008. PMID 18552753.
- ↑ "Metformin versus the combined oral contraceptive pill for hirsutism, acne, and menstrual pattern in polycystic ovary syndrome". The Cochrane Database of Systematic Reviews 2020 (8): CD005552. August 2020. doi:10.1002/14651858.CD005552.pub3. PMID 32794179.
- ↑ "Polycystic ovary syndrome – Treatment". United Kingdom: National Health Service. 17 October 2011. http://www.nhs.uk/Conditions/Polycystic-ovarian-syndrome/Pages/Treatment.aspx.
- ↑ 147.0 147.1 Polycystic Ovarian Syndrome~medication at eMedicine
- ↑ "Interventions for hirsutism (excluding laser and photoepilation therapy alone)". The Cochrane Database of Systematic Reviews 2015 (4): CD010334. April 2015. doi:10.1002/14651858.CD010334.pub2. PMID 25918921.
- ↑ "Irregular periods - NHS". Nhs.uk. 2020-10-21. https://www.nhs.uk/conditions/irregular-periods/. Retrieved 2022-07-19.
- ↑ "What are the health risks of PCOS?". Verity. 2011. http://www.verity-pcos.org.uk/guide_to_pcos/what_is_pcos/health_risks.
- ↑ "Inositol treatment of anovulation in women with polycystic ovary syndrome: a meta-analysis of randomised trials". BJOG 125 (3): 299–308. February 2018. doi:10.1111/1471-0528.14754. PMID 28544572. https://pure-oai.bham.ac.uk/ws/files/41620024/Pundir_et_al_Inositol_treatment_BJOG.pdf.
- ↑ "Effects of myoinositol and D-chiro inositol on hyperandrogenism and ovulation in women with polycystic ovary syndrome: a systematic review". Endocrine Abstracts. 20 October 2017. doi:10.1530/endoabs.50.P363.
- ↑ "Effects of myo-inositol in women with PCOS: a systematic review of randomized controlled trials". Gynecological Endocrinology 28 (7): 509–515. July 2012. doi:10.3109/09513590.2011.650660. PMID 22296306.
- ↑ "Effectiveness of myoinositol for polycystic ovary syndrome: a systematic review and meta-analysis". Endocrine 59 (1): 30–38. January 2018. doi:10.1007/s12020-017-1442-y. PMID 29052180.
- ↑ "Myo-inositol supplementation reduces the amount of gonadotropins and length of ovarian stimulation in women undergoing IVF: a systematic review and meta-analysis of randomized controlled trials". Archives of Gynecology and Obstetrics 298 (4): 675–684. October 2018. doi:10.1007/s00404-018-4861-y. PMID 30078122.
- ↑ "D-Chiro-inositol and its significance in polycystic ovary syndrome: a systematic review". Gynecological Endocrinology 27 (4): 256–262. April 2011. doi:10.3109/09513590.2010.538099. PMID 21142777.
- ↑ "Acupuncture for polycystic ovarian syndrome". The Cochrane Database of Systematic Reviews 2019 (7): CD007689. July 2019. doi:10.1002/14651858.CD007689.pub4. PMID 31264709.
- ↑ "Effect of Acupuncture and Clomiphene in Chinese Women With Polycystic Ovary Syndrome: A Randomized Clinical Trial". JAMA 317 (24): 2502–2514. June 2017. doi:10.1001/jama.2017.7217. PMID 28655015.
- ↑ 159.0 159.1 159.2 Polycystic Ovary Syndrome. Cambridge University Press. 2007-02-22. p. 4. ISBN 9781139462037. https://books.google.com/books?id=bpn1u9hziVgC&pg=PA4. Retrieved 29 March 2013.
- ↑ "Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010". Lancet 380 (9859): 2163–2196. December 2012. doi:10.1016/S0140-6736(12)61729-2. PMID 23245607.
- ↑ "New diagnosis of polycystic ovary syndrome". BMJ 356: i6456. January 2017. doi:10.1136/bmj.i6456. PMID 28082338.
- ↑ "One in five Indian women suffers from PCOS". 26 September 2019. https://www.thehindu.com/sci-tech/health/one-in-five-indian-women-suffers-from-pcos/article29513588.ece.
- ↑ "Racial influence on the polycystic ovary syndrome phenotype: a black and white case-control study". Fertility and Sterility 96 (1): 224–229.e2. July 2011. doi:10.1016/j.fertnstert.2011.05.002. PMID 21723443.
- ↑ "Black women with polycystic ovary syndrome (PCOS) have increased risk for metabolic syndrome (MET SYN) and cardiovascular disease (CVD) compared to white women with PCOS". Fertility and Sterility 100 (3): S100–S101. September 2013. doi:10.1016/j.fertnstert.2013.07.1707. ISSN 0015-0282.
- ↑ "Concerns and expectations in women with polycystic ovary syndrome vary across age and ethnicity: findings from PCOS Pearls Study". Frontiers in Endocrinology 14: 1175548. 2023. doi:10.3389/fendo.2023.1175548. PMID 37621648.
- ↑ "Recommendations from the 2023 International Evidence-based Guideline for the Assessment and Management of Polycystic Ovary Syndrome (2023)" (in en). https://www.asrm.org/practice-guidance/practice-committee-documents/recommendations-from-the-2023-international-evidence-based-guideline-for-the-assessment-and-management-of-polycystic-ovary-syndrome/.
- ↑ "Polycystic ovaries--a common finding in normal women". Lancet 1 (8590): 870–872. April 1988. doi:10.1016/s0140-6736(88)91612-1. PMID 2895373.
- ↑ 168.0 168.1 "How common are polycystic ovaries in normal women and what is their significance for the fertility of the population?". Clinical Endocrinology 37 (2): 127–134. August 1992. doi:10.1111/j.1365-2265.1992.tb02296.x. PMID 1395063.
- ↑ "The prevalence of polycystic ovaries on ultrasound scanning in a population of randomly selected women". The Australian & New Zealand Journal of Obstetrics & Gynaecology 34 (1): 67–72. February 1994. doi:10.1111/j.1479-828X.1994.tb01041.x. PMID 8053879.
- ↑ "Classification of normogonadotropic infertility: polycystic ovaries diagnosed by ultrasound versus endocrine characteristics of polycystic ovary syndrome". Fertility and Sterility 67 (3): 452–458. March 1997. doi:10.1016/S0015-0282(97)80068-4. PMID 9091329.
- ↑ "Intrauterine devices: an update". American Family Physician 89 (6): 445–450. March 2014. PMID 24695563.
- ↑ "Comparison of metabolic syndrome elements in White and Asian women with polycystic ovary syndrome: results of a regional, American cross-sectional study". F&S Reports 1 (3): 305–313. December 2020. doi:10.1016/j.xfre.2020.09.008. PMID 34223261.
- ↑ "Health care-related economic burden of the polycystic ovary syndrome during the reproductive life span". The Journal of Clinical Endocrinology and Metabolism 90 (8): 4650–4658. August 2005. doi:10.1210/jc.2005-0628. PMID 15944216.
- ↑ "RCDC Estimates of Funding for Various Research, Condition, and Disease Categories (RCDC)". https://report.nih.gov/categorical_spending.aspx#tab1.
- ↑ 175.0 175.1 "Anxiety, Depression, and Quality of Life in Women with Polycystic Ovarian Syndrome". Indian Journal of Psychological Medicine 40 (3): 239–246. 2018. doi:10.4103/IJPSYM.IJPSYM_561_17. PMID 29875531.
- ↑ "Sarah Hall investigates polycystic ovary syndrome" (in en). 2002-02-28. http://www.theguardian.com/lifeandstyle/2002/feb/28/healthandwellbeing.health.
- ↑ "'Teen Mom' Star Nails the 'Lose-Lose' Side of Chronic Illness Doctors Don't Always Get" (in en). https://themighty.com/2018/02/maci-bookout-teen-mom-og-pcos/.
- ↑ "All the celebrities who've opened up about life with Polycystic Ovary Syndrome" (in en). 26 November 2021. https://www.cosmopolitan.com/uk/body/health/g38290937/celebrities-pcos/.
- ↑ "What Every Woman Should Know About PCOS" (in en). https://www.refinery29.com/en-us/2015/07/91099/harnaam-kaur-women-with-facial-hair-true-story-pcos.
- ↑ "Actress Jaime King on her investment in Allara, a chronic care platform for women" (in en). https://fortune.com/2022/01/23/actress-jaime-king-investment-chronic-care-allara/.
- ↑ "Chrisette Michele Opens Up About Living With PCOS & No Longer Being Vegan - BlackDoctor.org - Where Wellness & Culture Connect" (in en-US). 2015-12-10. https://blackdoctor.org/chrisette-michele-pcos-vegan/.
- ↑ "Lea Michele On How PCOS Changed Her Relationship With Food: 'The Side Effects Can Be Brutal'" (in en). https://www.health.com/celebrities/lea-michele-interview.
- ↑ "Keke Palmer Says PCOS Causes Facial Hair and Adult Acne" (in en-US). 2021-11-17. https://www.prevention.com/health/health-conditions/a38280615/keke-palmer-pcos-symptoms/.
- ↑ "Sasha Pieterse Tears Up Over Health Problems, Opens Up About Losing 15 Pounds Since Joining 'DWTS'". September 26, 2017. http://www.etonline.com/sasha-pieterse-tears-over-health-problems-opens-about-losing-15-pounds-joining-dwts-88109.
- ↑ "Sasha Pieterse Wows on People's Ones to Watch Red Carpet as She Reveals Why She's 'So Thankful to DWTS'" (in en). October 5, 2017. https://people.com/tv/sasha-pieterse-medical-condition-response-amazing-dwts/.
- ↑ "'Star Wars: The Force Awakens' Actress Opens Up About Painful Disorder" (in en). https://abcnews.go.com/Entertainment/star-wars-force-awakens-actress-opens-painful-disorder/story?id=39745956.
- ↑ "Romee Strijd's Pregnancy Announcement Comes With an Honest Message About Reproductive Health" (in en). 29 May 2020. https://www.vogue.com/article/romee-strijd-pregnancy-announcement#:~:text=But%20along%20with%20the%20sweet,seven%20years%20without%20a%20period.
- ↑ "Lee's American Dream". The Cut (New York Media). March 10, 2020. https://www.thecut.com/2020/03/wellness-influencer-lee-from-americas-story.html.
Further reading
- "Polycystic ovary syndrome in the pediatric population". Metabolic Syndrome and Related Disorders 8 (5): 375–394. October 2010. doi:10.1089/met.2010.0039. PMID 20939704.
- "Polycystic Ovary Syndrome (PCOS)". Eunice Kennedy Shriver National Institute of Child Health and Human Development. 31 January 2017. https://www.nichd.nih.gov/health/topics/pcos.
External links
| Classification | |
|---|---|
| External resources |
 |



