Medicine:Chronic pain
| Chronic Pain | |
|---|---|
| Other names | Burning pain, dull pain, throbbing pain |
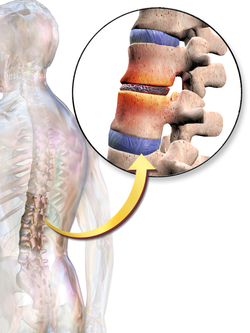
| Chronic pain can be caused by joint or bone damage during heavy and irregular sports. | |
| Heavy and irregular sports, in a long term, can be the basis of joint or bone injuries and as a result chronic pain.[1][2] | |
| Specialty | Specialist in pain, neurology and psychology[3] |
| Symptoms | Pain lasts longer than the expected period of recovery. |
| Usual onset | All age groups |
| Duration | From three months to several years |
| Causes | high blood sugar, cancer, genetic disorder in neural differentiation, tissue damage, neurological disorder and viral diseases[4] |
| Risk factors | diabetes, cancer and heart diseases[citation needed] |
| Diagnostic method | Based on medical history, clinical examination, questionnaire and neuroimaging[4] |
| Differential diagnosis | gastric ulcer, bone fracture, hernia and neoplasia of the spinal cord[5] |
| Medication | Non-opioid: ibuprofen, acetaminophen, naproxen, NSAIDs and olanzapine[citation needed] Opioid: morphine, codeine, endorphins and buprenorphine[6] |
| Frequency | 8% to 55.2% in different countries[citation needed] |
Chronic pain or chronic pain syndrome is a type of pain that is also known by other titles such as gradual burning pain, electrical pain, throbbing pain, and nauseating pain. This type of pain is sometimes confused with acute pain[lower-alpha 1] and can last from three months to several years; Various diagnostic manuals such as DSM-5 and ICD-11 have proposed several definitions of chronic pain, but the accepted definition is that it is "pain that lasts longer than the expected period of recovery."
Creating a pain mechanism prevents possible damage to the body, but chronic pain is a pain without biological value (doesn't have a positive effect). This pain has different divisions; Cancer, post-traumatic or surgery, musculoskeletal and visceral are the most important of these divisions. Various factors cause the formation of chronic pain, which can be neurogenic (gene-dependent), nociceptive, neuropathic, psychological or unknown. Some diseases such as diabetes (high blood sugar), shingles (some viral diseases), phantom limb pain, hypertension and stroke also play a role in the formation of chronic pain. The most common types of chronic pain are back pain, severe headache, migraine, and facial pain.
Chronic pain can cause very severe psychological and physical effects that sometimes continue until the end of life. Analysis of the grey matter (damage to brain neurons), insomnia and sleep deprivation, metabolic problems, chronic stress, obesity and heart attack are examples of physical disorder; And depression, cognitive disorders, perceived injustice (PI) and neurosis are examples of mental disorder.
A wide range of treatments are performed for this disease; Drug therapy (types of opioid and non-opioid drugs), cognitive behavioral therapy and physical therapy are the most significant of them. Medicines are usually associated with side effects and are prescribed when the effects of pain become severe. Medicines such as aspirin and ibuprofen are used for milder pain and morphine and codeine for severe pain. Other treatment methods, such as behavioral therapy and physiotherapy, are often used as a supplement along with drugs due to their low effectiveness. There is currently no definitive cure for any of these methods, and research continues into a wide variety of new management and therapeutic interventions, such as nerve block and radiation therapy.
Chronic pain is considered a kind of disease, this type of pain has affected the people of the world more than diabetes, cancer and heart diseases. During several epidemiological studies conducted in different countries, wide differences in the prevalence rate of chronic pain have been reported from 8% to 55.2% in countries; For example, studies evaluate the incidence in Iran and Canada between 10% and 20% and in the United States between 30% and 40%. The results show that an average of 8% to 11.2% of people in different countries have severe chronic pain, and its epidemic is higher in industrialized countries than in other countries. According to the estimates of the American Medical Association, the costs related to this disease in this country are about 560 to 635 billion dollars.
Classification
The International Association for the Study of Pain (IASP) defines chronic pain as a general pain without biological value that sometimes continues even after the healing of the affected area;[8][9] A type of pain that cannot be classified as acute pain[lower-alpha 2] and lasts longer than expected to heal, or typically, pain that has been experienced on most days or daily for the past six months, is considered chronic pain.[11][12] According to the DSM-5 index, a complication is "chronic" when the resulting complication (pain, disorder, and illness) lasts for a period of more than six months (this type of classification does not have any prerequisites such as physical or mental injury).[13] The classification of chronic pain is not only limited to pains that arise in the presence of real tissue damage (secondary pains resulting from a primary event); The title "nociplastic pain" or primary pain is related to the pains that occur in the absence of a health-threatening factor, such as disease or damage to the body's somatosensory system, and as a result of permanent nerve stimulation.[14][15]
The International Statistical Classification of Diseases, in its 11th edition (ICD-11), proposed a seven-category classification for chronic pain:[16]
- Primary chronic pain: Defined by 3 months of continuous pain in one or more areas of the body, the origin of which is not understood.
- Chronic cancer pain: pain in one of the body's organs caused by cancer damage (in internal organs, bone or skeletal muscular) is formed.
- Chronic pain post-traumatic or surgery: Pain that occurs 3 months after an injury or surgery, without taking into account infectious conditions and the severity of tissue damage; Also, the person's past pain is not important in this classification.
- Chronic neuropathic pain: pain caused by damage to the somatosensory nervous system.
- Chronic headache and orofacial pain: pain that originates in the head or face, and occurs for 50% or more days over a 3 months period.
- Chronic visceral pain: pain originating in an internal organ.
- Chronic musculoskeletal pain: pain originating in the bones, muscles, joints or connective tissue.
Also, the World Health Organization (WHO) states that optional criteria or codes can be used in the classification of chronic pain for each of the seven categories of chronic pain (for example, "diabetic neuropathic" pain).[15]
Another classification for chronic pain is "nociceptive" (caused by inflamed or damaged tissue that activates special pain sensors called nociceptors) and "neuropathic" (caused by damage or malfunction of the nervous system).[16] The type of "nociceptive" itself is divided into two parts: "superficial" and "deep"; also, deep pains are divided into two parts: "deep physical" and "deep visceral" pain.[17] "neuropathic" pains are also divided into "peripheral" (source The peripheral nervous system) and "central" (Central nervous system from the brain or spinal cord) are divided.[18][19] Peripheral neuropathic pain is often described as "burning", "tingling", "electrical", "stabbing", or "pins and needles".[20]
"Superficial pain" is the result of the activation of pain receptors in the skin or superficial tissues; "Deep somatic pain" is caused by stimulation of pain receptors in ligaments, tendons, bones, blood vessels, fascia, and muscles. (this type of pain is constant but weak)[21] and "deep visceral pain" is pain that originates from one of the body's organs. Deep pain is often very difficult to localize and occurs in multiple areas of the body when injured or inflamed. In the "deep visceral" type, the feeling of pain exists in a place far from the injury, for this reason it is also called vague pain.[21]
Etiology
Chronic pain has many pathophysiological and environmental causes and can occur in cases such as neuropathy of the central nervous system, after cerebral hemorrhage, tissue damage such as extensive burns, inflammation, autoimmune disorders such as rheumatoid arthritis, psychological stress such as headache, migraine or abdominal pain (caused by emotional, psychological or behavioral) and mechanical pain caused by tissue wear and tear such as arthritis.[4] In some cases, chronic pain can be caused by genetic factors which interfere with neuronal differentiation, leading to a permanently lowered threshold for pain.[22]
The pathophysiology of chronic pain remains unclear. Many theories of chronic pain[23][24] fail to clearly explain why the same pathological conditions do not invariably result in chronic pain. A recent hypothesis-based analysis of literature suggests that patients' anatomical predisposition to proximal neural compression (especially at the level of spinal plexuses and dorsal root ganglia) may be the answer to this conundrum.[25] This hypothesis states that any type of chronic pain is driven by a proximal compressive neuropathy, which can be primary or can develop in the course of background diseases. Difficulties in diagnosing proximal neural lesion may account for the theoretical perplexity of chronic pain.
Pathophysiology
The mechanism of continuous activation and transmission of pain messages, leads the body to an activity to relieve pain (a mechanism to prevent damage in the body), this action causes the release of prostaglandin and increase the sensitivity of that part to stimulation; Prostaglandin secretion causes unbearable and chronic pain.[26] Under persistent activation, the transmission of pain signals to the dorsal horn may produce a pain wind-up phenomenon. This triggers changes that lower the threshold for pain signals to be transmitted. In addition, it may cause non-nociceptive nerve fibers to respond to, generate, and transmit pain signals.[27][28] Researchers believe that the nerve fibers that cause this type of pain are group C nerve fibers; These fibers are not myelinated (have low transmission speed) and cause long-term pain.[29][30]
These changes in neural structure can be explained by neuroplasticity.[30] When there is chronic pain, the somatotopic arrangement of the body (the distribution view of nerve cells) is abnormally changed due to continuous stimulation and can cause allodynia or hyperalgesia.[lower-alpha 3] In chronic pain, this process is difficult to reverse or stop once established.[32] EEG of people with chronic pain showed that brain activity and synaptic plasticity change as a result of pain, and specifically, the relative activity of beta wave increases and alpha and theta waves decrease.[33]
Inefficient management of dopamine secretion in the brain can act as a common mechanism between chronic pain, insomnia and major depressive disorder and cause its unpleasant side effects.[34] Astrocytes, microglia and satellite glial cells also lose their effective function in chronic pain. Increasing the activity of microglia, changing microglia networks, and increasing the production of chemokines and cytokines by microglia may exacerbate chronic pain.[26][35] It has also been observed that astrocytes lose their ability to regulate the excitability of neurons and increase the spontaneous activity of neurons in pain circuits.[35]
Management
Pain management is a branch of medicine that uses an interdisciplinary approach. The combined knowledge of various medical professions and allied health professions is used to ease pain and improve the quality of life of those living with pain.[36] The typical pain management team includes medical practitioners (particularly anesthesiologists), rehabilitation psychologists, physiotherapists, occupational therapists, physician assistants, and nurse practitioners.[37] Acute pain usually resolves with the efforts of one practitioner; however, the management of chronic pain frequently requires the coordinated efforts of a treatment team.[38][39][40] Complete, longterm remission of many types of chronic pain is rare.[41]
Chronic pain may originate in the body, or in the brain or spinal cord. It is often difficult to treat. Epidemiological studies have found that 8–11.2% of people in various countries have chronic widespread pain.[42] Various non-opioid medicines are initially recommended to treat chronic pain, depending on whether the pain is due to tissue damage or is neuropathic.[43][44] Psychological treatments including cognitive behavioral therapy and acceptance and commitment therapy may be effective for improving quality of life in those with chronic pain. Some people with chronic pain may benefit from opioid treatment while others can be harmed by it.[45][46] People with non-cancer pain who have not been helped by non-opioid medicines might be recommended to try opioids if there is no history of substance use disorder and no current mental illness.[47]
Nonopioids
Initially recommended efforts are non-opioid based therapies.[47] Non-opioid treatment of chronic pain with pharmaceutical medicines might include acetaminophen (paracetamol)[48] or NSAIDs.[49]
Various other nonopioid medicines can be used, depending on whether the pain is a result of tissue damage or is neuropathic (pain caused by a damaged or dysfunctional nervous system). There is limited evidence that cancer pain or chronic pain from tissue damage as a result of a conditions (e.g. rheumatoid arthritis) is best treated with opioids. For neuropathic pain other drugs may be more effective than opioids,[43][44][50][51] such as tricyclic antidepressants,[52] serotonin-norepinephrine reuptake inhibitors,[53] and anticonvulsants.[53] Some atypical antipsychotics, such as olanzapine, may also be effective, but the evidence to support this is in very early stages.[54] In women with chronic pain, hormonal medications such as oral contraceptive pills ("the pill") might be helpful.[55] When there is no evidence of a single best fit, doctors may need to look for a treatment that works for the individual person.[52] It is difficult for doctors to predict who will use opioids just for pain management and who will go on to develop an addiction. It is also challenging for doctors to know which patients ask for opioids because they are living with an opioid addiction. Withholding, interrupting or withdrawing opioid treatment in people who benefit from it can cause harm.[45]
Interventional pain management may be appropriate, including techniques such as trigger point injections, neurolytic blocks, and radiotherapy. While there is no high quality evidence to support ultrasound, it has been found to have a small effect on improving function in non-specific chronic low back pain.[56]
Psychological treatments, including cognitive behavioral therapy[57][58] and acceptance and commitment therapy[59][60] can be helpful for improving quality of life and reducing pain interference. Brief mindfulness-based treatment approaches have been used, but they are not yet recommended as a first-line treatment.[61] The effectiveness of mindfulness-based pain management (MBPM) has been supported by a range of studies.[6][62][63]
Among older adults psychological interventions can help reduce pain and improve self-efficacy for pain management.[64] Psychological treatments have also been shown to be effective in children and teens with chronic headache or mixed chronic pain conditions.[65]
While exercise has been offered as a method to lessen chronic pain and there is some evidence of benefit, this evidence is tentative.[66] For people living with chronic pain, exercise results in few side effects.[66]
Opioids
In those who have not benefited from other measures and have no history of either mental illness or substance use disorder treatment with opioids may be tried.[47] If significant benefit does not occur it is recommended that they be stopped.[47] In those on opioids, stopping or decreasing their use may improve outcomes including pain.[67]
Some people with chronic pain benefit from opioid treatment and others do not; some are harmed by the treatment.[45] Possible harms include reduced sex hormone production, hypogonadism, infertility, impaired immune system, falls and fractures in older adults, neonatal abstinence syndrome, heart problems, sleep-disordered breathing, opioid-induced hyperalgesia, physical dependence, addiction, abuse, and overdose.[68][69]
Alternative medicine
Alternative medicine refers to health practices or products that are used to treat pain or illness that are not necessarily considered a part of conventional medicine.[70] When dealing with chronic pain, these practices generally fall into the following four categories: biological, mind-body, manipulative body, and energy medicine.[70]
Implementing dietary changes, which is considered a biological-based alternative medicine practice, has been shown to help improve symptoms of chronic pain over time.[70] Adding supplements to one's diet is a common dietary change when trying to relieve chronic pain, with some of the most studied supplements being: acetyl-L-carnitine, alpha-lipoic acid, and vitamin E.[70][71][72][73] Vitamin E is perhaps the most studied out of the three, with strong evidence that it helps lower neurotoxicity in those with cancer, multiple sclerosis, and cardiovascular diseases.[73]
Hypnosis, including self-hypnosis, has tentative evidence.[74] Hypnosis, specifically, can offer pain relief for most people and may be a safe alternative to pharmaceutical medication.[75] Evidence does not support hypnosis for chronic pain due to a spinal cord injury.[76]
Preliminary studies have found medical marijuana to be beneficial in treating neuropathic pain, but not other kinds of long term pain.[77] (As of 2018), the evidence for its efficacy in treating neuropathic pain or pain associated with rheumatic diseases is not strong for any benefit and further research is needed.[78][79][80] For chronic non-cancer pain, a recent study concluded that it is unlikely that cannabinoids are highly effective.[81] However, more rigorous research into cannabis or cannabis-based medicines is needed.[80]
Tai chi has been shown to improve pain, stiffness, and quality of life in chronic conditions such as osteoarthritis, low back pain, and osteoporosis.[82][83] Acupuncture has also been found to be an effective and safe treatment in reducing pain and improving quality of life in chronic pain including chronic pelvic pain syndrome.[84][85]
Transcranial magnetic stimulation for reduction of chronic pain is not supported by high quality evidence, and the demonstrated effects are small and short-term.[86]
Spa therapy could potentially improve pain in patients with chronic lower back pain, but more studies are needed to provide stronger evidence of this.[87]
While some studies have investigated the efficacy of St John's Wort or nutmeg for treating neuropathic (nerve) pain, their findings have raised serious concerns about the accuracy of their results.[88]
Kinesio tape has not been shown to be effective in managing chronic non-specific low-back pain.[89]
Myofascial release has been used in some cases of fibromyalgia, chronic low back pain, and tennis elbow but there is not enough evidence to support this as method of treatment.[90]
Epidemiology
Chronic pain varies in different countries affecting anywhere from 8% to 55% of the population. It affects women at a higher rate than men, and chronic pain uses a large amount of healthcare resources around the globe.[91][42]
A large-scale telephone survey of 15 European countries and Israel found that 19% of respondents over 18 years of age had suffered pain for more than 6 months, including the last month, and more than twice in the last week, with pain intensity of 5 or more for the last episode, on a scale of 1 (no pain) to 10 (worst imaginable). 4839 of these respondents with chronic pain were interviewed in-depth. Sixty-six percent scored their pain intensity at moderate (5–7), and 34% at severe (8–10); 46% had constant pain, 56% intermittent; 49% had suffered pain for 2–15 years; and 21% had been diagnosed with depression due to the pain. Sixty-one percent were unable or less able to work outside the home, 19% had lost a job, and 13% had changed jobs due to their pain. Forty percent had inadequate pain management and less than 2% were seeing a pain management specialist.[92]
In the United States, chronic pain has been estimated to occur in approximately 35% of the population, with approximately 50 million Americans experiencing partial or total disability as a consequence.[93] According to the Institute of Medicine, there are about 116 million Americans living with chronic pain, which suggests that approximately half of American adults have some chronic pain condition.[94][95] The Mayday Fund estimate of 70 million Americans with chronic pain is slightly more conservative.[96] In an internet study, the prevalence of chronic pain in the United States was calculated to be 30.7% of the population: 34.3% for women and 26.7% for men.[97]
In Canada it is estimated that approximately 1 in 5 Canadians live with chronic pain and half of those people have lived with chronic pain for 10 years or longer.[98] Chronic pain in Canada also occurs more and is more severe in women and Canada's Indigenous communities.[98]
Outcomes
Sleep disturbance, and insomnia due to medication and illness symptoms are often experienced by those with chronic pain.[99] These conditions can be difficult to treat due to the high potential of medication interactions, especially when the conditions are treated by different doctors.[100]
Severe chronic pain is associated with increased risk of death over a ten-year period, particularly from heart disease and respiratory disease.[101] Several mechanisms have been proposed for this increase, such as an abnormal stress response in the body's endocrine system.[102] Additionally, chronic stress seems to affect risks to heart and lung (cardiovascular) health by increasing how quickly plaque can build up on artery walls (arteriosclerosis). However, further research is needed to clarify the relationship between severe chronic pain, stress and cardiovascular health.[101]
People with chronic pain tend to have higher rates of depression[103] and although the exact connection between the comorbidities is unclear, a 2017 study on neuroplasticity found that "injury sensory pathways of body pains have been shown to share the same brain regions involved in mood management."[104] Chronic pain can contribute to decreased physical activity due to fear of making the pain worse. Pain intensity, pain control, and resilience to pain can be influenced by different levels and types of social support that a person with chronic pain receives, and are also influenced by the person's socioeconomic status.[105]
Chronic pain of different causes has been characterized as a disease that affects brain structure and function. MRI studies have shown abnormal anatomical[106] and functional connectivity, even during rest[107][108] involving areas related to the processing of pain. Also, persistent pain has been shown to cause grey matter loss, which is reversible once the pain has resolved.[109][110]
One approach to predicting a person's experience of chronic pain is the biopsychosocial model, according to which an individual's experience of chronic pain may be affected by a complex mixture of their biology, psychology, and their social environment.[111]
Psychology
Personality
Two of the most frequent personality profiles found in people with chronic pain by the Minnesota Multiphasic Personality Inventory (MMPI) are the conversion V and the neurotic triad. The conversion V personality expresses exaggerated concern over body feelings, develops bodily symptoms in response to stress, and often fails to recognize their own emotional state, including depression. The neurotic triad personality also expresses exaggerated concern over body feelings and develops bodily symptoms in response to stress, but is demanding and complaining.[112]
Some investigators have argued that it is this neuroticism that causes acute pain to turn chronic, but clinical evidence points the other way, to chronic pain causing neuroticism. When long term pain is relieved by therapeutic intervention, scores on the neurotic triad and anxiety fall, often to normal levels.[113][114][115][116] Self-esteem, often low in people with chronic pain, also shows improvement once pain has resolved.[116]
It has been suggested that catastrophizing might play a role in the experience of pain. Pain catastrophizing is the tendency to describe a pain experience in more exaggerated terms than the average person, to think a great deal more about the pain when it occurs, or to feel more helpless about the experience.[117] People who score highly on measures of catastrophization are likely to rate a pain experience as more intense than those who score low on such measures. It is often reasoned that the tendency to catastrophize causes the person to experience the pain as more intense. One suggestion is that catastrophizing influences pain perception through altering attention and anticipation, and heightening emotional responses to pain.[118] However, at least some aspects of catastrophization may be the product of an intense pain experience, rather than its cause. That is, the more intense the pain feels to the person, the more likely they are to have thoughts about it that fit the definition of catastrophization.[119]
Comorbidity with trauma
Individuals with post-traumatic stress disorder (PTSD) have a high comorbidity with chronic pain.[120] Patients with both PTSD and chronic pain report higher severity of pain than those who do not have a PTSD comorbidity.[121][122]
Comorbidity with depression
People with chronic pain may also have symptoms of depression.[123][124] In 2017, the British Medical Association found that 49% of people with chronic pain had depression.[125]
Effect on cognition
Chronic pain's impact on cognition is an under-researched area, but several tentative conclusions have been published. Most people with chronic pain complain of cognitive impairment, such as forgetfulness, difficulty with attention, and difficulty completing tasks. Objective testing has found that people in chronic pain tend to experience impairment in attention, memory, mental flexibility, verbal ability, speed of response in a cognitive task, and speed in executing structured tasks.[126] A review of studies in 2018 reports a relationship between people in chronic pain and abnormal results in test of memory, attention, and processing speed.[127]
Prognosis
Chronic pain leads to a significant decrease in quality of life, decreased productivity, decreased wages, worsening of other chronic diseases, and mental disorders such as depression, anxiety, and substance use disorder.[4] Many drugs that are often used to treat chronic pain have risks and potential side effects and possible complications associated with their use, and the constant use of opioids is associated with decreased life expectancy and increased mortality of patients.[128][129] Acetaminophen, a standard drug treatment for chronic pain, can cause hepatotoxicity when taken in excess of four grams per day.[130][131] In addition, therapeutic doses for patients with chronic liver diseases may also cause hepatotoxicity.[132] Long-term risks and side effects of opioids include constipation, drug tolerance or dependence, nausea, indigestion, arrhythmia (QT prolongation of electrocardiography in methadone treatment), and endocrine gland that can lead to amenorrhea, impotence, gynecomastia, and decreased become energy. Also there is a risk of opioid overdose depending on the dose taken by the patient.[4][133]
Current treatments for chronic pain can reduce pain by 30%.[134] This reduction in pain can significantly improve patients' performance and quality of life. However, the general and long-term prognosis of chronic pain shows decreased function and quality of life.[135] Also, this disease causes many complications and increases the possibility of death of patients and suffering from other chronic diseases and obesity.[4] Similarly, patients with chronic pain who require opioids often develop drug tolerance over time, and this increase in the amount of the dose taken to be effective increases the risk of side effects and death.[4]
Mental disorders can amplify pain signals and make symptoms more severe.[136] In addition, comorbid psychiatric disorders, such as major depressive disorder, can significantly delay the diagnosis of pain disorders.[137] Major depressive disorder and generalized anxiety disorder are the most common comorbidities associated with chronic pain. Patients with underlying pain and comorbid mental disorders receive twice as much medication from doctors annually as compared to patients who do not have such co-morbidities.[138] Studies have shown that when coexisting diseases exist along with chronic pain, the treatment and improvement of one of these disorders can be effective in the improvement of the other.[139][140] Patients with chronic pain are at higher risk for suicide and suicidal thoughts. Research has shown approximately 20% of people with suicidal thoughts and between 5 and 14% of patients with chronic pain who commit suicide.[139] Of patients who attempted suicide, 53.6% died of gunshot wounds and 16.2% died of opioid overdose.[140]
A multimodal treatment approach is important for better pain control and outcomes, as well as minimizing the need for high-risk treatments such as opioid medications. Managing comorbid depression and anxiety is critical in reducing chronic pain.[4][139] Also, patients with chronic pain should be carefully monitored for severe depression and any suicidal thoughts and plans.[4][140] Periodic referral of the patient to the doctor for physical examination and to check the effectiveness of treatment 2 is necessary, and the rapid and correct treatment and management of chronic pain can prevent the occurrence of potential negative consequences on the patient's life and increase in healthcare costs.[4]
Social and personal impacts
Social support
Social support has important consequences for individuals with chronic pain. In particular, pain intensity, pain control, and resiliency to pain have been implicated as outcomes influenced by different levels and types of social support. Much of this research has focused on emotional, instrumental, tangible and informational social support. People with persistent pain conditions tend to rely on their social support as a coping mechanism and therefore have better outcomes when they are a part of larger more supportive social networks. Across a majority of studies investigated, there was a direct significant association between social activities or social support and pain. Higher levels of pain were associated with a decrease in social activities, lower levels of social support, and reduced social functioning.[141][142]
Racial disparities
Evidence exists for unconscious biases and negative stereotyping against racial minorities requesting pain treatment, although clinical decision making was not affected, according to one 2017 review.[143] Minorities may be denied diagnoses for pain and pain medications, and are more likely to go through substance abuse assessment, and are less likely to transfer for pain specialist referral.[144] A 2010 University of Michigan Health study found that black patients in pain clinics received 50% of the amount of drugs that patients who were white received.[145] Preliminary research showed that health providers might have less empathy for black patients and underestimated their pain levels, resulting in treatment delays.[143][144] Minorities may experience a language barrier, limiting the high level of engagement between the person with pain and health providers for treatment.[144]
Perceptions of injustice
Similar to the damaging effects seen with catastrophizing, perceived injustice is thought to contribute to the severity and duration of chronic pain.[146] Pain-related injustice perception has been conceptualized as a cognitive appraisal reflecting the severity and irreparability of pain- or injury-related loss (e.g., "I just want my life back"), and externalizing blame and unfairness ("I am suffering because of someone else's negligence.").[147] It has been suggested that understanding problems with top down processing/cognitive appraisals can be used to better understand and treat this problem.[148]
Chronic pain and COVID-19
COVID-19 has disrupted the lives of many, leading to major physical, psychological and socioeconomic impacts in the general population.[149] Social distancing practices defining the response to the pandemic alter familiar patterns of social interaction, creating the conditions for what some psychologists are describing as a period of collective grief.[150] Individuals with chronic pain tend to embody an ambiguous status, at times expressing that their type of suffering places them between and outside of conventional medicine.[151] With a large proportion of the global population enduring prolonged periods of social isolation and distress, one study found that people with chronic pain from COVID-19 experienced more empathy towards their suffering during the pandemic.[149]
Effect of chronic pain in the workplace
In the workplace, chronic pain conditions are a significant problem for both the person with the condition and the organization; a problem only expected to increase in many countries due to an aging workforce.[111] In light of this, it may be helpful for organizations to consider the social environment of their workplace, and how it may be working to ease or worsen chronic pain issues for employees.[111] As an example of how the social environment can affect chronic pain, some research has found that high levels of socially prescribed perfectionism (perfectionism induced by external pressure from others, such as a supervisor) can interact with the guilt felt by a person with chronic pain, thereby increasing job tension, and decreasing job satisfaction.[111]
See also
- Childhood chronic pain
- Dopaminergic pathways
- List of investigational analgesics
- Neurodegeneration
- Neuroinflammation
Notes
- ↑ Doctors define acute pain as pain associated with a cause that can be relieved by treating the cause. In the general sense, acute pain means pain that decreases or stops when the disease improves.[7]
- ↑ Doctors define acute pain as pain associated with a cause that can be relieved by treating the cause. In the general sense, acute pain means pain that decreases or stops when the disease improves.[10]
- ↑ The continuous sending of messages from one body part causes its somatotopic area to become larger than the normal state, and the brain of the area attaches more and abnormal energy and importance to the tissue stimuli of that part of the body.[31]
References
- ↑ Buckwalter, Joseph A. (October 2003). "Sports, joint injury, and posttraumatic osteoarthritis". The Journal of Orthopaedic and Sports Physical Therapy 33 (10): 578–588. doi:10.2519/jospt.2003.33.10.578. ISSN 0190-6011. PMID 14620787. https://pubmed.ncbi.nlm.nih.gov/14620787/.
- ↑ Saxon, L.; Finch, C.; Bass, S. (August 1999). "Sports participation, sports injuries and osteoarthritis: implications for prevention". Sports Medicine (Auckland, N.Z.) 28 (2): 123–135. doi:10.2165/00007256-199928020-00005. ISSN 0112-1642. PMID 10492030. https://pubmed.ncbi.nlm.nih.gov/10492030/.
- ↑ "Pain terms and taxonomies". Bonica's Management of Pain (3rd ed.). Lippincott Williams & Wilkins. 2001. pp. 18–25. ISBN 978-0683304626. https://books.google.com/books?id=TyNEicOiJqQC&q=Pain+terms+and+taxonomies&pg=RA1-PA18.
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 4.6 4.7 4.8 4.9 Dydyk, Alexander M; Till, Conermann (June 2023). Abrazo Central Campus. ed. "Chronic Pain". StatPearls [Internet] (StatPearls Publishing). https://www.ncbi.nlm.nih.gov/books/NBK553030/.
- ↑ "Chronic Pain Syndrome Differential Diagnoses". 2020-01-14. https://emedicine.medscape.com/article/310834-differential.
- ↑ 6.0 6.1 "A literature review of Breathworks and mindfulness intervention". British Journal of Healthcare Management 24 (5): 235–241. 2018. doi:10.12968/bjhc.2018.24.5.235. ISSN 1358-0574.
- ↑ "Acute Pain Causes, Symptoms, and Treatments | UPMC" (in en). https://www.upmc.com/services/pain-management/conditions/acute-pain.
- ↑ "Pain terms and taxonomies". Bonica's Management of Pain (3rd ed.). Lippincott Williams & Wilkins. 2001. pp. 18–25. ISBN 978-0-683-30462-6. https://books.google.com/books?id=TyNEicOiJqQC&q=Pain+terms+and+taxonomies&pg=RA1-PA18.
- ↑ "Classification of pain". Pain management: A practical guide for clinicians (6 ed.). American Academy of Pain Management. 2002. ISBN 978-0-8493-0926-7. https://books.google.com/books?id=lg7sIgP9D3kC&q=chronic+acute+subacute+pain+idiopathic&pg=PA28.
- ↑ "Acute Pain Causes, Symptoms, and Treatments | UPMC" (in en). https://www.upmc.com/services/pain-management/conditions/acute-pain.
- ↑ Henning, Troy; Chang, Wilson; Stanos, Steven (September 2022). El Miedany, Yasser. ed. "Classification of Chronic Pain" (in en). Springer Link. Contemporary Rheumatology: 3-10. ISSN 2662-7531. https://link.springer.com/chapter/10.1007/978-3-031-10687-3_1.
- ↑ Pain management: an interdisciplinary approach. Elsevier. 2001. p. 93. ISBN 978-0-443-05683-3. https://books.google.com/books?id=r9FWvgAACAAJ&dq=Pain+Management:+An+Interdisciplinary+Approach&hl=en&sa=X&ved=2ahUKEwiAsuW1yPjyAhWPkhQKHRPuDeUQ6AF6BAgDEAI.
- ↑ Katz, Joel; Rosenbloom, Brittany N.; Fashler, Samantha (April 2015). "Chronic Pain, Psychopathology, and DSM-5 Somatic Symptom Disorder". Canadian Journal of Psychiatry. Revue Canadienne De Psychiatrie 60 (4): 160–167. doi:10.1177/070674371506000402. ISSN 0706-7437. PMID 26174215. PMC 4459242. https://pubmed.ncbi.nlm.nih.gov/26174215/.
- ↑ "Terminology | International Association for the Study of Pain" (in en-US). https://www.iasp-pain.org/resources/terminology/.
- ↑ 15.0 15.1 Treede, Rolf-Detlef; Rief, Winfried; Barke, Antonia; Aziz, Qasim; Bennett, Michael I.; Benoliel, Rafael; Cohen, Milton; Evers, Stefan et al. (January 2019). "Chronic pain as a symptom or a disease: the IASP Classification of Chronic Pain for the International Classification of Diseases (ICD-11)". Pain 160 (1): 19–27. doi:10.1097/j.pain.0000000000001384. ISSN 1872-6623. PMID 30586067. https://pubmed.ncbi.nlm.nih.gov/30586067/?dopt=Abstract.
- ↑ 16.0 16.1 Treede, Rolf-Detlef; Rief, Winfried; Barke, Antonia; Aziz, Qasim; Bennett, Michael I.; Benoliel, Rafael; Cohen, Milton; Evers, Stefan et al. (June 2015). "A classification of chronic pain for ICD-11". Pain 156 (6): 1003–1007. doi:10.1097/j.pain.0000000000000160. ISSN 1872-6623. PMID 25844555. PMC 4450869. https://pubmed.ncbi.nlm.nih.gov/25844555/.
- ↑ "General considerations of acute pain". Bonica's management of pain (3 ed.). Philadelphia: Lippincott Williams & Wilkins. 2001. ISBN 978-0-443-05683-3. https://archive.org/details/painmanagementin0000main.
- ↑ Classification of chronic pain: descriptions of chronic pain syndromes and definitions of pain terms (second ed.). Seattle: IASP Press. 1994. p. 212. ISBN 978-0931092053. https://archive.org/details/classificationof0000unse_o5f1/page/212.
- ↑ Diagnostic Methods for Neuropathic Pain: A Review of Diagnostic Accuracy Rapid Response Report: Summary with Critical Appraisal.. Canadian Agency for Drugs and Technologies in Health. April 2015.
- ↑ "Mechanisms and management of neuropathic pain in cancer". The Journal of Supportive Oncology 1 (2): 107–120. Jul–Aug 2003. PMID 15352654. http://www.supportiveoncology.net/journal/articles/0102107.pdf. Retrieved 2010-05-03.
- ↑ 21.0 21.1 "General considerations of acute pain". Bonica's management of pain (3 ed.). Philadelphia: Lippincott Williams & Wilkins. 2001. ISBN 978-0443056833. https://archive.org/details/painmanagementin0000main.
- ↑ "Notch3 is necessary for neuronal differentiation and maturation in the adult spinal cord". Journal of Cellular and Molecular Medicine 18 (10): 2103–16. October 2014. doi:10.1111/jcmm.12362. PMID 25164209.
- ↑ "Towards a theory of chronic pain". Progress in Neurobiology 87 (2): 81–97. February 2009. doi:10.1016/j.pneurobio.2008.09.018. PMID 18952143.
- ↑ "Why does pain persist in so many cases?". Sciatica and Chronic Pain. Springer International Publishing. 2019. pp. 71–88. doi:10.1007/978-3-319-93904-9_7. ISBN 978-3-319-93903-2.
- ↑ "Chronic pain and local pain in usually painless conditions including neuroma may be due to compressive proximal neural lesion". Frontiers in Pain Research 4: 1037376. February 2023. doi:10.3389/fpain.2023.1037376.
- ↑ 26.0 26.1 Neuroscience, Association; Panahi, Reza; Soor, Behnam; Shahbazi, Ali; Haqparest, Abbas (2018). Brain facts. Tehran.Iran: Satish Hasti Publishing House. p. 113. ISBN 978-622-6445-63-4.
- ↑ Nociceptive and neurogenic pain. Pharmacia & Upjon AB. 1998. pp. 52–63.
- ↑ Jena, Monalisa; Mishra, Swati Mishra; Pradhan, Sarita; Jena, Swetalina; Mishra, Sudhansu Sekhar (2015-09-01). "Chronic pain, its management and psychological issues: A review" (in en). Asian Journal of Pharmaceutical and Clinical Research: 42–47. ISSN 2455-3891. https://innovareacademics.in/journals/index.php/ajpcr/article/view/7403.
- ↑ Jena, Monalisa; Mishra, Swati Mishra; Pradhan, Sarita; Jena, Swetalina; Mishra, Sudhansu Sekhar (2015-09-01). "Chronic pain, its management and psychological issues: A review" (in en). Asian Journal of Pharmaceutical and Clinical Research: 42–47. ISSN 2455-3891. https://innovareacademics.in/journals/index.php/ajpcr/article/view/7403.
- ↑ 30.0 30.1 Dickenson, Anthony H.; Matthews, Elizabeth A.; Suzuki, Rie (2002). "Neurobiology of neuropathic pain: mode of action of anticonvulsants" (in en). European Journal of Pain 6 (SA): 51–60. doi:10.1053/eujp.2001.0323. ISSN 1532-2149. https://onlinelibrary.wiley.com/doi/abs/10.1053/eujp.2001.0323.
- ↑ "Neuromodulatory approaches for chronic pain management: research findings and clinical implications". Journal of Neurotherapy 13 (4): 196–213. 2009. doi:10.1080/10874200903334371.
- ↑ "Recent advances in elucidating pain mechanisms". Current Opinion in Anesthesiology 18 (5): 540–7. October 2005. doi:10.1097/01.aco.0000183109.27297.75. PMID 16534290.
- ↑ "Neuromodulatory approaches for chronic pain management: research findings and clinical implications". Journal of Neurotherapy 13 (4): 196–213. 2009. doi:10.1080/10874200903334371.
- ↑ Finan, Patrick H.; Smith, Michael T. (June 2013). "The comorbidity of insomnia, chronic pain, and depression: dopamine as a putative mechanism". Sleep Medicine Reviews 17 (3): 173–183. doi:10.1016/j.smrv.2012.03.003. ISSN 1532-2955. PMID 22748562. PMC 3519938. https://pubmed.ncbi.nlm.nih.gov/22748562/.
- ↑ 35.0 35.1 Ji, Ru-Rong; Berta, Temugin; Nedergaard, Maiken (December 2013). "Glia and pain: is chronic pain a gliopathy?". Pain 154 Suppl 1: S10–S28. doi:10.1016/j.pain.2013.06.022. ISSN 1872-6623. PMID 23792284. PMC 3858488. https://pubmed.ncbi.nlm.nih.gov/23792284/.
- ↑ Chronic pain management: the essentials. UK: Greenwich Medical Media. 1997. p. 10. ISBN 978-1900151856. https://archive.org/details/chronicpainmanag0000hard. "the reduction of suffering and enhanced quality of life ."
- ↑ Pain management: an interdisciplinary approach. Churchill Livingstone. 2000. ISBN 978-0443056833. https://archive.org/details/painmanagementin0000main.
- ↑ "The classification of pain". Pain management: A practical guide for clinicians. CRC Press. 2002. p. 29. ISBN 978-0849309267. https://books.google.com/books?id=L2CSdeiMZi4C&q=%22chronic%20pain%20frequently%20requires%20the%20coordinated%20efforts%20of%20a%20broadly%20based%20treatment%20team%22&pg=PA27.
- ↑ "Management of functional somatic syndromes". Lancet 369 (9565): 946–55. March 2007. doi:10.1016/S0140-6736(07)60159-7. PMID 17368156.
- ↑ "Multidisciplinary and interdisciplinary management of chronic pain". Physical Medicine and Rehabilitation Clinics of North America 17 (2): 435–450, vii. May 2006. doi:10.1016/j.pmr.2005.12.004. PMID 16616276.
- ↑ "Medications for acute and chronic low back pain: a review of the evidence for an American Pain Society/American College of Physicians clinical practice guideline". Annals of Internal Medicine 147 (7): 505–514. October 2007. doi:10.7326/0003-4819-147-7-200710020-00008. PMID 17909211.
- ↑ 42.0 42.1 "Chronic widespread pain prevalence in the general population: A systematic review". European Journal of Pain 22 (1): 5–18. January 2018. doi:10.1002/ejp.1090. PMID 28815801.
- ↑ 43.0 43.1 "Nonopioid medications for pain". Physical Medicine and Rehabilitation Clinics of North America 26 (2): 219–248. May 2015. doi:10.1016/j.pmr.2015.01.005. PMID 25952062.
- ↑ 44.0 44.1 "[Opioids in chronic noncancer pain-are opioids superior to nonopioid analgesics? A systematic review and meta-analysis of efficacy, tolerability and safety in randomized head-to-head comparisons of opioids versus nonopioid analgesics of at least four week's duration]" (in de). Schmerz 29 (1): 85–95. February 2015. doi:10.1007/s00482-014-1436-0. PMID 25376546.
- ↑ 45.0 45.1 45.2 "National Institutes of Health Pathways to Prevention Workshop: the role of opioids in the treatment of chronic pain". Annals of Internal Medicine 162 (4): 295–300. February 2015. doi:10.7326/M14-2775. PMID 25581341.
- ↑ "The effectiveness and risks of long-term opioid therapy for chronic pain: a systematic review for a National Institutes of Health Pathways to Prevention Workshop". Annals of Internal Medicine 162 (4): 276–286. February 2015. doi:10.7326/M14-2559. PMID 25581257.
- ↑ 47.0 47.1 47.2 47.3 "Guideline for opioid therapy and chronic noncancer pain". CMAJ 189 (18): E659–E666. May 2017. doi:10.1503/cmaj.170363. PMID 28483845.
- ↑ "Acetaminophen Monograph for Professionals" (in en). https://www.drugs.com/monograph/acetaminophen.html.
- ↑ "A turbulent decade for NSAIDs: update on current concepts of classification, epidemiology, comparative efficacy, and toxicity". Rheumatology International 32 (6): 1491–502. June 2012. doi:10.1007/s00296-011-2263-6. PMID 22193214.
- ↑ "Nonopioid drugs in the treatment of cancer pain". Journal of Clinical Oncology 32 (16): 1677–1690. June 2014. doi:10.1200/JCO.2013.52.8356. PMID 24799483.
- ↑ "Pain and Cancer: A systematic review". The Gulf Journal of Oncology 1 (18): 32–37. May 2015. PMID 26003103.
- ↑ 52.0 52.1 "Amitriptyline for neuropathic pain in adults". The Cochrane Database of Systematic Reviews 7 (7): CD008242. July 2015. doi:10.1002/14651858.CD008242.pub3. PMID 26146793.
- ↑ 53.0 53.1 "Neuropathic pain: principles of diagnosis and treatment". Mayo Clinic Proceedings 90 (4): 532–545. April 2015. doi:10.1016/j.mayocp.2015.01.018. PMID 25841257.
- ↑ "A Systematic Review of Atypical Antipsychotics in Chronic Pain Management: Olanzapine Demonstrates Potential in Central Sensitization, Fibromyalgia, and Headache/Migraine". The Clinical Journal of Pain 34 (6): 585–591. June 2018. doi:10.1097/AJP.0000000000000567. PMID 29077621.
- ↑ "Pharmacological Management of Chronic Pelvic Pain in Women". Drugs 77 (3): 285–301. March 2017. doi:10.1007/s40265-016-0687-8. PMID 28074359.
- ↑ "Therapeutic ultrasound for chronic low back pain". The Cochrane Database of Systematic Reviews 2020 (7): CD009169. July 2020. doi:10.1002/14651858.CD009169.pub3. PMID 32623724.
- ↑ "Assessing the role of cognitive behavioral therapy in the management of chronic nonspecific back pain". Journal of Pain Research 5: 371–380. 2012. doi:10.2147/JPR.S25330. PMID 23091394.
- ↑ "The cognitive behavioral therapy causes an improvement in quality of life in patients with chronic musculoskeletal pain". Arquivos de Neuro-Psiquiatria 70 (11): 864–868. November 2012. doi:10.1590/s0004-282x2012001100008. PMID 23175199.
- ↑ "Acceptance and commitment therapy for fibromyalgia: a randomized controlled trial". European Journal of Pain 17 (4): 599–611. April 2013. doi:10.1002/j.1532-2149.2012.00224.x. PMID 23090719.
- ↑ "Acceptance- and mindfulness-based interventions for the treatment of chronic pain: a meta-analytic review". Cognitive Behaviour Therapy 45 (1): 5–31. 2016. doi:10.1080/16506073.2015.1098724. PMID 26818413. https://research.utwente.nl/en/publications/acceptance-and-mindfulnessbased-interventions-for-the-treatment-of-chronic-pain-a-metaanalytic-review(f2f3c3c2-58a3-4458-a179-659f6990dedd).html.
- ↑ "Brief Mindfulness-Based Interventions for Acute and Chronic Pain: A Systematic Review". Journal of Alternative and Complementary Medicine 25 (3): 265–278. March 2019. doi:10.1089/acm.2018.0351. PMID 30523705.
- ↑ "Starting where I am: a grounded theory exploration of mindfulness as a facilitator of transition in living with a long-term condition". Journal of Advanced Nursing 72 (10): 2445–2456. October 2016. doi:10.1111/jan.12998. PMID 27174075. http://eprints.whiterose.ac.uk/111569/3/LongStarting%20where%20I%20am.pdf.
- ↑ "Psychobiological correlates of improved mental health in patients with musculoskeletal pain after a mindfulness-based pain management program". The Clinical Journal of Pain 29 (3): 233–244. March 2013. doi:10.1097/AJP.0b013e31824c5d9f. PMID 22874090.
- ↑ "Association Between Psychological Interventions and Chronic Pain Outcomes in Older Adults: A Systematic Review and Meta-analysis". JAMA Internal Medicine 178 (6): 830–839. June 2018. doi:10.1001/jamainternmed.2018.0756. PMID 29801109.
- ↑ "Psychological therapies for the management of chronic and recurrent pain in children and adolescents". The Cochrane Database of Systematic Reviews 9 (9): CD003968. September 2018. doi:10.1002/14651858.CD003968.pub5. PMID 30270423.
- ↑ 66.0 66.1 "Physical activity and exercise for chronic pain in adults: an overview of Cochrane Reviews". The Cochrane Database of Systematic Reviews 4 (2): CD011279. April 2017. doi:10.1002/14651858.CD011279.pub3. PMID 28436583.
- ↑ "Patient Outcomes in Dose Reduction or Discontinuation of Long-Term Opioid Therapy: A Systematic Review". Annals of Internal Medicine 167 (3): 181–191. August 2017. doi:10.7326/m17-0598. PMID 28715848.
- ↑ "Opioids for chronic noncancer pain: a position paper of the American Academy of Neurology". Neurology 83 (14): 1277–1284. September 2014. doi:10.1212/wnl.0000000000000839. PMID 25267983.
- ↑ "Incidence of iatrogenic opioid dependence or abuse in patients with pain who were exposed to opioid analgesic therapy: a systematic review and meta-analysis". British Journal of Anaesthesia 120 (6): 1335–1344. June 2018. doi:10.1016/j.bja.2018.03.009. PMID 29793599.
- ↑ 70.0 70.1 70.2 70.3 "Complementary and alternative medicine in chronic pain". Pain 152 (1): 28–30. January 2011. doi:10.1016/j.pain.2010.09.023. PMID 20933330.
- ↑ "What are the benefits and harms of acetyl-L-carnitine for treatment of diabetic peripheral neuropathy (DPN)?". Cochrane Clinical Answers. 2019-10-15. doi:10.1002/cca.2721. ISSN 2050-4217.
- ↑ "Painful diabetic neuropathy: advantage of novel drugs over old drugs?". Diabetes Care 32 (suppl_2): S414–419. November 2009. doi:10.2337/dc09-s350. PMID 19875591.
- ↑ 73.0 73.1 "Preventing paclitaxel-induced peripheral neuropathy: a phase II trial of vitamin E supplementation". Journal of Pain and Symptom Management 32 (3): 237–244. September 2006. doi:10.1016/j.jpainsymman.2006.03.013. PMID 16939848.
- ↑ "Cognitive hypnotherapy for pain management". The American Journal of Clinical Hypnosis 54 (4): 294–310. April 2012. doi:10.1080/00029157.2011.654284. PMID 22655332.
- ↑ "The effectiveness of hypnosis for pain relief: A systematic review and meta-analysis of 85 controlled experimental trials". Neuroscience and Biobehavioral Reviews 99: 298–310. April 2019. doi:10.1016/j.neubiorev.2019.02.013. PMID 30790634. http://gala.gre.ac.uk/id/eprint/23018/7/23108%20THOMPSON_The_Effectiveness_of_Hypnosis_for_Pain_Relief_2019.pdf.
- ↑ "Non-pharmacological interventions for chronic pain in people with spinal cord injury". The Cochrane Database of Systematic Reviews 11 (11): CD009177. November 2014. doi:10.1002/14651858.CD009177.pub2. PMID 25432061.
- ↑ "The Effects of Cannabis Among Adults With Chronic Pain and an Overview of General Harms: A Systematic Review". Annals of Internal Medicine 167 (5): 319–331. September 2017. doi:10.7326/M17-0155. PMID 28806817.
- ↑ "Medical Marijuana: Just the Beginning of a Long, Strange Trip?". Physical Therapy 97 (2): 239–248. February 2017. doi:10.2522/ptj.20160367. PMID 27660328.
- ↑ "[115 Cannabinoids for Chronic Pain | Therapeutics Initiative"]. 23 November 2018. https://www.ti.ubc.ca/2018/11/22/115-cannabinoids-for-chronic-pain/.
- ↑ 80.0 80.1 "Efficacy, tolerability and safety of cannabis-based medicines for chronic pain management – An overview of systematic reviews". European Journal of Pain 22 (3): 455–470. March 2018. doi:10.1002/ejp.1118. PMID 29034533.
- ↑ "Cannabis and cannabinoids for the treatment of people with chronic noncancer pain conditions: a systematic review and meta-analysis of controlled and observational studies". Pain 159 (10): 1932–1954. October 2018. doi:10.1097/j.pain.0000000000001293. PMID 29847469.
- ↑ "The effect of Tai Chi on four chronic conditions-cancer, osteoarthritis, heart failure and chronic obstructive pulmonary disease: a systematic review and meta-analyses". British Journal of Sports Medicine 50 (7): 397–407. April 2016. doi:10.1136/bjsports-2014-094388. PMID 26383108. http://bjsm.bmj.com/cgi/content/short/50/7/397.
- ↑ "Tai Chi for Chronic Pain Conditions: A Systematic Review and Meta-analysis of Randomized Controlled Trials". Scientific Reports 6: 25325. April 2016. doi:10.1038/srep25325. PMID 27125299. Bibcode: 2016NatSR...625325K.
- ↑ "Acupuncture for Chronic Pain: Update of an Individual Patient Data Meta-Analysis". The Journal of Pain 19 (5): 455–474. May 2018. doi:10.1016/j.jpain.2017.11.005. PMID 29198932.
- ↑ "Effect of acupuncture on clinical symptoms and laboratory indicators for chronic prostatitis/chronic pelvic pain syndrome: a systematic review and meta-analysis". International Urology and Nephrology 48 (12): 1977–1991. December 2016. doi:10.1007/s11255-016-1403-z. PMID 27590134.
- ↑ "Non-invasive brain stimulation techniques for chronic pain". The Cochrane Database of Systematic Reviews 4 (8): CD008208. April 2018. doi:10.1002/14651858.CD008208.pub5. PMID 29652088.
- ↑ "Effectiveness of spa therapy for patients with chronic low back pain: An updated systematic review and meta-analysis". Medicine 98 (37): e17092. September 2019. doi:10.1097/MD.0000000000017092. PMID 31517832.
- ↑ "Herbal medicinal products or preparations for neuropathic pain". The Cochrane Database of Systematic Reviews 4 (5): CD010528. April 2019. doi:10.1002/14651858.CD010528.pub4. PMID 30938843.
- ↑ "Effectiveness of Kinesio Taping in Patients With Chronic Nonspecific Low Back Pain: A Systematic Review With Meta-analysis". Spine 44 (1): 68–78. January 2019. doi:10.1097/BRS.0000000000002756. PMID 29952880.
- ↑ "Effectiveness of myofascial release in treatment of chronic musculoskeletal pain: a systematic review". Clinical Rehabilitation 32 (4): 440–450. April 2018. doi:10.1177/0269215517732820. PMID 28956477.
- ↑ "How Prevalent Is Chronic Pain?". Pain Clinical Updates (International Association for the Study of Pain) XI (2): 1–4. June 2003. http://iasp.files.cms-plus.com/Content/ContentFolders/Publications2/PainClinicalUpdates/Archives/PCU03-2_1390265045864_38.pdf.
- ↑ "Survey of chronic pain in Europe: prevalence, impact on daily life, and treatment". European Journal of Pain 10 (4): 287–333. May 2006. doi:10.1016/j.ejpain.2005.06.009. PMID 16095934. https://archive-ouverte.unige.ch/unige:126435.
- ↑ Chronic Pain Syndrome: Practice Essentials, Etiology, Patient Education. February 18, 2022. https://emedicine.medscape.com/article/310834-overview.
- ↑ "Caring for patients with chronic pain: pearls and pitfalls". The Journal of the American Osteopathic Association 113 (8): 620–627. August 2013. doi:10.7556/jaoa.2013.023. PMID 23918913.
- ↑ Institute of Medicine of the National Academies Report (2011). Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research. Washington DC: The National Academies Press.
- ↑ A Call to Revolutionize Chronic Pain Care in America: An Opportunity in Health Care Reform. The Mayday Fund. 2009.
- ↑ "The prevalence of chronic pain in United States adults: results of an Internet-based survey". The Journal of Pain 11 (11): 1230–1239. November 2010. doi:10.1016/j.jpain.2010.07.002. PMID 20797916.
- ↑ 98.0 98.1 Health Canada (2019-08-08). "Canadian Pain Task Force Report: June 2019". https://www.canada.ca/en/health-canada/corporate/about-health-canada/public-engagement/external-advisory-bodies/canadian-pain-task-force/report-2019.html.
- ↑ "Sleep Disorders: Sleep disorders in multiple sclerosis". Handbook of Clinical Neurology 99: 1139–1146. 2011. doi:10.1016/B978-0-444-52007-4.00025-4. ISBN 978-0444520074. PMID 21056246.
- ↑ Research, Center for Drug Evaluation and (2020-03-17). "Drug Interactions: What You Should Know" (in en). FDA. https://www.fda.gov/drugs/resources-drugs/drug-interactions-what-you-should-know.
- ↑ 101.0 101.1 "Severe chronic pain is associated with increased 10 year mortality. A cohort record linkage study". European Journal of Pain 14 (4): 380–386. April 2010. doi:10.1016/j.ejpain.2009.07.006. PMID 19726210.
- ↑ "Hypothalamic-pituitary-adrenal stress axis function and the relationship with chronic widespread pain and its antecedents". Arthritis Research & Therapy 7 (5): R992–R1000. 2005. doi:10.1186/ar1772. PMID 16207340.
- ↑ "Pain and Depression: A Systematic Review". Harvard Review of Psychiatry 26 (6): 352–363. 2018. doi:10.1097/HRP.0000000000000198. PMID 30407234.
- ↑ "The Link between Depression and Chronic Pain: Neural Mechanisms in the Brain". Neural Plasticity 2017: 9724371. 2017-06-19. doi:10.1155/2017/9724371. PMID 28706741.
- ↑ "Effective Coping of Chronic Pain Varies With Psychosocial Resource Profiles". APA Journals Article Spotlight (American Psychological Association). 2019-09-20. https://www.apa.org/pubs/highlights/spotlight/issue-154.
- ↑ "The brain in chronic CRPS pain: abnormal gray-white matter interactions in emotional and autonomic regions". Neuron 60 (4): 570–81. November 2008. doi:10.1016/j.neuron.2008.08.022. PMID 19038215.
- ↑ "Beyond feeling: chronic pain hurts the brain, disrupting the default-mode network dynamics". The Journal of Neuroscience 28 (6): 1398–403. February 2008. doi:10.1523/JNEUROSCI.4123-07.2008. PMID 18256259.
- ↑ "Brain resting state is disrupted in chronic back pain patients". Neuroscience Letters 485 (1): 26–31. November 2010. doi:10.1016/j.neulet.2010.08.053. PMID 20800649.
- ↑ "Chronic pain may change the structure of the brain". Pain 137 (1): 7–15. July 2008. doi:10.1016/j.pain.2008.02.034. PMID 18410991.
- ↑ "Effective treatment of chronic low back pain in humans reverses abnormal brain anatomy and function". The Journal of Neuroscience 31 (20): 7540–50. May 2011. doi:10.1523/JNEUROSCI.5280-10.2011. PMID 21593339.
- ↑ 111.0 111.1 111.2 111.3 "The Interactive Effects of Chronic Pain, Guilt, and Perfectionism on Work Outcomes" (in en). Journal of Applied Social Psychology 40 (1): 76–100. 2010. doi:10.1111/j.1559-1816.2009.00564.x.
- ↑ Clinical manual of pain management in psychiatry. Washington, DC: American Psychiatric Publishing. 2007. p. 58. ISBN 978-1585622757.
- ↑ "Chronic pain and the measurement of personality: do states influence traits?". Pain Medicine 7 (6): 509–529. 1 November 2006. doi:10.1111/j.1526-4637.2006.00239.x. PMID 17112364.
- ↑ "Neuroticism in relation to recovery and persisting pain after laparoscopic cholecystectomy". Scandinavian Journal of Gastroenterology 33 (5): 550–553. May 1998. doi:10.1080/00365529850172151. PMID 9648998.
- ↑ "The validity of Eysenck's neuroticism dimension within the Minnesota Multiphasic Personality Inventory in patients with duodenal ulcer. The Hvidovre Ulcer Project Group". Psychotherapy and Psychosomatics 62 (3–4): 168–175. 1994. doi:10.1159/000288919. PMID 7846260. http://www.hopkinsguides.com/hopkins/ub/citation/7846260/The_validity_of_Eysenck%27s_neuroticism_dimension_within_the_Minnesota_Multiphasic_Personality_Inventory_in_patients_with_duodenal_ulcer__The_Hvidovre_Ulcer_Project_Group_.
- ↑ 116.0 116.1 The Challenge of Pain (2nd ed.). London: Penguin. 1996. pp. 31–32. ISBN 0140256709.
- ↑ "A confirmatory factor analysis of the Pain Catastrophizing Scale: invariant factor structure across clinical and non-clinical populations". Pain 96 (3): 319–324. April 2002. doi:10.1016/S0304-3959(01)00463-8. PMID 11973004.
- ↑ "Pain catastrophizing and neural responses to pain among persons with fibromyalgia". Brain 127 (Pt 4): 835–843. April 2004. doi:10.1093/brain/awh098. PMID 14960499.
- ↑ "The causal status of pain catastrophizing: an experimental test with healthy participants". European Journal of Pain 9 (3): 257–265. June 2005. doi:10.1016/j.ejpain.2004.07.005. PMID 15862475.
- ↑ "Chronic Pain Types Differ in Their Reported Prevalence of Post–Traumatic Stress Disorder (PTSD) and There Is Consistent Evidence That Chronic Pain Is Associated with PTSD: An Evidence-Based Structured Systematic Review". Pain Medicine 18 (4): 711–735. April 2017. doi:10.1093/pm/pnw065. PMID 27188666. https://academic.oup.com/painmedicine/article-lookup/doi/10.1093/pm/pnw065.
- ↑ "The relationship between PTSD and chronic pain: mediating role of coping strategies and depression". Pain 154 (4): 609–616. April 2013. doi:10.1016/j.pain.2013.01.001. PMID 23398939.
- ↑ "Post-traumatic stress disorder moderates the relationship between trauma exposure and chronic pain". European Journal of Psychotraumatology 8 (1): 1375337. January 2017. doi:10.1080/20008198.2017.1375337. PMID 29038680.
- ↑ Sheng, Jiyao; Liu, Shui; Wang, Yicun; Cui, Ranji; Zhang, Xuewen (2017). "The Link between Depression and Chronic Pain: Neural Mechanisms in the Brain". Neural Plasticity 2017: 9724371. doi:10.1155/2017/9724371. ISSN 2090-5904. PMID 28706741.
- ↑ "Chronic pain and depression". British Journal of Anaesthesia 14 (2): 85–9. 1 April 2014. doi:10.1093/bjaceaccp/mkt046. https://www.bjaed.org/article/S1743-1816(17)30112-9/fulltext.
- ↑ "Chronic pain: supporting safer prescribing of analgesics". British Medical Association. 2017. https://www.bma.org.uk/media/2100/analgesics-chronic-pain.pdf.
- ↑ "Cognitive impairment in chronic pain" (pdf). Pain: Clinical Updates XV (4): 1–4. 2007. https://www.iasp-pain.org/PublicationsNews/NewsletterIssue.aspx?ItemNumber=2111. Retrieved 2019-01-06.
- ↑ "The Relationship Between Chronic Pain and Neurocognitive Function: A Systematic Review". The Clinical Journal of Pain 34 (3): 262–275. March 2018. doi:10.1097/AJP.0000000000000536. PMID 28719507.
- ↑ Cavalcante, Alexandre N.; Sprung, Juraj; Schroeder, Darrell R.; Weingarten, Toby N. (July 2017). "Multimodal Analgesic Therapy With Gabapentin and Its Association With Postoperative Respiratory Depression". Anesthesia and Analgesia 125 (1): 141–146. doi:10.1213/ANE.0000000000001719. ISSN 1526-7598. PMID 27984223. https://pubmed.ncbi.nlm.nih.gov/27984223/.
- ↑ Gomes, Tara; Greaves, Simon; van den Brink, Wim; Antoniou, Tony; Mamdani, Muhammad M.; Paterson, J. Michael; Martins, Diana; Juurlink, David N. (2018-11-20). "Pregabalin and the Risk for Opioid-Related Death: A Nested Case-Control Study". Annals of Internal Medicine 169 (10): 732–734. doi:10.7326/M18-1136. ISSN 1539-3704. PMID 30140853. https://pubmed.ncbi.nlm.nih.gov/30140853/.
- ↑ Watkins, Paul B.; Kaplowitz, Neil; Slattery, John T.; Colonese, Connie R.; Colucci, Salvatore V.; Stewart, Paul W.; Harris, Stephen C. (2006-07-05). "Aminotransferase elevations in healthy adults receiving 4 grams of acetaminophen daily: a randomized controlled trial". JAMA 296 (1): 87–93. doi:10.1001/jama.296.1.87. ISSN 1538-3598. PMID 16820551. https://pubmed.ncbi.nlm.nih.gov/16820551/.
- ↑ Holubek, William J.; Kalman, Susanne; Hoffman, Robert S. (April 2004). "Acetaminophen-induced acute liver failure: results of a United States multicenter, prospective study". Hepatology (Baltimore, Md.) 43 (4): 880; author reply 882. doi:10.1002/hep.21106. ISSN 0270-9139. PMID 16557558. https://pubmed.ncbi.nlm.nih.gov/16557558/.
- ↑ Jalan, Rajiv; Williams, Roger; Bernuau, Jacques (2006-12-23). "Paracetamol: are therapeutic doses entirely safe?". Lancet (London, England) 368 (9554): 2195–2196. doi:10.1016/S0140-6736(06)69874-7. ISSN 1474-547X. PMID 17189017. https://pubmed.ncbi.nlm.nih.gov/17189017/.
- ↑ Lee, Marion; Silverman, Sanford M.; Hansen, Hans; Patel, Vikram B.; Manchikanti, Laxmaiah (2011). "A comprehensive review of opioid-induced hyperalgesia". Pain Physician 14 (2): 145–161. ISSN 2150-1149. PMID 21412369. https://pubmed.ncbi.nlm.nih.gov/21412369/.
- ↑ Turk, Dennis C.; Wilson, Hilary D.; Cahana, Alex (2011-06-25). "Treatment of chronic non-cancer pain". Lancet (London, England) 377 (9784): 2226–2235. doi:10.1016/S0140-6736(11)60402-9. ISSN 1474-547X. PMID 21704872. https://pubmed.ncbi.nlm.nih.gov/21704872/.
- ↑ Farrar, John T.; Young, James P.; LaMoreaux, Linda; Werth, John L.; Poole, Michael R. (November 2001). "Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale". Pain 94 (2): 149–158. doi:10.1016/S0304-3959(01)00349-9. ISSN 0304-3959. PMID 11690728. https://pubmed.ncbi.nlm.nih.gov/11690728/.
- ↑ Price, D. D. (2000-06-09). "Psychological and neural mechanisms of the affective dimension of pain". Science (New York, N.Y.) 288 (5472): 1769–1772. doi:10.1126/science.288.5472.1769. ISSN 0036-8075. PMID 10846154. https://pubmed.ncbi.nlm.nih.gov/10846154/.
- ↑ Clark, Lauren; Jones, Katherine; Pennington, Karen (November 2004). "Pain assessment practices with nursing home residents". Western Journal of Nursing Research 26 (7): 733–750. doi:10.1177/0193945904267734. ISSN 0193-9459. PMID 15466611. https://pubmed.ncbi.nlm.nih.gov/15466611/.
- ↑ Closs, S. José; Briggs, Michelle (July 2002). "Patients' verbal descriptions of pain and discomfort following orthopaedic surgery". International Journal of Nursing Studies 39 (5): 563–572. doi:10.1016/s0020-7489(01)00067-0. ISSN 0020-7489. PMID 11996877. https://pubmed.ncbi.nlm.nih.gov/11996877/.
- ↑ 139.0 139.1 139.2 Tang, Nicole K. Y.; Crane, Catherine (May 2006). "Suicidality in chronic pain: a review of the prevalence, risk factors and psychological links". Psychological Medicine 36 (5): 575–586. doi:10.1017/S0033291705006859. ISSN 0033-2917. PMID 16420727. https://pubmed.ncbi.nlm.nih.gov/16420727/.
- ↑ 140.0 140.1 140.2 Petrosky, Emiko; Harpaz, Rafael; Fowler, Katherine A.; Bohm, Michele K.; Helmick, Charles G.; Yuan, Keming; Betz, Carter J. (2018-10-02). "Chronic Pain Among Suicide Decedents, 2003 to 2014: Findings From the National Violent Death Reporting System". Annals of Internal Medicine 169 (7): 448–455. doi:10.7326/M18-0830. ISSN 1539-3704. PMID 30208405. PMC 6913029. https://pubmed.ncbi.nlm.nih.gov/30208405/.
- ↑ "Overview of persistent pain in older adults". The American Psychologist 69 (2): 197–207. 2014. doi:10.1037/a0035794. PMID 24547805.
- ↑ "Cancer pain and psychosocial factors: a critical review of the literature". Journal of Pain and Symptom Management 24 (5): 526–542. November 2002. doi:10.1016/s0885-3924(02)00497-9. PMID 12547052.
- ↑ 143.0 143.1 "A Systematic Review of the Impact of Physician Implicit Racial Bias on Clinical Decision Making". Academic Emergency Medicine 24 (8): 895–904. August 2017. doi:10.1111/acem.13214. PMID 28472533.
- ↑ 144.0 144.1 144.2 "Racial/ethnic disparities in the assessment and treatment of pain: psychosocial perspectives". The American Psychologist 69 (2): 131–141. 2014. doi:10.1037/a0035204. PMID 24547799.
- ↑ "4 Ways Racism in Health Care Is Still a Problem Today". ThoughtCo. https://www.thoughtco.com/racism-in-health-care-still-a-problem-2834530.
- ↑ "Perceived Injustice and Adverse Recovery Outcomes". Psychological Injury and Law 7 (4): 325–334. 1 November 2014. doi:10.1007/s12207-014-9209-8.
- ↑ "The role of perceived injustice in the experience of chronic pain and disability: scale development and validation". Journal of Occupational Rehabilitation 18 (3): 249–261. September 2008. doi:10.1007/s10926-008-9140-5. PMID 18536983.
- ↑ "Perceived injustice in chronic pain: an examination through the lens of predictive processing". Pain Management 8 (2): 129–138. March 2018. doi:10.2217/pmt-2017-0051. PMID 29451429.
- ↑ 149.0 149.1 "Chronic pain experience and health inequities during the COVID-19 pandemic in Canada: qualitative findings from the chronic pain & COVID-19 pan-Canadian study". International Journal for Equity in Health 20 (1): 147. June 2021. doi:10.1186/s12939-021-01496-1. PMID 34162393.
- ↑ "Grieving Life and Loss". Monitor on Psychology 51 (4). June 2020. https://www.apa.org/monitor/2020/06/covid-grieving-life.
- ↑ "Stigma, Liminality, and Chronic Pain: Mind-Body Borderlands". American Ethnologist 32 (3): 332–353. 2005. doi:10.1525/ae.2005.32.3.332. ISSN 0094-0496. https://www.jstor.org/stable/3805289.
Further reading
- "CDC Guideline for Prescribing Opioids for Chronic Pain – United States, 2016". JAMA 315 (15): 1624–1645. April 2016. doi:10.1001/jama.2016.1464. PMID 26977696.
External links
| Classification | |
|---|---|
| External resources |
 |

