Medicine:Pharmacological therapy
| It has been suggested that this page be merged into Pharmacotherapy. (Discuss) |
Pharmacological therapy, also known as pharmacotherapy or drug therapy, is defined as medical treatment that utilizes one or more pharmaceutical drugs to improve on-going symptoms (symptomatic relief), treat the underlying condition, or act as a prevention for other diseases (prophylaxis). Today's pharmacological therapy has evolved from a long history of medication use, and it has changed most rapidly in the last century due to advancements in drug discovery. The therapy is administered and adjusted by healthcare professionals according to the evidence-based guidelines and the patient's health condition. Personalized medicine also plays a crucial role in pharmacological therapy. Personalized medicine, or precision medicine, takes account of the patient's genetic variation, liver function, kidney function, etc, to provide a tailor-made treatment for a patient. In pharmacological therapy, pharmacists will also consider medication compliance. Medication compliance, or medication adherence, is defined as the degree to which the patient follows the therapy that is recommended by the healthcare professionals.[1]
History
From natural compounds to pharmaceutical drugs
The use of medicinal substances can be traced back to 4000 BC in the Sumer civilization.[2] Healers at the time (called apothecaries), for example, understood the application of opium for pain relief.[3] The history of natural remedies can also be found in other cultures, including traditional Chinese medicine in China and Ayurvedic medicine in India, which are still in use nowadays.[4] Dioscorides, a 1st -century Greek surgeon, described more than six hundred animals, plants, and their derivatives in his medical botany, which remained the most influential pharmacopeia for fourteen hundred years.[5] Besides substances derived from living organisms, metals, including copper, mercury, and antimony, were also used as medical therapies.[5] They were said to cure various diseases during the late Renaissance. In 1657, tartar emetic, which is an antimony compound, was credited with curing Louis XIV of typhoid fever.[5] The drug was also administered intravenously for the treatment of schistosomiasis in the 20th century.[6] However, due to the concern over acute and chronic antimony poisoning, the role of tartar emetic as an antischistosomal agent was gradually replaced after the advent of praziquantel[6].
Other than using natural products, humans also learned to compound medicine by themselves. The first pharmaceutical text was found on clay tablets from the Mesopotamians, who lived around 2100 BC.[4] Later in the 2nd century AD, compounding was formally introduced by Galen as “a process of mixing two or more medicines to meet the individual needs of a patient”.[4] Initially, compounding was only done by individual pharmacists, but in the post-World War II period, pharmaceutical manufacturers surged in number and took over the role of making medicine.[2] Meanwhile, there was a marked increase in pharmaceutical research, which led to a growing number of new drugs.[2] Most drug discovery milestones were made in the last hundred years, from antibiotics to biologics,[4] contributing to the foundation of current pharmacological therapy.
Drug discovery
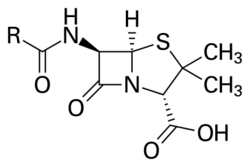
Most drugs were discovered by empirical means, including observation, accident, and trial and error.[5] One famous example is the discovery of penicillin, the first antibiotic in the world. The substance was discovered by Alexander Fleming in 1928 after a combination of unanticipated events occurred in his laboratory during his summer vacation.[7] The Penicillium mold on the petri dish was believed to secrete a substance (later named "penicillin") that inhibited bacterial growth.[7] Large pharmaceutical companies then started to establish their microbiological departments and search for new antibiotics.[8] The screening program for antimicrobial compounds also led to the discovery of drugs with other pharmacological properties, such as immunosuppressants like Cyclosporin A.[8]
The discovery of penicillin was a serendipitous (i.e. chance) discovery. Another, more advanced approach to drug discovery is rational drug design. The method is underpinned by an understanding of the biological targets of the drugs, including enzymes, receptors, and other proteins. In the late 19th century, Paul Ehrlich observed the selective affinity of dyes for different tissues and proposed the existence of chemoreceptors in our bodies.[8][9] Receptors were believed to be the specific binding sites for drugs.[8] The drug-receptor recognition was described as a key-and-lock interplay by Emil Fischer in the early 1890s.[10] It was later found that the receptors can either be stimulated or inhibited by chemotherapeutic agents to attain the desired physiological response.[8] Once the ligand interacting with the target macromolecule is identified, drug candidates can be designed and optimized based on the structure-activity relationship.[10] Nowadays, artificial intelligence is employed in drug design to predict drug-protein interactions, drug activity, the 3D configuration of proteins, etc.[10]
Evidence-based medicine
Evidence-based medicine is defined as deploying the best current scientific evidence that is available to give the best treatment and make the best decision effectively and efficiently.[11] Clinical guidelines are developed based on scientific evidence; for example, the ACC/AHA guidelines (for cardiovascular diseases), the GOLD guidelines (for chronic obstructive pulmonary disease), the GINA guidelines (for asthma), etc. They convert and classify the evidence using a systematic method, aiming to provide care with quality.[12] The guidelines cannot substitute clinical judgment, as they cannot meet all the circumstances.[12] Healthcare professionals can use the clinical guidelines as references or evidence to support their clinical judgement when prescribing therapy to patients.
Example: Clinical Guideline for controlling blood pressure (hypertension)
If there is an Asian male patient who is 40 years old and has recently been diagnosed with high blood pressure (with a blood pressure of 140/90) and without any other chronic diseases (comorbidities), such as type-2 diabetes, gout, benign prostatic hyperplasia, etc. His estimated 10-year risk of cardiovascular disease is 15%.
According to the NICE 2019 Hypertension guideline, the healthcare professional can consider starting anti-hypertensive therapy after a discussion with the patient.[13] The first-line therapy will be either an Angiotensin Converting Enzyme Inhibitor (ACEi) or an Angiotensin receptor blocker (ARB) (if the patient cannot tolerate ACEi).[13] If the blood pressure of the patient is not well controlled, the healthcare professionals can consider adding a calcium channel blocker (CCB)[14] or a Thiazide-like diuretic to the previous therapy, i,e, ACEi or ARBs with a CCB or a thiazide-like diuretic.[13]
Personalized medicine
Every patient has their own body condition, for example, kidney function, liver function, genetic variations, medical history, etc. These are all the factors that should be considered by healthcare professionals before giving any pharmacological therapy. Most importantly, the advancing technology in genetics guides us to have more insight into the linkage between health and genes.[15] In pharmacological therapy, two areas of study are evolving: pharmacogenetics and pharmacogenomics. Age will affect the pharmacokinetics and pharmacodynamics of drugs, and hence the efficacy of the therapy. The effect of age causes deterioration of organ function,[16] like liver function and kidney function. Pharmacokinetics is the study of drugs' effects on absorption, distribution, metabolism, and elimination. Pharmacodynamics is the study of drugs' effects on our body and their mechanisms.
Pharmacogenetics and pharmacogenomics
Pharmacogenetics is defined as the study of inherited genes causing different drug metabolisms that vary from each other, such as the rate of metabolism and metabolites.[17] Pharmacogenomics is defined as the study of associating the drug response with one's gene.[18] Both terms are similar in nature, so they are used interchangeably.
Multiple alleles can contribute together to a change in response to a drug by expressing a different form of an enzyme that responds differently than the normal ones.[17] The different forms of enzymes (phenotypes) include ultra-rapid metabolizers, moderate metabolizers, no-enzyme activity, etc. The genetic variations can also be used to match the particular adverse drug reaction in order to prevent the patient from suffering the unfavorable outcomes.[19] The genetic make-up can affect the pharmacokinetics.
Example: Azathioprine Therapy
Azathioprine is an immunomodulator for inflammatory bowel disease, for instance. Its metabolite relies on two different enzymes (TPMT and NUDT15) to eliminate its effect on our body during its metabolism. If the patient has the phenotype of the enzymes that metabolize it poorly, i.e., the poor metabolizer, more toxic metabolites are accumulated in the body. Thus, the patient has a greater risk of the related side-effect.[20] The side effect causes the adjustment of dosage[20] or switching to another drug.
Example: Omalizumab Therapy
Omalizumab is a humanized monoclonal antibody for the treatment of various allergic diseases, including asthma, urticaria, and allergic rhinitis.[21] It targets the immunoglobulin E (IgE) in human body, which plays an important role in allergic reactions.[22] The efficacy of omalizumab may vary among patients. To identify responders to omalizumab, the level of several biomarkers can be measured, including serum eosinophils, fractional exhaled nitric oxide, and serum IgE.[22][23] For instance, patients with higher baseline eosinophil counts are likely to respond better to omalizumab therapy.[23]
Medication compliance
Medication compliance is defined as the degree to which the patient follows the therapy that is recommended by healthcare professionals.[1] There are direct and indirect methods to evaluate compliance. Direct method refers to the measurement that the healthcare professionals observed or measure the patient's drug-taking behavior. Indirect method refers to the healthcare professionals do not observe or measure the drug-taking behavior of the patient but use the other source of information to evaluate the compliance.
The direct method includes measurement of drug (or the corresponding metabolite) concentration,[1][24] while the indirect method includes pill counting[1][24] and the self-report from the patient.[1][24] The direct method is more time-consuming, more expensive, more invasive, but it is more accurate.[1] The indirect method has a lower accuracy but is easier to administer to the patient.[1] If the patient fails to comply with treatment, for example, by not taking the medication according to the instructions, it leads to risk and a poor treatment outcome.
Example: Tuberculosis treatment
For tuberculosis patients, directly observed therapy is still part of the treatment.[25] This is to increase medication compliance.[26] This is to prevent treatment failure, relapse, and transmission in the community.[27] Apart from the traditional direct observed therapy (DOT), there is another method proposed to try increasing medication compliance. Video-observed therapy (VOT) is one of the methods. It has some advantages and disadvantages. It reduces the cost of healthcare and the travel costs for the patient.[26] The downside of the intervention is the need for quality control training as it would be hard to confirm the patient's adherence.[26]
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 Simon, Steven T.; Kini, Vinay; Levy, Andrew E.; Ho, P. Michael (2021-08-11). "Medication adherence in cardiovascular medicine". BMJ (Clinical research ed.) 374: n1493. doi:10.1136/bmj.n1493. ISSN 1756-1833. PMID 34380627. https://pubmed.ncbi.nlm.nih.gov/34380627.
- ↑ 2.0 2.1 2.2 "Historical Evolution of Pharmacy Practice". Encyclopedia of pharmacy practice and clinical pharmacy. 1. Zaheer-ud-din Babar. Amsterdam, Netherlands. 2019. pp. 191–202. ISBN 978-0-12-812736-0. OCLC 1110705461. https://www.worldcat.org/oclc/1110705461.
- ↑ Thum Bonanno, Sarah; Gill, Jennifer; Davies, James; Wlodarski, Michal; Taylor, David (2012). From making medicines to optimising outcomes : the evolution of a profession 1912-2012. Federation Internationale Pharmaceutique. OCLC 926313996. http://worldcat.org/oclc/926313996.
- ↑ 4.0 4.1 4.2 4.3 Barrett, Jeffrey S. (2022). Fundamentals of drug development. Hoboken, NJ. ISBN 978-1-119-91327-6. OCLC 1333930216. https://www.worldcat.org/oclc/1333930216.
- ↑ 5.0 5.1 5.2 5.3 Duffin, Jacalyn (1999). "Five: History of Pharmacology". History of medicine : a scandalously short introduction. Toronto: University of Toronto Press. pp. 90–114. ISBN 0-8020-0949-2. OCLC 40982537. https://www.worldcat.org/oclc/40982537.
- ↑ 6.0 6.1 Hagan, Paul (2009). "Schistosomiasis – a rich vein of research" (in en). Parasitology 136 (12): 1611–1619. doi:10.1017/S003118200999093X. ISSN 0031-1820. https://www.cambridge.org/core/product/identifier/S003118200999093X/type/journal_article.
- ↑ 7.0 7.1 Sneader, Walter (2005). "Antibiotics". Drug discovery : a history. Chichester, England: Wiley. pp. 287–318. ISBN 978-0-470-01553-7. OCLC 154714913. https://www.worldcat.org/oclc/154714913.
- ↑ 8.0 8.1 8.2 8.3 8.4 Drews, Jürgen (2000-03-17). "Drug Discovery: A Historical Perspective" (in en). Science 287 (5460): 1960–1964. doi:10.1126/science.287.5460.1960. ISSN 0036-8075. https://www.science.org/doi/10.1126/science.287.5460.1960.
- ↑ "Drugs Originating from the Screening of Dyes", Drug Discovery (Chichester, UK: John Wiley & Sons, Ltd): pp. 375–402, 2006-01-27, ISBN 978-0-470-01553-7, http://dx.doi.org/10.1002/0470015535.ch27, retrieved 2023-04-03
- ↑ 10.0 10.1 10.2 Doytchinova, Irini (2022-02-23). "Drug Design—Past, Present, Future" (in en). Molecules 27 (5): 1496. doi:10.3390/molecules27051496. ISSN 1420-3049. PMID 35268598. PMC 8911833. https://www.mdpi.com/1420-3049/27/5/1496.
- ↑ Li, Shu; Cao, Meijuan; Zhu, Xuejiao. "Evidence-based practice: Knowledge, attitudes, implementation, facilitators, and barriers among community nurses—systematic review" (in en). Medicine 98 (39): e17209. doi:10.1097/MD.0000000000017209. ISSN 0025-7974. https://journals.lww.com/10.1097/MD.0000000000017209.
- ↑ 12.0 12.1 Grundy, Scott M.; Stone, Neil J.; Bailey, Alison L.; Beam, Craig; Birtcher, Kim K.; Blumenthal, Roger S.; Braun, Lynne T.; de Ferranti, Sarah et al. (2019-06-18). "2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines" (in en). Circulation 139 (25). doi:10.1161/CIR.0000000000000625. ISSN 0009-7322. https://www.ahajournals.org/doi/10.1161/CIR.0000000000000625.
- ↑ 13.0 13.1 13.2 "Recommendations | Hypertension in adults: diagnosis and management | Guidance | NICE". https://www.nice.org.uk/guidance/ng136/chapter/Recommendations#starting-antihypertensive-drug-treatment.
- ↑ Whelton, Paul K.; Carey, Robert M.; Aronow, Wilbert S.; Casey, Donald E.; Collins, Karen J.; Dennison Himmelfarb, Cheryl; DePalma, Sondra M.; Gidding, Samuel et al.. "2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines" (in en). Hypertension 71 (6). doi:10.1161/HYP.0000000000000065. ISSN 0194-911X. https://www.ahajournals.org/doi/10.1161/HYP.0000000000000065.
- ↑ Goetz, Laura H.; Schork, Nicholas J.. "Personalized medicine: motivation, challenges, and progress". Fertility and Sterility 109 (6): 952–963. doi:10.1016/j.fertnstert.2018.05.006. ISSN 1556-5653. PMID 29935653. PMC 6366451. https://pubmed.ncbi.nlm.nih.gov/29935653.
- ↑ Andres, Tate M.; McGrane, Tracy; McEvoy, Matthew D.; Allen, Brian F. S.. "Geriatric Pharmacology: An Update". Anesthesiology Clinics 37 (3): 475–492. doi:10.1016/j.anclin.2019.04.007. ISSN 1932-2275. PMID 31337479. https://pubmed.ncbi.nlm.nih.gov/31337479.
- ↑ 17.0 17.1 Khalil, Islam A. (2021-11-24) (in en). Introductory Chapter. IntechOpen. ISBN 978-1-83969-218-5. https://www.intechopen.com/chapters/78925.
- ↑ Pharmacogenomics : a primer for clinicians. Jerika T. Lam, Mary A. Gutierrez, Samit Shah. [New York]. 2021. ISBN 978-1-260-45710-0. OCLC 1242235520. https://www.worldcat.org/oclc/1242235520.
- ↑ López-Fernández, Luis A. (2022-02-22) (in en). Pharmacogenetics to Avoid Adverse Drug Reactions. MDPI, Basel. ISBN 978-3-0365-3344-5. https://www.mdpi.com/books/book/5039.
- ↑ 20.0 20.1 Dean, Laura (2012), Pratt, Victoria M.; Scott, Stuart A.; Pirmohamed, Munir et al., eds., "Azathioprine Therapy and TPMT and NUDT15 Genotype", Medical Genetics Summaries (Bethesda (MD): National Center for Biotechnology Information (US)), PMID 28520349, http://www.ncbi.nlm.nih.gov/books/NBK100661/, retrieved 2023-03-12
- ↑ Okayama, Yoshimichi; Matsumoto, Hisako; Odajima, Hiroshi; Takahagi, Shunsuke; Hide, Michihiro; Okubo, Kimihiro (2020-04-01). "Roles of omalizumab in various allergic diseases" (in en). Allergology International 69 (2): 167–177. doi:10.1016/j.alit.2020.01.004. ISSN 1323-8930. https://www.sciencedirect.com/science/article/pii/S1323893020300101.
- ↑ 22.0 22.1 Kawakami, Toshiaki; Blank, Ulrich (2016-12-01). "From IgE to Omalizumab". The Journal of Immunology 197 (11): 4187–4192. doi:10.4049/jimmunol.1601476. ISSN 0022-1767. PMID 27864548. PMC 5123831. https://doi.org/10.4049/jimmunol.1601476.
- ↑ 23.0 23.1 Tabatabaian, Farnaz; Ledford, Dennis K. (2018-04-03). "Omalizumab for severe asthma: toward personalized treatment based on biomarker profile and clinical history" (in English). Journal of Asthma and Allergy 11: 53–61. doi:10.2147/JAA.S107982. PMID 29662320. PMC 5892947. https://www.dovepress.com/omalizumab-for-severe-asthma-toward-personalized-treatment-based-on-bi-peer-reviewed-fulltext-article-JAA.
- ↑ 24.0 24.1 24.2 Farmer, Kevin C. (1999-06-01). "Methods for measuring and monitoring medication regimen adherence in clinical trials and clinical practice" (in English). Clinical Therapeutics 21 (6): 1074–1090. doi:10.1016/S0149-2918(99)80026-5. ISSN 0149-2918. https://www.clinicaltherapeutics.com/article/S0149-2918(99)80026-5/abstract.
- ↑ Haas, Michelle K.; Belknap, Robert W.. "Updates in the Treatment of Active and Latent Tuberculosis". Seminars in Respiratory and Critical Care Medicine 39 (3): 297–309. doi:10.1055/s-0038-1660863. ISSN 1098-9048. PMID 30071545. https://pubmed.ncbi.nlm.nih.gov/30071545.
- ↑ 26.0 26.1 26.2 Garfein, Richard S.; Doshi, Riddhi P.. "Synchronous and asynchronous video observed therapy (VOT) for tuberculosis treatment adherence monitoring and support". Journal of Clinical Tuberculosis and Other Mycobacterial Diseases 17: 100098. doi:10.1016/j.jctube.2019.100098. ISSN 2405-5794. PMID 31867442. PMC 6904830. https://pubmed.ncbi.nlm.nih.gov/31867442.
- ↑ Alipanah, Narges; Jarlsberg, Leah; Miller, Cecily; Linh, Nguyen Nhat; Falzon, Dennis; Jaramillo, Ernesto; Nahid, Payam. "Adherence interventions and outcomes of tuberculosis treatment: A systematic review and meta-analysis of trials and observational studies". PLoS medicine 15 (7): e1002595. doi:10.1371/journal.pmed.1002595. ISSN 1549-1676. PMID 29969463. PMC 6029765. https://pubmed.ncbi.nlm.nih.gov/29969463.