Medicine:Radiofrequency ablation
| Radiofrequency ablation | |
|---|---|
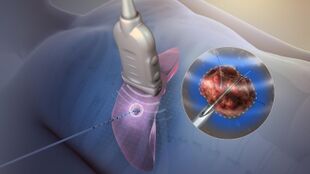 Tissue ablation using radiofrequency. | |
| Specialty | Interventional radiology |
| ICD-9-CM | 01.32, 04.2, 37.33, 37.34, 60.97 |
| MeSH | D017115 |
Radiofrequency ablation (RFA), also called fulguration,[1] is a medical procedure in which part of the electrical conduction system of the heart, tumor, sensory nerves or a dysfunctional tissue is ablated using the heat generated from medium frequency alternating current (in the range of 350–500 kHz).[2][3] RFA is generally conducted in the outpatient setting, using either a local anesthetic[3] or twilight anesthesia. When it is delivered via catheter, it is called radiofrequency catheter ablation.
Two advantages of radio frequency current (over previously used low frequency AC or pulses of DC) are that it does not directly stimulate nerves or heart muscle, and therefore can often be used without the need for general anesthesia, and that it is specific for treating the desired tissue without significant collateral damage.[3][4] Due to this, RFA is an alternative for eligible patients who have comorbidities or do not want to undergo surgery.[3][5][6]
Documented benefits have led to RFA becoming widely used during the 21st century.[3][5][7][8][9] RFA procedures are performed under image guidance (such as X-ray screening, CT scan or ultrasound) by an interventional pain specialist (such as an anesthesiologist), interventional radiologist, otolaryngologists, a gastrointestinal or surgical endoscopist, or a cardiac electrophysiologist, a subspecialty of cardiologists.
Tumors

RFA may be performed to treat tumors in the lung,[10][11][12] liver,Cite error: Closing </ref> missing for <ref> tag
Radiofrequency ablation is also used in pancreatic cancer and bile duct cancer.[13]
RFA has become increasingly important in the care of benign bone tumors, most notably osteoid osteomas. Since the procedure was first introduced for the treatment of osteoid osteomas in the 1990s,[14] it has been shown in numerous studies to be less invasive and expensive, to result in less bone destruction and to have equivalent safety and efficacy to surgical techniques, with 66 to 95% of people reporting freedom from symptoms.[15][16][17] While initial success rates with RFA are high, symptom recurrence after RFA treatment has been reported, with some studies demonstrating a recurrence rate similar to that of surgical treatment.[18] RFA is also increasingly used in the palliative treatment of painful metastatic bone disease in people who are not eligible or do not respond to traditional therapies ( i.e. radiation therapy, chemotherapy, palliative surgery, bisphosphonates or analgesic medications).[19]
Cardiology
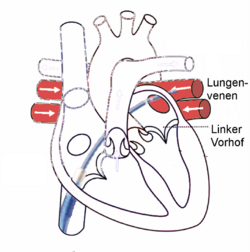
Radiofrequency energy is used in heart tissue or normal parts to destroy abnormal electrical pathways that are contributing to a cardiac arrhythmia. It is used in recurrent atrial flutter (Afl), atrial fibrillation (AF), supraventricular tachycardia (SVT), atrial tachycardia, Multifocal Atrial Tachycardia (MAT) and some types of ventricular arrhythmia. The energy-emitting probe (electrode) is at the tip of a catheter which is placed into the heart, usually through a vein. This catheter is called the ablator. The practitioner first "maps" an area of the heart to locate the abnormal electrical activity (electrophysiology study) before the responsible tissue is eliminated. Radiofrequency ablation technique can be used in AF, either to block the atrioventricular node after implantation of a pacemaker or to block conduction within the left atrium, especially around the pulmonary veins. Radiofrequency ablation for AF can be unipolar (one electrode) or bipolar (two electrodes).[20] Although bipolar can be more successful, it is technically more difficult, resulting in unipolar being used more often.[20] But bipolar is more effective in preventing recurrent atrial arrhythmias.[21]
Ablation is now the standard treatment for SVT and typical atrial flutter, In some conditions, especially forms of intra-nodal re-entry (the most common type of SVT), also called atrioventricular nodal reentrant tachycardia or AVNRT, ablation can also be accomplished by cryoablation (tissue freezing using a coolant which flows through the catheter) which avoids the risk of complete heart block – a potential complication of radiofrequency ablation in this condition. Recurrence rates with cryoablation are higher, though.[22] Microwave ablation, where tissue is ablated by the microwave energy "cooking" the adjacent tissue, and ultrasonic ablation, creating a heating effect by mechanical vibration, or laser ablation have also been developed but are not in widespread use.
Renal sympathetic denervation
A new indication for the use of radiofrequency technology has made news in the last few years. Hypertension is a very common condition, with about 1 billion people over the world, nearly 75 million in the US alone. Complications of inadequately controlled hypertension are many and have both individual and global impact. Treatment options include medications, diet, exercise, weight reduction and meditation. Inhibition of the neural impulses that are believed to cause or worsen hypertension has been tried for a few decades. Surgical sympathectomy has helped but not without significant side effects. Therefore, the introduction of non-surgical means of renal denervation using a radiofrequency ablation catheter was enthusiastically welcomed. Although the initial use of radiofrequency-generated heat to ablate nerve endings in the renal arteries to aid in management of 'resistant hypertension' were encouraging, the most recent phase 3 studying looking at catheter-based renal denervation for the treatment of resistant hypertension failed to show any significant reduction in systolic blood pressure.[23]
Aesthetics dermatology
Radiofrequency ablation[24] is a dermatosurgical procedure by using various forms of alternating current. Types of radiofrequency are electrosection, electrocoagulation, electrodessication and fulguration. The use of radiofrequency ablation has obtained importance as it can be used to treat most of the skin lesions with minimal side effects and complications.
Varicose veins
Radiofrequency ablation is a minimally invasive procedure used in the treatment of varicose veins. It is an alternative to the traditional stripping operation. Under ultrasound guidance, a radiofrequency catheter is inserted into the abnormal vein and the vessel treated with radio-energy, resulting in closure of the involved vein. Radiofrequency ablation is used to treat the great saphenous vein, the small saphenous vein, and the perforator veins. The latter are connecting veins that transport blood from the superficial veins to the deep veins. Branch varicose veins are then usually treated with other minimally invasive procedures, such as ambulatory phlebectomy, sclerotherapy, or foam sclerotherapy. Currently, the VNUS ClosureRFS stylet is the only device specifically cleared by FDA for endovenous ablation of perforator veins.[25]
The possibility of skin burn during the procedure is very small, because the large volumes (500 cc) of dilute Lidocaine (0.1%) tumescent anesthesia injected along the entire vein prior to the application of radiofrequency provide a heat sink that absorbs the heat created by the device. Early studies have shown a high success rate with low rates of complications.[26]
Obstructive sleep apnea
RFA was first studied in obstructive sleep apnea (OSA) in a pig model.[27] RFA has been recognized as a somnoplasty treatment option in selected situations by the American Academy of Otolaryngology[27] but was not endorsed for general use in the American College of Physicians guidelines.[28]
The clinical application of RFA in obstructive sleep apnea is reviewed in that main article, including controversies and potential advantages in selected medical situations. Unlike other electrosurgical devices,[29] RFA allows very specific treatment targeting of the desired tissue with a precise line of demarcation that avoids collateral damage, which is crucial in the head and neck region due to its high density of major nerves and blood vessels. RFA also does not require high temperatures. However, overheating from misapplication of RFA can cause harmful effects such as coagulation on the surface of the electrode, boiling within tissue that can leave "a gaping hole", tears, or even charring.[30]
Pain management
Back
RFA, or rhizotomy, was developed by Nikolai Bogduk to treat chronic pain arising from the facet joints in the lower (lumbar) back. Radiofrequency waves are used to produce heat on specifically identified nerves surrounding the facet joints called the lumbar medial branches of the dorsal ramus of the spinal nerves.[31] By generating heat around the nerve, the nerve is ablated, thus destroying its ability to transmit signals to the brain.
The nerves to be ablated are identified through injections of local anesthesia (such as lidocaine) around the medial branches prior to the RFA procedure to first confirm the diagnosis. If the local anesthesia injections provide temporary pain relief, the injection is repeated a second time to confirm the diagnosis. Then RFA is performed on the nerve(s) that responded well to the injections.
RFA is a minimally invasive procedure which can usually be done in day-surgery clinics, going home shortly after completion of the procedure. The person is awake during the procedure, so risks associated with general anesthesia are avoided. Whether for back or knee pain, a drawback for this procedure is that nerves recover function over time, so the pain relief achieved lasts only temporarily (3–15 months) in most people.[9]
Knees
Radiofrequency ablation of sensory nerves in the knee, also called genicular neurotomy or genicular RFA, is clinically preceded by confirming pain reduction upon anesthetizing the main knee sensory nerves in a test procedure called genicular nerve block.[3][32][33] Genicular nerve block is a short (10-30 minutes), outpatient procedure usually performed weeks before genicular RFA.[3][34][35] The extent of pain reduction by injecting a local anesthetic, such as bupivacaine, at specific locations of the target genicular nerves, is self-assessed by the person for hours after the procedure, leading to confirmation with the physician of the need for RFA.[3][35]
In the procedure for genicular RFA, a guide cannula is first directed under local anesthesia and imaging (ultrasound or fluoroscopy) to each target genicular nerve, then the radiofrequency electrode is passed through the cannula, and the electrode tip is heated to about 80 °C (176 °F) for one minute to cauterize a small segment of the nerve.[3][32] The heat destroys that segment of the nerve, which is prevented from sending pain signals to the brain.[3][32]
As of 2019, several hundred publications showed promise for substantial, long-term (6 months or longer) reduction of knee pain following genicular RFA.[3][36]
The US Food and Drug Administration had approved in 2017 a commercial device using cooled RFA, with effects lasting for up to a year of pain relief from knee arthritis.[9][37] As of 2023, reviews of clinical outcomes indicated that efficacy for reducing knee pain was achieved by ablating three or more branches of the genicular nerve (one of the articular branches of the tibial nerve).[34][36][38][39] Other sources indicate 4-5 genicular nerve targets may be justified for ablation to optimize pain relief,[33][34] while a 2022 analysis indicated that as many as 10 genicular nerve targets for RFA would produce better long-term relief of knee pain.[40]
Knee pain relief of 50% or more following genicular RFA may last from several months to two years,[3][38][39] and can be repeated by the same outpatient procedure when pain recurs.[3]
An anatomical study of cadaver knees indicated that ultrasound-guided bony landmarks could be used to effectively target the superior medial geniculate nerve, superior lateral geniculate nerve, and inferior medial geniculate nerve – the three nerves commonly targeted for knee RFA[3] – with average nerve-to-needle distances of 1.7, 3.2, and 1.8 mm, respectively.[41]
Barrett's esophagus
Radiofrequency ablation has been shown to be a safe and effective treatment for Barrett's esophagus. The balloon-based radiofrequency procedure was invented by Robert A. Ganz, Roger Stern and Brian Zelickson in 1999 (System and Method for Treating Abnormal Tissue in the Human Esophagus). While the person is sedated, a catheter is inserted into the esophagus and radiofrequency energy is delivered to the diseased tissue. This outpatient procedure typically lasts from fifteen to thirty minutes. Two months after the procedure, the physician performs an upper endoscopic examination to assess the esophagus for residual Barrett's esophagus. If any Barrett's esophagus is found, the disease can be treated with a focal RFA device. Between 80 and 90% or greater of people in numerous clinical trials have shown complete eradication of Barrett's esophagus in approximately two to three treatments with a favorable safety profile. The treatment of Barrett's esophagus by RFA is durable for up to 5 years.[42][43][44][45][46]
Thyroid nodules
Radiofrequency ablation has been used successfully on benign thyroid nodules for decades, most notably in Europe, South America and Korea.[citation needed] In the United States, the FDA approved the use of RFA techniques for thyroid nodules in 2018. Since then, professional guidelines reflect its use as a viable treatment modality for thyroid nodules, and the procedure is increasingly applied.[citation needed]
Timeline in the United States
- 2023: the American Thyroid Association issued the position statement "Thyroid ablative procedures provide valid alternative treatment strategies to conventional surgical management for a subset of patients with symptomatic benign thyroid nodules.[47]
- 2022: the American Association of Clinical Endocrinologists published an update in Endocrine Practice, stating that the "new image-guided minimally invasive approaches appear safe and effective alternatives when used appropriately and by trained professionals to treat symptomatic or enlarging thyroid masses".[48]
- 2018: FDA approved the RFA procedure for treatment of benign thyroid nodules.[citation needed]
Procedure
The procedure is similar to a thyroid biopsy, although instead of using a needle to remove cells from the nodule, a probe delivers heat to the interior of the nodule that effectively cauterizes the tissue. Over the course of 3-6 months, the nodule will continue to shrink, typically achieving a 50-80% reduction total size.
In order to qualify for an RFA procedure, a person must have a clearly benign thyroid nodule, usually proven by two fine needle aspiration biopsies.
As of 2020, RFA is not recommended for the treatment of malignant thyroid nodules, although research into this topic is ongoing.[49]
Other uses
RFA is used to treat uterine fibroids using the heat energy of radio frequency waves to ablate the fibroid tissue. The Acessa device[50] obtained FDA approval in 2012.[51] The device is inserted via a laparoscopic probe and guided inside the fibroid tissue using an ultrasound probe. The heat shrinks the fibroids. Clinical data on the procedure show an average of 45% shrinkage.
RFA is also used in the treatment of Morton's neuroma[52] where the outcome appears to be more reliable than alcohol injections.[53]
See also
References
- ↑ "Fulguration: NCI Dictionary of Cancer Terms" (in en). National Cancer Institute. 2011-02-02. https://www.cancer.gov/publications/dictionaries/cancer-terms/def/fulguration.
- ↑ Courtney M. Townsend (2012). Sabiston textbook of surgery : the biological basis of modern surgical practice (19th ed.). Philadelphia, PA: Elsevier Saunders. p. 236. ISBN 978-1-4377-1560-6.
- ↑ 3.00 3.01 3.02 3.03 3.04 3.05 3.06 3.07 3.08 3.09 3.10 3.11 3.12 3.13 "Genicular Nerve Radiofrequency Ablation for Painful Knee Arthritis: The Why and the How". JBJS Essential Surgical Techniques 9 (1): e10. March 2019. doi:10.2106/JBJS.ST.18.00016. PMID 31333900.
- ↑ "Radiofrequency neurotomy". Mayo Clinic. 6 April 2024. https://www.mayoclinic.org/tests-procedures/radiofrequency-neurotomy/about/pac-20394931.
- ↑ 5.0 5.1 "Radiofrequency Ablation for Pain Management". Cleveland Clinic. 14 March 2022. https://my.clevelandclinic.org/health/treatments/17411-radiofrequency-ablation.
- ↑ Hussain, Iram; Zulfiqar, Fizza; Li, Xilong; Ahmad, Shahzad; Aljammal, Jules (2021-08-01). "Safety and Efficacy of Radiofrequency Ablation of Thyroid Nodules-Expanding Treatment Options in the United States". Journal of the Endocrine Society 5 (8): bvab110. doi:10.1210/jendso/bvab110. ISSN 2472-1972. PMID 34258495.
- ↑ "Ablation for Arrhythmias". American Heart Association. 2017. http://www.heart.org/HEARTORG/Conditions/Arrhythmia/PreventionTreatmentofArrhythmia/Ablation-for-Arrhythmias_UCM_301991_Article.jsp.
- ↑ "Radiofrequency ablation for cancer". Mayo Clinic. 2017. http://www.mayoclinic.org/radiofrequency-ablation.
- ↑ 9.0 9.1 9.2 "'Cool' New Knee Procedure Eases Arthritis Pain Without Surgery". NBC News, New York. 13 June 2017. https://www.nbcnews.com/health/health-news/cool-new-knee-procedure-eases-arthritis-pain-without-surgery-n771221.
- ↑ "Long-term results of radiofrequency ablation treatment of stage I non-small cell lung cancer: a prospective intention-to-treat study". J Thorac Oncol 6 (12): 2044–51. 2011. doi:10.1097/JTO.0b013e31822d538d. PMID 22052222.
- ↑ "NHS, June 2008 – Radiofrequency ablation for lung cancer". http://www.nhs.uk/news/2008/06June/Pages/Radiofrequencyablationforlungcancer.aspx.
- ↑ Daily Telegraph – June 2008 – Lung cancer radiation treatment offers new hope
- ↑ Hadjicostas, P.; Malakounides, N.; Varianos, C.; Kitiris, E.; Lerni, F.; Symeonides, P. (2006). "Radiofrequency ablation in pancreatic cancer". HPB 8 (1): 61–64. doi:10.1080/13651820500466673. PMID 18333241.
- ↑ Rosenthal, D I; Alexander, A; Rosenberg, A E; Springfield, D (1992-04-01). "Ablation of osteoid osteomas with a percutaneously placed electrode: a new procedure.". Radiology 183 (1): 29–33. doi:10.1148/radiology.183.1.1549690. ISSN 0033-8419. PMID 1549690.
- ↑ Weber, Marc-André; Sprengel, Simon David; Omlor, Georg W.; Lehner, Burkhard; Wiedenhöfer, Bernd; Kauczor, Hans-Ulrich; Rehnitz, Christoph (2015-04-25). "Clinical long-term outcome, technical success, and cost analysis of radiofrequency ablation for the treatment of osteoblastomas and spinal osteoid osteomas in comparison to open surgical resection" (in en). Skeletal Radiology 44 (7): 981–93. doi:10.1007/s00256-015-2139-z. ISSN 0364-2348. PMID 25910709.
- ↑ Rosenthal, Daniel I.; Hornicek, Francis J.; Torriani, Martin; Gebhardt, Mark C.; Mankin, Henry J. (2003-10-01). "Osteoid Osteoma: Percutaneous Treatment with Radiofrequency Energy". Radiology 229 (1): 171–75. doi:10.1148/radiol.2291021053. ISSN 0033-8419. PMID 12944597.
- ↑ Rimondi, Eugenio; Mavrogenis, Andreas F.; Rossi, Giuseppe; Ciminari, Rosanna; Malaguti, Cristina; Tranfaglia, Cristina; Vanel, Daniel; Ruggieri, Pietro (2011-08-14). "Radiofrequency ablation for non-spinal osteoid osteomas in 557 patients" (in en). European Radiology 22 (1): 181–88. doi:10.1007/s00330-011-2240-1. ISSN 0938-7994. PMID 21842430.
- ↑ Rosenthal, Daniel I.; Hornicek, Francis J.; Wolfe, Michael W.; Jennings, L. Candace; Gebhardt, Mark C.; Mankin, Henry J. (1998-06-01). "Percutaneous Radiofrequency Coagulation of Osteoid Osteoma Compared with Operative Treatment*" (in en). J Bone Joint Surg Am 80 (6): 815–21. doi:10.2106/00004623-199806000-00005. ISSN 0021-9355. PMID 9655099. http://jbjs.org/content/80/6/815. Retrieved 2016-08-07.
- ↑ Dupuy, Damian E.; Liu, Dawei; Hartfeil, Donna; Hanna, Lucy; Blume, Jeffrey D.; Ahrar, Kamran; Lopez, Robert; Safran, Howard et al. (2010-02-15). "Percutaneous radiofrequency ablation of painful osseous metastases" (in en). Cancer 116 (4): 989–97. doi:10.1002/cncr.24837. ISSN 1097-0142. PMID 20041484.
- ↑ 20.0 20.1 "Use of Bipolar Radiofrequency Catheter Ablation in the Treatment of Cardiac Arrhythmias". Current Cardiology Reviews 14 (3): 185–191. 2018. doi:10.2174/1573403X14666180524100608. PMID 29792146.
- ↑ "Minimally Invasive Epicardial Surgical Ablation Alone Versus Hybrid Ablation for Atrial Fibrillation: A Systematic Review and Meta-Analysis". Arrhythmia & Electrophysiology Review 6 (4): 202–209. 2017. doi:10.15420/aer/2017.29.2. PMID 29326836.
- ↑ "Cryoablation Versus Radiofrequency Energy for the Ablation of Atrioventricular Nodal Reentrant Tachycardia (the CYRANO Study) : Results From a Large Multicenter Prospective Randomized Trial". Circulation 122 (22): 2239–45. 2010. doi:10.1161/circulationaha.110.970350. PMID 21098435.
- ↑ "A Controlled Trial of Renal Denervation for Resistant Hypertension (SYMPLICITY HTN-3 Trial)". N Engl J Med 370 (15): 1393–401. 2014. doi:10.1056/NEJMoa1402670. PMID 24678939.
- ↑ "Skin resurfacing procedures: new and emerging options". Clin Cosmet Investig Dermatol 7: 231–41. 2014. doi:10.2147/CCID.S50367. PMID 25210469.
- ↑ Endovenous ablation of perforator veins
- ↑ "Radiofrequency ablation as first-line treatment of varicose veins". Am Surg 80 (3): 231–35. 2014. doi:10.1177/000313481408000316. PMID 24666862.
- ↑ 27.0 27.1 "Submucosal Ablation of the Tongue Base for OSAS". American Academy of Otolaryngology – Head and Neck Surgery. http://www.entnet.org/Practice/Submucosal-ablation-of-the-tongue-base-for-OSAS.cfm.
- ↑ Qaseem, A; Holty, JE; Owens, DK; Dallas, P; Starkey, M; Shekelle, P; for the Clinical Guidelines Committee of the American College of, Physicians (Sep 24, 2013). "Management of Obstructive Sleep Apnea in Adults: A Clinical Practice Guideline From the American College of Physicians". Annals of Internal Medicine 159 (7): 471–83. doi:10.7326/0003-4819-159-7-201310010-00704. PMID 24061345.
- ↑ Bashetty, Kusum; Gururaj Nadig Sandhya Kapoor (19 November 2009). "Electrosurgery in aesthetic and restorative dentistry: A literature review and case reports". Journal of Conservative Dentistry 12 (4): 139–44. doi:10.4103/0972-0707.58332. PMID 20543922.
- ↑ Eick, Olaf J (1 July 2002). "Temperature Controlled Radiofrequency Ablation". Indian Pacing Electrophysiol. 3 2 (3): 66–73. PMID 17006561.
- ↑ Russo, Marc; Santarelli, Danielle; Wright, Robert; Gilligan, Chris (2021). "A History of the Development of Radiofrequency Neurotomy". Journal of Pain Research 14: 3897–3907. doi:10.2147/JPR.S334862. ISSN 1178-7090. PMID 34992451.
- ↑ 32.0 32.1 32.2 "Radiofrequency ablation for pain management". Cleveland Clinic. 14 March 2022. https://my.clevelandclinic.org/health/treatments/17411-radiofrequency-ablation.
- ↑ 33.0 33.1 "Genicular Nerve Ablation Review Using Cooled-Radiofrequency Nerve Ablation". Seminars in Interventional Radiology 39 (2): 130–137. April 2022. doi:10.1055/s-0042-1745797. PMID 35781999.
- ↑ 34.0 34.1 34.2 "Genicular Nerve Radiofrequency Ablation for the Treatment of Painful Knee Osteoarthritis: Current Evidence and Future Directions". Pain Medicine 22 (Suppl 1): S20–S23. July 2021. doi:10.1093/pm/pnab129. PMID 34308957. https://academic.oup.com/painmedicine/article/22/Supplement_1/S20/6328220.
- ↑ 35.0 35.1 "Genicular nerve block". Cleveland Clinic. 17 March 2023. https://my.clevelandclinic.org/health/treatments/24823-genicular-nerve-block.
- ↑ 36.0 36.1 "Indications of the Neurotomy of Genicular Nerves by Radiofrequency for the Treatment of Knee Osteoarthritis: A Literature Review". Revista Brasileira De Ortopedia 54 (3): 233–240. May 2019. doi:10.1055/s-0039-1692121. PMID 31363275.
- ↑ "FDA Green Lights Halyard Health's Coolief for the Management of Osteoarthritis Knee Pain". FDA News. 21 April 2017. http://www.fdanews.com/articles/181449-fda-green-lights-halyard-healths-coolief-for-the-management-of-osteoarthritis-knee-pain.
- ↑ 38.0 38.1 Tran, Andrew; Gonzalez, Felix M. (2023). "Review of cooled radiofrequency ablation utilization for the treatment of symptomatic advanced knee arthritis and total knee arthroplasty". Skeletal Radiology 52 (5): 941–949. doi:10.1007/s00256-022-04058-w. PMID 35462577. https://link.springer.com/article/10.1007/s00256-022-04058-w.
- ↑ 39.0 39.1 Gupta, A; Huettner, D. P; Dukewich, M (2017). "Comparative Effectiveness Review of Cooled Versus Pulsed Radiofrequency Ablation for the Treatment of Knee Osteoarthritis: A Systematic Review". Pain Physician 20 (3): 155–171. doi:10.36076/ppj.2017.171. PMID 28339430. http://www.painphysicianjournal.com/current/pdf?article=NDMwNA%3D%3D&journal=104.
- ↑ "How I Do It: Genicular Nerve Radiofrequency Ablation". ASRA Pain Medicine News, #47. 2022. doi:10.52211/asra020122.006. https://www.asra.com/news-publications/asra-newsletter/newsletter-item/asra-news/2022/02/07/how-i-do-it-genicular-nerve-radiofrequency-ablation.
- ↑ "Can ultrasound-guided radiofrequency ablation of genicular nerves of the knee, be performed without locating corresponding arterial pulsations – a cadaveric study". BMC Musculoskeletal Disorders 24 (1): 654. August 2023. doi:10.1186/s12891-023-06761-8. PMID 37587439.
- ↑ "Complete Ablation of Esophageal Epithelium Using a Balloon-based Bipolar Electrode". Gastrointestinal Endoscopy 60 (6): 1002–10. 2004. doi:10.1016/s0016-5107(04)02220-5. PMID 15605025.
- ↑ "Endoscopic radiofrequency ablation for Barrett's esophagus: 5-year outcomes from a prospective multicenter trial". Endoscopy 42 (10): 781–89. 2010. doi:10.1055/s-0030-1255779. PMID 20857372.
- ↑ "Radiofrequency Ablation in Barrett's Esophagus with Dysplasia". New England Journal of Medicine 360 (22): 2277–88. 2009. doi:10.1056/NEJMoa0808145. PMID 19474425.
- ↑ "Durability of Ablation in Barrett's Esophagus with Dysplasia". Gastroenterology 141 (2): 460–68. 2011. doi:10.1053/j.gastro.2011.04.061. PMID 21679712.
- ↑ "Stepwise radical endoscopic resection versus radiofrequency ablation for Barrett's oesophagus with high grade dysplasia or early cancer: a multicentre randomised trial". Gut 60 (6): 765–73. June 2011. doi:10.1136/gut.2010.229310. PMID 21209124.
- ↑ "General Principles for the Safe Performance, Training, and Adoption of Ablation Techniques for Benign Thyroid Nodules: An American Thyroid Association Statement". Thyroid 33 (10): 1150–1170. October 2023. doi:10.1089/thy.2023.0281. PMID 37642289.
- ↑ "American Association of Clinical Endocrinology Disease State Clinical Review: The Clinical Utility of Minimally Invasive Interventional Procedures in the Management of Benign and Malignant Thyroid Lesions". Endocrine Practice 28 (4): 433–448. April 2022. doi:10.1016/j.eprac.2022.02.011. PMID 35396078.
- ↑ "Radiofrequency Ablation of Papillary Thyroid Microcarcinomas". AACE Clinical Case Reports 8 (2): 99–101. 2022. doi:10.1016/j.aace.2022.02.005. PMID 35415224.
- ↑ "Acessa Health Procedure". https://acessaprocedure.com/.
- ↑ King, Paula (10 December 2012). "Brentwood medical company obtains FDA approval for new medical device". San Jose, CA: The Mercury News, Digital First Media. http://www.mercurynews.com/top-stories/ci_22162361/brentwood-medical-company-obtains-fda-approval-new-medical.
- ↑ "Ultrasound-guided radiofrequency ablation in the management of interdigital (Morton's) neuroma". Skeletal Radiol 42 (1): 107–11. Jan 2013. doi:10.1007/s00256-012-1527-x. PMID 23073898.
- ↑ "Alcohol injection for Morton's neuroma: a five-year follow-up". Foot Ankle Int 34 (8): 1064–67. 2013. doi:10.1177/1071100713489555. PMID 23669161.
es:Ablación (Medicina)#Ablación por radiofrecuencia
 |
