Medicine:Vitamin D toxicity
| Vitamin D toxicity | |
|---|---|
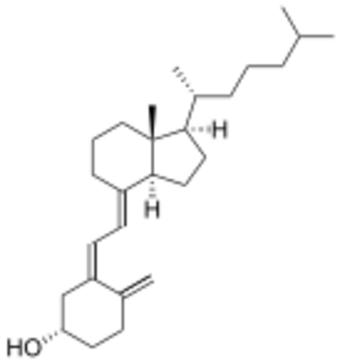 | |
| Cholecalciferol (shown above) and ergocalciferol are the two major forms of Vitamin D. | |
| Specialty | Endocrinology, toxicology |
Vitamin D toxicity, or hypervitaminosis D is the toxic state of an excess of vitamin D. The normal range for blood concentration in adults is 20 to 50 nanograms per milliliter (ng/mL).
Signs and symptoms
An excess of vitamin D causes abnormally high blood concentrations of calcium, which can cause overcalcification of the bones, soft tissues, heart and kidneys. In addition, hypertension can result.[1] Symptoms of vitamin D toxicity may include the following:
- Dehydration
- Vomiting
- Diarrhea
- Decreased appetite
- Irritability
- Constipation
- Fatigue
- Muscle weakness
- Metastatic calcification of the soft tissues
- Insomnia
Symptoms of vitamin D toxicity appear several months after excessive doses of vitamin D are administered. In almost every case, a low-calcium diet combined with corticosteroid drugs will allow for a full recovery within a month. It is possible that some of the symptoms of vitamin D toxicity are actually due to vitamin K depletion. One animal experiment has demonstrated that co-consumption with vitamin K reduced adverse effects, but this has not been tested in humans.[2] However the interconnected relationships between vitamin A, vitamin D, and vitamin K, outlined in a 2007 paper[3] published in the journal Medical Hypotheses, describes potential feedback loops between these three vitamins that could be elucidated by future research.
A mutation of the CYP24A1 gene can lead to a reduction in the degradation of vitamin D and to hypercalcemia (see Vitamin D: Excess).
Recommended supplement limits
The U.S National Academy of Medicine has established a Tolerable Upper Intake Level (UL) to protect against vitamin D toxicity ("The UL is not intended as a target intake; rather, the risk for harm begins to increase once intakes surpass this level.").[4] These levels in microgram (mcg or µg) and International Units (IU) for both males and females, by age, are:
(Conversion : 1 µg = 40 IU and 0.025 µg = 1 IU.[5])
- 0–6 months: 25 µg/d (1000 IU/d)
- 7–12 months: 38 µg/d (1500 IU/d)
- 1–3 years: 63 µg/d (2500 IU/d)
- 4–8 years: 75 µg/d (3000 IU/d)
- 9+ years: 100 µg/d (4000 IU/d)
- Pregnant and lactating: 100 µg/d (4000 IU/d)
The recommended dietary allowance is 15 µg/d (600 IU per day; 800 IU for those over 70 years). Overdose has been observed at 1,925 µg/d (77,000 IU per day).[citation needed] Acute overdose requires between 15,000 µg/d (600,000 IU per day) and 42,000 µg/d (1,680,000 IU per day) over a period of several days to months.
Suggested tolerable upper intake level
Based on risk assessment, a safe upper intake level of 250 µg (10,000 IU) per day in healthy adults has been suggested by non-government authors.[6][7] Blood levels of 25-hydroxyvitamin D necessary to cause adverse effects in adults are thought to be greater than about 150 ng/mL, leading the Endocrine Society to suggest an upper limit for safety of 100 ng/mL.[8]
Long-term effects of supplementary oral intake
Excessive exposure to sunlight poses no risk in vitamin D toxicity through overproduction of vitamin D precursor, cholecalciferol, regulating vitamin D production. During ultraviolet exposure, the concentration of vitamin D precursors produced in the skin reaches an equilibrium, and any further vitamin D that is produced is degraded.[9] This process is less efficient with increased melanin pigmentation in the skin. Endogenous production with full body exposure to sunlight is comparable to taking an oral dose between 250 µg and 625 µg (10,000 IU and 25,000 IU) per day.[9][10]
Vitamin D oral supplementation and skin synthesis have a different effect on the transport form of vitamin D, plasma calcifediol concentrations. Endogenously synthesized vitamin D3 travels mainly with vitamin D-binding protein (DBP), which slows hepatic delivery of vitamin D and the availability in the plasma.[11] In contrast, orally administered vitamin D produces rapid hepatic delivery of vitamin D and increases plasma calcifediol.[11]
It has been questioned whether to ascribe a state of sub-optimal vitamin D status when the annual variation in ultraviolet will naturally produce a period of falling levels, and such a seasonal decline has been a part of Europeans' adaptive environment for 1000 generations.[12][13] Still more contentious is recommending supplementation when those supposedly in need of it are labeled healthy and serious doubts exist as to the long-term effect of attaining and maintaining serum 25(OH)D of at least 80 nmol/L by supplementation.[14]
Current theories of the mechanism behind vitamin D toxicity (starting at a plasmatic concentration of ≈750 nmol/L[15]) propose that:
- Intake of vitamin D raises calcitriol concentrations in the plasma and cell
- Intake of vitamin D raises plasma calcifediol concentrations which exceed the binding capacity of the DBP, and free calcifediol enters the cell
- Intake of vitamin D raises the concentration of vitamin D metabolites which exceed DBP binding capacity and free calcitriol enters the cell
All of these affect gene transcription and overwhelm the vitamin D signal transduction process, leading to vitamin D toxicity.[15]
Cardiovascular disease
Evidence suggests that dietary vitamin D may be carried by lipoprotein particles into cells of the artery wall and atherosclerotic plaque, where it may be converted to active form by monocyte-macrophages.[11][16][17] This raises questions regarding the effects of vitamin D intake on atherosclerotic calcification and cardiovascular risk as it may be causing vascular calcification.[18] Calcifediol is implicated in the etiology of atherosclerosis, especially in non-Whites.[19][20]
The levels of the active form of vitamin D, calcitriol, are inversely correlated with coronary calcification.[21] Moreover, the active vitamin D analog, alfacalcidol, seems to protect patients from developing vascular calcification.[22][23] Serum vitamin D has been found to correlate with calcified atherosclerotic plaque in African Americans as they have higher active serum vitamin D levels compared to Euro-Americans.[20][24][25][26] Higher levels of calcidiol positively correlate with aorta and carotid calcified atherosclerotic plaque in African Americans but not with coronary plaque, whereas individuals of European descent have an opposite, negative association.[20] There are racial differences in the association of coronary calcified plaque in that there is less calcified atherosclerotic plaque in the coronary arteries of African-Americans than in whites.[27]
Among descent groups with heavy sun exposure during their evolution, taking supplemental vitamin D to attain the 25(OH)D level associated with optimal health in studies done with mainly European populations may have deleterious outcomes.[14] Despite abundant sunshine in India, vitamin D status in Indians is low and suggests a public health need to fortify Indian foods with vitamin D. However, the levels found in India are consistent with many other studies of tropical populations which have found that even an extreme amount of sun exposure, does not raise 25(OH)D levels to the levels typically found in Europeans.[28][29][30][31]
Recommendations stemming for a single standard for optimal serum 25(OH)D concentrations ignores the differing genetically mediated determinates of serum 25(OH)D and may result in ethnic minorities in Western countries having the results of studies done with subjects not representative of ethnic diversity applied to them. Vitamin D levels vary for genetically mediated reasons as well as environmental ones.[32][33][34][35]
Ethnic differences
Possible ethnic differences in physiological pathways for ingested vitamin D, such as the Inuit, may confound across the board recommendations for vitamin D levels. Inuit compensate for lower production of vitamin D by converting more of this vitamin to its most active form.[36]
A Toronto study of young Canadians of diverse ancestry applied a standard of serum 25(OH)D levels that was significantly higher than official recommendations.[37][38] These levels were described to be 75 nmol/L as "optimal", between 75 nmol/L and 50 nmol/L as "insufficient" and <50 nmol/L as "deficient". 22% of individuals of European ancestry had 25(OH)D levels less than the 40 nmol/L cutoff, comparable to the values observed in previous studies (40 nmol/L is 15 ng/mL). 78% of individuals of East Asian ancestry and 77% of individuals of South Asian ancestry had 25(OH)D concentrations lower than 40 nmol/L. The East Asians in the Toronto sample had low 25(OH)D levels when compared to whites. In a Chinese population at particular risk for esophageal cancer and with the high serum 25(OH)D concentrations have a significantly increased risk of the precursor lesion.[39]
Studies on the South Asian population uniformly point to low 25(OH)D levels, despite abundant sunshine.[40] Rural men around Delhi average 44 nmol/L. Healthy Indians seem have low 25(OH)D levels which are not very different from healthy South Asians living in Canada. Measuring melanin content to assess skin pigmentation showed an inverse relationship with serum 25(OH)D.[37] The uniform occurrence of very low serum 25(OH)D in Indians living in India and Chinese in China does not support the hypothesis that the low levels seen in the more pigmented are due to lack of synthesis from the sun at higher latitudes.
Premature aging
Complex regulatory mechanisms control metabolism. Recent epidemiologic evidence suggests that there is a narrow range of vitamin D levels in which vascular function is optimized. Animal research suggests that both excess and deficiency of vitamin D appears to cause abnormal functioning and premature aging.[41][42][43][44]
Comparative Toxicity: Use of Vitamin D in Rodenticides
Vitamin D compounds, specifically cholecalciferol (D3) and ergocalciferol (D2), are used in rodenticides due to their ability to induce hypercalcemia, a condition characterized by elevated calcium levels in the blood. This overdose leads to organ failure and is pharmacologically similar to vitamin D's toxic effects in humans.
Concentrations used in these rodenticides are several orders of magnitude higher than the maximum recommended human intake, with acute baits containing 3,000,000 IU/g for D3 and 4,000,000 IU/g for D2. This leads to hypercalcemia in the rodents and subsequent death several days after ingestion.[45][46]
See also
References
- ↑ Vitamin D at Merck Manual of Diagnosis and Therapy Professional Edition
- ↑ "Comparison between the protective effects of vitamin K and vitamin A on the modulation of hypervitaminosis D3 short-term toxicity in adult albino rats". Turk J Med Sci 46 (2): 524–38. 2016. doi:10.3906/sag-1411-6. PMID 27511521.
- ↑ Masterjohn, C. (2007). "Vitamin D toxicity redefined: Vitamin K and the molecular mechanism". Medical Hypotheses 68 (5): 1026–34. doi:10.1016/j.mehy.2006.09.051. PMID 17145139. https://pubmed.ncbi.nlm.nih.gov/17145139/.
- ↑ Ross (2010). "The 2011 Report on Dietary Reference Intakes for Calcium and Vitamin D from the Institute of Medicine: What Clinicians Need to Know". J Clin Endocrinol Metab 96 (1): 53–58. doi:10.1210/jc.2010-2704. PMID 21118827.
- ↑ "Dietary Reference Intakes Tables [Health Canada, 2005"]. http://dietarysupplementdatabase.usda.nih.gov/ingredient_calculator/help.php#q9.
- ↑ "Risk assessment for vitamin D". The American Journal of Clinical Nutrition 85 (1): 6–18. January 2007. doi:10.1093/ajcn/85.1.6. PMID 17209171.
- ↑ "Vitamin D toxicity, policy, and science". Journal of Bone and Mineral Research 22 (Suppl 2): V64-8. December 2007. doi:10.1359/jbmr.07s221. PMID 18290725.
- ↑ "Evaluation, Treatment, and Prevention of Vitamin D Deficiency: an Endocrine Society Clinical Practice Guideline". J Clin Endocrinol Metab 96 (7): 1922. 2011. doi:10.1210/jc.2011-0385. PMID 21646368.
- ↑ 9.0 9.1 "Environmental factors that influence the cutaneous production of vitamin D". The American Journal of Clinical Nutrition 61 (3 Suppl): 638S–645S. March 1995. doi:10.1093/ajcn/61.3.638S. PMID 7879731. http://www.ajcn.org/cgi/pmidlookup?view=long&pmid=7879731.
- ↑ [Effects Of Vitamin D and the Natural selection of skin color:how much vitamin D nutrition are we talking about http://www.direct-ms.org/pdf/VitDVieth/Vieth%20Anthropology%20vit%20D.pdf][full citation needed]
- ↑ 11.0 11.1 11.2 "Human plasma transport of vitamin D after its endogenous synthesis". The Journal of Clinical Investigation 91 (6): 2552–5. June 1993. doi:10.1172/JCI116492. PMID 8390483.
- ↑ "Seasonal variance of 25-(OH) vitamin D in the general population of Estonia, a Northern European country". BMC Public Health 9: 22. January 2009. doi:10.1186/1471-2458-9-22. PMID 19152676.
- ↑ "Out of Africa: modern human origins special feature: the spread of modern humans in Europe". Proceedings of the National Academy of Sciences of the United States of America 106 (38): 16040–5. September 2009. doi:10.1073/pnas.0903446106. PMID 19571003. Bibcode: 2009PNAS..10616040H.
- ↑ 14.0 14.1 Tseng, Lisa (2003). "Controversies in Vitamin D Supplementation". Nutrition Bytes 9 (1). http://escholarship.org/uc/item/4m84d4fn.
- ↑ 15.0 15.1 "Pharmacokinetics of vitamin D toxicity". The American Journal of Clinical Nutrition 88 (2): 582S–586S. August 2008. doi:10.1093/ajcn/88.2.582s. PMID 18689406. http://www.ajcn.org/cgi/pmidlookup?view=long&pmid=18689406.
- ↑ "Vitamin D and osteogenic differentiation in the artery wall". Clinical Journal of the American Society of Nephrology 3 (5): 1542–7. September 2008. doi:10.2215/CJN.01220308. PMID 18562594.
- ↑ "Investigation of the potential association of vitamin D binding protein with lipoproteins". Annals of Clinical Biochemistry 47 (Pt 2): 143–50. March 2010. doi:10.1258/acb.2009.009018. PMID 20144976.
- ↑ "Vascular calcification: pathobiology of a multifaceted disease". Circulation 117 (22): 2938–48. June 2008. doi:10.1161/CIRCULATIONAHA.107.743161. PMID 18519861.
- ↑ "The physiological economy of vitamin D". Lancet 1 (8331): 969–72. April 1983. doi:10.1016/S0140-6736(83)92090-1. PMID 6132277.
- ↑ 20.0 20.1 20.2 "Vitamin d, adiposity, and calcified atherosclerotic plaque in african-americans". The Journal of Clinical Endocrinology and Metabolism 95 (3): 1076–83. March 2010. doi:10.1210/jc.2009-1797. PMID 20061416.
- ↑ "Active serum vitamin D levels are inversely correlated with coronary calcification". Circulation 96 (6): 1755–60. September 1997. doi:10.1161/01.cir.96.6.1755. PMID 9323058.
- ↑ "1alpha(OH)D3 One-alpha-hydroxy-cholecalciferol--an active vitamin D analog. Clinical studies on prophylaxis and treatment of secondary hyperparathyroidism in uremic patients on chronic dialysis". Danish Medical Bulletin 55 (4): 186–210. November 2008. PMID 19232159. http://www.danmedj.dk/dmb_2008/0408/0408-disputatser/dmb4040.htm.
- ↑ "Relation of oral 1alpha-hydroxy vitamin D3 to the progression of aortic arch calcification in hemodialysis patients". Heart and Vessels 25 (1): 1–6. January 2010. doi:10.1007/s00380-009-1151-4. PMID 20091391.
- ↑ "Evidence for alteration of the vitamin D-endocrine system in blacks". The Journal of Clinical Investigation 76 (2): 470–3. August 1985. doi:10.1172/JCI111995. PMID 3839801.
- ↑ "Vitamin D economy in blacks". Journal of Bone and Mineral Research 22 (Suppl 2): V34-8. December 2007. doi:10.1359/jbmr.07s220. PMID 18290719.
- ↑ "Racial/ethnic considerations in making recommendations for vitamin D for adult and elderly men and women". The American Journal of Clinical Nutrition 80 (6 Suppl): 1763S–6S. December 2004. doi:10.1093/ajcn/80.6.1763S. PMID 15585802. http://www.ajcn.org/cgi/pmidlookup?view=long&pmid=15585802.
- ↑ "Racial differences in the association of coronary calcified plaque with left ventricular hypertrophy: the National Heart, Lung, and Blood Institute Family Heart Study and Hypertension Genetic Epidemiology Network". The American Journal of Cardiology 97 (10): 1441–8. May 2006. doi:10.1016/j.amjcard.2005.11.076. PMID 16679080.
- ↑ "Presence of 25(OH) D deficiency in a rural North Indian village despite abundant sunshine". The Journal of the Association of Physicians of India 56: 755–7. October 2008. PMID 19263699.
- ↑ "Worldwide status of vitamin D nutrition". The Journal of Steroid Biochemistry and Molecular Biology 121 (1–2): 297–300. July 2010. doi:10.1016/j.jsbmb.2010.02.021. PMID 20197091.
- ↑ "Abundant sunshine and vitamin D deficiency". The British Journal of Nutrition 99 (6): 1171–3. June 2008. doi:10.1017/S0007114508898662. PMID 18234141.
- ↑ "Global vitamin D levels in relation to age, gender, skin pigmentation and latitude: an ecologic meta-regression analysis". Osteoporosis International 20 (1): 133–40. January 2009. doi:10.1007/s00198-008-0626-y. PMID 18458986.
- ↑ "Genetic and environmental determinants of 25-hydroxyvitamin D and 1,25-dihydroxyvitamin D levels in Hispanic and African Americans". The Journal of Clinical Endocrinology and Metabolism 93 (9): 3381–8. September 2008. doi:10.1210/jc.2007-2702. PMID 18593774.
- ↑ "DBP (vitamin D binding protein) and BF (properdin factor B) allele distribution in Namibian San and Khoi and in other South African populations". Gene Geography 9 (3): 185–9. December 1995. PMID 8740896.
- ↑ "Vitamin D status and nutrition in Europe and Asia". The Journal of Steroid Biochemistry and Molecular Biology 103 (3–5): 620–5. March 2007. doi:10.1016/j.jsbmb.2006.12.076. PMID 17287117.
- ↑ "Full-length characterization of proteins in human populations". Clinical Chemistry 56 (2): 202–11. February 2010. doi:10.1373/clinchem.2009.134858. PMID 19926773.
- ↑ "Vitamin D insufficiency in Greenlanders on a westernized fare: ethnic differences in calcitropic hormones between Greenlanders and Danes". Calcified Tissue International 74 (3): 255–63. March 2004. doi:10.1007/s00223-003-0110-9. PMID 14708040.
- ↑ 37.0 37.1 "Low wintertime vitamin D levels in a sample of healthy young adults of diverse ancestry living in the Toronto area: associations with vitamin D intake and skin pigmentation". BMC Public Health 8: 336. September 2008. doi:10.1186/1471-2458-8-336. PMID 18817578.
- ↑ Scientific Advisory Committee on Nutrition (2007) Update on Vitamin D Position Statement by the Scientific Advisory Committee on Nutrition 2007 ISBN:978-0-11-243114-5[page needed]
- ↑ "Serum 25(OH)-vitamin D concentration and risk of esophageal squamous dysplasia". Cancer Epidemiology, Biomarkers & Prevention 16 (9): 1889–93. September 2007. doi:10.1158/1055-9965.EPI-07-0461. PMID 17855710.
- ↑ "Vitamin D Status in India – Its Implications and Remedial Measures". https://citeseerx.ist.psu.edu/document?repid=rep1&type=pdf&doi=1d83883e2277545dcac936364dffc4a11a011178.
- ↑ "Vitamin D and aging". The Journal of Steroid Biochemistry and Molecular Biology 114 (1–2): 78–84. March 2009. doi:10.1016/j.jsbmb.2008.12.020. PMID 19444937.
- ↑ "Premature aging in vitamin D receptor mutant mice". The Journal of Steroid Biochemistry and Molecular Biology 115 (3–5): 91–7. July 2009. doi:10.1016/j.jsbmb.2009.03.007. PMID 19500727.
- ↑ "Vitamin D, nervous system and aging". Psychoneuroendocrinology 34 (Suppl 1): S278-86. December 2009. doi:10.1016/j.psyneuen.2009.07.003. PMID 19660871.
- ↑ "Vitamin D and aging: old concepts and new insights". The Journal of Nutritional Biochemistry 18 (12): 771–7. December 2007. doi:10.1016/j.jnutbio.2007.02.002. PMID 17531460.
- ↑ "CHOLECALCIFEROL: A UNIQUE TOXICANT FOR RODENT CONTROL". Proceedings of the Eleventh Vertebrate Pest Conference (1984). University of Nebraska Lincoln. March 1984. https://digitalcommons.unl.edu/vpc11/22/. "Cholecalciferol is an acute (single-feeding) and/or chronic (multiple-feeding) rodenticide toxicant with unique activity for controlling commensal rodents including anticoagulant-resistant rats. Cholecalciferol differs from conventional acute rodenticides in that no bait shyness is associated with consumption and time to death is delayed, with first dead rodents appearing 3-4 days after treatment."
- ↑ Rizor, Suzanne E.; Arjo, Wendy M.; Bulkin, Stephan; Nolte, Dale L.. "Efficacy of Cholecalciferol Baits for Pocket Gopher Control and Possible Effects on Non-Target Rodents in Pacific Northwest Forests". Vertebrate Pest Conference (2006). USDA. https://naldc.nal.usda.gov/download/39036/PDF. Retrieved August 27, 2019. "0.15% cholecalciferol bait appears to have application for pocket gopher control.' Cholecalciferol can be a single high-dose toxicant or a cumulative multiple low-dose toxicant."
External links
| Classification | |
|---|---|
| External resources |
 |

