Medicine:Amplified musculoskeletal pain syndrome
| Amplified musculoskeletal pain syndrome | |
|---|---|
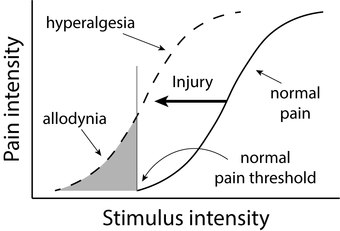 | |
| Image showing hyperalgesia and allodynia, two common symptoms of AMPS, compared to normal pain levels in response to stimuli. | |
| Specialty | Rheumatology, Pediatrics, Psychology |
| Symptoms | Chronic pain, allodynia, abdominal pain, anxiety, depression, dysphagia, dizziness, fatigue, headache, joint pain, movement issues, such as stiffness, shakiness, or coordination difficulty, swelling, fast heart rate, skin texture, color, or temperature changes, paresthesia, changes in nail or hair growth[1][2][3][4] |
| Complications | Major depressive disorder, anxiety, psychological stress, osteoporosis, muscle atrophy[1] |
| Usual onset | Childhood and adolescence.[1] Some evidence shows 14 years of age to be an average.[5] |
| Types | Complex regional pain syndrome, Diffuse idiopathic pain (Also known as juvenile fibromyalgia), Intermittent amplified pain, Localized amplified pain[1][2] |
| Causes | Psychological trauma, physical injury, illness[1][6] |
| Risk factors | Asthma, autoimmune diseases,[1] arthritis, myositis, Ehlers-Danlos syndrome, rheumatologic diseases, being female[3] |
| Diagnostic method | Full overview of patient history and out rule of potential physical causes[1][7] |
| Differential diagnosis | Myofascial pain syndrome, idiopathic chronic pain, degenerative disc disease, lordosis,[1] Greater trochanteric pain syndrome |
| Management | Aerobic exercise, message therapy to desensitize physical contact, occupational therapy, physical therapy, psychotherapy, medication (selective serotonin reuptake inhibitors),[8] procedures and injections |
| Medication | Selective serotonin reuptake inhibitors[8] |
| Prognosis | Good[citation needed] |
| Frequency | 2-6% of children have a mild case of AMPS.[6] |
Amplified musculoskeletal pain syndrome (AMPS) is an illness characterized by notable pain intensity without an identifiable physical cause.[1][6]
Characteristic symptoms include skin sensitivity to light touch, also known as allodynia. Associated symptoms may include changes associated with disuse including changes in skin texture, color, and temperature, and changes in hair and nail growth. In up to 80% of cases, symptoms are associated with psychological trauma or psychological stress.[3] AMPS may also follow physical injury or illness.[2] Other associations with AMPS include Ehlers-danlos syndrome, myositis, arthritis, and other rheumatologic diseases.[3] Due to the nature of the condition, AMPS is often not diagnosed when it first presents. AMPS is diagnosed through a review of a patient's medical history, as well as multiple tests to rule out the diagnosis of other conditions, such as bone fracture.[1]
AMPS is treated through various methods. As there is no cure for the condition, pain management and treatment of potential causes, such as psychological stress, are used. This can include psychotherapy, physical therapy, and other pain management treatments. The prognosis for the condition is very positive, with the ability for majority of effected individuals to recover completely, but the management of the condition is a gradual improvement over time, which can leave many individuals feeling a lack of motivation or progress in their AMPS management. Anyone can be affected with AMPS, though the most commonly affected individuals are children and adolescents, with up to 80% of affected individuals being women.[3][1]
Signs and symptoms
Amplified musculoskeletal pain syndrome is characterized by various symptoms. This includes chronic pain, allodynia, abdominal pain, dysphagia, dizziness, fatigue, headache, joint pain, movement issues, such as stiffness, shakiness, or coordination difficulty, swelling, fast heart rate, skin texture, color, or temperature changes, paresthesia, and changes in nail or hair growth are all common symptoms of AMPS.[1][2][3][6] These symptoms can also cause various other complications, which, while being mainly mental symptoms, still have a heavy impact on the effected individual. This can include anxiety, depression, psychological trauma, and psychological stress.[9][10]
Chronic pain
Chronic pain is one of the main symptoms of AMPS. The pain associated with the disorder can either be constant or intermittent. It is also distinguishable based on whether the pain is isolated to one region of the body, or is felt throughout the body. No matter the type of pain felt by AMPS, all kinds can be equally debilitating and have heavy impacts on the quality of life for the effected individual.
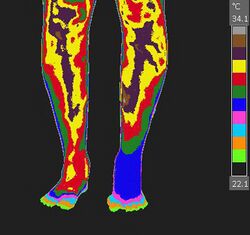
Visual changes
Because of the mechanics of AMPS, individuals with the condition can have visual changes to the affected area. This is mainly seen in complex regional pain syndrome. Visual changes in AMPS can include swelling; skin texture, color, and temperature changes; and changes in nail and hair growth.[3] Because these symptoms do not present in all forms or cases of AMPS, individuals effected with the condition often do not receive a diagnosis when the condition first presents, and often are given other diagnoses that are not accurate, such as a physiological cause.
Complications
Because of the mechanism of AMPS, the condition can often result in complications as the result of the presented symptoms. This can include various physical symptoms, including muscle atrophy and osteoporosis.[1] While physical conditions are possible as the result of AMPS, mental health conditions are very frequent, including anxiety, depression, psychological trauma, and psychological stress.
Causes
Various events can cause AMPS. The three main causes include psychological stress, physical injury, and illness.[1][2][3] Various other conditions can be risk factors or causes of the disease, including arthritis, myositis, Ehlers-Danlos syndrome, and autoimmune diseases, such as asthma.[1]
Psychological trauma
Psychological trauma is the main cause of AMPS. Evidence shows it is capable of causing up to 80% of reported AMPS cases.[3] This is often a target of the treatment of AMPS, which includes psychotherapy, occupational therapy, and is one of the reasons for which selective serotonin reuptake inhibitors are used as a management for the condition.[1]
Physical injury
Physical injury, such as a bone fracture or surgery, is the second most common cause, often resulting in complex regional pain syndrome, a type of AMPS that is isolated to one region of the body, such as a hand or foot.
Risk factors
Mechanism
While AMPS has little research dedicated to it,[6] evidence has showed a mutual cause of condition. The amplified pain is believed to be caused by pain signals sent to the brain, which are also incorrectly sent through the sympathetic nervous system, also known as the "fight or flight" nerves. This causes an involuntary response to pain, including vein constriction. This causes increased heart rate, increase in muscle tone, increased respiratory rate, and a reduce of blood flow to the muscles and bone, resulting in an increase in waste products, such as lactic acid.[1] This buildup of waste products, as well as depletion of oxygen, results in the amplified pain associated with AMPS.[7] This is only a common theory for the cause, and health care professionals and researchers do not have complete evidence of the cause of AMPS, largely do to the lack of research associated with the disorder and its lack of awareness in medicine.[1]
Classification
AMPS is classified into four different types, of which may be divided into multiple sub-types. This includes complex regional pain syndrome, diffuse idiopathic pain, intermittent amplified pain, and localized amplified pain.[1]
Complex regional pain syndrome
Complex regional pain syndrome is a term for any amount of spontaneous regional pain lasting longer than the expected recovery time of an observed physical trauma, or other injury. This includes two separate types: type I and type II. Type I CRPS, formerly known as reflex sympathetic dystrophy (RSD) or "Sudeck's atrophy", refers to CRPS without any observed nerve damage. Type II, formerly known as causalgia, refers to CRPS with observed nerve damage. This form, similarly to other forms of AMPS, is known to be able to spread from one limb to a new limb. 35% of people effected with CRPS report full-body impacts from the condition. Common symptoms of CRPS include musculoskeletal pain; swelling; changes to the skin texture, color, or temperature; and limited range of motion.[11]
Diffuse idiopathic pain
This type of AMPS includes full-body pain. It is also known as juvenile fibromyalgia.
Intermittent amplified pain
This type of AMPS refers to amplified pain that varies in intensity over time.
Localized amplified pain
This refers to localized amplified pain without other symptoms. This type cannot include symptoms such as swelling; skin texture, color, or temperature changes; or perspiration. Observation of these symptoms implies the diagnosis of complex regional pain syndrome.
Diagnosis
Because of the little awareness on AMPS, the condition is frequently not diagnosed when symptoms first present, often with multiple diagnoses of physical conditions before the diagnosis of AMPS.[3][12]
The condition is diagnosed through observation of various patient traits. A full overview of the patients medical history, as well as out rule of any potention physical causes, such as a bone fracture. If no physical causes are observed, a diagnosis of AMPS is likely possible.[3][12] Other common steps that are taken may include bone scans to detect possible signs of reduced blood flow; magnetic resonance imaging (MRI) to detect possible edema, or muscle atrophy; Nerve testing can be used to look for pain or sensitivity issues; and X-rays can detect osteoporosis as the result of AMPS.[1] While all of these tests can detect possible signs of AMPS, better outcomes are usually made with less tests, and immediate treatment of AMPS without looking for possible differential diagnoses.[3]
Management
As AMPS is not a disease, there is no one specific cure for it.[12] Management of the condition is a process of patients learning to manage the abnormal amplified pain. This can include a combination of treating the cause(s) of the condition, as well as managing the symptoms of the condition.
Medication
As psychological stress accounts for up to 80% of cases of AMPS, medication often involves typical antidepressants. These are also often prescribed for chronic pain do to the impact they have on serotonin and its impact on muscular pain and control.[8] Many providers also use an injectable medication for treatment of AMPS. Opioid use is not recommended for most AMPS cases, as it can worsen recovery, and in rare cases, make the condition worse.[1]
Physical therapy
Physical treatment of AMPS is very common and is shown to have long term benefit. This includes physical therapy, message therapy, and aerobic exercise. Physical therapy involves training the use of the affected limb or training the use of the body. This is for the purpose of retraining muscles after muscle atrophy, and retraining how to use the affected muscles with less amplified pain.
Message therapy is used to desensitize the affected area or body so it can build a tolerance to pain. This can help with symptoms such as allodynia and hyperalgesia in AMPS, as well as indirectly help with other common symptoms by relieving the patient of pain which could have been the cause of psychological stress, depression, anxiety, as well as a number of physiological conditions, including headaches.
Psychotherapy
Prognosis
See also
References
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 1.13 1.14 1.15 1.16 1.17 1.18 1.19 1.20 "Amplified Musculoskeletal Pain Syndrome in Children". Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/17933-amplified-musculoskeletal-pain-syndrome-amps-in-children.
- ↑ 2.0 2.1 2.2 2.3 2.4 "Amplified Musculoskeletal Pain Syndrome in Children". Johns Hopkins All Children's Hospital. https://www.hopkinsallchildrens.org/Services/Anesthesiology/Pain-Management/Chronic-Pain-Management/Amplified-Musculoskeletal-Pain-Syndrome-in-Childre.
- ↑ 3.00 3.01 3.02 3.03 3.04 3.05 3.06 3.07 3.08 3.09 3.10 3.11 "Amplified Musculoskeletal Pain Syndrome (AMPS)". Children's Health. https://www.childrens.com/specialties-services/conditions/amplified-musculoskeletal-pain-syndrome-amps.
- ↑ "Amplified Musculoskeletal Pain Syndrome (AMPS)". American College of Rheumatology. https://rheumatology.org/patients/amplified-musculoskeletal-pain-syndrome-amps.
- ↑ Monica L. Friedman, DO. "When Your Child Hurts: What Is Amplified Musculoskeletal Pain Syndrome?". Orlando Health. https://www.orlandohealth.com/content-hub/when-your-child-hurts-what-is-amplified-musculoskeletal-pain-syndrome.
- ↑ 6.0 6.1 6.2 6.3 6.4 "Expressing support for the designation of "National Amplified Musculoskeletal Pain Syndrome Awareness Day"". United States Congress. https://www.congress.gov/bill/116th-congress/house-resolution/588/text.
- ↑ 7.0 7.1 "Amplified Musculoskeletal Pain Syndrome". Hospital for Special Surgery. https://www.hss.edu/condition-list_amplified-musculoskeletal-pain-syndrome.asp#symptoms.
- ↑ 8.0 8.1 8.2 Pain Res Manag (2016). "SSRIs for Chronic Pain: What do we know?". Pain Research & Management (National Institutes of Health) 2016. doi:10.1155/2016/2020915. PMID 27445601.
- ↑ "Pain and Depression: Is there a link?". Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/depression/expert-answers/pain-and-depression/faq-20057823.
- ↑ "Chronic Pain and Anxiety Disorders". Anxiety and Depression Association of America. https://adaa.org/understanding-anxiety/related-illnesses/other-related-conditions/chronic-pain.
- ↑ "The natural history of complex regional pain syndrome". The Clinical Journal of Pain 25 (4): 273–280. May 2009. doi:10.1097/AJP.0b013e31818ecea5. PMID 19590474.
- ↑ 12.0 12.1 12.2 "Causes and Treatment for Pain Amplification Syndrome". Children's Hospital of Orange County. https://care.choc.org/causes-and-treatment-for-pain-amplification-syndrome.
 |