Chemistry:Silver diammine fluoride
| Clinical data | |
|---|---|
| Trade names | Fagamin, Advantage Arrest |
| Other names | Diammine Silver Fluoride, Diamine silver fluoride |
| ATC code |
|
| Legal status | |
| Legal status |
|
| Identifiers | |
| |
| CAS Number | |
| ChemSpider | |
| UNII | |
| Chemical and physical data | |
| Formula | AgFH6N2 |
| Molar mass | 160.929 g·mol−1 |
| 3D model (JSmol) | |
| |
| |
Silver diammine fluoride (SDF), also known as silver diamine fluoride in most of the dental literature, (although this is a chemical misnomer) is a topical medication used to treat and prevent dental caries (tooth decay) and relieve dentinal hypersensitivity.[1] It is a colorless (most products) or blue-tinted (Advantage Arrest), odourless liquid composed of silver, ammonium and fluoride ions at a pH of 10.4 (most products) or 13 (Riva Star).[2] Ammonia compounds reduce the oxidative potential of SDF, increase its stability and helps to maintain a constant concentration over a period of time, rendering it safe for use in the mouth.[3] Silver and fluoride ions possess antimicrobial properties[1] and are used in the remineralization of enamel and dentin on teeth for preventing and arresting dental caries.[4][5]
SDF is also known as diammine silver fluoride, silver fluoride, and silver ammonium fluoride. It is frequently spelled "silver diamine fluoride" (with one m); however, this is a misnomer, as SDF contains two ammine (NH3) groups, not amine (NH2) groups.[6]
Based on the current, best available evidence, SDF can be used by licensed dental professionals. In the United Kingdom , this is classified as 'off-label' [7] use of a topical medicament for arresting caries as it is licensed for treatment of dentine hypersensitivity.[1] It is supported by a robust, extensive evidence base[8][9][10][11] with regard to its efficacy and can be used as long as the following criteria are realised: there is a body of evidence supporting its efficacy; and there is no alternative, licensed medicine.[12]
The product was cleared for sale by the U.S. Food and Drug Administration as a Class II medical device for the treatment of dentinal hypersensitivity,[13] and has been classified as an ‘effective, efficient, equitable and safe caries-preventative agent’ by the Institute of Medicine and the Millennium Goals of the World Health Organization in 2009.[1]
It is on the World Health Organization's List of Essential Medicines.[14]
Brand names
- Argentina: 38% SDF solution, Fluoroplat, TEDEQUIM Laboratories, Córdoba, Argentina. 38% SDF Solution, FAgamin, Bv. de los Poles 6136, Córdoba, Argentina.
- Japan: 38% SDF solution, Saforide, Toyo Seiyaku Kasei Co. Ltd., Osaka, Japan.
- Thailand: 38% SDF solution: Topamine, PharmaDesign Thailand/Dentalife Australia, e-SDF (Caliham Group)
- USA: 38% SDF solution, Advantage Arrest, Elevate Oral Care LLC, West Palm Beach, Florida, USA.
- India: 38% SDF solution, e-SDF (Kids-e-dental LLP, India)
- Australia: 38% SDF solution, Riva Star, unit doses, SDI, TOPAMINE (Dentalife Australia)
- (there are 30%, 12%, and 10% SDF's available from Argentina and Brazil. CarieStop and others.)
Indications and Contraindications of SDF
Indications
SDF use is indicated in the clinical scenarios listed below.
Patients
- With severe caries risk due to xerostomia (dry mouth from reduced salivary flow);[15]
- Severe early childhood caries, which does not typically resolve with operative treatment.[15][16]
- Babies and toddlers with Early Childhood Caries;[15][17]
- Pre-cooperative children, to slow down the progress of the disease prior to building cooperation for treatment;[15]
- Patients with physical or cognitive disabilities or dental phobia for whom more invasive procedures are not appropriate;[15]
- Where aerosol generating procedures (AGPs) are unable to be performed or approved;
- With no or limited access to dental centres owing to its ease of use and minimal equipment requirement.[15]
Teeth
- Carious primary teeth showing radiographic evidence of being close to exfoliation;
- Non-restorable asymptomatic teeth where extraction is contra-indicated;[17]
- With symptomatic Molar-Incisal Hypomineralization (MIH) to ease dentin hypersensitivity and slow down disease progress;[18]
- With active root surface carious lesions;[19]
- No symptoms of an irreversible inflammation of the dental pulp.[17]
Contraindications
The use of SDF is contraindicated in the following scenarios:
Patients
- With an allergy to Silver or compounds containing silver;[20]
- With ulcerative gingivitis or stomatitis;[15] due to pain, can be managed with cautious use of a mucosal covering.
- Unable to tolerate treatment.
Teeth
- With irreversible pulpitis[17][21] or direct pulp exposure.
- Where it is not possible to achieve adequate isolation of tooth and oral tissues.
Mode of action
SDF's mode of action is well documented, but remains contested. Rosenblatt et al.[1] summarized how the constituents in SDF each have a role in the arrest of microbial species that cause dental caries. The higher the concentration of fluoride in a compound, the more effective its mechanisms in inhibiting bacterial biofilm formation. Fluorides can bind to bacterial cell walls, inhibiting enzymatic processes associated with sugar uptake and metabolism of carbohydrate, therefore producing a surface more resistant to acid dissolution.[2][22]
Similarly, the silver in SDF kills cariogenic bacteria by interacting with DNA and cellular proteins. This leads to cessation of cellular metabolism preventing bacterial cell wall synthesis and DNA synthesis, and ATP production. These actions destroy plaque biofilms, and subsequently arrest dental caries.[22][23]
SDF hardens carious dentin, such that it is twice as hard as healthy dentin[24]
Effect on cariogenic bacteria
Colony Forming Unit counts (CFU) and studies of multispecies carious biofilms were carried aiming to examine the action of SDF on cariogenic bacteria.[2] CFU counts on Streptococci mutans, Actinomyces naeslundii, Lactobacillus acidophilus, Streptococcus sobrinus, Lactobacillus rhamnosus (all of which are bacteria intimately associated with the carious process) were significant lower in both dentin surfaces and demineralized dentin treated with SDF when compared to water application. SDF also inhibits the adherence of S.mutans to tooth surfaces.[2]
Targino et al. (2014) reported that minimum bacterial concentration and minimum inhibitory concentration of SDF for S.mutans were 50.0 ug/ml and 33.3 ug/ml respectively.[25] This shows that SDF as a compound has better bactericidal effects than silver ammonium nitrate and sodium fluoride (commonly found in toothpastes).[26][27]
Effect on organic content on dentin
The affected layer of carious dentin in teeth can be identified by the presence of intact collagen fibres. Studies have revealed that a larger amount of intact collagen fibres remain on dentine surfaces (perpendicular to the enamel dentine junction) when treated with SDF as compared to water.[2]
SDF inhibits proteolytic activities such as enzymatic degradation of collagen fibres by matrix metalloproteinases MMP-2, 8 and 9.[2] Furthermore, SDF stops the degradation of cysteine cathepsins, which are also responsible for dentine collagen degradation.[23]
Recommended concentration
A systematic review conducted by Contreras et al. in 2017 concluded that 30% and 38% concentrations of SDF were most effective for caries arrest.[28] One of the clinical trials in this systematic review found 38% SDF to be significantly more effective for the prevention of caries in primary teeth, with 80% fewer new lesions in primary teeth, and 65% fewer new lesions in first permanent molars.[29] Yee et al. (2009) compared the effectiveness of 38% against 12% SDF, with or without using a reducing agent for the caries arrest. Over a 24-month period, it was concluded that there was a higher rate of lesion arrest in teeth treated with 38% SDF (with and without the reducing agents) as compared to 12% SDF.[30]
Frequency of application
A randomised clinical trial conducted by Zhi et al. (2012) found that increasing the frequency of SDF application from once to twice per year increased the rate of caries arrest.[31] The American Academy of Paediatric Dentistry (AAPD) recommends a 2-4 week follow-up to assess the arrest of carious lesions treated with SDF.[32][33] If the lesions do not appear to have arrested (i.e. dark in colour and tactilely hard), it is suggested by them to reapply. Subsequent restoration of the carious lesion may be indicated following the application of SDF to restore aesthetics. If these lesions are not restored following SDF application, the AAPD recommends application biannually, as this has shown an increased caries lesion arrest rate as compared to annual application.[34]
Maximum dose
Average LD50 in mice and rats by oral administration was 520 mg/kg, and by subcutaneous administration was 380 mg/kg. The subcutaneous route is taken here as a worst-case scenario. One drop (32.5 μL) is ample material to treat 5 teeth, and contains 12.35 mg silver diamine fluoride. Assuming the smallest child with caries would be in the range of 10 kg, the dose would be 1.235 mg / kg child. Based on this, UCSF recommended 1 drop per 10 kg of body weight per visit.[15]
The US FDA reviewed the dose limit based on all evidence for the US multi-centered clinical trial sponsored by the NIH and FDA run by UM, NYU, and UIowa, and set a dose limit of 260 µL for any patient 12 – 59 months old at the start of the study. ClinicalTrials.gov Identifier: NCT03649659.
Precautions and adverse effects
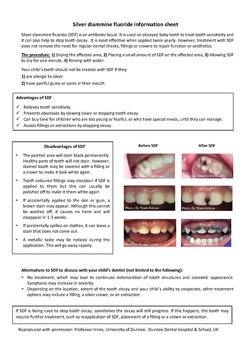
The main side effect of SDF is non-medical and is the prominent black staining of carious tooth tissue where the solution is applied.[35]
SDF will stain most things it touches, including skin, mucous membranes, clothing and work surfaces. Chu et al. reported on the first modern clinical trial of SDF that the stain was generally acceptable and "the presence of darkened teeth was mentioned by around 7% of the parents."[36]
Another side effect is an intensely bitter metallic flavor, which subsides in minutes.
No serious adverse reactions (e.g. life-threatening reactions, hospitalization, toxicity or death) have been reported in the scientific literature. Two safety studies have been done in children.[37][38]
Pharmacokinetic studies in adults found no adverse effects and demonstrated a lack of any increase of Fluoride in the blood. Increases in serum Silver were observed.[39]
Systematic reviews[40][15][11][41][42][28][32][19][1] reported adverse reactions following SDF use. These reactions manifested as small, white lesions of the oral mucosa that healed over the course of 48 hours. Furthermore, an umbrella review by Seifo et al. (2020) did not report any serious adverse reactions.[8]
Arresting caries progression
- A systematic review and meta-analysis from 2017 by Chibinski et al. analysed the arrest of caries in primary teeth over a 12-month period. SDF was able to arrest caries at a 66% higher (95% CI 41-91%; p < 0.00001) rate than any other active material, and 154% (95% CI 67-85%; p < 0.00001) more than placebos. Overall, the study concluded that caries arrest was 89% higher (95% CI 49-138%; p < 0.00001) in SDF as compared to using any other active materials or placebos.[10]
- A further systematic review and meta-analysis by Trieu et al. (2019) concluded that SDF works more effectively for the arrest of dentine caries as compared to high concentration sodium fluoride preparations (e.g. Duraphat varnish). The evidence from this meta-analysis is considered strong.[9]
- Gao et al. (2016) reviewed 19 studies, 16 of which considered primary (baby) teeth and 3 on permanent (adult) teeth. The associated meta-analysis included 8 studies and revealed that 38% SDF (44,800ppm Fluoride) had achieved caries arrest in 86% of (95% confidence interval [CI], 47% to 98%; P = 0.06) dentinal carious lesions in primary teeth at six months interval, 81% (95% CI, 59% to 93%; P = 0.01) at 12 months and 65% (95% CI, 35% to 86%; P = 0.32) at 24 months. Overall, 81% of active caries lesions had arrested following SDF treatment.[32]
- Horst (2018) reviewed 10 clinical trials in children and adults and suggested "to skip the rinsing step due to demonstration of safety in young children, start patients with high disease severity on an intensive regimen of multiple applications over the first few weeks, and continue with semiannual maintenance doses as previously suggested."[5]
- An umbrella review by Seifo et al. (2019) found that SDF was favoured as a treatment option for the arrest and prevention of root caries lesions. As for coronal caries lesions, comparisons were drawn between SDF, fluoride varnish, glass ionomer cement and placebos as treatment modalities.[8] It was found that SDF had the highest caries arrest rate.
- A systematic review of caries prevention by SDF in children with a low threshold for inclusion - any comparative clinical study with a control or placebo group - found a 61% preventive fraction.[43]
- One systematic review also presented and concluded that SDF may potentially be a treatment option for the prevention of caries in first permanent molars however the evidence to support this is inconclusive.[28]
History
- Dental use of silver nitrate can be traced back to Japan around 1000 AD, where it was used for cosmetic purposes of blackening of teeth. Silver nitrate followed by application of fluoride varnish was the only non-invasive option available for caries treatment before the advent for silver diamine fluoride (SDF). Cases of carious lesions treated and arrested by the application of silver nitrate date to 19th century. Medical research study that dates back to 19th century showed 87 of 142 treated carious lesions were arrested.[3]
- Silver diamine was formed when ammonia was added to silver nitrate to make it stable and effective as an antibacterial for application to caries lesions and infected root canals.[44]
- SDF was developed by Reichi Yamaga, Misuho Nishino, and colleagues to prevent and treat dental caries.[45]
- SDF was approved by PMDA (equivalent of FDA) in 1970 in Japan and has been used there since.
- SDF has been widely used in Australia and Brazil since 1980 with in vivo studies done in the respective countries.[3]
- In 2014 the FDA cleared SDF as a medical device for treating dental hypersensitivity.
- In January 2016 in the US, a new Code on Dental Procedures and Nomenclature (CDT), D1354, allowed billing claims for off-label use of SDF as an interim caries-arresting medicine.
- In 2017, Canada approved use to treat dental caries.
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 "Silver diamine fluoride: a caries "silver-fluoride bullet"". Journal of Dental Research 88 (2): 116–25. February 2009. doi:10.1177/0022034508329406. PMID 19278981.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 "Mechanisms of silver diamine fluoride on arresting caries: a literature review". International Dental Journal 68 (2): 67–76. April 2018. doi:10.1111/idj.12320. PMID 28542863.
- ↑ 3.0 3.1 3.2 "Is Silver Diamine Fluoride Effective in Preventing and Arresting Caries in Elderly Adults? A Systematic Review". Journal of International Society of Preventive & Community Dentistry 8 (3): 191–199. 2018. doi:10.4103/jispcd.JISPCD_99_18. PMID 29911054.
- ↑ "Silver Diamine Fluoride: A Successful Anticarious Solution with Limits". Advances in Dental Research 29 (1): 131–134. February 2018. doi:10.1177/0022034517740123. PMID 29355424.
- ↑ 5.0 5.1 "Silver Fluoride as a Treatment for Dental Caries". Advances in Dental Research 29 (1): 135–140. February 2018. doi:10.1177/0022034517743750. PMID 29355428.
- ↑ "Nonrestorative Approaches for Managing Cavitated Dentin Carious Lesions: Silver Fluoride". Pediatric Restorative Dentistry. Springer. September 11, 2018. p. 143. ISBN 978-3-319-93426-6. https://books.google.com/books?id=HDBuDwAAQBAJ&pg=PA143.
- ↑ "Off-label or unlicensed use of medicines: prescribers' responsibilities" (in en). https://www.gov.uk/drug-safety-update/off-label-or-unlicensed-use-of-medicines-prescribers-responsibilities.
- ↑ 8.0 8.1 8.2 "Silver diamine fluoride for managing carious lesions: an umbrella review". BMC Oral Health 19 (1): 145. July 2019. doi:10.1186/s12903-019-0830-5. PMID 31299955.
- ↑ 9.0 9.1 "Silver diamine fluoride versus sodium fluoride for arresting dentine caries in children: a systematic review and meta-analysis". Scientific Reports 9 (1): 2115. February 2019. doi:10.1038/s41598-019-38569-9. PMID 30765785. Bibcode: 2019NatSR...9.2115T.
- ↑ 10.0 10.1 "Silver Diamine Fluoride Has Efficacy in Controlling Caries Progression in Primary Teeth: A Systematic Review and Meta-Analysis". Caries Research 51 (5): 527–541. 2017. doi:10.1159/000478668. PMID 28972954.
- ↑ 11.0 11.1 "Clinical Trials of Silver Diamine Fluoride in Arresting Caries among Children: A Systematic Review" (in en-US). JDR Clinical and Translational Research 1 (3): 201–210. October 2016. doi:10.1177/2380084416661474. PMID 30931743.
- ↑ "The use of silver diamine fluoride (SDF) in dental practice". British Dental Journal 228 (2): 75–81. January 2020. doi:10.1038/s41415-020-1203-9. PMID 31980777. https://www.nature.com/articles/s41415-020-1203-9.
- ↑ "510(k) Premarket Notification". http://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfpmn/pmn.cfm?ID=K102973.
- ↑ World Health Organization model list of essential medicines: 22nd list (2021). Geneva: World Health Organization. 2021. WHO/MHP/HPS/EML/2021.02.
- ↑ 15.0 15.1 15.2 15.3 15.4 15.5 15.6 15.7 15.8 "UCSF Protocol for Caries Arrest Using Silver Diamine Fluoride: Rationale, Indications and Consent". Journal of the California Dental Association 44 (1): 16–28. January 2016. doi:10.1080/19424396.2016.12220962. PMID 26897901.
- ↑ "Evidence of Effectiveness of Current Therapies to Prevent and Treat Early Childhood Caries". Pediatric Dentistry 37 (3): 246–53. 2015. PMID 26063553.
- ↑ 17.0 17.1 17.2 17.3 "Use of Silver Diamine Fluoride for Dental Caries Management in Children and Adolescents, Including Those with Special Health Care Needs". Pediatric Dentistry 39 (5): 135–145. September 2017. PMID 29070149.
- ↑ "Minimally Invasive Treatment for Molar Incisor Hypomineralization" (in en-US). 6 November 2018. https://decisionsindentistry.com/article/minimally-invasive-treatment-for-molar-incisor-hypomineralization/.
- ↑ 19.0 19.1 "Controlling caries in exposed root surfaces with silver diamine fluoride: A systematic review with meta-analysis". Journal of the American Dental Association 149 (8): 671–679.e1. August 2018. doi:10.1016/j.adaj.2018.03.028. PMID 29805039.
- ↑ "Clinical Use of Silver Diamine Fluoride in Dental Treatment". Compendium of Continuing Education in Dentistry 37 (2): 93–8; quiz100. February 2016. PMID 26905088.
- ↑ "Evidence-Based Dentistry Update on Silver Diamine Fluoride". Dental Clinics of North America 63 (1): 45–68. January 2019. doi:10.1016/j.cden.2018.08.011. PMID 30447792.
- ↑ 22.0 22.1 "Effects of different antibacterial agents on enamel in a biofilm caries model". Journal of Oral Science 57 (4): 367–72. 2015. doi:10.2334/josnusd.57.367. PMID 26666861.
- ↑ 23.0 23.1 "The inhibitory effects of silver diamine fluorides on cysteine cathepsins". Journal of Dentistry 42 (3): 329–35. March 2014. doi:10.1016/j.jdent.2013.11.018. PMID 24316241.
- ↑ "Microhardness of dentine in primary teeth after topical fluoride applications". Journal of Dentistry 36 (6): 387–91. June 2008. doi:10.1016/j.jdent.2008.02.013. PMID 18378377.
- ↑ "An innovative approach to treating dental decay in children. A new anti-caries agent". Journal of Materials Science: Materials in Medicine 25 (8): 2041–7. August 2014. doi:10.1007/s10856-014-5221-5. PMID 24818873.
- ↑ "Effect of diammine silver fluoride on plaque formation by Streptococcus mutans". Japanese Journal of Oral Biology 18 (3): 268–278. 1976. doi:10.2330/joralbiosci1965.18.268.
- ↑ "[Effect of a silver ammonia fluoride solution on the prevention and inhibition of caries]". Zhonghua Kou Qiang Ke Za Zhi [Chinese Journal of Stomatology] 19 (2): 97–100. June 1984. PMID 6596183.
- ↑ 28.0 28.1 28.2 "Effectiveness of silver diamine fluoride in caries prevention and arrest: a systematic literature review". General Dentistry 65 (3): 22–29. 2017. PMID 28475081.
- ↑ "Efficacy of silver diamine fluoride for caries reduction in primary teeth and first permanent molars of schoolchildren: 36-month clinical trial". Journal of Dental Research 84 (8): 721–4. August 2005. doi:10.1177/154405910508400807. PMID 16040729.
- ↑ "Efficacy of silver diamine fluoride for Arresting Caries Treatment". Journal of Dental Research 88 (7): 644–7. July 2009. doi:10.1177/0022034509338671. PMID 19641152.
- ↑ "Randomized clinical trial on effectiveness of silver diamine fluoride and glass ionomer in arresting dentine caries in preschool children". Journal of Dentistry 40 (11): 962–7. November 2012. doi:10.1016/j.jdent.2012.08.002. PMID 22892463.
- ↑ 32.0 32.1 32.2 "Caries remineralisation and arresting effect in children by professionally applied fluoride treatment - a systematic review". BMC Oral Health 16 (1): 12. February 2016. doi:10.1186/s12903-016-0171-6. PMID 26831727.
- ↑ "Restorative approaches to treat dentin caries in preschool children: systematic review". European Journal of Paediatric Dentistry 17 (2): 113–21. June 2016. PMID 27377109.
- ↑ "Chairside Guide: Silver Diamine Fluoride in the Management of Dental Caries Lesions*". 2019–2020. https://www.aapd.org/media/Policies_Guidelines/R_ChairsideGuide.pdf.
- ↑ "Evaluation of the staining potential of silver diamine fluoride: in vitro". International Journal of Paediatric Dentistry 28 (5): 514–522. July 2018. doi:10.1111/ipd.12401. PMID 29974546.
- ↑ "Effectiveness of silver diamine fluoride and sodium fluoride varnish in arresting dentin caries in Chinese pre-school children". Journal of Dental Research 81 (11): 767–70. November 2002. doi:10.1177/0810767. PMID 12407092.
- ↑ "Topical silver diamine fluoride for dental caries arrest in preschool children: A randomized controlled trial and microbiological analysis of caries associated microbes and resistance gene expression". Journal of Dentistry 68: 72–78. January 2018. doi:10.1016/j.jdent.2017.08.015. PMID 28866468.
- ↑ "Adverse Effects of Silver Diamine Fluoride Treatment among Preschool Children". Journal of Dental Research 97 (4): 395–401. April 2018. doi:10.1177/0022034517746678. PMID 29237131.
- ↑ "Pharmacokinetics of Iodine and Fluoride following Application of an Anticaries Varnish in Adults". JDR Clinical and Translational Research 3 (3): 238–245. July 2018. doi:10.1177/2380084418771930. PMID 30938600.
- ↑ "Non-surgical treatment of dentin caries in preschool children--systematic review". BMC Oral Health 15 (1): 44. April 2015. doi:10.1186/s12903-015-0033-7. PMID 25888484.
- ↑ "A systematic review of silver diamine fluoride: Effectiveness and application in older adults". Gerodontology 34 (4): 411–419. December 2017. doi:10.1111/ger.12294. PMID 28812312.
- ↑ "The Effect of Silver Diamine Fluoride in Preventing Caries in the Primary Dentition: A Systematic Review and Meta-Analysis". Caries Research 53 (1): 24–32. 2019. doi:10.1159/000488686. PMID 29874642.
- ↑ "Prevention of Dental Caries by Silver Diamine Fluoride". Compend Contin Educ Dent 40 (3): 158–163. 2019. PMID 30829497.
- ↑ "A method of sterilizing and at the same time impregnating with a metal affected dentinal tissue". Dental Cosmos 59: 891–904. 1917.
- ↑ "Diammine Silver Fluoride and Its Clinical Application". J Osaka Univ Dent Sch 12: 1–20. 1972. PMID 4514730.
 |