Medicine:Stomatitis
| Stomatitis | |
|---|---|
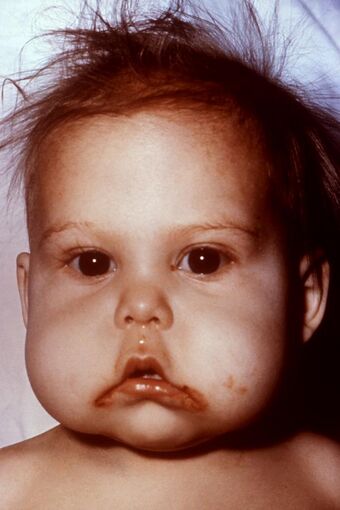 | |
| An infant with stomatitis due to kwashiorkor and an accompanying Vitamin B deficiency. | |
| Specialty | Dermatology |
Stomatitis is inflammation of the mouth and lips.[1] It refers to any inflammatory process affecting the mucous membranes of the mouth and lips, with or without oral ulceration.[2]
In its widest meaning, stomatitis can have a multitude of different causes and appearances. Common causes include infections, nutritional deficiencies, allergic reactions, radiotherapy, and many others.
When inflammation of the gums and the mouth generally presents itself, sometimes the term gingivostomatitis is used, though this is also sometimes used as a synonym for herpetic gingivostomatitis.
The term is derived from the Greek stoma (στόμα), meaning "mouth", and the suffix -itis (-ῖτις), meaning "inflammation".
Causes
Nutritional deficiency
Malnutrition (improper dietary intake) or malabsorption (poor absorption of nutrients into the body) can lead to nutritional deficiency states, several of which can lead to stomatitis. For example, deficiencies of iron, vitamin B2 (riboflavin),[3]: 490 vitamin B3 (niacin), vitamin B6 (pyridoxine), vitamin B9 (folic acid) or vitamin B12 (cobalamine) may all manifest as stomatitis. Iron is necessary for the upregulation of transcriptional elements for cell replication and repair. Lack of iron can cause genetic downregulation of these elements, leading to ineffective repair and regeneration of epithelial cells, especially in the mouth and lips. Many disorders which cause malabsorption can cause deficiencies, which in turn causes stomatitis. Examples include tropical sprue.[3]: 49
Aphthous stomatitis
Aphthous stomatitis (canker sores) is the recurrent appearance of mouth ulcers in otherwise healthy individuals. The cause is not completely understood, but it is thought that the condition represents a T cell mediated immune response which is triggered by a variety of factors. The individual ulcers (aphthae) recur periodically and heal completely, although in the more severe forms, new ulcers may appear in other parts of the mouth before the old ones have finished healing. Aphthous stomatitis is one of the most common diseases of the oral mucosa, and is thought to affect about 20% of the general population to some degree.[4] The symptoms range from a minor nuisance to being disabling in their impact on eating, swallowing, and talking, and the severe forms can cause people to lose weight. There is no cure for aphthous stomatitis,[5] and therapies are aimed at alleviating the pain, reducing the inflammation and promoting healing of the ulcers, but there is little evidence of efficacy for any treatment that has been used.
Angular stomatitis
Inflammation of the corners (angles) of the lips is termed angular stomatitis or angular cheilitis. In children a frequent cause is repeated lip-licking, and in adults it may be a sign of underlying iron deficiency anemia, or vitamin B deficiencies (e.g., B2-riboflavin, B9-folate, or B12-cobalamin, which in turn may be evidence of poor diets or malnutrition such as celiac disease).
Also, angular cheilitis can be caused by a patient's jaws at rest being 'overclosed' due to edentulousness or tooth wear, causing the jaws to come to rest closer together than if the complete/unaffected dentition were present. This causes skin folds around the angle of the mouth which are kept moist by saliva, which in turn favours infection; mostly by Candida albicans or similar species. Treatment usually involves the administration of topical nystatin or similar antifungal agents. Another treatment can be to correct the jaw relationship with dental treatment (e.g., dentures or occlusal adjustment).
Denture-related stomatitis
This is a common condition present in denture wearers. It appears as reddened but painless mucosa beneath the denture. 90% of cases are associated with Candida species, and it is the most common form of oral candidiasis. Treatment is by antifungal medication and improved dental hygiene, such as not wearing the denture during sleep.
Allergic contact stomatitis
Allergic contact stomatitis (also termed "allergic gingivostomatitis" or "allergic contact gingivostomatitis")[6] is a type IV (delayed) hypersensitivity reaction that occurs in susceptible atopic individuals when allergens penetrate the skin or mucosa.[7]
Allergens, which may be different for different individuals, combine with epithelial-derived proteins, forming haptens which bind with Langerhans cells in the mucosa, which in turn present the antigen on their surface to T lymphocytes, sensitizing them to that antigen and causing them to produce many specific clones. The second time that specific antigen is encountered, an inflammatory reaction is triggered at the site of exposure.[7] Allergic contact stomatitis is less common than allergic contact dermatitis because the mouth is coated in saliva, which washes away antigens and acts as a barrier.[7] The oral mucosa is also more vascular (has a better blood supply) than skin, meaning that any antigens are more quickly removed from the area by the circulation.[7] Finally, there is substantially less keratin in oral mucosa, meaning that there is less likelihood that haptens will form.[7]
Allergic contact stomatitis appears as non-specific inflammation, so it may be mistaken for chronic physical irritation.[7] There may be burning or soreness of the mouth and ulceration.[7] Chronic exposure to the allergen may result in a lichenoid lesion.[7] Plasma cell gingivitis may also occur, which may be accompanied by glossitis and cheilitis.[7]

Allergens that may cause allergic contact stomatitis in some individuals include cinnamaldehyde, Balsam of Peru, peppermint, mercury, gold, pyrophosphates, zinc citrate, free acrylic monomer, nickel, fluoride, and sodium lauryl sulfate.[7][8][9][10][11][12][13] These allergens may originate from many sources, including various foods and drink, chewing gum, toothpaste, mouthwash, dental floss, dental fillings, dentures, orthodontic bands or wires, and many other sources.[7] If the substance containing the allergen comes into contact with the lips, allergic contact cheilitis can occur, together with allergic contact stomatitis.
The diagnosis is confirmed by patch test, and management is by avoidance of exposure to the allergen.[7]
Migratory stomatitis
Migratory stomatitis (or geographic stomatitis) is an atypical presentation of a condition which normally presents on the tongue, termed geographic tongue. Geographic tongue is so named because there are atrophic, erythematous areas of depapillation that migrate over time, giving a map-like appearance.
In migratory stomatitis, other mucosal sites in the mouth, such as the ventral surface (undersurface) of the tongue, buccal mucosa, labial mucosa, soft palate, or floor of mouth may be afflicted with identical lesions, usually in addition to the tongue.[14] Apart from not being restricted to the tongue, migratory stomatitis is an identical condition in every regard to geographic tongue. Another synonym for geographic tongue which uses the term stomatitis is "stomatitis areata migrans".
Herpetic gingivostomatitis

This is inflammation of the mouth caused by herpes simplex virus.
Irradiation and chemotherapy
Stomatitis may also be caused by chemotherapy, or radiation therapy of the oropharyngeal area.[15] The term mucositis is sometimes used synonymously with stomatitis, however the former usually refers to mucosal reactions to radiotherapy or chemotherapy, and may occur anywhere in the gastrointestinal tract and not just in the mouth.[16]
Necrotizing ulcerative gingivostomatitis
The term necrotizing ulcerative gingivostomatitis is sometimes used as a synonym of the necrotizing periodontal disease more commonly termed necrotizing ulcerative gingivitis, or a more severe form (also termed necrotizing stomatitis). The term necrotizing gingivostomatitis is also sometimes used.[17]
Stomatitis nicotina
Also called smoker's palatal keratosis,[18]: 176 this condition may occur in smokers, especially pipe smokers. The palate appears dry and cracked, and white from keratosis. The minor salivary glands appear as small, red and swollen bumps. It is not a premalignant condition, and the appearance reverses if the smoking is stopped.[18]: 176
Chronic ulcerative stomatitis
Chronic ulcerative stomatitis is a condition with specific immunopathologic features, which was first described in 1990.[19] It is characterized by erosions and ulcerations which relapse and remit. Lesions are located on the buccal mucosa (inside of the cheeks) or on the gingiva (gums).[20][21] The condition resembles oral lichen planus when biopsied.
The diagnosis is made by microscopic examination of biopsy tissue: direct immunofluorescence can reveal the presence of antinuclear antibodies specifically directed against the ΔNp63α form of the p63 protein, which is normally expressed within the basal layer of stratified epithelium.[19] Treatment with hydroxychloroquine can be effective.[19]
Plasma cell gingivostomatitis
Terms such as plasma cell gingivostomatitis,[22] atypical gingivostomatitis and idiopathic gingivostomatitis[23][24] are sometimes a synonym for plasma cell gingivitis, or specifically to refer to a severe form of plasma cell gingivitis.
Other forms of stomatitis
- Periodic fever, aphthous stomatitis, pharyngitis and adenitis (PFAPA) syndrome—occurs in children.
- Uremic stomatitis—a rare form of stomatitis that occurs with kidney failure.[25]
- Pyostomatitis vegetans
- Bovine papular stomatitis
References
- ↑ Pediatric infectious diseases. Philadelphia: Mosby/Elsevier. 2008. ISBN 9780323076333. https://books.google.com/books?id=e9rT3TcDYNAC&q=stomatitis+definition&pg=PT361.
- ↑ "35". Differential diagnosis in otolaryngology – head and neck surgery. New York: Thieme. 2010-10-04. ISBN 9781604062793. https://books.google.com/books?id=p-rSREngtBUC&q=stomatitis+definition&pg=PT151. Retrieved 2020-11-03.
- ↑ 3.0 3.1 Textbook of gastroenterology (5th ed.). Chichester, West Sussex: Blackwell Pub.. 2009. ISBN 978-1-4051-6911-0.
- ↑ Oral & maxillofacial pathology (2nd ed.). Philadelphia: W.B. Saunders. 2002. pp. 253–284. ISBN 978-0721690032. https://archive.org/details/oralmaxillofacia00nevi.
- ↑ Brocklehurst, P; Tickle, M; Glenny, AM; Lewis, MA; Pemberton, MN; Taylor, J; Walsh, T; Riley, P et al. (Sep 12, 2012). Brocklehurst, Paul. ed. "Systemic interventions for recurrent aphthous stomatitis (mouth ulcers).". The Cochrane Database of Systematic Reviews 9 (9): CD005411. doi:10.1002/14651858.CD005411.pub2. PMID 22972085.
- ↑ Kanerva, L.; Alanko, K.; Estlander, T. (1 December 1999). "Allergic contact gingivostomatitis from a temporary crown made of methacrylates and epoxy diacrylates". Allergy 54 (12): 1316–1321. doi:10.1034/j.1398-9995.1999.00074.x. PMID 10688437.
- ↑ 7.00 7.01 7.02 7.03 7.04 7.05 7.06 7.07 7.08 7.09 7.10 7.11 Burket's oral medicine diagnosis & treatment (10th ed.). Hamilton, Ont.: BC Decker. 2003. pp. 60, 61. ISBN 978-1550091861. https://archive.org/details/burketsoralmedic00burk.
- ↑ Gottfried Schmalz; Dorthe Arenholt Bindslev (2008). Biocompatibility of Dental Materials. Springer. ISBN 9783540777823. https://books.google.com/books?id=mrreTHuo54wC&q=balsam+of+peru+allergy&pg=PA352. Retrieved March 5, 2014.
- ↑ Thomas P. Habif (2009). Clinical Dermatology. Elsevier Health Sciences. ISBN 978-0323080378. https://books.google.com/books?id=kDWlWR5UbqQC&q=%22balsam+of+peru%22+allergy&pg=PT530. Retrieved March 6, 2014.
- ↑ Edward T. Bope; Rick D. Kellerman (2013). Conn's Current Therapy 2014: Expert Consult. Elsevier Health Sciences. ISBN 9780323225724. https://books.google.com/books?id=fmwYAgAAQBAJ&q=%22balsam+of+peru%22+allergy&pg=PT264. Retrieved March 6, 2014.
- ↑ "Balsam of Peru contact allergy". Dermnetnz.org. December 28, 2013. http://dermnetnz.org/dermatitis/balsam-of-peru-allergy.html.
- ↑ James, William D.; Berger, Timothy G.; et al. (2006). Andrews' Diseases of the Skin: Clinical Dermatology. Saunders Elsevier. p. 63. ISBN 0-7216-2921-0.
- ↑ J. J. Shea, M.D., F.A.C.A., S. M. Gillespie, M.D., G. L. Waldbott, M.D. Allergy to Fluoride. Annals of Allergy, Volume 25, July, 1967
- ↑ Clinical oral medicine and pathology. New York: Humana Press. 2010. pp. 20, 21. ISBN 978-1-60327-519-4. https://archive.org/details/clinicaloralmedi00bruc.
- ↑ Berger, Ann M.; Shuster, John L.; von Roenn, Jamie H. (2007). Principles and Practice of Palliative Care and Supportive Oncology. Lippincott Williams & Wilkins. ISBN 9780781795951. https://books.google.com/books?id=LngD6RFXY_AC&q=cause+%22stomatitis%22&pg=PA205. Retrieved 2014-03-20.
- ↑ Zeppetella, Giovambattista (2012-06-14). Palliative care in clinical practice. London: Springer. p. 132. ISBN 9781447128434. https://books.google.com/books?id=S8mJLlnuNcMC&q=stomatitis+definition&pg=PA132.
- ↑ Horning, GM (October 1996). "Necotizing gingivostomatitis: NUG to noma.". Compendium of Continuing Education in Dentistry 17 (10): 951–4, 956, 957–8 passim; quiz 964. PMID 9533316.
- ↑ 18.0 18.1 Master dentistry volume 1, oral and maxillofacial surgery, radiology, pathology and oral medicine (2nd ed.). Edinburgh: Churchill Livingstone/Elsevier. 2008. ISBN 9780443068966. https://archive.org/details/masterdentistry0000unse.
- ↑ 19.0 19.1 19.2 "Chronic ulcerative stomatitis: A comprehensive review and proposal for diagnostic criteria". Oral Diseases 25 (6): 1465–1491. 2019. doi:10.1111/odi.13001. PMID 30457193. http://www.exodontia.info/files/Oral_Diseases_2019._Chronic_Ulcerative_Stomatitis._A_Comprehensive_Review_Proposal_for_Diagnostic_Criteria.pdf.
- ↑ Scully, Crispian (2008). Oral and maxillofacial medicine: the basis of diagnosis and treatment (2nd ed.). Edinburgh: Churchill Livingstone. ISBN 9780443068188.
- ↑ "Chronic ulcerative stomatitis: a distinct clinical entity?". South African Dental Journal 66 (3): 119–21. April 2011. PMID 21874892.
- ↑ Oral & maxillofacial pathology (2nd ed.). Philadelphia: W.B. Saunders. 2002. pp. 141, 142. ISBN 978-0721690032. https://archive.org/details/oralmaxillofacia00nevi.
- ↑ Janam, P; Nayar, BR; Mohan, R; Suchitra, A (January 2012). "Plasma cell gingivitis associated with cheilitis: A diagnostic dilemma!". Journal of Indian Society of Periodontology 16 (1): 115–9. doi:10.4103/0972-124X.94618. PMID 22628976.
- ↑ Kerr, DA; McClatchey, KD; Regezi, JA (September 1971). "Idiopathic gingivostomatitis. Cheilitis, glossitis, gingivitis syndrome; atypical gingivostomatitis, plasma-cell gingivitis, plasmacytosis of gingiva.". Oral Surgery, Oral Medicine, and Oral Pathology 32 (3): 402–23. doi:10.1016/0030-4220(71)90201-5. PMID 5285187.
- ↑ Laskaris, George (2006). Pocket atlas of oral diseases (2nd ed.). Stuttgart: Thieme. p. 12. ISBN 9781588902498. https://archive.org/details/pocketatlasorald00lask.
External links
| Classification |
|---|
 |
