Medicine:Hippocampal sclerosis
| Hippocampal sclerosis | |
|---|---|
 | |
| Mesial temporal sclerosis (MTS) | |
| Specialty | Neurology |
Hippocampal sclerosis (HS) or mesial temporal sclerosis (MTS) is a neuropathological condition with severe neuronal cell loss and gliosis in the hippocampus.[1] Neuroimaging tests such as magnetic resonance imaging (MRI) and positron emission tomography (PET) may identify individuals with hippocampal sclerosis.[2] Hippocampal sclerosis occurs in 3 distinct settings: mesial temporal lobe epilepsy, adult neurodegenerative disease and acute brain injury.[2][3]:1503
History
In 1825, Bouchet and Cazauvieilh described palpable firmness and atrophy of the uncus and medial temporal lobe of brains from epileptic and non-epileptic individuals.[4]:565 In 1880, Wilhelm Sommer investigated 90 brains and described the classical Ammon's horn sclerosis pattern, severe neuronal cell loss in hippocampal subfield cornum Ammonis 1 (CA1) and some neuronal cell loss in hippocampal subfield CA4. a finding later confirmed by Bratz.[4]:565[5] In 1927, Spielmeyer described cell loss of all hippocampal subfields, the total Ammon's horn sclerosis pattern, and in 1966, Margerison and Corsellis described cell loss primarily involving the CA4 subfield, the end folium sclerosis pattern.[4]:566 In 1935. Stauder linked mesial temporal lobe seizures to hippocampal sclerosis.[4]:566
Hippocampal sclerosis was later found to occur in older adults with neurodegenerative diseases such as frontotemporal lobar degeneration and amyotrophic lateral sclerosis.[6][3]:1505 In 2006, researchers determined that amyotrophic lateral sclerosis and frontotemporal lobar degeneration are often TAR DNA-binding protein 43 (TDP-43) proteinopathies.[3]:1506 In 2009, researchers recognized that about 10-20% of individuals with frontotemporal lobar degeneration not caused by tau proteinopathy occurred because of a RNA-binding protein FUS (FUS) proteinopathy; hippocampal sclerosis often accompanied the FUS proteinopathy.[7]
In 1994, Dickson et al. described hippocampal sclerosis occurring in elderly demented individuals > 80 years old with disproportionately greater impaired memory.[8][9] In 2007, researchers determined that this neurodegenerative disease, Limbic-predominant age-related TDP-43 encephalopathy (LATE), is a TDP-43 proteinopathy.[3]:1505
Pathology
Mesial temporal lobe epilepsy
The typical brain sample is a surgical specimen, a brain sample obtained during epilepsy surgery.[1] The International League Against Epilepsy (ILAE) defines 3 hippocampal sclerosis (HS) types: predominant neuronal cell loss in subfields CA1 and CA4 (HS ILAE type 1), subfield CA1 (HS ILAE type 2) or subfield CA4 (HS ILAE type 3).[1]:1315 The classic and total Ammon's horn sclerosis pattern correspond to HS ILAE type 1.[1]:1318 Among brain samples with hippocampal sclerosis, HS ILAE type 1 is the most prevalent, HS ILAE type 2 has a 5-10% prevalence, and HS ILAE type 3 has a 4-7.4% prevalence.[1]:1318–1319 Mossy fiber sprouting is common.[10]:697
Dentate gyrus granule cell dispersion refers to a granule cell layer that is widened, poorly demarcated, or accompanied by granule cells outside the layer (ectopic granule cells).[1]:1318 Although this pattern was thought to be linked to hippocampal sclerosis, a comparative study has shown this association is not correct as the same pattern occurs in brains without hippocampal sclerosis.[11]
A dual pathology is a temporal lobe abnormality that accompanying hippocampal sclerosis.[12]:126 This occurs in about 15% of those with hippocampal sclerosis who completed epilepsy surgery.[12]:126 The dual pathologies include cavernous hemangioma, heterotopia, cortical dysplasia, arteriovenous malformation, dysembryoplastic neuroepithelial tumor, cerebral infarction and cerebral contusion.[12]:129 The common association is dual pathology with HS ILAE type 3.[1]:1319
Adult neurodegenerative disease
The typical brain sample is an autopsy specimen, a brain sample obtained during an autopsy.[3]:1503
For elderly adults with suspected LATE, TDP-43 immunochemistry will determine if TDP-43 proteinopathy caused hippocampal sclerosis.[13]:8–9 Pyramidal cell loss and gliosis occurs in the CA1 sector, subiculum, entorhinal cortex, and the amygdala.[3] The hippocampal neuronal cell loss and gliosis are disproportionate to the Alzheimer's disease "neuropathological change in the same section."[13] One sided hippocampal sclerosis has a 40-50% prevalence even when the TDP-43 inclusions involve both sides of the brain.[3]:1508 TDP-43 immunochemistry does not identify TDP-43 proteinopathy if hippocampal sclerosis arises from hypoxia or mesial temporal lobe epilepsy.[3]:1506 Mossy fiber sprouting is uncommon.[10]:697
The LATE consensus working group report proposed a LATE staging system based on the anatomic location of TPD-43 proteinopathy: amygdala alone (stage1), amygdala and hippocampus (stage 2), and amygdala, hippocampus, and middle frontal gyrus (stage 3); hippocampal sclerosis is not sufficient or necessary for staging.[3]:1505
Immunochemistry may identify RNA-binding protein FUS, phosphorylated tau protein or ubiquitin if frontotemporal lobar degeneration is not caused by TGP-43 proteinopathy.[13]:9
Neuroimaging
Mesial temporal lobe epilepsy
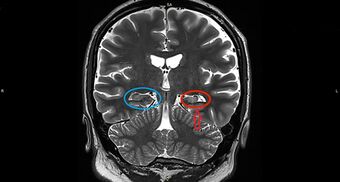
On a MRI T2-weighted or T2–fluid‐attenuated inversion recovery (FLAIR) scan, hippocampal sclerosis appears as an increased signal, smaller sized (atrophic) hippocampus with a less well-defined internal structure.[2] Increased signal means that hippocampal sclerosis will appear brighter on the MRI image. Less well-defined internal structure means the expected sharp boundaries between hippocampal gray and white matter structures are absent.[2] The total volume of the hippocampus is also reduced.[2] The reduced volume arises from neuronal cell loss, and increased signal arises from gliosis.[2]
The 18F-fluorodeoxyglucose PET (18F-FDG) scan may show decreased glucose metabolism in the temporal lobe with hippocampal atrophy.[2] This region of decreased glucose metabolism may extend beyond the hippocampus and involve the medial and lateral temporal lobe.[2]
Adult neurodegenerative disease
In LATE, MRI often shows asymmetrical hippocampal atrophy that progresses in a rostral-caudal gradient.[3]:1509 Inferior frontal, anterior temporal, and insular cortex atrophy often accompanies LATE hippocampal atrophy, the same anatomical pattern of TDP-43 proteinopathy at autopsy.[3]:1509 Reduced subiculum and CA1 volumes identified by MRI correspond to hippocampal sclerosis later identified at autopsy.[14]
The 18F-FDG PET scans of those with LATE show reduced glucose metabolism in the medial temporal lobe including the hippocampus.[15]:8S
Disorders with hippocampal sclerosis
Mesial temporal lobe epilepsy
Hippocampal sclerosis is the most common brain abnormality in those with temporal lobe epilepsy.[16] Hippocampal sclerosis may occur in children under 2 years of age with 1 instance seen as early as 6 months.[17] About 70% of those evaluated for temporal lobe epilepsy surgery have hippocampal sclerosis.[1]:1316 About 7% of those with temporal lobe epilepsy have familial mesial temporal lobe epilepsy, and 57% of those with familial mesial temporal lobe epilepsy have MRI evidence of hippocampal sclerosis.[18]
Electroencephalographic and surgical studies show that temporal lobe seizures arise from hippocampal regions with severe neuronal cell loss.[19]:9 Intracranial electroencephalogram records anterior hippocampal seizure onset in those with severe anterior hippocampal neuronal loss and combined anterior and posterior hippocampal seizure onset in those with severe combined anterior and posterior neuronal cell loss.[19]:9 Surgical removal of the hippocampus that spares neighboring structures leads to improved seizure control in many instances of mesial temporal lobe epilepsy.[19]:9 The absence of hippocampal sclerosis in some with temporal lobe epilepsy suggests that uncontrolled seizures do not invariably lead to hippocampal sclerosis.[19]:9
There is no clear relationship between febrile seizures and development of mesial temporal sclerosis.[20] Investigators found that hippocampal sclerosis and greater than 10-year epilepsy duration leads to parasympathetic dysfunction, refractory epilepsy leads to sympathetic dysfunction, and left hippocampal sclerosis leads to relatively greater parasympathetic dysfunction.[21] Hippocampal sclerosis may influence how the thalamus modulates the seizures of mesial temporal lobe epilepsy.[22]
The morbidity and mortality of refractory epilepsy and the adverse effects of medication treatment have a severe impact on life.[17] Those with an early age of epilepsy onset and hippocampal sclerosis have a poorer prognosis for becoming seizure-free.[16] Among those with intractable mesial temporal lobe epilepsy and hippocampal sclerosis, about 70% become seizure-free after epilepsy surgery.[23]:751
Adult neurodegenerative disease
In LATE, TDP-43, a normally non-phosphorylated protein residing in the nucleus, is phosphorylated and mislocalized in the cytoplasm and neurites.[3]:1506 The inclusions occur in the amygdala, hippocampus, entorhinal cortex, or dentate gyrus.[3]:1511 LATE occurs in about 20-50% of elderly individuals' brains.[3]:1505 About 5-40% of those with LATE occur without hippocampal sclerosis.[3]:1506 LATE appears as amnestic dementia similar to Alzheimer's disease in elderly adults > 80 years of age.[3]:1503
Hippocampal sclerosis occurs in other neurodegenerative diseases. Hippocampal sclerosis occurs in about 66% of those with frontotemporal lobar degeneration arising from TDP-43 or FUS proteinopathy.[24][7] Hippocampal sclerosis occurs in about 60% of those with progressive supranuclear palsy TDP-43 proteinopathy (PSP-TDP) and in about 5% of those with Lewy body dementia.[6][25] Hippocampal sclerosis occurs in about 23% of those with chronic traumatic encephalopathy; TP-43 proteinopathy accompanied 96% of those with hippocampal sclerosis.[26]
Acute brain injury
Hippocampal sclerosis may occur with hypoxic-ischemic injury, hypoglycemia, toxins (kainic acid, domoic acid), and viral human herpesvirus 6 limbic encephalitis.[3]:1506[27][28][29][30][31][32][33]
Notes
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 Blümcke et al. 2013.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 2.7 Malmgren & Thom 2012.
- ↑ 3.00 3.01 3.02 3.03 3.04 3.05 3.06 3.07 3.08 3.09 3.10 3.11 3.12 3.13 3.14 3.15 3.16 Nelson et al. 2019.
- ↑ 4.0 4.1 4.2 4.3 Thom 2009.
- ↑ Sommer 1880.
- ↑ 6.0 6.1 Yokota et al. 2010.
- ↑ 7.0 7.1 Neumann et al. 2009.
- ↑ Dickson et al. 1994.
- ↑ Neumann et al. 2006.
- ↑ 10.0 10.1 Love et al. 2015.
- ↑ Roy, Millen & Kapur 2020.
- ↑ 12.0 12.1 12.2 Salanova, Markand & Worth 2004.
- ↑ 13.0 13.1 13.2 Montine et al. 2012.
- ↑ Woodworth et al. 2021.
- ↑ Minoshima et al. 2022.
- ↑ 16.0 16.1 Varoglu et al. 2009.
- ↑ 17.0 17.1 Kadom, Tsuchida & Gaillard 2011.
- ↑ Kobayashi et al. 2001.
- ↑ 19.0 19.1 19.2 19.3 De Lanerolle & Lee 2005.
- ↑ Mewasingh, Chin & Scott 2020.
- ↑ Koseoglu et al. 2009.
- ↑ Kim et al. 2010.
- ↑ Lamberink et al. 2020.
- ↑ Josephs & Dickson 2007.
- ↑ Aoki et al. 2015.
- ↑ Nicks et al. 2023.
- ↑ Andersen & Skullerud 1999.
- ↑ Rees & Inder 2005.
- ↑ Teitelbaum et al. 1990.
- ↑ Ho et al. 2008.
- ↑ Hubele et al. 2012.
- ↑ Lefebvre & Robertson 2010.
- ↑ Lévesque & Avoli 2013.
References
- Andersen, Solveig Norheim; Skullerud, Kari (1999). "Hypoxic/ischaemic brain damage, especially pallidal lesions, in heroin addicts". Forensic Science International 102 (1): 51–59. doi:10.1016/s0379-0738(99)00040-7. PMID 10423852.
- Aoki, Naoya; Murray, Melissa E.; Ogaki, Kotaro; Fujioka, Shinsuke et al. (2015). "Hippocampal sclerosis in Lewy body disease is a TDP-43 proteinopathy similar to FTLD-TDP Type A" (in en). Acta Neuropathologica 129 (1): 53–64. doi:10.1007/s00401-014-1358-z. ISSN 1432-0533. PMID 25367383.
- Blümcke, Ingmar; Thom, Maria; Aronica, Eleonora; Armstrong, Dawna D. et al. (2013). "International consensus classification of hippocampal sclerosis in temporal lobe epilepsy: A Task Force report from the ILAE Commission on Diagnostic Methods". Epilepsia 54 (7): 1315–1329. doi:10.1111/epi.12220. PMID 23692496.
- De Lanerolle, N.C.; Lee, T.S. (2005). "New facets of the neuropathology and molecular profile of human temporal lobe epilepsy". Epilepsy Behav 7 (2): 190–203. doi:10.1016/j.yebeh.2005.06.003. PMID 16098816.
- Dickson, D. W.; Davies, P.; Bevona, C.; Van Hoeven, K. H. et al. (1994). "Hippocampal sclerosis: a common pathological feature of dementia in very old (≥80 years of age) humans". Acta Neuropathologica 88 (3): 212–221. doi:10.1007/BF00293396. PMID 7810292.
- Ho, Margaret S.; Weller, Narelle J.; Ives, F. Jay; Carne, Christine L. et al. (2008). "Prevalence of Structural Central Nervous System Abnormalities in Early-Onset Type 1 Diabetes Mellitus". The Journal of Pediatrics 153 (3): 385–390. doi:10.1016/j.jpeds.2008.03.005. PMID 18534238.
- Hubele, Fabrice; Bilger, Karin; Kremer, Stéphane; Imperiale, Alessio et al. (2012). "Sequential FDG PET and MRI Findings in a Case of Human Herpes Virus 6 Limbic Encephalitis". Clinical Nuclear Medicine 37 (7): 716–717. doi:10.1097/RLU.0b013e31824c5e2f. PMID 22691524.
- Josephs, Keith A.; Dickson, Dennis W. (2007). "Hippocampal sclerosis in tau-negative frontotemporal lobar degeneration". Neurobiology of Aging 28 (11): 1718–1722. doi:10.1016/j.neurobiolaging.2006.07.010. PMID 16930776.
- Kadom, N.; Tsuchida, T.; Gaillard, W.D. (2011). "Hippocampal sclerosis in children younger than 2 years". Pediatr Radiol 41 (10): 1239–1245. doi:10.1007/s00247-011-2166-4. PMID 21735179.
- Kim, C.H.; Koo, B.B.; Chung, C.K.; Lee, J.M. et al. (2010). "Thalamic changes in temporal lobe epilepsy with and without hippocampal sclerosis: A diffusion tensor imaging study". Epilepsy Res 90 (1): 21–27. doi:10.1016/j.eplepsyres.2010.03.002. PMID 20307957.
- Kobayashi, E.; Lopes-Cendes, I.; Guerreiro, C. A.; Sousa, S. C. et al. (2001). "Seizure outcome and hippocampal atrophy in familial mesial temporal lobe epilepsy". Neurology 56 (2): 166–172. doi:10.1212/wnl.56.2.166. ISSN 0028-3878. PMID 11160950. https://pubmed.ncbi.nlm.nih.gov/11160950/.
- Koseoglu, E.; Kucuk, S.; Arman, F.; Erosoy, A.O. (2009). "Factors that affect interictal cardiovascular autonomic dysfunction in temporal lobe epilepsy: Role of hippocampal sclerosis". Epilepsy Behav 16 (4): 617–621. doi:10.1016/j.yebeh.2009.09.021. PMID 19854109.
- Lamberink, Herm J; Otte, Willem M; Blümcke, Ingmar; Braun, Kees P J et al. (2020). "Seizure outcome and use of antiepileptic drugs after epilepsy surgery according to histopathological diagnosis: a retrospective multicentre cohort study". The Lancet Neurology 19 (9): 748–757. doi:10.1016/S1474-4422(20)30220-9. PMID 32822635. https://discovery.ucl.ac.uk/id/eprint/10110005/.
- Lefebvre, Kathi A.; Robertson, Alison (2010). "Domoic acid and human exposure risks: A review". Toxicon 56 (2): 218–230. doi:10.1016/j.toxicon.2009.05.034. PMID 19505488.
- Lévesque, Maxime; Avoli, Massimo (2013). "The kainic acid model of temporal lobe epilepsy". Neuroscience & Biobehavioral Reviews 37 (10): 2887–2899. doi:10.1016/j.neubiorev.2013.10.011. PMID 24184743.
- Love, Seth; Budka, Herbert; Ironside, James; Perry, Arie (2015). Greenfield's neuropathology : two volume set (Ninth ed.). Boca Raton. ISBN 978-1-4987-2905-5.
- Malmgren, Kristina; Thom, Maria (2012). "Hippocampal sclerosis-Origins and imaging: Hippocampal Sclerosis". Epilepsia 53: 19–33. doi:10.1111/j.1528-1167.2012.03610.x. PMID 22946718.
- Mewasingh, Leena D; Chin, Richard F M; Scott, Rod C (2020). "Current understanding of febrile seizures and their long-term outcomes". Developmental Medicine & Child Neurology 62 (11): 1245–1249. doi:10.1111/dmcn.14642. PMID 32748466.
- Minoshima, Satoshi; Cross, Donna; Thientunyakit, Tanyaluck; Foster, Norman L. et al. (2022). "18F-FDG PET Imaging in Neurodegenerative Dementing Disorders: Insights into Subtype Classification, Emerging Disease Categories, and Mixed Dementia with Copathologies". Journal of Nuclear Medicine 63 (Supplement 1): 2S–12S. doi:10.2967/jnumed.121.263194. PMID 35649653.
- Montine, Thomas J.; Phelps, Creighton H.; Beach, Thomas G.; Bigio, Eileen H. et al. (2012). "National Institute on Aging–Alzheimer's Association guidelines for the neuropathologic assessment of Alzheimer's disease: a practical approach". Acta Neuropathologica 123 (1): 1–11. doi:10.1007/s00401-011-0910-3. PMID 22101365.
- Nelson, P.T.; Schmitt, F.A.; Lin, Y.S.; Abner, E.L. et al. (2011). "Hippocampal sclerosis in advanced age: clinical and pathological features". Brain 134 (5): 1506–1518. doi:10.1093/brain/awr053. PMID 21596774.
- Nelson, Peter T; Dickson, Dennis W; Trojanowski, John Q; Jack, Clifford R et al. (2019). "Limbic-predominant age-related TDP-43 encephalopathy (LATE): consensus working group report". Brain 142 (6): 1503–1527. doi:10.1093/brain/awz099. PMID 31039256.
- Neumann, M.; Rademakers, R.; Roeber, S.; Baker, M. et al. (2009). "A new subtype of frontotemporal lobar degeneration with FUS pathology". Brain 132 (11): 2922–2931. doi:10.1093/brain/awp214. PMID 19674978.
- Neumann, Manuela; Sampathu, Deepak M.; Kwong, Linda K.; Truax, Adam C. et al. (2006). "Ubiquitinated TDP-43 in frontotemporal lobar degeneration and amyotrophic lateral sclerosis". Science 314 (5796): 130–133. doi:10.1126/science.1134108. ISSN 1095-9203. PMID 17023659. Bibcode: 2006Sci...314..130N. https://pubmed.ncbi.nlm.nih.gov/17023659.
- Nicks, Raymond; Clement, Nathan F.; Alvarez, Victor E.; Tripodis, Yorghos et al. (2023). "Repetitive head impacts and chronic traumatic encephalopathy are associated with TDP-43 inclusions and hippocampal sclerosis". Acta Neuropathologica 145 (4): 395–408. doi:10.1007/s00401-023-02539-3. PMID 36681782.
- Rees, Sandra; Inder, Terrie (2005). "Fetal and neonatal origins of altered brain development". Early Human Development 81 (9): 753–761. doi:10.1016/j.earlhumdev.2005.07.004. PMID 16107304.
- Roy, Achira; Millen, Kathleen J.; Kapur, Raj P. (2020). "Hippocampal granule cell dispersion: a non-specific finding in pediatric patients with no history of seizures". Acta Neuropathologica Communications 8 (1): 54. doi:10.1186/s40478-020-00928-3. PMID 32317027.
- Salanova, V.; Markand, O.; Worth, R. (2004). "Temporal lobe epilepsy: analysis of patients with dual pathology: Temporal lobe epilepsy surgery: dual pathology, outcome". Acta Neurologica Scandinavica 109 (2): 126–131. doi:10.1034/j.1600-0404.2003.00183.x. PMID 14705975.
- Shinnar, Shlomo (2003). "Febrile Seizures and Mesial Temporal Sclerosis" (in en). Epilepsy Currents 3 (4): 115–118. doi:10.1046/j.1535-7597.2003.03401.x. ISSN 1535-7597. PMID 15309049.
- Sommer, W. (1880). "Erkrankung des Ammon's horn als aetiologis ches moment der epilepsien". Arch Psychiatr Nurs 10 (3): 631–675. doi:10.1007/BF02224538. https://zenodo.org/record/1702037.
- Teitelbaum, Jeanne S.; Zatorre, Robert J.; Carpenter, Stirling; Gendron, Daniel et al. (1990). "Neurologic Sequelae of Domoic Acid Intoxication Due to the Ingestion of Contaminated Mussels". New England Journal of Medicine 322 (25): 1781–1787. doi:10.1056/NEJM199006213222505. PMID 1971710.
- Thom, Maria (2009). "Hippocampal Sclerosis:Progress Since Sommer" (in en). Brain Pathology 19 (4): 565–572. doi:10.1111/j.1750-3639.2008.00201.x. PMID 18761661.
- Varoglu, Asuman Orhan; Saygi, Serap; Acemoglu, Hamit; Ciger, Abdurrahman (2009). "Prognosis of patients with mesial temporal lobe epilepsy due to hippocampal sclerosis". Epilepsy Research 85 (2–3): 206–211. doi:10.1016/j.eplepsyres.2009.03.001. PMID 19345070.
- Woodworth, Davis C.; Nguyen, Hannah L.; Khan, Zainab; Kawas, Claudia H. et al. (2021). "Utility of MRI in the identification of hippocampal sclerosis of aging". Alzheimer's & Dementia 17 (5): 847–855. doi:10.1002/alz.12241. PMID 33615673.
- Yokota, Osamu; Davidson, Yvonne; Bigio, Eileen H.; Ishizu, Hideki et al. (2010). "Phosphorylated TDP-43 pathology and hippocampal sclerosis in progressive supranuclear palsy". Acta Neuropathologica 120 (1): 55–66. doi:10.1007/s00401-010-0702-1. PMID 20512649.
External links
| Classification |
|---|
 |

