Medicine:Hypercapnia
| Hypercapnia | |
|---|---|
| Other names | Hypercarbia, CO2 retention, carbon dioxide poisoning |
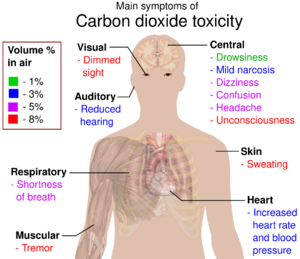 | |
| Main symptoms of carbon dioxide toxicity, by increasing volume percent in air.[1][2] | |
| Specialty | Pulmonology, critical care medicine |
Hypercapnia (from the Greek hyper = "above" or "too much" and kapnos = "smoke"), also known as hypercarbia and CO2 retention, is a condition of abnormally elevated carbon dioxide (CO2) levels in the blood. Carbon dioxide is a gaseous product of the body's metabolism and is normally expelled through the lungs. Carbon dioxide may accumulate in any condition that causes hypoventilation, a reduction of alveolar ventilation (the clearance of air from the small sacs of the lung where gas exchange takes place) as well as resulting from inhalation of CO2. Inability of the lungs to clear carbon dioxide, or inhalation of elevated levels of CO2, leads to respiratory acidosis. Eventually the body compensates for the raised acidity by retaining alkali in the kidneys, a process known as "metabolic compensation".
Acute hypercapnia is called acute hypercapnic respiratory failure (AHRF) and is a medical emergency as it generally occurs in the context of acute illness. Chronic hypercapnia, where metabolic compensation is usually present, may cause symptoms but is not generally an emergency. Depending on the scenario both forms of hypercapnia may be treated with medication, with mask-based non-invasive ventilation or with mechanical ventilation.
Hypercapnia is a hazard of underwater diving associated with breath-hold diving, scuba diving, particularly on rebreathers, and deep diving where it is associated with increased breathing gas density due to the high ambient pressure.[3][4][5]
Signs and symptoms
Hypercapnia may happen in the context of an underlying health condition, and symptoms may relate to this condition or directly to the hypercapnia. Specific symptoms attributable to early hypercapnia are dyspnea (breathlessness), headache, confusion and lethargy. Clinical signs include flushed skin, full pulse (bounding pulse), rapid breathing, premature heart beats, muscle twitches, and hand flaps (asterixis). The risk of dangerous irregularities of the heart beat is increased.[6][7] Hypercapnia also occurs when the breathing gas is contaminated with carbon dioxide, or respiratory gas exchange cannot keep up with the metabolic production of carbon dioxide, which can occur when gas density limits ventilation at high ambient pressures.[3]
In severe hypercapnia (generally greater than 10 kPa or 75 mmHg), symptomatology progresses to disorientation, panic, hyperventilation, convulsions, unconsciousness, and eventually death.[8][9]
Causes
Carbon dioxide is a normal metabolic product but it accumulates in the body if it is produced faster than it is cleared. During strenuous exercise the production rate of carbon dioxide can increase more than tenfold over the production rate during rest. Carbon dioxide is dissolved in the blood and elimination is by gas exchange in the lungs during breathing.[10] Hypercapnia is generally caused by hypoventilation, lung disease, or diminished consciousness. It may also be caused by exposure to environments containing abnormally high concentrations of carbon dioxide, such as from volcanic or geothermal activity, or by rebreathing exhaled carbon dioxide. In this situation the hypercapnia can also be accompanied by respiratory acidosis.[11]
Acute hypercapnic respiratory failure may occur in acute illness caused by chronic obstructive pulmonary disease (COPD), chest wall deformity, some forms of neuromuscular disease (such as myasthenia gravis, and obesity hypoventilation syndrome.[12] AHRF may also develop in any form of respiratory failure where the breathing muscles become exhausted, such as severe pneumonia and acute severe asthma. It can also be a consequence of profound suppression of consciousness such as opioid overdose.[citation needed]
During diving
Normal respiration in divers results in alveolar hypoventilation resulting in inadequate CO2 elimination or hypercapnia. Lanphier's work at the US Navy Experimental Diving Unit answered the question, "Why don't divers breathe enough?":[13]
- Higher inspired oxygen () at 4 atm (400 kPa) accounted for not more than 25% of the elevation in end tidal CO2 (ETCO2)[14] above values found at the same work rate when breathing air just below the surface.[15][16][17][4]
- Increased work of breathing accounted for most of the elevation of (alveolar gas equation) in exposures above 1 atm (100 kPa), as indicated by the results when helium was substituted for nitrogen at 4 atm (400 kPa).[15][16][17][4]
- Inadequate ventilatory response to exertion was indicated by the fact that, despite resting values in the normal range, rose markedly with exertion even when the divers breathed air at a depth of only a few feet.[15][16][17][4]
A variety of reasons exist for carbon dioxide not being expelled completely when the diver exhales:
- The diver is exhaling into an enclosed space that does not allow all the CO2 to escape to the environment, such as a long snorkel, full-face diving mask, or diving helmet, and the diver then re-inhales from that dead space.[4]
- The carbon dioxide scrubber in the diver's rebreather is failing to remove sufficient carbon dioxide from the loop (higher inspired CO2), the breathing gas is contaminated with CO2, or the non-return valves in the breathing circuit are malfunctioning.[3]
- The diver is overexercising, producing excess carbon dioxide due to elevated metabolic activity and respiratory gas exchange cannot keep up with the metabolic production of carbon dioxide.[3][18]
- Gas density limits ventilation at high ambient pressures. The density of the breathing gas is higher at depth, so the effort required to fully inhale and exhale increases, making breathing more difficult and less efficient (high work of breathing).[13][3][18] Higher gas density also causes gas mixing within the lung to be less efficient, thus increasing the effective dead space.[4][5]
- The diver is deliberately hypoventilating, known as "skip breathing".[5]
Skip breathing
Skip breathing is a controversial technique to conserve breathing gas when using open-circuit scuba, which consists of briefly holding one's breath between inhalation and exhalation (i.e., "skipping" a breath). It can lead to CO2 not being exhaled efficiently.[19] The risk of burst lung (pulmonary barotrauma of ascent) is increased if the breath is held while ascending. It is particularly counterproductive with a rebreather, where the act of breathing pumps the gas around the "loop", pushing carbon dioxide through the scrubber and mixing freshly injected oxygen.[5]
In closed-circuit rebreather diving, exhaled carbon dioxide must be removed from the breathing system, usually by a scrubber containing a solid chemical compound with a high affinity for CO2, such as soda lime. If not removed from the system, it may be reinhaled, causing an increase in the inhaled concentration.[20]
Under hyperbaric conditions, hypercapnia contributes to nitrogen narcosis and oxygen toxicity by causing cerebral vasodilation which increases the dosage of oxygen to the brain.[18]
Mechanism
Hypercapnia normally triggers a reflex which increases breathing and access to oxygen (O2), such as arousal and turning the head during sleep. A failure of this reflex can be fatal, for example as a contributory factor in sudden infant death syndrome.[21]
Hypercapnia can induce increased cardiac output, an elevation in arterial blood pressure (higher levels of carbon dioxide stimulate aortic and carotid chemoreceptors with afferents -CN IX and X- to medulla oblongata with following chrono- and ino-tropic effects),[clarification needed] and a propensity toward cardiac arrhythmias. Hypercapnia may increase pulmonary capillary resistance.[citation needed]
Physiological effects
A high arterial partial pressure of carbon dioxide () causes changes in brain activity that adversely affect both fine muscular control and reasoning. EEG changes denoting minor narcotic effects can be detected for expired gas end tidal partial pressure of carbon dioxide () increase from 40 torrs (0.053 atm) to approximately 50 torrs (0.066 atm). The diver does not necessarily notice these effects.[10]
Higher levels of have a stronger narcotic effect: Confusion and irrational behaviour may occur around 72 torrs (0.095 atm), and loss of consciousness around 90 torrs (0.12 atm). High triggers the fight or flight response, affects hormone levels and can cause anxiety, irritability and inappropriate or panic responses, which can be beyond the control of the subject, sometimes with little or no warning. Vasodilation is another effect, notably in the skin, where feelings of unpleasant heat are reported, and in the brain, where blood flow can increase by 50% at a of 50 torrs (0.066 atm), Intracranial pressure may rise, with a throbbing headache. If associated with a high the high delivery of oxygen to the brain may increase the risk of CNS oxygen toxicity at partial pressures usually considered acceptable.[10]
In many people a high causes a feeling of shortness of breath, but the lack of this symptom is no guarantee that the other effects are not occurring. A significant percentage of rebreather deaths have been associated with CO2 retention. The effects of high can take several minutes to hours to resolve once the cause has been removed.[10]
Diagnosis
Blood gas tests may be performed, typically by radial artery puncture, in the setting of acute breathing problems or other acute medical illness. Hypercapnia is generally defined as an arterial blood carbon dioxide level over 45 mmHg (6 kPa). Since carbon dioxide is in equilibrium with carbonic acid in the blood, hypercapnia drives serum pH down, resulting in respiratory acidosis. Clinically, the effect of hypercapnia on pH is estimated using the ratio of the arterial pressure of carbon dioxide to the concentration of bicarbonate ion, .[citation needed]
Tolerance
| %CO2 in inspired air |
Expected tolerance for useful activity on continued exposure to elevated CO2 | |
|---|---|---|
| Duration | Major limitation | |
| 0.03 | lifetime | atmosphere, year 1780[22] |
| 0.04 | lifetime | current atmosphere |
| 0.5 | lifetime | no detectable limitations (Note: refer to modern research in Carbon dioxide which shows measurable effects below 1%.) |
| 1.0 | lifetime | |
| 1.5 | > 1 month | mild respiratory stimulation |
| 2.0 | > 1 month | |
| 2.5 | > 1 month | |
| 3.0 | > 1 month | moderate respiratory stimulation |
| 3.5 | > 1 week | |
| 4.0 | > 1 week | moderate respiratory stimulation, exaggerated respiratory response to exercise |
| 4.5 | > 8 hours | |
| 5.0 | > 4 hours | prominent respiratory stimulus, exaggerated respiratory response to exercise |
| 5.5 | > 1 hours | |
| 6.0 | > 0.5 hours | prominent respiratory stimulus, exaggerated respiratory response to exercise, beginnings of mental confusion |
| 6.5 | > 0.25 hours | |
| 7.0 | > 0.1 hours | limitation by dyspnea and mental confusion |
CO2 toxicity in animal models
Tests performed on mongrel dogs showed the physiological effect of carbon dioxide on the body of the animal: after inhalation of a 50% CO2 and 50% air mixture, respiratory movement increased for about 2 minutes, and then, it decreased for 30 to 90 minutes. Hill and Flack showed that CO2 concentrations up to 35% have an exciting effect upon both circulation and respiration, but those beyond 35% are depressant upon them.[citation needed] The blood pressure (BP) decreased transiently during the increased respiratory movement and then rose again and maintained the original level for a while. The heart rate slowed slightly just after the gas mixture inhalation. It is believed that the initial BP depression with the decreased heart rate is due to the direct depressant effect of CO2 upon the heart and that the return of blood pressure to its original level was due to the rapid rise of . After 30–90 min, the respiratory center was depressed, and hypotension occurred gradually or suddenly from reduced cardiac output, leading to an apnea and eventually to circulatory arrest.
At higher concentrations of CO2, unconsciousness occurred almost instantaneously and respiratory movement ceased in 1 minute. After a few minutes of apnea, circulatory arrest was seen. These findings imply that the cause of death in breathing high concentrations of CO2 is not the hypoxia but the intoxication of carbon dioxide.[23]
Treatment
The treatment for acute hypercapnic respiratory failure depends on the underlying cause, but may include medications and mechanical respiratory support. In those without contraindications, non-invasive ventilation (NIV) is often used in preference to invasive mechanical ventilation.[12] In the past, the drug doxapram (a respiratory stimulant), was used for hypercapnia in acute exacerbation of chronic obstructive pulmonary disease but there is little evidence to support its use compared to NIV,[24] and it does not feature in recent professional guidelines.[12]
Very severe respiratory failure, in which hypercapnia may also be present, is often treated with extracorporeal membrane oxygenation (ECMO), in which oxygen is added to and carbon dioxide removed directly from the blood.[25]
A relatively novel modality is extracorporeal carbon dioxide removal (ECCO2R). This technique removes CO2 from the bloodstream and may reduce the time mechanical ventilation is required for those with AHRF; it requires smaller volumes of blood flow compared to ECMO.[25][26]
Terminology
Hypercapnia is the opposite of hypocapnia, the state of having abnormally reduced levels of carbon dioxide in the blood.
See also
- Medicine:Dead space (physiology) – Inhaled air not part of gas exchange
- Chemistry:Inert gas asphyxiation – Insufficient oxygen in breathed air
- Earth:Lake Nyos – Crater lake in the Northwest Region of Cameroon
- Biology:Ocean acidification – Decrease of pH levels in the ocean
- Medicine:Permissive hypercapnia – Hypercapnia in respiratory insufficiency
References
- ↑ Toxicity of Carbon Dioxide Gas Exposure, CO2 Poisoning Symptoms, Carbon Dioxide Exposure Limits, and Links to Toxic Gas Testing Procedures By Daniel Friedman – InspectAPedia
- ↑ Davidson, Clive. 7 February 2003. "Marine Notice: Carbon Dioxide: Health Hazard". Australian Maritime Safety Authority.
- ↑ 3.0 3.1 3.2 3.3 3.4 Anthony, Gavin; Mitchell, Simon J. (2016). "Respiratory Physiology of Rebreather Diving". in Pollock, NW; Sellers, SH; Godfrey, JM. Wrigley Marine Science Center, Catalina Island, CA. pp. 66–79. https://www.omao.noaa.gov/sites/default/files/documents/Rebreathers%20and%20Scientific%20Diving%20Proceedings%202016.pdf.
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 Lanphier EH (1956). "Nitrogen-Oxygen Mixture Physiology. Phase 5. Added Respiratory Dead Space (Value in Personnel Selection tests) (Physiological Effects Under Diving Conditions)". US Navy Experimental Diving Unit Technical Report AD0725851.
- ↑ 5.0 5.1 5.2 5.3 Mitchell, Simon (August 2008). "Four: Carbon Dioxide Retention". in Mount, Tom; Dituri, Joseph. Exploration and Mixed Gas Diving Encyclopedia (1st ed.). Miami Shores, Florida: International Association of Nitrox Divers. pp. 279–286. ISBN 978-0-915539-10-9.
- ↑ Stapczynski J. S, "Chapter 62. Respiratory Distress" (Chapter). Tintinalli JE, Kelen GD, Stapczynski JS, Ma OJ, Cline DM: Tintinalli's Emergency Medicine: A Comprehensive Study Guide, 6th Edition: "PageError". http://www.accessmedicine.com/content.aspx?aID=591330..
- ↑ Morgan GE Jr., Mikhail MS, Murray MJ, "Chapter 3. Breathing Systems" (Chapter). Morgan GE Jr., Mikhail MS, Murray MJ: Clinical Anesthesiology, 4th Edition: "AccessMedicine - Lange Anesthesiology: Key Concepts". http://www.accessmedicine.com/content.aspx?aID=886013..
- ↑ 8.0 8.1 Lambertsen, Christian J. (1971). "Carbon Dioxide Tolerance and Toxicity". Environmental Biomedical Stress Data Center, Institute for Environmental Medicine, University of Pennsylvania Medical Center IFEM Report No. 2–71.
- ↑ Glatte Jr H. A.; Motsay G. J.; Welch B.E. (1967). "Carbon Dioxide Tolerance Studies". Brooks AFB, TX School of Aerospace Medicine Technical Report SAM-TR-67-77.
- ↑ 10.0 10.1 10.2 10.3 Shykoff, Barbara; Warkander, Dan (28 February 2018). "What's All the Fuss about CO2 in Breathing Gas?". https://www.shearwater.com/monthly-blog-posts/whats-fuss-co2-breathing-gas/.
- ↑ Dement, Roth, Kryger, 'Principles & Practices of Sleep Medicine' 3rd edition, 2000, p. 887. [|permanent dead link|dead link}}]
- ↑ 12.0 12.1 12.2 Davidson, A Craig; Banham, Stephen; Elliott, Mark; Kennedy, Daniel; Gelder, Colin; Glossop, Alastair; Church, Alistair Colin; Creagh-Brown, Ben et al. (14 March 2016). "BTS/ICS guideline for the ventilatory management of acute hypercapnic respiratory failure in adults". Thorax 71 (Suppl 2): ii1–ii35. doi:10.1136/thoraxjnl-2015-208209. PMID 26976648.
- ↑ 13.0 13.1 US Navy Diving Manual, 6th revision. United States: US Naval Sea Systems Command. 2006. http://www.supsalv.org/00c3_publications.asp?destPage=00c3&pageID=3.9. Retrieved 2008-06-10.
- ↑ ETCO2 is defined as the level of carbon dioxide released at end of expiration
- ↑ 15.0 15.1 15.2 Lanphier, EH (1955). "Nitrogen-Oxygen Mixture Physiology, Phases 1 and 2". US Navy Experimental Diving Unit Technical Report AD0784151.
- ↑ 16.0 16.1 16.2 "Nitrogen-Oxygen Mixture Physiology – Phase 3. End-Tidal Gas Sampling System. Carbon Dioxide Regulation in Divers. Carbon Dioxide Sensitivity Tests". US Navy Experimental Diving Unit Technical Report AD0728247. 1956.
- ↑ 17.0 17.1 17.2 Lanphier EH (1958). "Nitrogen-oxygen mixture physiology. Phase 4. Carbon Dioxide sensitivity as a potential means of personnel selection. Phase 6. Carbon Dioxide regulation under diving conditions". US Navy Experimental Diving Unit Technical Report AD0206734.
- ↑ 18.0 18.1 18.2 Mitchell, Simon. "Respiratory failure in technical diving". DAN Southern Africa. https://www.youtube.com/watch?v=QBajM3xmOtc.
- ↑ Cheshire, William P; Ott, Michael C (2001). "Headache in Divers". Headache: The Journal of Head and Face Pain 41 (3): 235–247. doi:10.1046/j.1526-4610.2001.111006235.x. PMID 11264683. "Carbon dioxide can accumulate insidiously in the diver who intentionally holds the breath intermittently (skip breathing) in a mistaken attempt to conserve air".
- ↑ Richardson, Drew, ed (1996). "Proceedings of Rebreather Forum 2.0.". Diving Science and Technology Workshop.: 286.
- ↑ Kinney, Hannah C; Thach, Bradley T (2009). "The sudden infant death syndrome". The New England Journal of Medicine 361 (8): 795–805. doi:10.1056/NEJMra0803836. PMID 19692691.
- ↑ "Current & Historical Carbon Dioxide (CO2) Levels Graph". https://www.co2levels.org/.
- ↑ Permentier, Kris; Vercammen, Steven; Soetaert, Sylvia; Schellemans, Christian (4 April 2017). "Carbon dioxide poisoning: a literature review of an often forgotten cause of intoxication in the emergency department". International Journal of Emergency Medicine 10 (1): 14. doi:10.1186/s12245-017-0142-y. ISSN 1865-1372. PMID 28378268.
- ↑ Greenstone, M.; Lasserson, T.J. (2003). "Doxapram for ventilatory failure due to exacerbations of chronic obstructive pulmonary disease". The Cochrane Database of Systematic Reviews (1): CD000223. doi:10.1002/14651858.CD000223. PMID 12535393.
- ↑ 25.0 25.1 Pisani, Lara; Polastri, Massimiliano; Pacilli, Angela Maria Grazia; Nava, Stefano (2018). "Extracorporeal Lung Support for Hypercapnic Ventilatory Failure". Respiratory Care 63 (9): 1174–1179. doi:10.4187/respcare.06277. PMID 30166412.
- ↑ Morales-Quinteros, Luis; Del Sorbo, Lorenzo; Artigas, Antonio (2019). "Extracorporeal carbon dioxide removal for acute hypercapnic respiratory failure". Annals of Intensive Care 9 (1): 79. doi:10.1186/s13613-019-0551-6. PMID 31267300.
External links
| Classification |
|---|
 |
