Medicine:Pulmonary edema
| Pulmonary edema | |
|---|---|
| Other names | Pulmonary oedema |
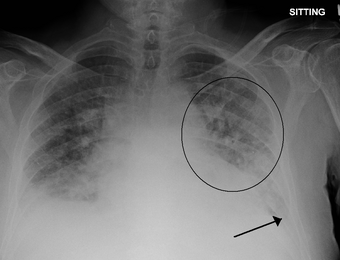 | |
| Pulmonary edema with small pleural effusions on both sides | |
| Specialty | Cardiology, critical care medicine pulmonology |
| Symptoms | Progressive dyspnea, cough, fever, cyanosis, tachycardia |
| Complications | ARDS, respiratory failure |
| Causes | Cardiogenic, Noncardiogenic (pneumonia, inhalation injury, sepsis, airway obstruction, high altitude) |
| Diagnostic method | Medical imaging, lab tests, ECG, echocardiography |
| Treatment | Supplemental oxygen, diuretics, treat underlying disease process |
Pulmonary edema, also known as pulmonary congestion, is excessive fluid accumulation in the tissue or air spaces (usually alveoli) of the lungs.[1] This leads to impaired gas exchange, most often leading to dyspnea (difficulty breathing) which can progress to hypoxemia and respiratory failure. Pulmonary edema has multiple causes and is traditionally classified as cardiogenic (caused by the heart) or noncardiogenic (all other types not caused by the heart).[2][3]
Various laboratory tests (CBC, troponin, BNP, etc.) and imaging studies (chest x-ray, CT scan, ultrasound) are often used to diagnosis and classify the cause of pulmonary edema.[4][5][6] Treatment is focused on three aspects: firstly improving respiratory function, secondly, treating the underlying cause, and thirdly preventing further damage and assuring full recovery to the lung. Pulmonary edema can cause permanent organ damage, and when sudden (acute) can lead to respiratory failure or cardiac arrest due to hypoxia.[7] The term edema is from the Greek οἴδημα (oidēma, "swelling"), from οἰδέω (oidéō, "(I) swell").[8][9]
Pathophysiology
The amount of fluid in the lungs is governed by multiple forces and is visualized using the Starling equation. There are two hydrostatic pressures (fluid) pressures and two oncotic (protein) pressures that determine the fluid movement within the lung air spaces (alveoli). Of the forces that explain fluid movement, only the pulmonary wedge pressure is obtainable via pulmonary artery catheterization.[10] Due to the complication rate associated with pulmonary artery catheterization, other imaging modalities and diagnostic methods have become more popular.[11] Imbalance in any of these forces can cause fluid movement (or lack of movement) causing to a buildup of fluid where it should not normally be. Although rarely clinically measured, these forces allow us to classify, and subsequently treat the underlying cause of pulmonary edema.
Classification
Pulmonary edema has a multitude of causes, and is typically classified as cardiogenic or noncardiogenic. As discussed above, cardiogenic pulmonary edema is caused by increased hydrostatic pressure causing increased fluid in the pulmonary interstitium and alveoli. Noncardiogenic causes are associated with the oncotic pressure as discussed above causing malfunctioning barriers in the lungs (increased microvascular permeability).[12]
Cardiogenic
Cardiogenic pulmonary edema is typically caused by either volume overload or impaired left ventricular function. As a result, pulmonary pressures rises from the normal average of 15 mmHg.[13] As the pulmonary pressure rises, these pressures overwhelm the barriers and fluid enters the alveoli when the pressure is above 25 mmHg.[14] Depending whether the cause is acute (quick) or chronic (happening over time), determines how fast pulmonary edema develops and the severity of symptoms.[12] Some of the common causes of cardiogenic pulmonary edema include:
- Acute exacerbation of congestive heart failure which is due to the heart's inability to pump the blood out of the pulmonary circulation at a sufficient rate resulting in elevation in pulmonary wedge pressure and edema. Acute exacerbations of heart failure can be due to many causes including but not limited to: arrhythmias, fluid overload, (e.g. from kidney failure or intravenous therapy), or myocardial infarction.
- Pericardial tamponade as well as treating pericardial tamponade via pericardiocentesis has shown to cause pulmonary edema as a result of increased left-sided heart strain.[15]
- Heart Valve Dysfunction such as mitral valve regurgitation can cause increased pressure and energy on the left side of the heart (increased pulmonary wedge pressure) causing pulmonary edema.[16]
- Hypertensive crisis can cause pulmonary edema as the elevation in blood pressure and increased afterload on the left ventricle hinders forward flow in blood vessels and causes the elevation in wedge pressure and subsequent pulmonary edema. In a recent systematic review, it was found that pulmonary edema was the second most common condition associated with hypertensive crisis after ischemic stroke.[17]
Noncardiogenic
Noncardiogenic pulmonary edema is caused by increased microvascular permeability (increased oncotic pressure) leading to increased fluid transfer into the alveolar spaces. The pulmonary artery wedge pressure is typically normal as opposed to cardiogenic pulmonary edema where the elevated pressure is causing the fluid transfer. There are multiple causes of noncardiogenic edema with multiple subtypes within each cause. Acute respiratory distress syndrome (ARDS) is a type of respiratory failure characterized by rapid onset of widespread inflammation in the lungs. Although ARDS can present with pulmonary edema (fluid accumulation), it is a distinct clinical syndrome that is not synonymous with pulmonary edema.
Direct Lung Injury
Acute lung injury may cause pulmonary edema directly through injury to the vasculature and parenchyma of the lung, causes include:
- Inhalation of hot or toxic gases[12] (including vaping-associated lung injury)
- Pulmonary contusion, i.e., high-energy trauma (e.g. vehicle accidents)
- Aspiration, e.g., gastric fluid
- Reexpansion, i.e. post large volume thoracocentesis, resolution of pneumothorax, post decortication, removal of endobronchial obstruction, effectively a form of negative pressure pulmonary oedema.
- Reperfusion injury, i.e., postpulmonary thromboendartectomy or lung transplantation
- Swimming induced pulmonary edema also known as immersion pulmonary edema[18][19][20]
- Transfusion associated Acute Lung Injury is a specific type of blood-product transfusion injury that occurs when the donors plasma contained antibodies against the recipient, such as anti-HLA or anti-neutrophil antibodies.[21]
- Negative pressure pulmonary edema[22] is when inspiration is attempted against some sort of obstruction in the upper airway, most commonly happens as a result of laryngospasm in adults. This negative pressure in the chest ruptures capillaries and floods the alveoli with blood[23]
- Pulmonary embolism[24]
Indirect Lung Injury
- Neurogenic causes[25] (seizures, head trauma, strangulation, electrocution).
- Transfusion Associated Circulatory Overload occurs when multiple blood transfusions or blood-products (plasma, platelets, etc.) are transfused over a short period of time.[26]
- It includes acute lung injury and acute respiratory distress syndrome.[27] (ALI-ARDS) cover many of these causes, Sepsis- Severe infection or inflammation which may be local or systemic. This is the classical form of acute lung injury-adult respiratory distress syndrome
- Pancreatitis
Special Causes
Some causes of pulmonary edema are less well characterized and arguably represent specific instances of the broader classifications above.
- Arteriovenous malformation
- Hantavirus pulmonary syndrome
- High altitude pulmonary edema (HAPE)[28][29]
- Envenomation, such as with the venom of Atrax robustus[30]
Signs and symptoms
The most common symptom of pulmonary edema is difficulty breathing (dyspnea) and may include other symptoms relating to inadequate oxygen (hypoxia) such as fast breathing (tachypnea), fast heart rate (tachycardia) and cyanosis. Other common symptoms include coughing up blood (classically seen as pink or red, frothy sputum), excessive sweating, anxiety, and pale skin. Other signs include end-inspiratory crackles (crackling sounds heard at the end of a deep breath) on auscultation and the presence of a third heart sound.[3]
Shortness of breath can manifest as orthopnea (inability to breathe sufficiently when lying down flat due to breathlessness) and/or paroxysmal nocturnal dyspnea (episodes of severe sudden breathlessness at night). These are common presenting symptoms of chronic and cardiogenic pulmonary edema due to left ventricular failure.
The development of pulmonary edema may be associated with symptoms and signs of "fluid overload" in the lungs; this is a non-specific term to describe the manifestations of right ventricular failure on the rest of the body. These symptoms may include peripheral edema (swelling of the legs, in general, of the "pitting" variety, wherein the skin is slow to return to normal when pressed upon due to fluid), raised jugular venous pressure and hepatomegaly, where the liver is excessively enlarged and may be tender or even pulsatile.
Additional symptoms such as fever, low blood pressure, injuries or burns may be present and can help further characterize the cause and subsequent treatment strategies.
Flash pulmonary edema
Flash pulmonary edema (FPE) is the name given to a clinical syndrome of acute heart failure that begins suddenly and accelerates rapidly. Frequently the most noticeable abnormality is edema of the lungs. Nevertheless it is a cardiovascular disease not a pulmonary disease. It is also known by other appellations including sympathetic crashing pulmonary edema.[31] It is often associated with severe hypertension[32] but may be precipitated by acute myocardial infarction or mitral regurgitation, but can be also caused by aortic regurgitation, heart failure, or almost any cause leading to elevated left ventricular filling pressures. Treatment of FPE should be directed at the underlying cause, but the mainstays are nitroglycerin, ensuring adequate oxygenation with non-invasive ventilation, and decrease of pulmonary circulation pressures while FPE stays.[33]
Recurrence of FPE is thought to be associated with hypertension[34] and may signify renal artery stenosis.[35] Prevention of recurrence is based on managing or preventing hypertension, coronary artery disease, renovascular hypertension, and heart failure.
Diagnosis
There is no single test for confirming that breathlessness is caused by pulmonary edema – there are many causes of shortness of breath; but there are methods to suggest a high probability of an edema.
Lab Tests
Low oxygen saturation in blood and disturbed arterial blood gas readings support the proposed diagnosis by suggesting a pulmonary shunt. Blood tests are performed for electrolytes (sodium, potassium) and markers of renal function (creatinine, urea). Elevated creatine levels may suggest a cardiogenic cause of pulmonary edema.[12] Liver enzymes, inflammatory markers (usually C-reactive protein) and a complete blood count as well as coagulation studies (PT, aPTT) are also typically requested as further diagnosis. Elevated white blood cell count (WBC) may suggest a non-cardiogenic cause such as sepsis or infection.[12] B-type natriuretic peptide (BNP) is available in many hospitals, sometimes even as a point-of-care test. Low levels of BNP (<100 pg/ml) suggest a cardiac cause is unlikely, and suggest noncardiogenic pulmonary edema.[3]
Imaging Tests
Chest X-ray has been used for many years to diagnose pulmonary edema due to its wide availability and relatively cheap cost.[4] A chest X-ray will show fluid in the alveolar walls, Kerley B lines, increased vascular shadowing in a classical batwing peri-hilum pattern, upper lobe diversion (biased blood flow to the superior parts instead of inferior parts of the lung), and possibly pleural effusions. In contrast, patchy alveolar infiltrates are more typically associated with noncardiogenic edema.[3]
Lung ultrasounds, employed by a healthcare provider at the point of care, is also a useful tool to diagnose pulmonary edema; not only is it accurate, but it may quantify the degree of lung water, track changes over time, and differentiate between cardiogenic and non-cardiogenic edema.[36] Lung ultrasound is recommended as the first-line method due to its wide availability, ability to be performed bedside, and wide diagnostic utility for other similar diseases.[4]
Especially in the case of cardiogenic pulmonary edema, urgent echocardiography may strengthen the diagnosis by demonstrating impaired left ventricular function, high central venous pressures and high pulmonary artery pressures leading to pulmonary edema.
Prevention
In those with underlying heart or lung disease, effective control of congestive and respiratory symptoms helps prevents pulmonary edema.[37]
Dexamethasone is in widespread use for the prevention of high altitude pulmonary edema. Sildenafil is used as a preventive treatment for altitude-induced pulmonary edema and pulmonary hypertension,[38][39] the mechanism of action is via phosphodiesterase inhibition which raises cGMP, resulting in pulmonary arterial vasodilation and inhibition of smooth muscle cell proliferation and indirectly fluid formation in the lungs.[40] While this effect has only recently been discovered, sildenafil is already becoming an accepted treatment for this condition, in particular in situations where the standard treatment of rapid descent (acclimatization) has been delayed for some reason.[41]
Management
The initial management of pulmonary edema, irrespective of the type or cause, is supporting vital functions while edema lasts. Hypoxia (abnormally low oxygen levels) may require supplementary oxygen to balance blood oxygen levels, but if this is insufficient then again mechanical ventilation may be required to prevent complications caused by hypoxia.[42] Therefore, if the level of consciousness is decreased it may be required to proceed to tracheal intubation and mechanical ventilation to prevent airway compromise. Treatment of the underlying cause is the next priority; pulmonary edema secondary to infection, for instance, would require the administration of appropriate antibiotics or antivirals.[2][3]
Cardiogenic pulmonary edema
Acute cardiogenic pulmonary edema often responds rapidly to medical treatment.[43] Positioning upright may relieve symptoms. A loop diuretic such as furosemide (or Lasix®) is administered, often together with morphine to reduce respiratory distress.[43] Both diuretic and morphine may have vasodilator effects, but specific vasodilators may be used (particularly intravenous glyceryl trinitrate or ISDN) provided the blood pressure is adequate.[43]
Continuous positive airway pressure and bilevel positive airway pressure (CPAP/BiPAP) has been demonstrated to reduce mortality and the need of mechanical ventilation in people with severe cardiogenic pulmonary edema.[44]
It is possible for cardiogenic pulmonary edema to occur together with cardiogenic shock, in which the cardiac output is insufficient to sustain an adequate blood pressure to the lungs. This can be treated with inotropic agents or by intra-aortic balloon pump, but this is regarded as temporary treatment while the underlying cause is addressed and the lungs recover.[43]
Prognosis
As pulmonary edema has a wide variety of causes and presentations, the outcome or prognosis is often disease-dependent and more accurately described in relation to the associated syndrome. It is a major health problem, with one large review stating an incidence of 7.6% with an associated in hospital mortality rate of 11.9%.[45] Generally, pulmonary edema is associated with a poor prognosis with a 50% survival rate at one year, and 85% mortality at six years.[46]
References
- ↑ Dorland's illustrated medical dictionary (32nd ed.). Saunders/Elsevier. 2 May 2011. p. 593. ISBN 978-1-4160-6257-8.
- ↑ 2.0 2.1 "Assessment of Pulmonary Edema: Principles and Practice". Journal of Cardiothoracic and Vascular Anesthesia 32 (2): 901–914. April 2018. doi:10.1053/j.jvca.2017.08.028. PMID 29174750. https://eprints.gla.ac.uk/155147/1/155147.pdf.
- ↑ 3.0 3.1 3.2 3.3 3.4 "Clinical practice. Acute pulmonary edema". The New England Journal of Medicine 353 (26): 2788–2796. December 2005. doi:10.1056/NEJMcp052699. PMID 16382065.
- ↑ 4.0 4.1 4.2 "Noninvasive Imaging Methods for Quantification of Pulmonary Edema and Congestion: A Systematic Review". JACC. Cardiovascular Imaging 16 (11): 1469–1484. November 2023. doi:10.1016/j.jcmg.2023.06.023. PMID 37632500.
- ↑ "Prevalence, in-hospital mortality, and factors related to neurogenic pulmonary edema after spontaneous subarachnoid hemorrhage: a systematic review and meta-analysis". Neurosurgical Review 46 (1): 169. July 2023. doi:10.1007/s10143-023-02081-6. PMID 37432487.
- ↑ "A systematic review of diagnostic methods to differentiate acute lung injury/acute respiratory distress syndrome from cardiogenic pulmonary edema". Critical Care 21 (1): 228. August 2017. doi:10.1186/s13054-017-1809-8. PMID 28841896.
- ↑ "Clinical Outcomes in Hypertensive Emergency: A Systematic Review and Meta-Analysis". Journal of the American Heart Association 12 (14): e029355. July 2023. doi:10.1161/JAHA.122.029355. PMID 37421281.
- ↑ οἴδημα, οἰδέω. Liddell, Henry George; Scott, Robert; A Greek–English Lexicon at the Perseus Project.
- ↑ Harper, Douglas. "edema". Online Etymology Dictionary. https://www.etymonline.com/?term=edema.
- ↑ "ACCF/SCAI/AATS/AHA/ASE/ASNC/HFSA/HRS/SCCM/SCCT/SCMR/STS 2012 appropriate use criteria for diagnostic catheterization: a report of the American College of Cardiology Foundation Appropriate Use Criteria Task Force, Society for Cardiovascular Angiography and Interventions, American Association for Thoracic Surgery, American Heart Association, American Society of Echocardiography, American Society of Nuclear Cardiology, Heart Failure Society of America, Heart Rhythm Society, Society of Critical Care Medicine, Society of Cardiovascular Computed Tomography, Society for Cardiovascular Magnetic Resonance, and Society of Thoracic Surgeons". Journal of the American College of Cardiology 59 (22): 1995–2027. May 2012. doi:10.1016/j.jacc.2012.03.003. PMID 22578925.
- ↑ "Pulmonary artery catheters for adult patients in intensive care". The Cochrane Database of Systematic Reviews 2013 (2): CD003408. February 2013. doi:10.1002/14651858.CD003408.pub3. PMID 23450539.
- ↑ 12.0 12.1 12.2 12.3 12.4 Textbook of critical care (8th ed.). Amsterdam: Elsevier. 2024. ISBN 978-0-323-75929-8.
- ↑ What Is Pulmonary Hypertension? From Diseases and Conditions Index (DCI). National Heart, Lung, and Blood Institute. Last updated September 2008. Retrieved on 6 April 2009.
- ↑ Cardiology secrets (2nd ed.). Elsevier Health Sciences. 2001. Chapter 41, page 210. ISBN 1-56053-420-6. https://books.google.com/books?id=IYFAsxAUA_MC.
- ↑ "Pericardial tamponade: A comprehensive emergency medicine and echocardiography review". The American Journal of Emergency Medicine 58: 159–174. August 2022. doi:10.1016/j.ajem.2022.05.001. PMID 35696801.
- ↑ "The vital role of the right ventricle in the pathogenesis of acute pulmonary edema". The American Journal of Cardiology 115 (7): 992–1000. April 2015. doi:10.1016/j.amjcard.2015.01.026. PMID 25697920.
- ↑ "Clinical Outcomes in Hypertensive Emergency: A Systematic Review and Meta-Analysis". Journal of the American Heart Association 12 (14): e029355. July 2023. doi:10.1161/JAHA.122.029355. PMID 37421281.
- ↑ "Pulmonary edema of scuba divers". Undersea & Hyperbaric Medicine 24 (1): 29–33. 1997. PMID 9068153. http://archive.rubicon-foundation.org/2388. Retrieved 2008-09-04.
- ↑ "Pulmonary edema in scuba divers: recurrence and fatal outcome". Undersea & Hyperbaric Medicine 32 (1): 39–44. 2005. PMID 15796313. http://archive.rubicon-foundation.org/4032. Retrieved 2008-09-04.
- ↑ "A literature review of immersion pulmonary edema". The Physician and Sportsmedicine 47 (2): 148–151. May 2019. doi:10.1080/00913847.2018.1546104. PMID 30403902.
- ↑ "Transfusion-related acute lung injury (TRALI)". Professional Education. 2016-06-17. https://professionaleducation.blood.ca/en/transfusion/publications/transfusion-related-acute-lung-injury-trali.
- ↑ "Negative-pressure acute tracheobronchial hemorrhage and pulmonary edema". Journal of Anesthesia 23 (3): 417–420. 2009. doi:10.1007/s00540-009-0757-0. PMID 19685125.
- ↑ Hines, Roberta L. and Marschall, Katherine. Stoelting's Anesthesia and Co-Existing Disease. 6th edition. 2012. pages 178 and 179.
- ↑ "Pulmonary edema". 2018-08-08. https://www.mayoclinic.org/diseases-conditions/pulmonary-edema/symptoms-causes/syc-20377009.
- ↑ "Neurogenic pulmonary oedema". Continuing Education in Anaesthesia, Critical Care & Pain 11 (3): 87–92. 2011. doi:10.1093/BJACEACCP/MKR006.
- ↑ "Adverse Reactions". Professional Education. 2016-06-02. https://professionaleducation.blood.ca/en/transfusion/clinical-guide/adverse-reactions.
- ↑ "Pharmacological treatments in ARDS; a state-of-the-art update". BMC Medicine 11: 166. August 2013. doi:10.1186/1741-7015-11-166. PMID 23957905.
- ↑ "Do we have a "best practice" for treating high altitude pulmonary edema?". High Altitude Medicine & Biology 9 (2): 111–114. 2008. doi:10.1089/ham.2008.1017. PMID 18578641.
- ↑ Bates, M (2007). "High altitude pulmonary edema". Altitude Physiology Expeditions. http://www.altitude.org/altitude_sickness.php#HAPE.
- ↑ White J, Gray M, Fisher M (1989). Atrax Robustus IPCS InChem
- ↑ "High-dose versus low-dose intravenous nitroglycerine for sympathetic crashing acute pulmonary edema: a randomised controlled trial". Emergency Medicine Journal 41 (2): 96–102. January 2024. doi:10.1136/emermed-2023-213285. PMID 38050078.
- ↑ "The pathogenesis of acute pulmonary edema associated with hypertension". The New England Journal of Medicine 344 (1): 17–22. January 2001. doi:10.1056/NEJM200101043440103. PMID 11136955.
- ↑ "Management of Heart Failure in the Emergency Department Setting: An Evidence-Based Review of the Literature". The Journal of Emergency Medicine 55 (5): 635–646. November 2018. doi:10.1016/j.jemermed.2018.08.002. PMID 30266198.
- ↑ "Flash pulmonary edema: association with hypertension and reoccurrence despite coronary revascularization". American Heart Journal 140 (3): 451–455. September 2000. doi:10.1067/mhj.2000.108828. PMID 10966547.
- ↑ "Recurrent pulmonary oedema in hypertension due to bilateral renal artery stenosis: treatment by angioplasty or surgical revascularisation". Lancet 2 (8610): 551–552. September 1988. doi:10.1016/S0140-6736(88)92668-2. PMID 2900930.
- ↑ "International evidence-based recommendations for point-of-care lung ultrasound". Intensive Care Medicine 38 (4): 577–591. April 2012. doi:10.1007/s00134-012-2513-4. PMID 22392031.
- ↑ "PLEURAL EFFUSIONS | Overview" (in en). Encyclopedia of Respiratory Medicine. Oxford: Academic Press. 2006-01-01. pp. 353–358. doi:10.1016/b0-12-370879-6/00299-4. ISBN 978-0-12-370879-3.
- ↑ "Sildenafil inhibits altitude-induced hypoxemia and pulmonary hypertension". American Journal of Respiratory and Critical Care Medicine 171 (3): 275–281. February 2005. doi:10.1164/rccm.200406-804OC. PMID 15516532.
- ↑ "Sildenafil for the treatment of altitude-induced hypoxaemia". Expert Opinion on Pharmacotherapy 6 (5): 835–837. May 2005. doi:10.1517/14656566.6.5.835. PMID 15934909.
- ↑ Clark, Michael; Kumar, Parveen J. (2009). Kumar and Clark's clinical medicine. St. Louis, Mo: Elsevier Saunders. p. 783. ISBN 978-0-7020-2993-6.
- ↑ "Treatment of high altitude pulmonary edema at 4240 m in Nepal". High Altitude Medicine & Biology 8 (2): 139–146. 2007. doi:10.1089/ham.2007.3055. PMID 17584008.
- ↑ "Supporting oxygenation in acute respiratory failure". Respiratory Care 58 (1): 142–150. January 2013. doi:10.4187/respcare.02087. PMID 23271824.
- ↑ 43.0 43.1 43.2 43.3 "Acute heart failure: focusing on acute cardiogenic pulmonary oedema". Clinical Medicine 10 (1): 59–64. February 2010. doi:10.7861/clinmedicine.10-1-59. PMID 20408310.
- ↑ "Non-invasive positive pressure ventilation (CPAP or bilevel NPPV) for cardiogenic pulmonary oedema". The Cochrane Database of Systematic Reviews 2019 (4): CD005351. April 2019. doi:10.1002/14651858.CD005351.pub4. PMID 30950507.
- ↑ "Assessment of Pulmonary Edema: Principles and Practice". Journal of Cardiothoracic and Vascular Anesthesia 32 (2): 901–914. April 2018. doi:10.1053/j.jvca.2017.08.028. PMID 29174750. https://eprints.gla.ac.uk/155147/1/155147.pdf.
- ↑ "Cardiogenic Pulmonary Edema in Emergency Medicine". Advances in Respiratory Medicine 91 (5): 445–463. October 2023. doi:10.3390/arm91050034. PMID 37887077.
| Classification | |
|---|---|
| External resources |
 |




