Medicine:Cerebral amyloid angiopathy
| Cerebral amyloid angiopathy | |
|---|---|
| Other names | Congophilic angiopathy[1] |
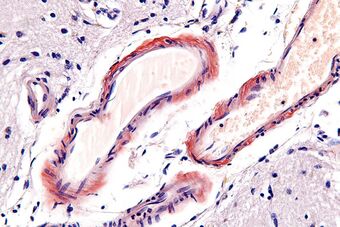 | |
| Micrograph of cerebral amyloid angiopathy using congo red stain | |
| Causes | Cause of CAA is unknown[2] |
| Diagnostic method | PET scan, CT scan[2] |
| Treatment | Management can be physical, occupational, or speech therapy.[2] |
Cerebral amyloid angiopathy (CAA) is a form of angiopathy in which amyloid beta peptide deposits in the walls of small to medium blood vessels of the central nervous system and meninges.[2][3] The term congophilic is sometimes used because the presence of the abnormal aggregations of amyloid can be demonstrated by microscopic examination of brain tissue after staining with Congo red. The amyloid material is only found in the brain and as such the disease is not related to other forms of amyloidosis.[4]
Signs and symptoms
CAA is associated with brain hemorrhages, particularly microhemorrhages. The accumulation of amyloid beta peptide deposits in the blood vessel walls results in damage of the blood vessels and hindrance of normal blood flow, making blood vessels more prone to bleeding [5] Since CAA can be caused by the same amyloid protein that is associated with Alzheimer's dementia, brain bleeds[6] are more common in people who have a diagnosis of Alzheimer's disease. However, they can also occur in those who have no history of dementia. The bleeding within the brain is usually confined to a particular lobe[7] and this is slightly different compared to brain bleeds which occur as a consequence of high blood pressure (hypertension) – a more common cause of a hemorrhagic stroke (or bleeding in the brain).[8] The location of the cerebral microbleed determines whether it is more likely to have been caused by hypertension or CAA. Tsai et al. conducted amyloid PET imaging in an Asian population with cerebral amyloid angiopathy–intracerebral hemorrhage and noticed that superficial cerebellar microbleeds are related to CAA, whereas deep or mixed-location cerebellar microbleeds are more likely related to hypertension.[9]
Causes
CAA has been identified as occurring either sporadically (generally in elderly populations)[10] or in familial forms such as Flemish, Iowa, and Dutch types. In all cases, it is defined by the deposition of amyloid beta (Aβ) in the leptomeningeal and cerebral vessel walls.[11] CAA occurring in the Flemish type has been observed to be linked to large dense-core plaques observed in this pedigree.[12]
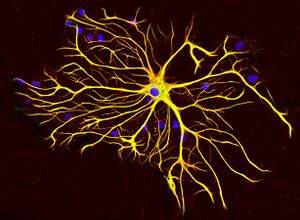
The reason for increased deposition of Aβ in sporadic CAA is still unclear with both increased production of the peptide and abnormal clearance having been proposed as potential causes.[13] Under normal physiology Aβ is cleared from the brain by four pathways: (1) endocytosis by astrocytes and microglial cells, (2) enzymatic degradation by neprilysin or insulysin (3) cleared by way of the blood–brain barrier or (4) drained along periarterial spaces. Abnormalities in each of these identified clearance pathways have been linked to CAA.[14][15]
In familial forms of CAA, the cause of Aβ build up is likely due to increased production rather than poor clearance.[16] Mutations in the amyloid precursor protein (APP), Presenilin (PS) 1 and PS2 genes can result in increased rates of cleavage of the APP into Aβ. An immune mechanism has also been proposed.[17][18] apolipoprotein E (APOE) ε2 and ε4 are associated with increased risk of getting cerebral amyloid antipathy. The use of antiplatelet and anticoagulant therapy increases the risk of getting intracerebral haemorrhage in CAA.[19]
Types
Several familial variants exist.[20] The condition is usually associated with amyloid beta.[21] However, there are types involving other amyloid peptides:
- the "Icelandic type" is associated with cystatin C amyloid (ACys).[22]
- the "British type" and "Danish type" are associated with British amyloid (ABri) and Danish amyloid (ADan) respectively. Both peptides are linked to mutations in ITM2B.[23]
- Familial amyloidosis-Finnish type is associated with gelsolin amyloid (AGel).[24]
Pathophysiology
The vascular amyloid pathology characteristic of CAA can be classified as either Type 1 or Type 2, the latter type being the more common. Type 1 CAA pathology entails detectable amyloid deposits within cortical capillaries as well as within the leptomeningeal and cortical arteries and arterioles. In type 2 CAA pathology, amyloid deposits are present in leptomeningeal and cortical arteries and arterioles, but not in capillaries. Deposits in veins or venules are possible in either type but are far less prevalent.[25]
Diagnosis
CAA can only be definitively diagnosed by a post-mortem autopsy.[27] Biopsies can play a role in diagnosing probable cases.[28] When no tissue is available for biopsy, the Boston Criteria are used to determine probable CAA cases from MRI or CT scan data. The Boston Criteria require evidence of multiple lobar or cortical hemorrhages to label a patient as probably having CAA.[27] Susceptibility weighted imaging has been proposed as a tool for identifying CAA-related microhemorrhages.[29]
Imaging
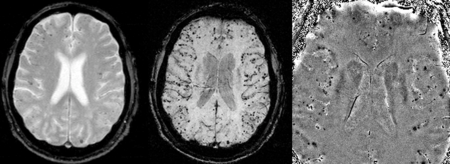
Cerebral amyloid angiopathy can be presented with lobar intracerebral hemorrhage or microbleeds in the brain. The bleeding usually occurs on the surfaces of the brain in contrast with intracranial haemorrhage due to high blood pressure which occurs in deep locations of the brain such as basal ganglia and pons. In lobar intracerebral bleed, computed tomography (CT) scan would show hyperdense haemorrhage area and hypodense odema around the haemorrhagic site.[19]
MRI sequence of gradient echo and susceptibility weighted imaging (SWI) are useful in detecting microbleeds and deposition of iron on the brain cortex (cortical superficial siderosis).[19] Other MRI indicators of CAA include white matter hyperintensities and cortical thinning.[30]
Management
The aim in cerebral amyloid angiopathy is to treat the symptoms, as there is no current cure. Physical, occupational and/or speech therapy may be helpful in the management of this condition.[2]
History
Gustav Oppenheim was the first to report vascular amyloid β deposits on the vasculature of the central nervous system in 1909. The first paper focusing solely on what would come to be known as CAA was published in 1938 by WZ Scholz. In 1979, H. Okazaki published a paper implicating CAA in certain cases of lobar intracerebral hemorrhage.[24] The Boston Criteria for CAA originated in a 1995 paper from Harvard Medical School.[27]
References
- ↑ "Severe cerebral congophilic angiopathy coincident with increased brain aluminium in a resident of Camelford, Cornwall, UK". J. Neurol. Neurosurg. Psychiatry 77 (7): 877–9. July 2006. doi:10.1136/jnnp.2005.086553. PMID 16627535.
- ↑ 2.0 2.1 2.2 2.3 2.4 "Cerebral amyloid angiopathy: MedlinePlus Medical Encyclopedia". https://www.nlm.nih.gov/medlineplus/ency/article/000719.htm.
- ↑ "UpToDate". https://www.uptodate.com/contents/cerebral-amyloid-angiopathy.
- ↑ Newfoundland, FRCP William Pryse-Phillips MD, FRCP(C) Faculty of Medicine Health Sciences Centre Memorial University of Newfoundland St John's (2009-05-06). Companion to Clinical Neurology. Oxford University Press, USA. ISBN 9780199710041. https://books.google.com/books?id=mBGB7FOFJMoC&pg=PA177.
- ↑ "Exploring cerebral amyloid angiopathy: Insights into pathogenesis, diagnosis, and treatment". https://www.jns-journal.com/article/S0022-510X(23)00327-1/fulltext.
- ↑ Godefroy, Olivier (2013-02-28). The Behavioral and Cognitive Neurology of Stroke. Cambridge University Press. ISBN 9781107310896. https://books.google.com/books?id=zdMgAwAAQBAJ&pg=PA397.
- ↑ Coleman, William B.; Tsongalis, Gregory J. (2010-02-16). Essential Concepts in Molecular Pathology. Academic Press. ISBN 9780080922188. https://books.google.com/books?id=z7r6paMUnmAC&pg=PA386.
- ↑ "Brain Basics: Preventing Stroke: National Institute of Neurological Disorders and Stroke (NINDS)". http://www.ninds.nih.gov/disorders/stroke/preventing_stroke.htm.
- ↑ Tsai, Hsin-Hsi; Pasi, Marco; Tsai, Li-Kai; Chen, Ya-Fang; Chen, Yu-Wei; Tang, Sung-Chun; Gurol, M. Edip; Yen, Ruoh-Fang et al. (January 2020). "Superficial Cerebellar Microbleeds and Cerebral Amyloid Angiopathy". Stroke 51 (1): 202–208. doi:10.1161/STROKEAHA.119.026235. PMID 31726962. https://www.ahajournals.org/doi/full/10.1161/STROKEAHA.119.026235. Retrieved 2023-11-17.
- ↑ Sirven, Joseph I.; Malamut, Barbara L. (2008). Clinical Neurology of the Older Adult. Lippincott Williams & Wilkins. ISBN 9780781769471. https://books.google.com/books?id=c1tL8C9ryMQC&pg=PA275.
- ↑ Ettinger, Alan B.; Weisbrot, Deborah M. (2014-04-17). Neurologic Differential Diagnosis: A Case-Based Approach. Cambridge University Press. ISBN 9781107014558. https://books.google.com/books?id=XDA4AwAAQBAJ&pg=PA429.
- ↑ Kumar-Singh, S. et al. (2002). "Dense-core senile plaques in the Flemish variant of Alzheimer's disease are vasocentric". American Journal of Pathology 161 (2): 507–20. doi:10.1016/S0002-9440(10)64207-1. PMID 12163376.
- ↑ Tolnay, Markus; Probst, Alphonse (2012-12-06). Neuropathology and Genetics of Dementia. Springer Science & Business Media. ISBN 9781461512493. https://books.google.com/books?id=5k_TBwAAQBAJ&pg=PA114.
- ↑ Subramaniam, Rathan; Barrio, Jorge (2013-10-15). Novel Imaging Techniques in Neurodegenerative and Movement Disorders, an Issue of Pet Clinics. Elsevier Health Sciences. ISBN 9780323227353. https://books.google.com/books?id=RPoxAgAAQBAJ&pg=PA393.
- ↑ Brain Extracellular Matrix in Health and Disease. Elsevier. 2014-10-30. ISBN 9780444634948. https://books.google.com/books?id=SMoSBAAAQBAJ&pg=PA213.
- ↑ Hall, Tim (2013-09-17). PACES for the MRCP: with 250 Clinical Cases. Elsevier Health Sciences. ISBN 978-0702054662. https://books.google.com/books?id=Tx2trEGUjyYC&pg=PA401.
- ↑ Mental Disorders: New Insights for the Healthcare Professional: 2011 Edition. ScholarlyEditions. 2012-01-09. ISBN 9781464900853. https://books.google.com/books?id=9ij0tqFkfx8C&pg=PT51.
- ↑ Advances in Dementia Research and Treatment: 2012 Edition. ScholarlyEditions. 2012-12-26. ISBN 9781464991721. https://books.google.com/books?id=VgzFWhErv2AC&pg=PT128.
- ↑ 19.0 19.1 19.2 Sharma, Rohit; Dearaugo, Stephanie; Infeld, Bernard; O'Sullivan, Richard; Gerraty, Richard P (August 2018). "Cerebral amyloid angiopathy: Review of clinico-radiological features and mimics" (in en). Journal of Medical Imaging and Radiation Oncology 62 (4): 451–463. doi:10.1111/1754-9485.12726. PMID 29604173.
- ↑ Revesz, Tamas; Holton, Janice L.; Lashley, Tammaryn; Plant, Gordon; Rostagno, Agueda; Ghiso, Jorge; Frangione, Blas (July 2002). "Sporadic and familial cerebral amyloid angiopathies". Brain Pathology (Zurich, Switzerland) 12 (3): 343–357. doi:10.1111/j.1750-3639.2002.tb00449.x. ISSN 1015-6305. PMID 12146803.
- ↑ Dickson, Dennis; Weller, Roy O. (2011-09-09). Neurodegeneration: The Molecular Pathology of Dementia and Movement Disorders. John Wiley & Sons. ISBN 9781444341232. https://books.google.com/books?id=4SYIwcoH_yoC&pg=PA100.
- ↑ Larner, A. J. (2008-04-24). Neuropsychological Neurology: The Neurocognitive Impairments of Neurological Disorders. Cambridge University Press. ISBN 9780521717922. https://books.google.com/books?id=AQxhmgISQ_UC&pg=PA108.
- ↑ Dening, Tom; Thomas, Alan (2013-09-26). Oxford Textbook of Old Age Psychiatry. OUP Oxford. ISBN 9780199644957. https://books.google.com/books?id=QXemAgAAQBAJ&pg=PA131.
- ↑ 24.0 24.1 Biffi, Alessandro; Greenburg, Steven M. (2011). "Cerebral Amyloid Angiopathy: A Systematic Review". Journal of Clinical Neurology 7 (1): 1–9. doi:10.3988/jcn.2011.7.1.1. PMID 21519520.
- ↑ Thal, Dietmar Rudolph; Ghebremidhin, Estifanos; Rüb, Udo; Haruyasu, Yamaguchi; Del Tredici, Kelly; Braak, Heiko (2002). "Two types of sporadic cerebral amyloid angiopathy". Journal of Neuropathology & Experimental Neurology 61 (3): 282–293. doi:10.1093/jnen/61.3.282. PMID 11895043.
- ↑ Mittal, S.; Wu, Z.; Neelavalli, J.; Haacke, E. M. (2009). "Susceptibility-Weighted Imaging: Technical Aspects and Clinical Applications, Part 2". American Journal of Neuroradiology 30 (2): 232–252. doi:10.3174/ajnr.A1461. ISSN 0195-6108. PMID 19131406.
- ↑ 27.0 27.1 27.2 Greenberg, Steven; Charidimou, Andreas (2018). "Diagnosis of Cerebral Amyloid Angiopathy: Evolution of the Boston Criteria". Stroke 49 (2): 491–497. doi:10.1161/STROKEAHA.117.016990. PMID 29335334.
- ↑ Verbeek, M. M.; Waal, R. M. de; Vinters, Harry V. (2013). Cerebral Amyloid Angiopathy in Alzheimer's Disease and Related Disorders. Springer Science & Business Media. ISBN 9789401710077. https://books.google.com/books?id=kRgrBgAAQBAJ&pg=PT43.
- ↑ Ellenbogen, Richard G.; Abdulrauf, Saleem I.; Sekhar, Laligam N. (2012). Principles of Neurological Surgery. Elsevier Health Sciences. ISBN 978-1437707014. https://books.google.com/books?id=vMtRtuz5mnwC&pg=PA67.
- ↑ Charidimou, Andreas; Boulouis, Gregoire; Gurol, M. Edip; Ayata, Cenk; Bacskai, Brian J.; Frosch, Matthew P.; Viswanathan, Anand; Greenberg, Steven M. (1 July 2017). "Emerging concepts in sporadic cerebral amyloid angiopathy" (in en). Brain 140 (7): 1829–1850. doi:10.1093/brain/awx047. ISSN 0006-8950. PMID 28334869.
Further reading
- Chao, Christine P.; Kotsenas, Amy L.; Broderick, Daniel F. (September 1, 2006). "Cerebral Amyloid Angiopathy: CT and MR Imaging Findings". RadioGraphics 26 (5): 1517–1531. doi:10.1148/rg.265055090. ISSN 0271-5333. PMID 16973779.
External links
| Classification | |
|---|---|
| External resources |
 |