Biology:Adrenergic blocking agent
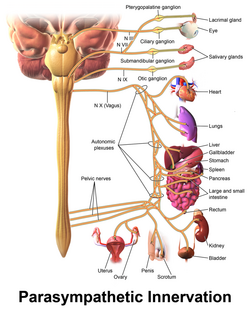
Adrenergic blocking agents are a class of drugs that exhibit its pharmacological action through inhibiting the action of the sympathetic nervous system[1] in the body. The sympathetic nervous system(SNS) is an autonomic nervous system that we cannot control by will. It triggers a series of responses after the body releases chemicals named noradrenaline and epinephrine.[1] These chemicals will act on adrenergic receptors, with subtypes Alpha-1, Alpha-2, Beta-1, Beta-2, Beta-3, which ultimately allow the body to trigger a "fight-or-flight" response to handle external stress.[1] These responses include vessel constriction in general vessels whereas there is vasodilation in vessels that supply skeletal muscles or in coronary vessels.[1] Additionally, the heart rate and contractile force increase when SNS is activated, which may be harmful to cardiac function as it increases metabolic demand.[1] Adrenergic blocking agents treat certain diseases through blocking the adrenergic receptor,[2][3] preventing it from being activated by noradrenaline and epinephrine. As a result, it stops the body from producing the "fight-or-flight" responses.
Medical Uses
There are drugs that are approved by the Food and Drug Administration (FDA), whereas there are some off-label uses as well.
Alpha 1 blocker
The alpha blockers mostly act in our smooth muscles, especially the ones that control the size of vessels.[3] Thus, alpha1 blockers can dilate blood vessels and decrease the blood pressure.[3] Depending on its site of action, it can be used to treat different diseases.[3] They can be used to treat signs and symptoms of benign prostatic hyperplasia, hypertension (but not as first line agent), pheochromocytoma, extravasation management and reversal of local anesthesia.[3]
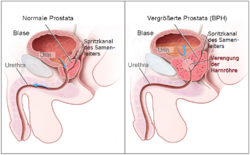

There are some off- label use as well, such as chronic prostatitis and lower urinary tract symptoms in males, ureteral calculus expulsion, ureteral stent-related urinary symptoms.[3] It can be used in post-traumatic stress disorder, Raynaud phenomenon, hypertensive crisis, Extravasation of sympathomimetic vasopressors, problem with urine related to neurogenic bladder, functional outlet obstruction and partial prostate obstruction.[3]
Alpha 2 blocker
Alpha2 blocker reduces the transmission of neurotransmitters circulating around the body, which contributes to contraction of smooth muscle.[4] Instead of treating diseases, they are used as antidotes for reversing overdose of alpha-2 agonist, reducing the toxic effect of the agonist.[4] Only limited indications are present for this drug. More research is in progress to investigate the possible use of alpha2 blockers.[4]
Beta 1 blocker

Since beta 1 receptor are mainly located in the heart, most beta 1 blockers take abnormalities associated with the heart as the target.[5] It treats medical conditions like hypertension, arrhythmias, heart failure, chest pain, myocardial infarction. It treats other symptoms unrelated to heart like migraines and anxiety.[5]
Beta 2 blocker
Beta2 blockers promote vasodilation in some tissues as mentioned above(arterioles in skeletal muscles or ciliary muscle in the eye etc.). Currently, there is no beta-2 blocker with FDA approval.[6] Butoxamine, an example of beta 2 blocker, has no clinical use but is used in research.[6]
Beta 3 blocker
Due to the relatively limited study on beta-3 receptor, there is not much development of beta-3 blocker. Therefore, beta-3 blocker has no clinical use now.[7]
Adverse Effect
Selectivity
Some drugs, being non-selective, can exert actions on 2 or more different receptors. Examples include non-selective beta blocker, which block both beta-1 receptor and beta-2 receptor as well.[2]
Non-selective alpha blocker
The adverse effects of non-selective alpha blockers are caused by the autonomic response to the systemic changes induced by the adrenergic blocking agents.[3] The common adverse effects of alpha blockers are due to the blockade of alpha-1 adrenergic receptors in tissue that requires high level of alpha adrenergic sympathetic input such as arterial resistance, vascular capacitance and the outflow tract of the urinary bladder.[8] The undesirable symptoms are mentioned in the following 'selective alpha-1 blocker' part.
Selective alpha 1 blocker
With the vasodilation and smooth muscle relaxation caused by alpha-1 blockers,[9] around 10 to 20% of patients present undesirable effects of asthenia(weakness), dizziness, faintness and syncope.[8] Other adverse outcomes that are even more uncommon include headache, drowsiness, palpitations, urinary incontinence and priapism.[8] Mild body weight gain of 1–2 kg, which may be associated with secondary hyperaldosteronism, is also observed in some patients.[8]

The alpha-1 blockers are associated with the first-dose effect, which refers to the tachycardia response and orthostatic hypotension that caused by the systemic vasodilation at the initial administration of alpha-1 blockers.[3] After the first administration, patients may experience a short period of orthostatic hypotension with a sensation of intense faintness, which is aggravated by upright posture, intravascular volume depletion or concurrent administration of other antihypertensive medications.[8]
Selective alpha 2 blocker
Apart from increasing the noradrenaline release, the selective alpha-2 blockers have the potential to bind with other receptors such as the 5-HT serotonin receptor.[10] However, the serotonin receptor antagonism has side effects such as weight gain and impaired movement.[11] Hence, alpha-2 blockers are not used clinically due to its extensive binding.
Similar to the alpha-1 blocker, the alpha-2 family will also present the first-dose effect, but it is generally less pronounced compared with the alpha-1 blockers.[3]
Non-selective beta blocker
The Central Nervous System (CNS) side effects of beta blockers including sleep impairment, dreaming, nightmares and hallucinations are generally small. Also, the effects on short-term memory are minimal.[12]
Selective beta 1 blocker

The cardio-selective beta-1 blockers could cause adverse effects including bradycardia, reduced exercise ability, hypotension, atrioventricular nodal blockage and heart failure.[5] Other possible adverse effects include nausea and vomiting, abdominal discomfort, dizziness, weakness, headache, fatigue, and dryness in mouth and eye.[5] Sexual impairment, memory loss, and confusion are regarded as rare side effects.[5] For diabetic patients, there is an extra risk of masking hypoglycemia-induced tachycardia, while a continuous hypoglycemia could cause acute brain damage.[5]
Selective beta 2 blocker

The blockade of beta-2 receptors will result in vasoconstriction and smooth muscle constriction,[6] and the effects are similar to the agonism of alpha-1 receptors. The side effects include hypertension, tachycardia, arrhythmia and subcutaneous ischemia at the site of injection.[3] Other possible side effects include Raynaud phenomenon, hypoglycemia during exercise, muscle cramps, and increase of airway resistance.[6]
Selective beta 3 blocker
Due to the relatively limited study on beta-3 receptor, there is not much development of beta-3 blocker. Therefore, there is limited information on the adverse effects caused by beta-3 blocker.
Contraindications
Alpha 1 blocker
As alpha 1 blocker will dilate blood vessels, it lowers the blood pressure.[3] Thus, it contraindicate to patients with a history of orthostatic hypotension and in current use of phosphodiesterase inhibitors.[3] Moreover, alpha 1 blocker should not be given to patients with heart failure since it expands blood volume.[13]
Alpha 2 blocker
There are limited information about the contraindication of alpha-2 blocker, since it has limited clinical uses.
Beta 1 blocker

Traditionally, Beta-1 blocker has several contraindications, including, recent history of fluid retention without use of diuretics, and complete or second degree of heart block.[5] Whilst some studies suggest that there are only minor differences in terms of adverse effect between asthma patients and non-asthma patients, beta-1 blockers are generally not prescribed to asthma patients or patients with chronic obstructive pulmonary disease, due to its potential blockage of beta 2 receptors.[5] Additionally, beta1 blocker should not be given to patients with peripheral vascular diseases, diabetes mellitus, since blockage of beta-2 receptors may lead to vasoconstriction and delayed response to hypoglycemia respectively.[5]
Beta 2 blocker
Beta 2 blocker should be avoided for patients with asthma, COPD as it causes bronchoconstriction.[6] It may also increase the chance of hypoglycemic comas in diabetic patients.[6]
Beta 3 blocker
Due to the relatively limited study on beta-3 receptor, there is not much development of beta-3 blocker. Therefore, beta-3 blocker has no clinical use. The contraindications of beta-3 blocker can not be observed.
Overdose effects
Alpha 1 blocker
Overdose of alpha-1 blocker will lead to an unopposed parasympathetic activity.[3] Symptoms include bradycardia, hypotension, miosis and sedation.
Alpha 2 blocker
There is a lack of information regarding toxicity caused by overdose of alpha-2 blocker, due to its limited clinical uses.
Beta 1 blocker
Toxicity of beta-1 blocker will contribute to symptoms including bradycardia, hypotension, due to its extensive blockage of beta-1 receptor.[5] Moreover, overdose of beta-1 blocker may lead to the loss of their selectivity and bind to beta-2 receptor, causing bronchopulmonary symptoms.[5] Overdose of lipophilic beta-1 blocker can disturb neurologic functioning, which eventually lead to altered mental states.[5]
To mitigate the toxicity of Beta-1 blocker, glucagon, salts like calcium and sodium bicarbonate, magnesium sulfate are used to reverse beta-1-blocker effect and treating hypotension respectively.[5]
Beta 2 blocker
Similar to alpha-2 blocker, there is a lack of information about beta-2 blocker's toxicity, due to its limited clinical uses.
Beta 3 blocker
Due to the relatively limited study on beta-3 receptor, there is not much development of beta-3 blocker. Therefore, there is not much information regarding the toxic effect of beta-3 blocker.
Drug Interaction
Alpha 1 blocker
CYP3A4 inhibitors
Alpha-1 blockers such as Alfuzosin, Doxazosin, Tamsulosin and Silodosin involve CYP450 enzyme metabolism, particularly by CYP3A4.[14] Alpha-1 blockers will conjugate in glucuronidation during metabolism. CYP3A4 inhibitors inhibit glucuronidation and hence reduce the glucuronide-conjugated metabolite.[15] Hence, potent CYP3A4 inhibitors can potentially increase their exposure to those alpha blockers. However, there are no clinically significant evidence supporting the drug interaction between alpha-1 blocker and CYP3A4 inhibitors.[16]
Alpha 2 blocker
Since alpha-2 blocker has limited clinical uses, there is a lack of information on drug interaction regarding alpha-2 blocker.
Beta 1 blocker
Antihypertensive drugs
Additional hypotensive effects may occur when patients are taking beta-1 blockers with other antihypertensive drugs such as nitrates, PDE inhibitors, ACE inhibitors and calcium channel blockers.[17] The combination of beta blockers and antihypertensive drugs will work on different mechanism to lower blood pressure.[17] For example, the co-administration of beta-1 blocker atenolol and ACE inhibitor lisinopril could produce a 50% larger reduction in blood pressure than using either drug alone.[18]
Hypertensive drugs

Antihypertensive drugs and hypertensive drugs affect blood pressure in an opposite way.[19] The most common hypertensive drugs in the UK are NSAIDs and steroids.[19] NSAIDs inhibit the synthesis of prostaglandin, which increases the blood pressure and potentially reduce the efficacy of several antihypertensive drugs.[20]
Beta 2 blocker
Since beta-2 blocker has limited clinical uses, there is a lack of information on drug interaction regarding beta-2 blocker.
Beta 3 blocker
Since beta-3 blocker is still under development, there is a lack of information on drug interaction about beta-3 blocker.
Mechanism of Action
Alpha 1 blocker
Alpha 1 blocker exerts its action on alpha-1 receptor, dilating the smooth muscles.[3] Alpha-1 receptor is a Gq type G-protein coupled receptor.[3] When it is activated, it will lead to activation of phospholipase C, raising the intracellular level of IP3 and DAG.[3] As a result, a higher intracellular concentration of Calcium is achieved, contributing to smooth muscle contraction and glycogenolysis.[3] Alpha 1 blockers, in contrast, bind to and act as inhibitors of alpha-1 receptors, hence preventing the downstream action mentioned(increase of phospholipase C, IP3 and DAG hence increase of Ca Concentration).[3] As a result, the contraction of smooth muscle is suppressed.
Alpha 2 blocker
The alpha-2 blocker acts on alpha-2 receptors. The alpha-2 receptor is a G-protein coupled receptor as well, which exert its action by Gi function, leading to an inhibition of adenylyl cyclase and thus reducing synthesis of cAMP.[3] It lowers the amount of calcium inside the cell.[3] Ultimately, release of noradrenaline and epinephrine will be inhibited and smooth muscles tend to dilate.[3] Alpha-2 blocker stops the downstream signaling pathway (inhibit adenylyl cyclase, reduce cAMP and Ca), thus lead to release of the mentioned neurotransmitters(noradrenaline and epinephrine) and contraction of smooth muscle eventually.[3]
Beta 1 blocker
Beta1 blocker will stop the action of beta-1 receptor via occupying the beta-1 receptor without any activation.[5] The beta-1 receptor is a G-protein-coupled receptor with Gs alpha subunit as its main communication method.[5] By signaling Gs, adenylyl cyclase is recruited to activate a cAMP pathway, which potentiates the receptor.[5] This kind of receptor is located at the heart, kidney and adipose tissue.[5] Eventually, a higher cardiac output(or an increased amount of perfusion to organs) will be resulted.[5] Moreover, more renin is released from the kidney to produce more angiotensin II, increasing the blood volume.[5] Moreover, it encourages lipolysis in adipose tissue. Beta-1 blocker blocks the beta-1 receptor and stops the action mentioned above. (signaling Gs, thus activate cAMP pathway by recruiting adenylyl cyclase, leading to higher cardiac output, renin release and lipolysis)
Beta 2 blocker
Beta 2 blockers cease action of beta-2 receptor by blocking the receptor and preventing it from being activated.[6] Similar to beta-1 receptor, the activated beta-2 receptor will lead to the detach of alpha subunit of Gs protein and attachment of adenylate cyclase.[6] Adenosine triphosphate(ATP), is then catalyzed to form cAMP.[6] cAMP will facilitate release of protein kinase A as well as reduction of intracellular calcium level, relaxing the smooth muscles.[6] Beta-2 blockers stops the above-mentioned signaling pathway, (formation of cAMP, release of protein kinase A, reduction of intracellular calcium level) by blocking the receptor.
Remarks: It has to be noted that alpha-1 receptor has an opposite action when it is compared with beta 2 receptor. However, the location of the two receptors differs in different tissues, which gives rise to different action of smooth muscle.[21] For example, in the eye, under stimulation of sympathetic nervous system, radial muscles of the iris contract through activation of alpha-1 receptor to allow more light to enter, while the ciliary muscle in the eye relaxes through activation of beta-2 receptor to allow far vision.[21] In the arterioles of skeletal muscle, there is only mild constriction under activation of SNS, due to the balance between alpha-1 and beta-2 receptors.[21][1]
Beta 3 blocker
Beta-3 blocker will inactivate beta-3 receptor and stops the following action.[7] Beta 3 receptor is a G-protein coupled receptor, similar to beta-1 and beta-2 receptors.[7] The receptor is involved in G-as activation.[7] The receptor will also stimulate adenylyl cyclase.[7] Eventually, it will lead to effects like increase of tryptophan and 5-hydroxytryptamine level, increase of lipolysis in adipose tissue.[7] Beta-3 blocker will antagonize the receptor, which will stop the signaling pathway(G-as activation, stimulation of adenylyl cyclase).[7]
History
Alpha Blocker
In 1978, a successful alpha blocker, phenoxybenzamine was confirmed to be clinically beneficial through a randomized, placebo-controlled study.[22] It was the first alpha blocker which was used for treating Benign Prostatic Hyperplasia.[22]
Another Alpha Blocker Prazosin, which was the first drug selective to alpha 1 receptor, was developed in 1987[22] for the therapy of Benign Prostatic Hyperplasia. Other alpha blockers are then introduced for several diseases.[22]
Beta Blocker
The first beta blocker, propranolol, was introduced in the early 1960s by the winner of The Nobel Prize in Physiology or Medicine 1988- Sir James W. Black.[23] The drug was originally developed in order to induce a calm effect on the heart by blocking the beta receptor for adrenaline, treating a range of cardiovascular disorders.[23]
Beta 3 blocker
Unlike other subtypes of receptor, beta 3 receptors were more recently discovered in 1989.[7] Therefore, Beta 3 blockers are still under development.
Agents
The following examples are the common adrenergic blocking agents used clinically.
Non-selective alpha blocker
- Phenoxybenzamine
- Phentolamine
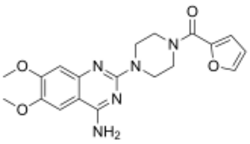
Selective alpha 1 blocker
- Prazosin
- Tamsulosin
Selective alpha 2 blocker
- Yohimbine
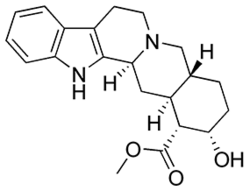
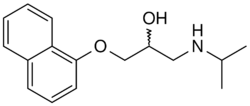
Non-selective beta blocker
- Propranolol
- Timolol
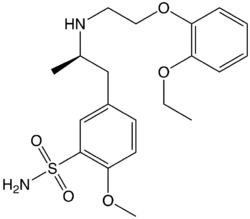
Selective beta 1 blocker
- Atenolol
- Metoprolol
Selective beta 2 blocker
- Butaxamine
Selective beta 3 blocker
- Still under development
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 Waxenbaum, Joshua A.; Reddy, Vamsi; Varacallo, Matthew (2021), "Anatomy, Autonomic Nervous System", StatPearls (Treasure Island (FL): StatPearls Publishing), PMID 30969667, http://www.ncbi.nlm.nih.gov/books/NBK539845/, retrieved 2021-03-31
- ↑ 2.0 2.1 Alhayek, Soubhi; Preuss, Charles V. (2021), "Beta 1 Receptors", StatPearls (Treasure Island (FL): StatPearls Publishing), PMID 30422499, http://www.ncbi.nlm.nih.gov/books/NBK532904/, retrieved 2021-03-31
- ↑ 3.00 3.01 3.02 3.03 3.04 3.05 3.06 3.07 3.08 3.09 3.10 3.11 3.12 3.13 3.14 3.15 3.16 3.17 3.18 3.19 3.20 3.21 3.22 Taylor, Bryce N.; Cassagnol, Manouchkathe (2021), "Alpha Adrenergic Receptors", StatPearls (Treasure Island (FL): StatPearls Publishing), PMID 30969652, http://www.ncbi.nlm.nih.gov/books/NBK539830/, retrieved 2021-03-31
- ↑ 4.0 4.1 4.2 Crassous, Pierre-Antoine; Denis, Colette; Paris, Hervé; Sénard, Jean Michel (2007). "Interest of alpha2-adrenergic agonists and antagonists in clinical practice: background, facts and perspectives". Current Topics in Medicinal Chemistry 7 (2): 187–194. doi:10.2174/156802607779318190. ISSN 1873-4294. PMID 17266605. https://pubmed.ncbi.nlm.nih.gov/17266605/.
- ↑ 5.00 5.01 5.02 5.03 5.04 5.05 5.06 5.07 5.08 5.09 5.10 5.11 5.12 5.13 5.14 5.15 5.16 5.17 5.18 Tucker, William D.; Sankar, Parvathy; Theetha Kariyanna, Pramod (2021), "Selective Beta-1-Blockers", StatPearls (Treasure Island (FL): StatPearls Publishing), PMID 29763157, http://www.ncbi.nlm.nih.gov/books/NBK499982/, retrieved 2021-03-31
- ↑ 6.00 6.01 6.02 6.03 6.04 6.05 6.06 6.07 6.08 6.09 Abosamak, Nour Eldin R.; Shahin, Mohamed H. (2021), "Beta 2 Receptor Agonists/Antagonists", StatPearls (Treasure Island (FL): StatPearls Publishing), PMID 32644495, http://www.ncbi.nlm.nih.gov/books/NBK559069/, retrieved 2021-03-31
- ↑ 7.0 7.1 7.2 7.3 7.4 7.5 7.6 7.7 Schena, Giorgia; Caplan, Michael J. (2019-04-16). "Everything You Always Wanted to Know about β3-AR * (* But Were Afraid to Ask)". Cells 8 (4): 357. doi:10.3390/cells8040357. ISSN 2073-4409. PMID 30995798.
- ↑ 8.0 8.1 8.2 8.3 8.4 Carruthers, S. G. (1994-07-11). "Adverse effects of alpha 1-adrenergic blocking drugs". Drug Safety 11 (1): 12–20. doi:10.2165/00002018-199411010-00003. ISSN 0114-5916. PMID 7917078. https://pubmed.ncbi.nlm.nih.gov/7917078/.
- ↑ "Alpha 1 Adrenergic Receptor Antagonists", LiverTox: Clinical and Research Information on Drug-Induced Liver Injury (Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases), 2012, PMID 31644028, http://www.ncbi.nlm.nih.gov/books/NBK548719/, retrieved 2021-03-15
- ↑ Haddjeri, N.; Blier, P.; de Montigny, C. (1996-05-01). "Effect of the alpha-2 adrenoceptor antagonist mirtazapine on the 5-hydroxytryptamine system in the rat brain". The Journal of Pharmacology and Experimental Therapeutics 277 (2): 861–871. ISSN 0022-3565. PMID 8627568. https://pubmed.ncbi.nlm.nih.gov/8627568/.
- ↑ Casey, Austen B.; Canal, Clinton E. (2017-06-21). "Classics in Chemical Neuroscience: Aripiprazole". ACS Chemical Neuroscience 8 (6): 1135–1146. doi:10.1021/acschemneuro.7b00087. ISSN 1948-7193. PMID 28368577.
- ↑ McAinsh, J.; Cruickshank, J. M. (1990). "Beta-blockers and central nervous system side effects". Pharmacology & Therapeutics 46 (2): 163–197. doi:10.1016/0163-7258(90)90092-g. ISSN 0163-7258. PMID 1969642. https://pubmed.ncbi.nlm.nih.gov/1969642/.
- ↑ Grimm, Richard H.; Flack, John M. (2011-09-13). "Alpha 1 adrenoreceptor antagonists". Journal of Clinical Hypertension (Greenwich, Conn.) 13 (9): 654–657. doi:10.1111/j.1751-7176.2011.00510.x. ISSN 1751-7176. PMID 21896145.
- ↑ Troost, Joachim; Tatami, Shinji; Tsuda, Yasuhiro; Mattheus, Michaela; Mehlburger, Ludwig; Wein, Martina; Michel, Martin C (2011-08-01). "Effects of strong CYP2D6 and 3A4 inhibitors, paroxetine and ketoconazole, on the pharmacokinetics and cardiovascular safety of tamsulosin". British Journal of Clinical Pharmacology 72 (2): 247–256. doi:10.1111/j.1365-2125.2011.03988.x. ISSN 0306-5251. PMID 21496064.
- ↑ Rossi, Maxime; Roumeguère, Thierry (2010-10-27). "Silodosin in the treatment of benign prostatic hyperplasia". Drug Design, Development and Therapy 4: 291–297. doi:10.2147/DDDT.S10428. ISSN 1177-8881. PMID 21116335.
- ↑ Bensalah, N.; Garcia, S.; Rose, F. X.; Bedouch, P.; Conort, O.; Juste, M.; Roubille, R.; Allenet, B. et al. (2017-04-27). "[How to act when an alpha-blocker is associated with a potent inhibitor of CYP3A4"]. Progrès en Urologie 27 (5): 275–282. doi:10.1016/j.purol.2017.02.003. ISSN 1166-7087. PMID 28365198. https://pubmed.ncbi.nlm.nih.gov/28365198/.
- ↑ 17.0 17.1 Laurent, Stéphane (2017-07-26). "Antihypertensive drugs". Pharmacological Research 124: 116–125. doi:10.1016/j.phrs.2017.07.026. ISSN 1096-1186. PMID 28780421. https://pubmed.ncbi.nlm.nih.gov/28780421/.
- ↑ Wing, L. M.; Chalmers, J. P.; West, M. J.; Russell, A. E.; Morris, M. J.; Cain, M. D.; Bune, A. J.; Southgate, D. O. (1988). "Enalapril and atenolol in essential hypertension: attenuation of hypotensive effects in combination". Clinical & Experimental Hypertension, Part A 10 (1): 119–133. doi:10.3109/10641968809046803. ISSN 0730-0077. PMID 2832102. https://pubmed.ncbi.nlm.nih.gov/2832102/.
- ↑ 19.0 19.1 Elliott, William J. (2006-10-01). "Drug interactions and drugs that affect blood pressure". Journal of Clinical Hypertension (Greenwich, Conn.) 8 (10): 731–737. doi:10.1111/j.1524-6175.2006.05939.x. ISSN 1524-6175. PMID 17028488.
- ↑ Polónia, J. (1997). "Interaction of antihypertensive drugs with anti-inflammatory drugs". Cardiology 88 Suppl 3 (3): 47–51. doi:10.1159/000177507. ISSN 0008-6312. PMID 9397294. https://pubmed.ncbi.nlm.nih.gov/9397294/.
- ↑ 21.0 21.1 21.2 Alshak, Mark N.; M Das, Joe (2021), "Neuroanatomy, Sympathetic Nervous System", StatPearls (Treasure Island (FL): StatPearls Publishing), PMID 31194352, http://www.ncbi.nlm.nih.gov/books/NBK542195/, retrieved 2021-03-31
- ↑ 22.0 22.1 22.2 22.3 Lepor, Herbert (2007). "Alpha Blockers for the Treatment of Benign Prostatic Hyperplasia". Reviews in Urology 9 (4): 181–190. ISSN 1523-6161. PMID 18231614.
- ↑ 23.0 23.1 "The Nobel Prize in Physiology or Medicine 1988" (in en-US). https://www.nobelprize.org/prizes/medicine/1988/black/facts/.
- ↑ Yoham, Athina L.; Casadesus, Damian (2021), "Phenoxybenzamine", StatPearls (Treasure Island (FL): StatPearls Publishing), PMID 32809502, http://www.ncbi.nlm.nih.gov/books/NBK560667/, retrieved 2021-03-15
- ↑ "Dibenzyline (Phenoxybenzamine): Uses, Dosage, Side Effects, Interactions, Warning" (in en). https://www.rxlist.com/dibenzyline-drug.htm.
- ↑ Grover, Harpreet Singh; Gupta, Anil; Saksena, Neha; Saini, Neha (2015-10-01). "Phentolamine mesylate: It's [sic] role as a reversal agent for unwarranted prolonged local analgesia". Journal of Indian Society of Pedodontics and Preventive Dentistry 33 (4): 265–268. doi:10.4103/0970-4388.165646. ISSN 1998-3905. PMID 26381625.
- ↑ "Regitine, OraVerse (phentolamine) dosing, indications, interactions, adverse effects, and more". https://reference.medscape.com/drug/regitine-oraverse-phentolamine-342392.
- ↑ "Prazosin - Search Results - PubMed" (in en). https://pubmed.ncbi.nlm.nih.gov/?term=Prazosin+&filter=pubt.review.
- ↑ "Drug Office | 藥 物 辦 公 室". https://www.drugoffice.gov.hk/eps/drug/productDetail/en/healthcare_providers/111892.
- ↑ "Tamsulosin", LiverTox: Clinical and Research Information on Drug-Induced Liver Injury (Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases), 2012, PMID 31643349, http://www.ncbi.nlm.nih.gov/books/NBK548017/, retrieved 2021-03-15
- ↑ "Drug Office | 藥 物 辦 公 室". https://www.drugoffice.gov.hk/eps/drug/productDetail/en/healthcare_providers/113925.
- ↑ Tam, S. W.; Worcel, M.; Wyllie, M. (2001-09-01). "Yohimbine: a clinical review". Pharmacology & Therapeutics 91 (3): 215–243. doi:10.1016/s0163-7258(01)00156-5. ISSN 0163-7258. PMID 11744068. https://pubmed.ncbi.nlm.nih.gov/11744068/.
- ↑ "Drug Office | 藥 物 辦 公 室". https://www.drugoffice.gov.hk/eps/drug/productDetail/en/healthcare_providers/68206.
- ↑ Linde, K.; Rossnagel, K. (2004). Hobson, Anna. ed. "Propranolol for migraine prophylaxis". The Cochrane Database of Systematic Reviews (2): CD003225. doi:10.1002/14651858.CD003225.pub2. ISSN 1469-493X. PMID 15106196. https://pubmed.ncbi.nlm.nih.gov/15106196/.
- ↑ "Drug Office | 藥 物 辦 公 室". https://www.drugoffice.gov.hk/eps/drug/productDetail/en/healthcare_providers/111589.
- ↑ Barnes, James; Moshirfar, Majid (2021), "Timolol", StatPearls (Treasure Island (FL): StatPearls Publishing), PMID 31424760, http://www.ncbi.nlm.nih.gov/books/NBK545176/, retrieved 2021-03-15
- ↑ "Drug Office | 藥 物 辦 公 室". https://www.drugoffice.gov.hk/eps/drug/productDetail/en/healthcare_providers/115898.
- ↑ Rehman, Baryiah; Sanchez, Daniela P.; Shah, Saumya (2021), "Atenolol", StatPearls (Treasure Island (FL): StatPearls Publishing), PMID 30969666, http://www.ncbi.nlm.nih.gov/books/NBK539844/, retrieved 2021-03-15
- ↑ "Drug Office | 藥 物 辦 公 室". https://www.drugoffice.gov.hk/eps/drug/productDetail/en/healthcare_providers/127821.
- ↑ "Metoprolol - Search Results - PubMed" (in en). https://pubmed.ncbi.nlm.nih.gov/?term=Metoprolol+&filter=pubt.review.
- ↑ "Drug Office | 藥 物 辦 公 室". https://www.drugoffice.gov.hk/eps/drug/productDetail/en/healthcare_providers/110932.
- ↑ PubChem. "Butaxamine" (in en). https://pubchem.ncbi.nlm.nih.gov/compound/18026.
 |