Chemistry:Nonsteroidal anti-inflammatory drug
| Non-steroidal anti-inflammatory drug | |
|---|---|
| Drug class | |
 | |
| Class identifiers | |
| Pronunciation | /ˈɛnsɛd/ EN-sed |
| Synonyms |
|
| Use | Pain,[1] fever,[1] inflammation,[1] antithrombosis[citation needed] |
| ATC code | M01A |
| Mechanism of action | Enzyme inhibitor |
| Biological target | COX-1 and COX-2 |
Non-steroidal anti-inflammatory drugs[1][3] (NSAID)[1] are members of a therapeutic drug class which reduces pain,[4] decreases inflammation, decreases fever,[1] and prevents blood clots. Side effects depend on the specific drug, its dose and duration of use, but largely include an increased risk of gastrointestinal ulcers and bleeds, heart attack, and kidney disease.[5][6]
The term non-steroidal, common from around 1960, distinguishes these drugs from corticosteroids, which during the 1950s had acquired a bad reputation due to overuse and side-effect problems after their initial introduction in 1948.[7][8][9]
NSAIDs work by inhibiting the activity of cyclooxygenase enzymes (the COX-1 and COX-2 isoenzymes). In cells, these enzymes are involved in the synthesis of key biological mediators, namely prostaglandins, which are involved in inflammation, and thromboxanes, which are involved in blood clotting.
There are two general types of NSAIDs available: non-selective, and COX-2 selective.[10] Most NSAIDs are non-selective, and inhibit the activity of both COX-1 and COX-2. These NSAIDs, while reducing inflammation, also inhibit platelet aggregation and increase the risk of gastrointestinal ulcers and bleeds.[10] COX-2 selective inhibitors have fewer gastrointestinal side effects, but promote thrombosis, and some of these agents substantially increase the risk of heart attack. As a result, certain COX-2 selective inhibitors—such as rofecoxib—are no longer used due to the high risk of undiagnosed vascular disease.[10] These differential effects are due to the different roles and tissue localisations of each COX isoenzyme.[10] By inhibiting physiological COX activity, NSAIDs may cause deleterious effects on kidney function,[11] and, perhaps as a result of water and sodium retention and decreases in renal blood flow, may lead to heart problems.[12] In addition, NSAIDs can blunt the production of erythropoietin, resulting in anaemia, since haemoglobin needs this hormone to be produced.
The most prominent NSAIDs are aspirin, ibuprofen, and naproxen; all available over the counter (OTC) in most countries.[13] Paracetamol (acetaminophen) is generally not considered an NSAID because it has only minor anti-inflammatory activity. Paracetamol treats pain mainly by blocking COX-2 and inhibiting endocannabinoid reuptake almost exclusively within the brain, and only minimally in the rest of the body.[14][15]
Medical uses
NSAIDs are often suggested for the treatment of acute or chronic conditions where pain and inflammation are present. NSAIDs are generally used for the symptomatic relief of the following conditions:[16][17][18]
- Osteoarthritis[17][19][20]
- Rheumatoid arthritis[21]
- Mild-to-moderate pain due to inflammation and tissue injury[17]
- Low back pain[17][22]
- Inflammatory arthropathies (e.g., ankylosing spondylitis, psoriatic arthritis, reactive arthritis)
- Tennis elbow[23]
- Headache[17]
- Migraine[16]
- Acute gout[16]
- Dysmenorrhea (menstrual pain)[16]
- Metastatic bone pain[16]
- Postoperative pain[16]
- Muscle stiffness and pain due to Parkinson's disease[16]
- Pyrexia (fever)[16]
- Ileus[16]
- Renal colic[16]
- Macular edema[24]
- Traumatic injury[25]
The effectiveness of NSAIDs for treating non-cancer chronic pain and cancer-related pain in children and adolescents is not clear.[26][27] There have not been sufficient numbers of high-quality randomised controlled trials conducted.[26][27]
Inflammation
Differences in anti-inflammatory activity between the various individual NSAIDs are small, but there is considerable variation in individual patient response, and tolerance to these drugs. About 60% of patients will respond to any NSAID; of the others, those who do not respond to one may well respond to another. Pain relief starts soon after taking the first dose, and a full analgesic effect should normally be obtained within a week, whereas an anti-inflammatory effect may not be achieved (or may not be clinically assessable) for up to three weeks. If appropriate responses are not obtained within these times, another NSAID should be tried.[3]
Surgical pain
Pain following surgery can be significant, and many people require strong pain medications such as opioids. There is some low-certainty evidence that starting NSAID painkiller medications in adults early, before surgery, may help reduce post-operative pain, and also reduce the dose or quantity of opioid medications required after surgery.[28] Any increase risk of surgical bleeding, bleeding in the gastrointestinal system, myocardial infarctions, or injury to the kidneys has not been well studied.[28] When used in combination with paracetamol, the analgesic effect on post-operative pain may be improved.[29]
Aspirin
Aspirin, the only NSAID able to irreversibly inhibit COX-1, is also indicated for antithrombosis through inhibition of platelet aggregation. This is useful for the management of arterial thrombosis, and prevention of adverse cardiovascular events like heart attacks. Aspirin inhibits platelet aggregation by inhibiting the action of thromboxane A2.[30]
Dentistry
NSAIDs are useful in the management of post-operative dental pain following invasive dental procedures such as dental extraction. When not contra-indicated, they are favoured over the use of paracetamol alone due to the anti-inflammatory effect they provide.[31] There is weak evidence suggesting that taking pre-operative analgesia can reduce the length of post operative pain associated with placing orthodontic spacers under local anaesthetic.[32]
Contraindications
NSAIDs may be used with caution by people with the following conditions:
- Persons who are over age 50, and who have a family history of gastrointestinal (GI) problems[17]
- Persons who have had previous gastrointestinal problems from NSAID use[17]
NSAIDs should usually be avoided by people with the following conditions:
- Peptic ulcer or stomach bleeding[17]
- Uncontrolled hypertension[17]
- Kidney disease[17]
- People with inflammatory bowel disease (Crohn's disease or ulcerative colitis)[17]
- Past transient ischemic attack (excluding aspirin)[17]
- Past stroke (excluding aspirin)[17]
- Past myocardial infarction (excluding aspirin)[17]
- Coronary artery disease (excluding aspirin)[17]
- Undergoing coronary artery bypass surgery[17]
- Congestive heart failure (excluding low-dose aspirin)[33]
- In third trimester of pregnancy[17]
- Persons who have undergone gastric bypass surgery[34][35]
- Persons who have a history of allergic or allergic-like NSAID hypersensitivity reactions, e.g. aspirin-exacerbated respiratory disease[36]
Adverse effects
The widespread use of NSAIDs has meant that the adverse effects of these drugs have become increasingly common. Use of NSAIDs increases risk of a range of gastrointestinal (GI) problems, kidney disease and adverse cardiovascular events.[37][38] As commonly used for post-operative pain, there is evidence of increased risk of kidney complications.[39] Their use following gastrointestinal surgery remains controversial, given mixed evidence of increased risk of leakage from any bowel anastomosis created.[40][41][42]
An estimated 10–20% of people taking NSAIDs experience indigestion. In the 1990s high doses of prescription NSAIDs were associated with serious upper gastrointestinal adverse events, including bleeding.[43]
NSAIDs, like all medications, may interact with other medications. For example, concurrent use of NSAIDs and quinolone antibiotics may increase the risk of quinolones' adverse central nervous system effects, including seizure.[44][45]
There is an argument over the benefits and risks of NSAIDs for treating chronic musculoskeletal pain. Each drug has a benefit-risk profile and balancing the risk of no treatment with the competing potential risks of various therapies should be considered.[46] For people over the age of 65 years old, the balance between the benefits of pain-relief medications such as NSAIDS and the potential for adverse effects has not been well determined.[47]
There is some evidence suggesting that, for some people, use of NSAIDs (or other anti-inflammatories) may contribute to the initiation of chronic pain.[48]
In October 2020, the U.S. Food and Drug Administration (FDA) required the drug label to be updated for all nonsteroidal anti-inflammatory medications to describe the risk of kidney problems in unborn babies that result in low amniotic fluid.[49][50] They are recommending avoiding NSAIDs in pregnant women at 20 weeks or later in pregnancy.[49][50]
Combinational risk
If a COX-2 inhibitor is taken, a traditional NSAID (prescription or over-the-counter) should not be taken at the same time.[51]
Rofecoxib (Vioxx) was shown to produce significantly fewer gastrointestinal adverse drug reactions (ADRs) compared with naproxen.[52] The study, the VIGOR trial, raised the issue of the cardiovascular safety of the coxibs (COX-2 inhibitors). A statistically significant increase in the incidence of myocardial infarctions was observed in patients on rofecoxib. Further data, from the APPROVe trial, showed a statistically significant relative risk of cardiovascular events of 1.97 versus placebo[53]—which caused a worldwide withdrawal of rofecoxib in October 2004.[54]
Use of methotrexate together with NSAIDs in rheumatoid arthritis is safe, if adequate monitoring is done.[55]
Cardiovascular
NSAIDs, aside from aspirin, increase the risk of myocardial infarction and stroke.[56][57] This occurs at least within a week of use.[5] They are not recommended in those who have had a previous heart attack as they increase the risk of death or recurrent MI.[58] Evidence indicates that naproxen may be the least harmful out of these.[57][59]
NSAIDs aside from (low-dose) aspirin are associated with a doubled risk of heart failure in people without a history of cardiac disease.[59] In people with such a history, use of NSAIDs (aside from low-dose aspirin) was associated with a more than 10-fold increase in heart failure.[60] If this link is proven causal, researchers estimate that NSAIDs would be responsible for up to 20 percent of hospital admissions for congestive heart failure. In people with heart failure, NSAIDs increase mortality risk (hazard ratio) by approximately 1.2–1.3 for naproxen and ibuprofen, 1.7 for rofecoxib and celecoxib, and 2.1 for diclofenac.[61]
On 9 July 2015, the Food and Drug Administration (FDA) toughened warnings of increased heart attack and stroke risk associated with nonsteroidal anti-inflammatory drugs (NSAIDs) other than aspirin.[62]
Possible erectile dysfunction risk
A 2005 Finnish survey study found an association between long term (over three months) use of NSAIDs and erectile dysfunction.[63]
A 2011 publication[64] in The Journal of Urology received widespread publicity.[65] According to the study, men who used NSAIDs regularly were at significantly increased risk of erectile dysfunction. A link between NSAID use and erectile dysfunction still existed after controlling for several conditions. However, the study was observational and not controlled, with low original participation rate, potential participation bias, and other uncontrolled factors. The authors warned against drawing any conclusion regarding cause.[66]
Gastrointestinal
The main adverse drug reactions (ADRs) associated with NSAID use relate to direct and indirect irritation of the gastrointestinal (GI) tract. NSAIDs cause a dual assault on the GI tract: the acidic molecules directly irritate the gastric mucosa, and inhibition of COX-1 and COX-2 reduces the levels of protective prostaglandins.[37] Inhibition of prostaglandin synthesis in the GI tract causes increased gastric acid secretion, diminished bicarbonate secretion, diminished mucus secretion and diminished trophic effects on the epithelial mucosa.[67]
Common gastrointestinal side effects include:[16]
Clinical NSAID ulcers are related to the systemic effects of NSAID administration. Such damage occurs irrespective of the route of administration of the NSAID (e.g., oral, rectal, or parenteral) and can occur even in people who have achlorhydria.[69]
Ulceration risk increases with therapy duration, and with higher doses. To minimize GI side effects, it is prudent to use the lowest effective dose for the shortest period of time—a practice that studies show is often not followed. Over 50% of patients who take NSAIDs have sustained some mucosal damage to their small intestine.[70]
The risk and rate of gastric adverse effects is different depending on the type of NSAID medication a person is taking. Indomethacin, ketoprofen, and piroxicam use appear to lead to the highest rate of gastric adverse effects, while ibuprofen (lower doses) and diclofenac appear to have lower rates.[16]
Certain NSAIDs, such as aspirin, have been marketed in enteric-coated formulations that manufacturers claim reduce the incidence of gastrointestinal ADRs. Similarly, some believe that rectal formulations may reduce gastrointestinal ADRs. However, consistent with the systemic mechanism of such ADRs, and in clinical practice, these formulations have not demonstrated a reduced risk of GI ulceration.[16]
Numerous "gastro-protective" drugs have been developed with the goal of preventing gastrointestinal toxicity in people who need to take NSAIDs on a regular basis.[37] Gastric adverse effects may be reduced by taking medications that suppress acid production such as proton pump inhibitors (e.g.: omeprazole and esomeprazole), or by treatment with a drug that mimics prostaglandin in order to restore the lining of the GI tract (e.g.: a prostaglandin analog misoprostol).[37] Diarrhea is a common side effect of misoprostol; however, higher doses of misoprostol have been shown to reduce the risk of a person having a complication related to a gastric ulcer while taking NSAIDs.[37] While these techniques may be effective, they are expensive for maintenance therapy.[71]
Hydrogen sulfide NSAID hybrids prevent the gastric ulceration/bleeding associated with taking the NSAIDs alone. Hydrogen sulfide is known to have a protective effect on the cardiovascular and gastrointestinal system.[72]
Inflammatory bowel disease
NSAIDs should be used with caution in individuals with inflammatory bowel disease (e.g., Crohn's disease or ulcerative colitis) due to their tendency to cause gastric bleeding and form ulceration in the gastric lining.[73]
Renal
NSAIDs are also associated with a fairly high incidence of adverse drug reactions (ADRs) on the kidney and over time can lead to chronic kidney disease. The mechanism of these kidney ADRs is due to changes in kidney blood flow. Prostaglandins normally dilate the afferent arterioles of the glomeruli. This helps maintain normal glomerular perfusion and glomerular filtration rate (GFR), an indicator of kidney function. This is particularly important in kidney failure where the kidney is trying to maintain renal perfusion pressure by elevated angiotensin II levels. At these elevated levels, angiotensin II also constricts the afferent arteriole into the glomerulus in addition to the efferent arteriole it normally constricts. Since NSAIDs block this prostaglandin-mediated effect of afferent arteriole dilation, particularly in kidney failure, NSAIDs cause unopposed constriction of the afferent arteriole and decreased RPF (renal perfusion flow) and GFR.[74]
Common ADRs associated with altered kidney function include:[16]
- Sodium and fluid retention
- Hypertension (high blood pressure)
These agents may also cause kidney impairment, especially in combination with other nephrotoxic agents. Kidney failure is especially a risk if the patient is also concomitantly taking an ACE inhibitor (which removes angiotensin II's vasoconstriction of the efferent arteriole) and a diuretic (which drops plasma volume, and thereby RPF)—the so-called "triple whammy" effect.[75]
In rarer instances NSAIDs may also cause more severe kidney conditions:[16]
- Interstitial nephritis
- Nephrotic syndrome
- Acute kidney injury
- Acute tubular necrosis
- Renal papillary necrosis
NSAIDs in combination with excessive use of phenacetin or paracetamol (acetaminophen) may lead to analgesic nephropathy.[76]
Photosensitivity
Photosensitivity is a commonly overlooked adverse effect of many of the NSAIDs.[77] The 2-arylpropionic acids are the most likely to produce photosensitivity reactions, but other NSAIDs have also been implicated including piroxicam, diclofenac, and benzydamine.[78]
Benoxaprofen, since withdrawn due to its liver toxicity, was the most photoactive NSAID observed. The mechanism of photosensitivity, responsible for the high photoactivity of the 2-arylpropionic acids, is the ready decarboxylation of the carboxylic acid moiety. The specific absorbance characteristics of the different chromophoric 2-aryl substituents, affects the decarboxylation mechanism.[79]
During pregnancy
While NSAIDs as a class are not direct teratogens, use of NSAIDs in late pregnancy can cause premature closure of the fetal ductus arteriosus and kidney ADRs in the fetus.[80] Thus, NSAIDs are not recommended during the third trimester of pregnancy because of the increased risk of premature constriction of the ductus arteriosus.[80] Additionally, they are linked with premature birth[81] and miscarriage.[82] Aspirin, however, is used together with heparin in pregnant women with antiphospholipid syndrome.[83] Additionally, indomethacin can be used in pregnancy to treat polyhydramnios by reducing fetal urine production via inhibiting fetal renal blood flow.[84]
In contrast, paracetamol (acetaminophen) is regarded as being safe and well tolerated during pregnancy, but Leffers et al. released a study in 2010, indicating that there may be associated male infertility in the unborn.[85][86] Doses should be taken as prescribed, due to risk of liver toxicity with overdoses.[87]
In France, the country's health agency contraindicates the use of NSAIDs, including aspirin, after the sixth month of pregnancy.[88]
In October 2020, the U.S. Food and Drug Administration (FDA) required the drug label to be updated for all nonsteroidal anti-inflammatory medications to describe the risk of kidney problems in unborn babies that result in low amniotic fluid.[49][50] They are recommending avoiding NSAIDs in pregnant women at 20 weeks or later in pregnancy.[49][50]
Allergy and allergy-like hypersensitivity reactions
A variety of allergic or allergic-like NSAID hypersensitivity reactions follow the ingestion of NSAIDs. These hypersensitivity reactions differ from the other adverse reactions listed here which are toxicity reactions, i.e. unwanted reactions that result from the pharmacological action of a drug, are dose-related, and can occur in any treated individual; hypersensitivity reactions are idiosyncratic reactions to a drug.[89] Some NSAID hypersensitivity reactions are truly allergic in origin: 1) repetitive IgE-mediated urticarial skin eruptions, angioedema, and anaphylaxis following immediately to hours after ingesting one structural type of NSAID but not after ingesting structurally unrelated NSAIDs; and 2) Comparatively mild to moderately severe T cell-mediated delayed onset (usually more than 24 hour), skin reactions such as maculopapular rash, fixed drug eruptions, photosensitivity reactions, delayed urticaria, and contact dermatitis; or 3) far more severe and potentially life-threatening t-cell-mediated delayed systemic reactions such as the DRESS syndrome, acute generalized exanthematous pustulosis, the Stevens–Johnson syndrome, and toxic epidermal necrolysis. Other NSAID hypersensitivity reactions are allergy-like symptoms but do not involve true allergic mechanisms; rather, they appear due to the ability of NSAIDs to alter the metabolism of arachidonic acid in favor of forming metabolites that promote allergic symptoms. Affected individuals may be abnormally sensitive to these provocative metabolites or overproduce them and typically are susceptible to a wide range of structurally dissimilar NSAIDs, particularly those that inhibit COX1. Symptoms, which develop immediately to hours after ingesting any of various NSAIDs that inhibit COX-1, are: 1) exacerbations of asthmatic and rhinitis (see aspirin-exacerbated respiratory disease) symptoms in individuals with a history of asthma or rhinitis and 2) exacerbation or first-time development of wheals or angioedema in individuals with or without a history of chronic urticarial lesions or angioedema.[36]
Possible effects on bone and soft tissue healing
It has been hypothesized that NSAIDs may delay healing from bone and soft-tissue injuries by inhibiting inflammation.[90] On the other hand, it has also been hypothesized that NSAIDs might speed recovery from soft tissue injuries by preventing inflammatory processes from damaging adjacent, non-injured muscles.[91]
There is moderate evidence that they delay bone healing.[92] Their overall effect on soft-tissue healing is unclear.[91][90][93]
Ototoxicity
Long-term use of NSAID analgesics and paracetamol is associated with an increased risk of hearing loss.[94][95][96]
Other
The use of NSAIDs for analgesia following gastrointestinal surgery remains controversial, given mixed evidence of an increased risk of leakage from any bowel anastomosis created. This risk may vary according to the class of NSAID prescribed.[40][41][42]
Common adverse drug reactions (ADR), other than listed above, include: raised liver enzymes, headache, dizziness.[16] Uncommon ADRs include an abnormally high level of potassium in the blood, confusion, spasm of the airways, and rash.[16] Ibuprofen may also rarely cause irritable bowel syndrome symptoms. NSAIDs are also implicated in some cases of Stevens–Johnson syndrome.[97]
Most NSAIDs penetrate poorly into the central nervous system (CNS). However, the COX enzymes are expressed constitutively in some areas of the CNS, meaning that even limited penetration may cause adverse effects such as somnolence and dizziness.[98]
NSAIDs may increase the risk of bleeding in patients with Dengue fever[99] For this reason, NSAIDs are only available with a prescription in India.[100]
In very rare cases, ibuprofen can cause aseptic meningitis.[101]
As with other drugs, allergies to NSAIDs might exist. While many allergies are specific to one NSAID, up to 1 in 5 people may have unpredictable cross-reactive allergic responses to other NSAIDs as well.[102]
Drug interactions
NSAIDs reduce kidney blood flow and thereby decrease the efficacy of diuretics, and inhibit the elimination of lithium and methotrexate.[103]
NSAIDs cause decreased ability to form blood clots, which can increase the risk of bleeding when combined with other drugs that also decrease blood clotting, such as warfarin.[103]
NSAIDs may aggravate hypertension (high blood pressure) and thereby antagonize the effect of antihypertensives,[103] such as ACE inhibitors.[104]
NSAIDs may interfere and reduce effectiveness of SSRI antidepressants.[105][106] NSAIDs, when used in combination with SSRIs, increase the risk of adverse gastrointestinal effects.[107] NSAIDs, when used in combination with SSRIs, increase the risk of internal bleeding and brain hemorrhages.[108]
Various widely used NSAIDs enhance endocannabinoid signaling by blocking the anandamide-degrading membrane enzyme fatty acid amide hydrolase (FAAH).[109]
NSAIDs may reduce the effectiveness of antibiotics. Tests on cultured bacteria found that antibiotic effectiveness was reduced by 18–30% on average compared to tests which did not include NSAIDs.[110]
Immune response
Although small doses generally have little to no effect on the immune system, large doses of NSAIDs significantly suppress the production of immune cells.[111] As NSAIDs affect prostaglandins, they affect the production of most fast growing cells.[111] This includes immune cells.[111] Unlike corticosteroids, they do not directly suppress the immune system and so their effect on the immune system is not immediately obvious.[111] They suppress the production of new immune cells, but leave existing immune cells functional.[111] Large doses slowly reduce the immune response as the immune cells are renewed at a much lower rate.[111] Causing a gradual reduction of the immune system, much slower and less noticeable than the immediate effect of Corticosteroids.[111] The effect significantly increases with dosage, in a nearly exponential rate.[111] Doubling of dose reduced cells by nearly four times.[111] Increasing dose by five times reduced cell counts to only a few percent of normal levels.[111] This is likely why the effect was not immediately obvious in low dose trials, as the effect is not apparent until much higher dosages are tested.[111]
Mechanism of action
Most NSAIDs act as nonselective inhibitors of the cyclooxygenase (COX) enzymes, inhibiting both the cyclooxygenase-1 (COX-1) and cyclooxygenase-2 (COX-2) isoenzymes. This inhibition is competitively reversible (albeit at varying degrees of reversibility), as opposed to the mechanism of aspirin, which is irreversible inhibition.[112] COX catalyzes the formation of prostaglandins and thromboxane from arachidonic acid (itself derived from the cellular phospholipid bilayer by phospholipase A2). Prostaglandins act (among other things) as messenger molecules in the process of inflammation. This mechanism of action was elucidated in 1970 by John Vane (1927–2004), who received a Nobel Prize for his work (see Mechanism of action of aspirin).[113][114]
COX-1 is a constitutively expressed enzyme with a "house-keeping" role in regulating many normal physiological processes. One of these is in the stomach lining, where prostaglandins serve a protective role, preventing the stomach mucosa from being eroded by its own acid. COX-2 is an enzyme facultatively expressed in inflammation, and it is inhibition of COX-2 that produces the desirable effects of NSAIDs.[115]
When nonselective COX-1/COX-2 inhibitors (such as aspirin, ibuprofen, and naproxen) lower stomach prostaglandin levels, ulcers of the stomach or duodenum and internal bleeding can result.[116] The discovery of COX-2 led to research to the development of selective COX-2 inhibiting drugs that do not cause gastric problems characteristic of older NSAIDs.[117]
NSAIDs have been studied in various assays to understand how they affect each of these enzymes. While the assays reveal differences, unfortunately, different assays provide differing ratios.[118]
Paracetamol (acetaminophen) is not considered an NSAID because it has little anti-inflammatory activity. It treats pain mainly by blocking COX-2 mostly in the central nervous system, but not much in the rest of the body.[14]
However, many aspects of the mechanism of action of NSAIDs remain unexplained, and for this reason, further COX pathways are hypothesized. The COX-3 pathway was believed to fill some of this gap but recent findings make it appear unlikely that it plays any significant role in humans and alternative explanation models are proposed.[14]
NSAIDs interact with the endocannabinoid system and its endocannabinoids, as COX2 have been shown to utilize endocannabinoids as substrates, and may have a key role in both the therapeutic effects and adverse effects of NSAIDs, as well as in NSAID-induced placebo responses.[119][120][121]
NSAIDs are also used in the acute pain caused by gout because they inhibit urate crystal phagocytosis besides inhibition of prostaglandin synthase.[122]
Antipyretic activity
NSAIDs have antipyretic activity and can be used to treat fever.[123][124] Fever is caused by elevated levels of prostaglandin E2 (PGE2), which alters the firing rate of neurons within the hypothalamus that control thermoregulation.[123][125] Antipyretics work by inhibiting the enzyme COX, which causes the general inhibition of prostanoid biosynthesis (PGE2) within the hypothalamus.[123][124] PGE2 signals to the hypothalamus to increase the body's thermal setpoint.[124][126] Ibuprofen has been shown more effective as an antipyretic than paracetamol (acetaminophen).[125][127] Arachidonic acid is the precursor substrate for cyclooxygenase leading to the production of prostaglandins F, D, and E.[128]
Classification
NSAIDs can be classified based on their chemical structure or mechanism of action. Older NSAIDs were known long before their mechanism of action was elucidated and were for this reason classified by chemical structure or origin. Newer substances are more often classified by mechanism of action.[129]
Salicylates
- Aspirin (acetylsalicylic acid)
- Diflunisal (Dolobid)
- Salicylic acid and its salts
- Salsalate (Disalcid)
Propionic acid derivatives
- Ibuprofen[130]
- Dexibuprofen
- Naproxen
- Fenoprofen
- Ketoprofen
- Dexketoprofen
- Flurbiprofen
- Oxaprozin
- Loxoprofen
- Pelubiprofen
- Zaltoprofen
- Fenbufen
- Tiaprofenic acid
- Carprofen
Acetic acid derivatives
- Indomethacin
- Acemetacin
- Tolmetin
- Sulindac
- Etodolac
- Ketorolac[25]
- Diclofenac
- Fenclofenac
- Aceclofenac
- Bromfenac
- Fentiazac
- Nabumetone (drug itself is non-acidic but the active, principal metabolite has a carboxylic acid group)
Enolic acid (oxicam) derivatives
- Piroxicam
- Meloxicam
- Tenoxicam
- Droxicam
- Lornoxicam
- Isoxicam (withdrawn from market 1985[131][132])
- Phenylbutazone (Bute)
Anthranilic acid derivatives (Fenamates)
The following NSAIDs are derived from fenamic acid, which is a derivative of anthranilic acid,[133]:235 which in turn is a nitrogen isostere of salicylic acid, which is the active metabolite of aspirin.[133]:235[134]:17
Selective COX-2 inhibitors (Coxibs)
- Celecoxib (FDA alert[135])
- Rofecoxib (withdrawn from market[136])
- Valdecoxib (withdrawn from market[137])
- Parecoxib FDA withdrawn, licensed in the EU
- Lumiracoxib TGA cancelled registration
- Etoricoxib not FDA approved, licensed in the EU
- Firocoxib used in dogs and horses
Sulfonanilides
- Nimesulide (systemic preparations are banned by several countries for the potential risk of hepatotoxicity)[138]
Others
- Clonixin
- Licofelone acts by inhibiting LOX (lipooxygenase) and COX and hence known as 5-LOX/COX inhibitor
- H-harpagide in figwort[139] or devil's claw[140]
Chirality
Most NSAIDs are chiral molecules; diclofenac and the oxicams are exceptions. However, the majority are prepared as racemic mixtures. Typically, only a single enantiomer is pharmacologically active. For some drugs (typically profens), an isomerase enzyme in vivo converts the inactive enantiomer into the active form, although its activity varies widely in individuals. This phenomenon is likely responsible for the poor correlation between NSAID efficacy and plasma concentration observed in older studies when specific analysis of the active enantiomer was not performed.
Ibuprofen and ketoprofen are now available in single-enantiomer preparations (dexibuprofen and dexketoprofen), which purport to offer quicker onset and an improved side-effect profile. Naproxen has always been marketed as the single active enantiomer.
Main practical differences
NSAIDs within a group tend to have similar characteristics and tolerability. There is little difference in clinical efficacy among the NSAIDs when used at equivalent doses.[141] Rather, differences among compounds usually relate to dosing regimens (related to the compound's elimination half-life), route of administration, and tolerability profile.
Regarding adverse effects, selective COX-2 inhibitors have lower risk of gastrointestinal bleeding.[141] With the exception of naproxen, nonselective NSAIDs increase the risk of having a heart attack.[141] Some data also supports that the partially selective nabumetone is less likely to cause gastrointestinal events.[141]
A consumer report noted that ibuprofen, naproxen, and salsalate are less expensive than other NSAIDs, and essentially as effective and safe when used appropriately to treat osteoarthritis and pain.[142]
Pharmacokinetics
Most nonsteroidal anti-inflammatory drugs are weak acids,[143] with a pKa of 3–5. They are absorbed well from the stomach and intestinal mucosa. They are highly protein-bound in plasma (typically >95%), usually to albumin, so that their volume of distribution typically approximates to plasma volume. Most NSAIDs are metabolized in the liver by oxidation and conjugation to inactive metabolites that typically are excreted in the urine, though some drugs are partially excreted in bile. Metabolism may be abnormal in certain disease states, and accumulation may occur even with normal dosage.
Ibuprofen and diclofenac have short half-lives (2–3 hours). Some NSAIDs (typically oxicams) have very long half-lives (e.g. 20–60 hours).
History
It is widely believed that naturally occurring salicin in willow trees and other plants was used by the ancients as a form of analgesic or anti-inflammatory drug,[144] but this story, although compelling, is not entirely true.[145][146] Hippocrates does not mention willow at all.[147] Dioscorides's De materia medica was arguably the most influential herbal from Roman to Medieval times but, if he mentions willow at all (there is doubt about the identity of 'Itea'), then he used the ashes, steeped in vinegar, as a treatment for corns,[148] which corresponds well with modern uses of salicylic acid.
Willow bark (from trees of the Salix genus) was widely known to be used as a medicine by multiple First Nations communities.[149] The bark would be chewed or steeped in water for its pain relieving and antipyretic effects. The effects are a result of the bark's salicin content. Meadowsweet, another plant to contain salicin, has strong roots in British folk medicine for the same maladies. Willow bark was first reported in Western science by Edward Stone in 1763 as a treatment for ague (fever) according to the pseudoscientific doctrine of signatures.[150]
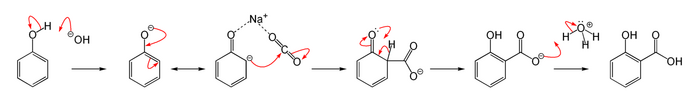
In the body, salicin is turned into salicylic acid, which produces the antipyretic and analgesic effects that the plants are known for.
Salicin was first isolated by Johann Andreas Buchner in 1827. By 1829, French chemist Henri Leroux had improved the extraction process to obtain about 30g of purified salicin from 1.5 kg of willow bark.[151] By hydrolysis, salicin releases glucose and salicyl alcohol which can be converted into salicylic acid, both in vivo and through chemical methods.[152] In 1869, Hermann Kolbe synthesised salicylic acid, although it was too acidic for the gastric mucosa.[152] The reaction used to synthesise aromatic acid from a phenol in the presence of CO
2 is known as the Kolbe-Schmitt reaction.[153][154][155]
By 1897 the German chemist Felix Hoffmann and the Bayer company prompted a new age of pharmacology by converting salicylic acid into acetylsalicylic acid—named aspirin by Heinrich Dreser. Other NSAIDs like ibuprofen were developed from the 1950s forward.[151] In 2001, NSAIDs accounted for 70,000,000 prescriptions and 30 billion over-the-counter doses sold annually in the United States .[43]
Research
While studies have been conducted to see if various NSAIDs can improve behavior in transgenic mouse models of Alzheimer's disease and observational studies in humans have shown promise, there is no good evidence from randomized clinical trials that NSAIDs can treat or prevent Alzheimer's in humans; clinical trials of NSAIDs for treatment of Alzheimer's have found more harm than benefit.[156][157][158] NSAIDs coordinate with metal ions affecting cellular function.[159]
Veterinary use
Research supports the use of NSAIDs for the control of pain associated with veterinary procedures such as dehorning and castration of calves.[citation needed] The best effect is obtained by combining a short-term local anesthetic such as lidocaine with an NSAID acting as a longer term analgesic.[citation needed] However, as different species have varying reactions to different medications in the NSAID family, little of the existing research data can be extrapolated to animal species other than those specifically studied, and the relevant government agency in one area sometimes prohibits uses approved in other jurisdictions.[citation needed]
In the United States, meloxicam is approved for use only in canines, whereas (due to concerns about liver damage) it carries warnings against its use in cats[160][161] except for one-time use during surgery.[162] In spite of these warnings, meloxicam is frequently prescribed "off-label" for non-canine animals including cats and livestock species.[163] In other countries, for example The European Union (EU), there is a label claim for use in cats.[164]
See also
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 "non-steroidal anti-inflammatory drug". Oxford English Dictionary. 2022. https://www.lexico.com/definition/non-steroidal_anti-inflammatory_drug.
- ↑ 2.0 2.1 "Studies of local anesthetic action on natural spike activity in the aortic nerve of cats". Anesthesiology (Ovid Technologies (Wolters Kluwer Health)) 66 (2): 210–3. February 1987. doi:10.1097/00000542-198702000-00016. PMID 3813081. "Non-steroidal anti-inflammatory drugs (NSAIDs) are the competitive inhibitors of cyclooxygenase (COX), the enzyme which mediates the bioconversion of arachidonic acid to inflammatory prostaglandins (PGs).".
- ↑ 3.0 3.1 "Non-steroidal anti-inflammatory drugs". British National Formulary (BNF), National Institute for Health and Care Excellence (NICE). 2022. https://BNF.NICE.org.uk/treatment-summary/non-steroidal-anti-inflammatory-drugs.html.
- ↑ Mallinson, Tom Edward (2017-12-02). "A review of ketorolac as a prehospital analgesic" (in en). Journal of Paramedic Practice 9 (12): 522–526. doi:10.12968/jpar.2017.9.12.522. ISSN 1759-1376.
- ↑ 5.0 5.1 "Risk of acute myocardial infarction with NSAIDs in real world use: bayesian meta-analysis of individual patient data". The BMJ 357: j1909. May 2017. doi:10.1136/bmj.j1909. PMID 28487435.
- ↑ "Peptic ulcer disease". The Lancet 390 (10094): 613–624. August 2017. doi:10.1016/S0140-6736(16)32404-7. PMID 28242110.
- ↑ "Origins and impact of the term 'NSAID'". Inflammopharmacology 22 (5): 263–267. October 2014. doi:10.1007/s10787-014-0211-2. PMID 25064056.
- ↑ "Old and new drugs used in rheumatoid arthritis: a historical perspective. Part 1: the older drugs". American Journal of Therapeutics 8 (2): 123–143. 2001. doi:10.1097/00045391-200103000-00007. PMID 11304666.
- ↑ The Rise and Fall of Modern Medicine. Abacus. 2011. p. 34.
- ↑ 10.0 10.1 10.2 10.3 "The Vascular Effects of COX-2 selective inhibitors". Australian Prescriber 27 (6): 142–145. 2004. doi:10.18773/austprescr.2004.119.
- ↑ "Renal effects of COX-2-selective inhibitors". American Journal of Nephrology 21 (1): 1–15. January 2001. doi:10.1159/000046212. PMID 11275626.
- ↑ "Nonsteroidal anti-inflammatory drugs and heart failure". Drugs 63 (6): 525–34. 2003. doi:10.2165/00003495-200363060-00001. PMID 12656651.
- ↑ "Prophylactic use of NSAIDs by athletes: a risk / benefit assessment". The Physician and Sportsmedicine 38 (1): 132–8. April 2010. doi:10.3810/psm.2010.04.1770. PMID 20424410.
- ↑ 14.0 14.1 14.2 "Acetaminophen (paracetamol) is a selective cyclooxygenase-2 inhibitor in man". FASEB Journal 22 (2): 383–90. February 2008. doi:10.1096/fj.07-8506com. PMID 17884974.
- ↑ (in Spanish) Farmacología integrada. Elsevier España. 1998. ISBN 84-8174-340-2. https://books.google.com/books?id=h7cxH6XH4-sC.
- ↑ 16.00 16.01 16.02 16.03 16.04 16.05 16.06 16.07 16.08 16.09 16.10 16.11 16.12 16.13 16.14 16.15 16.16 Simone Rossi, ed (2006). Australian medicines handbook 2006. Adelaide: Australian Medicines Handbook Pty Ltd. ISBN 978-0-9757919-2-9.[page needed]
- ↑ 17.00 17.01 17.02 17.03 17.04 17.05 17.06 17.07 17.08 17.09 17.10 17.11 17.12 17.13 17.14 17.15 17.16 Consumer Reports Health Best Buy Drugs (July 2013), "The Nonsteroidal Anti-Inflammatory Drugs: Treating Osteoarthritis and Pain. Comparing effectiveness, safety, and price.", NSAIDs, Yonkers, New York: Consumer Reports, http://consumerhealthchoices.org/wp-content/uploads/2012/02/BBD-NSAIDs-Full.pdf, retrieved 12 February 2014
- ↑ "Non-steroidal anti-inflammatory drugs for spinal pain: a systematic review and meta-analysis". Annals of the Rheumatic Diseases 76 (7): 1269–1278. July 2017. doi:10.1136/annrheumdis-2016-210597. PMID 28153830. https://ard.bmj.com/content/76/7/1269.
- ↑ "Acetaminophen for osteoarthritis". The Cochrane Database of Systematic Reviews 2010 (1): CD004257. January 2006. doi:10.1002/14651858.CD004257.pub2. PMID 16437479.
- ↑ "Topical NSAIDs for chronic musculoskeletal pain in adults". The Cochrane Database of Systematic Reviews 4 (4): CD007400. April 2016. doi:10.1002/14651858.CD007400.pub3. PMID 27103611.
- ↑ "Methodology and overt and hidden bias in reports of 196 double-blind trials of nonsteroidal antiinflammatory drugs in rheumatoid arthritis". Controlled Clinical Trials 10 (1): 31–56. March 1989. doi:10.1016/0197-2456(89)90017-2. PMID 2702836.
- ↑ "Cochrane Database of Systematic Reviews", The Cochrane Database of Systematic Reviews 2008 (1): CD000396, 2008, doi:10.1002/14651858.CD000396.pub3, PMID 18253976
- ↑ "Cochrane Database of Systematic Reviews", The Cochrane Database of Systematic Reviews 5 (5): CD003686, 2013, doi:10.1002/14651858.CD003686.pub2, PMID 23728646
- ↑ "Prophylactic non-steroidal anti-inflammatory drugs for the prevention of macular oedema after cataract surgery". The Cochrane Database of Systematic Reviews 2016 (11): CD006683. November 2016. doi:10.1002/14651858.CD006683.pub3. PMID 27801522.
- ↑ 25.0 25.1 "A review of ketorolac as a prehospital analgesic". Journal of Paramedic Practice 9 (12): 522–526. 2017. doi:10.12968/jpar.2017.9.12.522. https://www.researchgate.net/publication/321640488. Retrieved 2 June 2018.
- ↑ 26.0 26.1 "Non-steroidal anti-inflammatory drugs (NSAIDs) for chronic non-cancer pain in children and adolescents". The Cochrane Database of Systematic Reviews 8 (8): CD012537. August 2017. doi:10.1002/14651858.CD012537.pub2. PMID 28770976.
- ↑ 27.0 27.1 "Non-steroidal anti-inflammatory drugs (NSAIDs) for cancer-related pain in children and adolescents". The Cochrane Database of Systematic Reviews 7 (10): CD012563. July 2017. doi:10.1002/14651858.CD012563.pub2. PMID 28737843.
- ↑ 28.0 28.1 "Pre-emptive and preventive NSAIDs for postoperative pain in adults undergoing all types of surgery". The Cochrane Database of Systematic Reviews 2021 (6): CD012978. June 2021. doi:10.1002/14651858.CD012978.pub2. PMID 34125958.
- ↑ "Single dose oral analgesics for acute postoperative pain in adults - an overview of Cochrane reviews". The Cochrane Database of Systematic Reviews 2015 (9): CD008659. September 2015. doi:10.1002/14651858.CD008659.pub3. PMID 26414123.
- ↑ (in German) Arzneimittelwirkungen. Wissenschaftliche Verlagsgesellschaft Stuttgart. 2013. p. 473. ISBN 978-3-8047-2898-1.
- ↑ "Drug Prescribing for Dentistry". Scottish Dental Clinical Effectiveness Programme, NHS Education for Scotland. January 2016. https://www.SDCEP.org.uk/published-guidance/drug-prescribing/.
- ↑ "Preoperative analgesics for additional pain relief in children and adolescents having dental treatment". The Cochrane Database of Systematic Reviews 2016 (8): CD008392. August 2016. doi:10.1002/14651858.CD008392.pub3. PMID 27501304. PMC 8568367. http://discovery.ucl.ac.uk/1508941/1/Ashley_et_al-2016-The_Cochrane_Library.pdf.
- ↑ "Safety of non-steroidal anti-inflammatory drugs in patients with cardiovascular disease". Pharmacotherapy 35 (5): 520–35. May 2015. doi:10.1002/phar.1584. PMID 25940579.
- ↑ "Predictors of endoscopic findings after Roux-en-Y gastric bypass". The American Journal of Gastroenterology 101 (10): 2194–9. October 2006. doi:10.1111/j.1572-0241.2006.00770.x. PMID 17032183.
- ↑ "Long term medical issues associated after Roux-en-Y Gastric Bypass Procedure (RYGBP)". SSMHealth. http://www.SSMHealth.com/weightloss/documents/infosheet-pcp-longterm-medissues.pdf.
- ↑ 36.0 36.1 "Classification and practical approach to the diagnosis and management of hypersensitivity to nonsteroidal anti-inflammatory drugs". Allergy 68 (10): 1219–32. October 2013. doi:10.1111/all.12260. PMID 24117484.
- ↑ 37.0 37.1 37.2 37.3 37.4 37.5 "Prevention of NSAID-induced gastroduodenal ulcers". The Cochrane Database of Systematic Reviews 2011 (4): CD002296. 2002. doi:10.1002/14651858.CD002296. PMID 12519573.
- ↑ "Medications - non-steroidal anti-inflammatory drugs" (in en). U.S. Department of Health & Human Services. https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/medications-non-steroidal-anti-inflammatory-drugs.
- ↑ "Effects of nonsteroidal anti-inflammatory drugs on postoperative renal function in adults with normal renal function". The Cochrane Database of Systematic Reviews 2018 (2): CD002765. April 2007. doi:10.1002/14651858.CD002765.pub3. PMID 17443518.
- ↑ 40.0 40.1 StarSurg Collaborative (January 2017). "Safety of Nonsteroidal Anti-inflammatory Drugs in Major Gastrointestinal Surgery: A Prospective, Multicenter Cohort Study". World Journal of Surgery 41 (1): 47–55. doi:10.1007/s00268-016-3727-3. PMID 27766396.
- ↑ 41.0 41.1 StarSurg Collaborative (October 2014). "Impact of postoperative non-steroidal anti-inflammatory drugs on adverse events after gastrointestinal surgery". The British Journal of Surgery 101 (11): 1413–23. doi:10.1002/bjs.9614. PMID 25091299.
- ↑ 42.0 42.1 "Postoperative nonsteroidal anti-inflammatory drugs and risk of anastomotic leak: meta-analysis of clinical and experimental studies". World Journal of Surgery 38 (9): 2247–57. September 2014. doi:10.1007/s00268-014-2531-1. PMID 24682313.
- ↑ 43.0 43.1 "Understanding NSAIDs: from aspirin to COX-2". Clinical Cornerstone 3 (5): 50–60. 2001. doi:10.1016/S1098-3597(01)90069-9. PMID 11464731.
- ↑ Bayer HealthCare Pharmaceuticals Inc (September 2008). "Cipro Medication Guide". Food and Drug Administration (FDA). http://www.accessdata.fda.gov/drugsatfda_docs/label/2008/019537s68,19847s42,19857s49,20780s26,21473s24lbl.pdf.
- ↑ Royal Pharmaceutical Society of Great Britain (2009). "5 Infections". British National Formulary (BNF 57). BMJ Group and RPS Publishing. ISBN 978-0-85369-845-6.
- ↑ "Relative benefit-risk comparing diclofenac to other traditional non-steroidal anti-inflammatory drugs and cyclooxygenase-2 inhibitors in patients with osteoarthritis or rheumatoid arthritis: a network meta-analysis". Arthritis Research & Therapy 17 (1): 66. March 2015. doi:10.1186/s13075-015-0554-0. PMID 25879879.
- ↑ "Oral non-steroidal anti-inflammatory drugs versus other oral analgesic agents for acute soft tissue injury". The Cochrane Database of Systematic Reviews 2020 (8): CD007789. August 2020. doi:10.1002/14651858.CD007789.pub3. PMID 32797734.
- ↑ "Acute inflammatory response via neutrophil activation protects against the development of chronic pain". Science Translational Medicine 14 (644): eabj9954. 11 May 2022. doi:10.1126/scitranslmed.abj9954. PMID 35544595.
- ↑ 49.0 49.1 49.2 49.3
 One or more of the preceding sentences incorporates text from a work now in the public domain: "FDA Warns that Using a Type of Pain and Fever Medication in Second Half of Pregnancy Could Lead to Complications". U.S. Food and Drug Administration (FDA) (Press release). 15 October 2020. Retrieved 15 October 2020.
One or more of the preceding sentences incorporates text from a work now in the public domain: "FDA Warns that Using a Type of Pain and Fever Medication in Second Half of Pregnancy Could Lead to Complications". U.S. Food and Drug Administration (FDA) (Press release). 15 October 2020. Retrieved 15 October 2020.
- ↑ 50.0 50.1 50.2 50.3
 One or more of the preceding sentences incorporates text from a work now in the public domain: "NSAIDs may cause rare kidney problems in unborn babies". 21 July 2017. https://www.fda.gov/drugs/drug-safety-and-availability/fda-recommends-avoiding-use-nsaids-pregnancy-20-weeks-or-later-because-they-can-result-low-amniotic.
One or more of the preceding sentences incorporates text from a work now in the public domain: "NSAIDs may cause rare kidney problems in unborn babies". 21 July 2017. https://www.fda.gov/drugs/drug-safety-and-availability/fda-recommends-avoiding-use-nsaids-pregnancy-20-weeks-or-later-because-they-can-result-low-amniotic.
- ↑ "What Are NSAIDs?". http://orthoinfo.aaos.org/fact/thr_report.cfm?Thread_ID=398&topcategory=About.
- ↑ "Comparison of upper gastrointestinal toxicity of rofecoxib and naproxen in patients with rheumatoid arthritis. VIGOR Study Group". The New England Journal of Medicine 343 (21): 1520–8, 2 p following 1528. November 2000. doi:10.1056/NEJM200011233432103. PMID 11087881.
- ↑ "Cardiovascular events associated with rofecoxib: final analysis of the APPROVe trial". The Lancet 372 (9651): 1756–64. November 2008. doi:10.1016/S0140-6736(08)61490-7. PMID 18922570.
- ↑ "Rofecoxib (Vioxx) voluntarily withdrawn from market". CMAJ 171 (9): 1027–8. October 2004. doi:10.1503/cmaj.1041606. PMID 15505253.
- ↑ "Safety of non-steroidal anti-inflammatory drugs, including aspirin and paracetamol (acetaminophen) in people receiving methotrexate for inflammatory arthritis (rheumatoid arthritis, ankylosing spondylitis, psoriatic arthritis, other spondyloarthritis)". The Cochrane Database of Systematic Reviews (11): CD008872. November 2011. doi:10.1002/14651858.CD008872.pub2. PMID 22071858.
- ↑ "Do selective cyclo-oxygenase-2 inhibitors and traditional non-steroidal anti-inflammatory drugs increase the risk of atherothrombosis? Meta-analysis of randomised trials". BMJ 332 (7553): 1302–8. June 2006. doi:10.1136/bmj.332.7553.1302. PMID 16740558.
- ↑ 57.0 57.1 "Cardiovascular safety of non-steroidal anti-inflammatory drugs: network meta-analysis". BMJ 342 (jan11 1): c7086. January 2011. doi:10.1136/bmj.c7086. PMID 21224324.
- ↑ "Duration of treatment with nonsteroidal anti-inflammatory drugs and impact on risk of death and recurrent myocardial infarction in patients with prior myocardial infarction: a nationwide cohort study". Circulation 123 (20): 2226–35. May 2011. doi:10.1161/CIRCULATIONAHA.110.004671. PMID 21555710.
- ↑ 59.0 59.1 "Vascular and upper gastrointestinal effects of non-steroidal anti-inflammatory drugs: meta-analyses of individual participant data from randomised trials". The Lancet 382 (9894): 769–79. August 2013. doi:10.1016/S0140-6736(13)60900-9. PMID 23726390.
- ↑ "Consumption of NSAIDs and the development of congestive heart failure in elderly patients: an underrecognized public health problem". Archives of Internal Medicine 160 (6): 777–84. March 2000. doi:10.1001/archinte.160.6.777. PMID 10737277.
- ↑ "Increased mortality and cardiovascular morbidity associated with use of nonsteroidal anti-inflammatory drugs in chronic heart failure". Archives of Internal Medicine 169 (2): 141–9. January 2009. doi:10.1001/archinternmed.2008.525. PMID 19171810.
- ↑ Staff (9 July 2015). "FDA Strengthens Warning of Heart Attack and Stroke Risk for Non-Steroidal Anti-Inflammatory Drugs". Food and Drug Administration (FDA). https://www.fda.gov/ForConsumers/ConsumerUpdates/ucm453610.htm.
- ↑ "Effect of nonsteroidal anti-inflammatory drug use on the incidence of erectile dysfunction". The Journal of Urology 175 (5): 1812–5; discussion 1815–6. May 2006. doi:10.1016/S0022-5347(05)01000-1. PMID 16600768. http://www.jurology.com/article/S0022-5347%2805%2901000-1/abstract.
- ↑ "Regular nonsteroidal anti-inflammatory drug use and erectile dysfunction". The Journal of Urology 185 (4): 1388–93. April 2011. doi:10.1016/j.juro.2010.11.092. PMID 21334642. http://www.jurology.com/article/S0022-5347(10)05203-1/abstract. Retrieved 21 July 2014.
- ↑ "Regular NSAID Use Linked to Erectile Dysfunction". 8 March 2011. http://www.medscape.org/viewarticle/738584.
- ↑ "NSAID Use Tied to Men's Sexual Performance". 5 March 2011. https://www.medpagetoday.org/urology/erectiledysfunction/25204.
- ↑ "Prostaglandins, NSAIDs, and gastric mucosal protection: why doesn't the stomach digest itself?". Physiological Reviews 88 (4): 1547–1565. October 2008. doi:10.1152/physrev.00004.2008. PMID 18923189.
- ↑ "Gastroduodenal toxicity of different nonsteroidal antiinflammatory drugs". Epidemiology 6 (1): 49–54. January 1995. doi:10.1097/00001648-199501000-00010. PMID 7888445.
- ↑ Textbook of Gastroenterology, Tadataka Yamada, 2008, Ch.40, Peptic Ulcer Disease, page 941
- ↑ "Present status and strategy of NSAIDs-induced small bowel injury". Journal of Gastroenterology 44 (9): 879–88. July 2009. doi:10.1007/s00535-009-0102-2. PMID 19568687.
- ↑ "Effective and safe proton pump inhibitor therapy in acid-related diseases - A position paper addressing benefits and potential harms of acid suppression". BMC Medicine 14 (1): 179. November 2016. doi:10.1186/s12916-016-0718-z. PMID 27825371.
- ↑ "Hydrogen sulfide and translational medicine" (in En). Acta Pharmacologica Sinica 34 (10): 1284–91. October 2013. doi:10.1038/aps.2013.127. PMID 24096643.
- ↑ "Role of Nonsteroidal Anti-Inflammatory Drugs in Exacerbations of Inflammatory Bowel Disease". Journal of Clinical Gastroenterology 50 (2): 152–6. February 2016. doi:10.1097/MCG.0000000000000421. PMID 26485106.
- ↑ "Nonsteroidal Anti-Inflammatory Drugs and the Kidney". Pharmaceuticals 3 (7): 2291–2321. July 2010. doi:10.3390/ph3072291. PMID 27713354.
- ↑ "Diuretics, ACE inhibitors and NSAIDs--the triple whammy". The Medical Journal of Australia 172 (4): 184–5. February 2000. doi:10.5694/j.1326-5377.2000.tb125548.x. PMID 10772593.
- ↑ "Analgesic nephropathy". The New England Journal of Medicine 338 (7): 446–52. February 1998. doi:10.1056/NEJM199802123380707. PMID 9459649.
- ↑ "Drug-induced cutaneous photosensitivity: incidence, mechanism, prevention and management". Drug Safety 25 (5): 345–372. 2002. doi:10.2165/00002018-200225050-00004. PMID 12020173.
- ↑ "Latest Evidence Regarding the Effects of Photosensitive Drugs on the Skin: Pathogenetic Mechanisms and Clinical Manifestations". Pharmaceutics 12 (11): 1104. November 2020. doi:10.3390/pharmaceutics12111104. PMID 33213076.
- ↑ "Computational Studies of the Photodegradation Mechanism of the Highly Phototoxic Agent Benoxaprofen". ACS Omega 7 (33): 29475–29482. August 2022. doi:10.1021/acsomega.2c03118. PMID 36033698.
- ↑ 80.0 80.1 "Nonsteroidal antiinflammatory drugs during third trimester and the risk of premature closure of the ductus arteriosus: a meta-analysis". The Annals of Pharmacotherapy 40 (5): 824–829. May 2006. doi:10.1345/aph.1G428. PMID 16638921.
- ↑ "Anti-inflammatory pharmacotherapy during pregnancy". Expert Opinion on Pharmacotherapy 5 (3): 571–580. March 2004. doi:10.1517/14656566.5.3.571. PMID 15013926.
- ↑ "Use of nonaspirin nonsteroidal anti-inflammatory drugs during pregnancy and the risk of spontaneous abortion". CMAJ 183 (15): 1713–1720. October 2011. doi:10.1503/cmaj.110454. PMID 21896698.
- ↑ "The management of pregnant patients with antiphospholipid syndrome". Lupus 13 (9): 683–687. 2004. doi:10.1191/0961203304lu1092oa. PMID 15485103.
- ↑ "Polyhydramnios: Causes, Diagnosis and Therapy" (in de). Geburtshilfe und Frauenheilkunde 73 (12): 1241–1246. December 2013. doi:10.1055/s-0033-1360163. PMID 24771905.
- ↑ "Tolerability of paracetamol". Drug Safety 28 (3): 227–40. 2005. doi:10.2165/00002018-200528030-00004. PMID 15733027.
- ↑ "Intrauterine exposure to mild analgesics is a risk factor for development of male reproductive disorders in human and rat". Human Reproduction 26 (1): 235–44. January 2011. doi:10.1093/humrep/deq323. PMID 21059752.
- ↑ "Acetaminophen overdose in pregnancy". Southern Medical Journal 98 (11): 1118–22. November 2005. doi:10.1097/01.smj.0000184792.15407.51. PMID 16351032.
- ↑ "Grossesse – Mamans attention" (in fr). France Soir. 2 March 2009. http://www.francesoir.fr/societe/2009/03/02/grossesse-mamans-attention.html.
- ↑ "Seven steps to the diagnosis of NSAIDs hypersensitivity: how to apply a new classification in real practice?". Allergy, Asthma & Immunology Research 7 (4): 312–20. July 2015. doi:10.4168/aair.2015.7.4.312. PMID 25749768.
- ↑ 90.0 90.1 "Effects of Perioperative Nonsteroidal Anti-inflammatory Drug Administration on Soft Tissue Healing: A Systematic Review of Clinical Outcomes After Sports Medicine Orthopaedic Surgery Procedures". Orthopaedic Journal of Sports Medicine 7 (4): 2325967119838873. April 2019. doi:10.1177/2325967119838873. PMID 31019986.
- ↑ 91.0 91.1 "Effect of NSAIDs on Recovery From Acute Skeletal Muscle Injury: A Systematic Review and Meta-analysis". The American Journal of Sports Medicine 46 (1): 224–233. January 2018. doi:10.1177/0363546517697957. PMID 28355084.
- ↑ "Effects of NSAID use on bone healing: A meta-analysis of retrospective case–control and cohort studies within clinical settings" (in en). Trauma 22 (2): 94–111. Apr 2020. doi:10.1177/1460408619886211. ISSN 1460-4086.
- ↑ "Nonsteroidal Anti-Inflammatory Drugs (NSAIDs) and Their Effect on Musculoskeletal Soft-Tissue Healing: A Scoping Review" (in en-US). JBJS Reviews 7 (12): e4. December 2019. doi:10.2106/JBJS.RVW.19.00055. PMID 31851037.
- ↑ "Duration of Analgesic Use and Risk of Hearing Loss in Women". American Journal of Epidemiology 185 (1): 40–47. January 2017. doi:10.1093/aje/kww154. PMID 27974293.
- ↑ "Analgesic use and the risk of hearing loss in women". American Journal of Epidemiology 176 (6): 544–54. September 2012. doi:10.1093/aje/kws146. PMID 22933387.
- ↑ "Analgesic use and the risk of hearing loss in men". The American Journal of Medicine 123 (3): 231–7. March 2010. doi:10.1016/j.amjmed.2009.08.006. PMID 20193831.
- ↑ "Ibuprofen Toxicity". StatPearls. Treasure Island (FL): StatPearls Publishing. 2022. http://www.ncbi.nlm.nih.gov/books/NBK526078/. Retrieved 19 October 2022.
- ↑ "Selective COX-2 Inhibitors: A Review of Their Structure-Activity Relationships". Iranian Journal of Pharmaceutical Research 10 (4): 655–683. 2011. PMID 24250402.
- ↑ "Dengue". United States Centers for Disease Control and Prevention. 28 March 2016. https://wwwnc.cdc.gov/travel/diseases/dengue. "Use acetaminophen. Do not take pain relievers that contain aspirin and ibuprofen (Advil), it may lead to a greater tendency to bleed."
- ↑ "Delhi government bans over the counter sale of NSAIDs without prescription". The Economic Times. 2015. https://economictimes.indiatimes.com/industry/healthcare/biotech/pharmaceuticals/delhi-government-bans-over-the-counter-sale-of-nsaids-without-prescription/articleshow/48441880.cms.
- ↑ "Nonsteroidal anti-inflammatory drugs exposure and the central nervous system". Neurologic Aspects of Systemic Disease Part I. Handbook of Clinical Neurology. 119. 2014. 577–84. doi:10.1016/B978-0-7020-4086-3.00038-2. ISBN 9780702040863.
- ↑ "NSAID single-drug-induced reactions". Immunology and Allergy Clinics of North America 33 (2): 237–49. May 2013. doi:10.1016/j.iac.2012.12.002. PMID 23639711.
- ↑ 103.0 103.1 103.2 "Nonsteroidal Antiinflammatory Drugs (NSAIDs)"]. MedicineNet. 17 December 2008. https://www.medicinenet.com/nonsteroidal_antiinflammatory_drugs/article.htm.
- ↑ "Pharmacokinetic drug interactions with ACE inhibitors". Clinical Pharmacokinetics 25 (1): 20–58. July 1993. doi:10.2165/00003088-199325010-00003. PMID 8354016. http://adisonline.com/pharmacokinetics/Abstract/1993/25010/Pharmacokinetic_Drug_Interactions_with_ACE.3.aspx. Retrieved 30 November 2012.
- ↑ "Why Painkillers Interfere with Anti-depressants". healthcentral.com. https://www.healthcentral.com/article/why-painkillers-interfere-with-anti-depressants.
- ↑ "Antidepressant effects of selective serotonin reuptake inhibitors (SSRIs) are attenuated by antiinflammatory drugs in mice and humans". Proceedings of the National Academy of Sciences of the United States of America 108 (22): 9262–7. May 2011. doi:10.1073/pnas.1104836108. PMID 21518864. Bibcode: 2011PNAS..108.9262W.
- ↑ "Combined use of SSRIs and NSAIDs increases the risk of gastrointestinal adverse effects". British Journal of Clinical Pharmacology 55 (6): 591–5. June 2003. doi:10.1046/j.0306-5251.2002.01770.x. PMID 12814454.
- ↑ "Risk of intracranial haemorrhage in antidepressant users with concurrent use of non-steroidal anti-inflammatory drugs: nationwide propensity score matched study". BMJ (Clinical Research Ed.) 351: h3517. July 2015. doi:10.1136/bmj.h3517. PMID 26173947.
- ↑ "A binding site for nonsteroidal anti-inflammatory drugs in fatty acid amide hydrolase". Journal of the American Chemical Society 135 (1): 22–5. January 2013. doi:10.1021/ja308733u. PMID 23240907.
- ↑ Comparison between effects of antibiotics, NSAIDs and their mixture on the growth of microorganisms. Porto Biomedical Journal. Vol. 2. Issue 5. pages 176-177. S. Bhattacharya, Y. Akula, G.M. Mitongo, Q. Khorram
- ↑ 111.00 111.01 111.02 111.03 111.04 111.05 111.06 111.07 111.08 111.09 111.10 "Ibuprofen and other widely used non-steroidal anti-inflammatory drugs inhibit antibody production in human cells". Cellular Immunology 258 (1): 18–28. 2009. doi:10.1016/j.cellimm.2009.03.007. PMID 19345936.
- ↑ "Defining the COX inhibitor selectivity of NSAIDs: implications for understanding toxicity". Expert Review of Clinical Pharmacology (Web MD LLC) 3 (6): 769–76. November 2010. doi:10.1586/ecp.10.120. PMID 22111779. https://www.medscape.com/viewarticle/733075_5. Retrieved 17 February 2013.
- ↑ Vane, J.R; Botting, R.M (June 2003). "The mechanism of action of aspirin" (in en). Thrombosis Research 110 (5–6): 255–258. doi:10.1016/S0049-3848(03)00379-7. PMID 14592543. https://linkinghub.elsevier.com/retrieve/pii/S0049384803003797.
- ↑ "Sir John Vane, FRS" (in english). https://www.williamharveyresearch.com/about-us/sir-john-vane-frs.
- ↑ "Selective COX-2 Inhibitors: A Review of Their Structure-Activity Relationships". Iranian Journal of Pharmaceutical Research 10 (4): 655–83. 2011. PMID 24250402.
- ↑ "Non-steroidal anti-inflammatory drug-induced enteropathy". Clinical Endoscopy 45 (2): 138–144. June 2012. doi:10.5946/ce.2012.45.2.138. PMID 22866254.
- ↑ "The double-edged sword of COX-2 selective NSAIDs". CMAJ 167 (10): 1131–1137. November 2002. PMID 12427705.
- ↑ "Inhibitors of cyclooxygenases: mechanisms, selectivity and uses". Journal of Physiology and Pharmacology 57 (Suppl 5): 113–24. November 2006. PMID 17218763. http://www.jpp.krakow.pl/journal/archive/11_06_s5/pdf/113_11_06_s5_article.pdf.
- ↑ "The contribution of cyclooxygenase-2 to endocannabinoid metabolism and action". British Journal of Pharmacology 152 (5): 594–601. November 2007. doi:10.1038/sj.bjp.0707379. PMID 17618306.
- ↑ "Non-redundant functions of cyclooxygenases: oxygenation of endocannabinoids". The Journal of Biological Chemistry 283 (13): 8065–9. March 2008. doi:10.1074/jbc.R800005200. PMID 18250160.
- ↑ "Mechanisms of non-opioid analgesics beyond cyclooxygenase enzyme inhibition". Current Molecular Pharmacology 2 (1): 1–14. January 2009. doi:10.2174/1874-470210902010001. PMID 19779578.
- ↑ "Mechanistic aspects of inflammation and clinical management of inflammation in acute gouty arthritis". Journal of Clinical Rheumatology 19 (1): 19–29. January 2013. doi:10.1097/RHU.0b013e31827d8790. PMID 23319019.
- ↑ 123.0 123.1 123.2 "Antipyretics: mechanisms of action and clinical use in fever suppression". The American Journal of Medicine 111 (4): 304–15. September 2001. doi:10.1016/S0002-9343(01)00834-8. PMID 11566461.
- ↑ 124.0 124.1 124.2 "Inhibitors of the microsomal prostaglandin E(2) synthase-1 as alternative to non steroidal anti-inflammatory drugs (NSAIDs)--a critical review". Current Medicinal Chemistry 16 (32): 4274–96. 2009. doi:10.2174/092986709789578178. PMID 19754418.
- ↑ 125.0 125.1 "Is combining or alternating antipyretic therapy more beneficial than monotherapy for febrile children?". BMJ 339: b3540. October 2009. doi:10.1136/bmj.b3540. PMID 19797346.
- ↑ "Prostaglandin E2 and fever: a continuing debate". The Yale Journal of Biology and Medicine 59 (2): 169–74. 1986. PMID 3488620.
- ↑ "Ibuprofen: pharmacology, efficacy and safety". Inflammopharmacology 17 (6): 275–342. December 2009. doi:10.1007/s10787-009-0016-x. PMID 19949916.
- ↑ "Prostaglandin Synthase - an overview | ScienceDirect Topics". https://www.sciencedirect.com/topics/medicine-and-dentistry/prostaglandin-synthase.
- ↑ "Non-steroidal anti-inflammatory drugs (NSAIDs) and organ damage: A current perspective". Biochemical Pharmacology 180: 114147. October 2020. doi:10.1016/j.bcp.2020.114147. PMID 32653589.
- ↑ "Ibuprofen". DrugBank. https://www.drugbank.ca/drugs/DB01050.
- ↑ Consolidated List of products whose consumption or sale have been banned, withdrawn, severely restricted or not approved by Governments, United Nations, 2003, p. 123 link to 2005 ed
- ↑ "Evaluation of the Characteristics of Safety Withdrawal of Prescription Drugs from Worldwide Pharmaceutical Markets-1960 to 1999". Therapeutic Innovation & Regulatory Science 35 (1): 293–317. 1 January 2001. doi:10.1177/009286150103500134.
- ↑ 133.0 133.1 Sriram D, Yogeeswari P. Medicinal Chemistry, 2nd Edition. Pearson Education India, 2010. ISBN:9788131731444
- ↑ Auburn University course material. Jack DeRuiter, Principles of Drug Action 2, Fall 2002 1: Non-Steroidal Antiinflammatory Drugs (NSAIDs)
- ↑ "Information for Healthcare Professionals: Celecoxib (marketed as Celebrex)". Food and Drug Administration (FDA). https://www.fda.gov/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPatientsandProviders/ucm124655.htm.
- ↑ "Safety of Vioxx". FDA Public Health Advisory. Food and Drug Administration (FDA). https://www.fda.gov/drugs/drugsafety/postmarketdrugsafetyinformationforpatientsandproviders/ucm106274.htm.
- ↑ "Information for Healthcare Professionals: Valdecoxib (marketed as Bextra)". Food and Drug Administration (FDA). https://www.fda.gov/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPatientsandProviders/ucm124649.htm.
- ↑ "An investigation into drug products withdrawn from the EU market between 2002 and 2011 for safety reasons and the evidence used to support the decision-making". BMJ Open 4 (1): e004221. January 2014. doi:10.1136/bmjopen-2013-004221. PMID 24435895.
- ↑ "Anti-inflammatory iridoids of botanical origin". Current Medicinal Chemistry 19 (14): 2104–27. 2012. doi:10.2174/092986712800229005. PMID 22414102.
- ↑ "Effects of β-glucosidase hydrolyzed products of harpagide and harpagoside on cyclooxygenase-2 (COX-2) in vitro". Bioorganic & Medicinal Chemistry 19 (16): 4882–6. August 2011. doi:10.1016/j.bmc.2011.06.069. PMID 21775152.
- ↑ 141.0 141.1 141.2 141.3 "Comparing NSAIDs". PubMed Clinical Q&A. National Center for Biotechnology Information. 1 May 2011. https://www.ncbi.nlm.nih.gov/books/NBK45590/.
- ↑ Treating Osteoarthritis and Pain: The Non-Steroidal Anti-Inflammatory Drugs Comparing Effectiveness, Safety, and Price Consumers Union 2005 [|permanent dead link|dead link}}]
- ↑ "Why are non-steroidal anti-inflammatory drugs so variable in their efficacy? A description of ion trapping". Annals of the Rheumatic Diseases 52 (3): 241–243. March 1993. doi:10.1136/ard.52.3.241. PMID 8484682.
- ↑ Aspirin: the story of a wonder drug. London: Bloomsbury. 2004.
- ↑ "The Mythology of Aspirin". https://skeptoid.com/blog/2014/05/22/the-mythology-of-asprin/.
- ↑ "Hippocrates and willow bark? What you know about the history of aspirin is probably wrong". 18 October 2020. https://theconversation.com/hippocrates-and-willow-bark-what-you-know-about-the-history-of-aspirin-is-probably-wrong-148087.
- ↑ "Works by Hippocrates". http://classics.mit.edu/Browse/browse-Hippocrates.html.
- ↑ "De Materia Medica". https://archive.org/details/de-materia-medica.
- ↑ American Indian contributions to the world: 15,000 years of inventions and innovations. Checkmark Books. 2003. ISBN 0-8160-4052-4. OCLC 249349540. http://worldcat.org/oclc/249349540.
- ↑ "The History of Aspirin: The Discoveries That Changed Contemporary Medicine". Paths of Discovery 18: 175–184. 2013. https://www.pas.va/content/dam/casinapioiv/pas/pdf-volumi/acta/acta18pas.pdf#page=243.
- ↑ 151.0 151.1 "Capítulo 27: Analgésicos-antipiréticos, antiinflamatorios y fármacos que se utilizan en el tratamiento de la gota.". Goodman & Gilman, las bases farmacológicas de la terapéutica. (9 ed.). México: Ed. McGraw-Hill Interamericana. 1996. ISBN 978-0-07-026266-9.
- ↑ 152.0 152.1 John McMurry. Química Orgánica (in Spanish). Published by Cengage Learning Editores, 2005. ISBN:970-686-354-0
- ↑ Hermann Kolbe (1860). "Ueber Synthese der Salicylsäure". Annalen der Chemie und Pharmacie 113 (1): 125–27. doi:10.1002/jlac.18601130120. https://zenodo.org/record/1427141.
- ↑ R. Schmitt (1885). "Beitrag zur Kenntniss der Kolbe'schen Salicylsäure Synthese". Journal für Praktische Chemie 31 (1): 397–411. doi:10.1002/prac.18850310130. https://zenodo.org/record/1427904.
- ↑ "The Kolbe-Schmitt Reaction". Chem. Rev. 57 (4): 583–620. 1957. doi:10.1021/cr50016a001. (Review)
- ↑ "Non-steroidal anti-inflammatory drugs as a treatment for Alzheimer's disease: a systematic review and meta-analysis of treatment effect". Drugs & Aging 32 (2): 139–47. February 2015. doi:10.1007/s40266-015-0239-z. PMID 25644018.
- ↑ "Aspirin, steroidal and non-steroidal anti-inflammatory drugs for the treatment of Alzheimer's disease". The Cochrane Database of Systematic Reviews (2): CD006378. February 2012. doi:10.1002/14651858.CD006378.pub2. PMID 22336816.
- ↑ "Anti-inflammatory drugs and risk of Alzheimer's disease: an updated systematic review and meta-analysis". Journal of Alzheimer's Disease 44 (2): 385–96. 2015. doi:10.3233/JAD-141506. PMID 25227314.
- ↑ Banti Christina N (2016). "Non-Steroidal Anti-Inflammatory Drugs (NSAIDs) in Metal Complexes and Their Effect at the Cellular Level". European Journal of Inorganic Chemistry 2016 (19): 3048–3071. doi:10.1002/ejic.201501480.
- ↑ "NADA 141–213: New Animal Drug Application Approval (for Metacam (meloxicam) 0.5 mg/mL and 1.5 mg/mL Oral Suspension)". Food and Drug Administration (FDA). 15 April 2003. http://www.fda.gov/downloads/AnimalVeterinary/Products/ApprovedAnimalDrugProducts/FOIADrugSummaries/ucm118006.pdf.
- ↑ Metacam Client Information Sheet , product description: "Non-steroidal anti-inflammatory drug for oral use in dogs only", and in the "What Is Metacam" section in bold-face type: "Do not use in cats.", January 2005.
- ↑ Metacam 5 mg/mL Solution for Injection, Supplemental Approval 28 October 2004.
- ↑ Off-label use discussed in: Arnold Plotnick MS, DVM, ACVIM, ABVP, Pain Management using Metacam , and Stein, Robert, Perioperative Pain Management Part IV, Looking Beyond Butorphanol, September 2006.
- ↑ "Put a label (claim) on it: Getting non-surgical contraceptives approved for use in cats and dogs". Journal of Feline Medicine and Surgery 17 (9): 783–9. September 2015. doi:10.1177/1098612x15594993. PMID 26323803.
External links
 |