Biology:Adrenergic receptor
File:100-AdrenergicReceptors-2rh1.tifThe adrenergic receptors or adrenoceptors are a class of G protein-coupled receptors that are targets of many catecholamines like norepinephrine (noradrenaline) and epinephrine (adrenaline) produced by the body, but also many medications like beta blockers, beta-2 (β2) agonists and alpha-2 (α2) agonists, which are used to treat high blood pressure and asthma, for example.
Many cells have these receptors, and the binding of a catecholamine to the receptor will generally stimulate the sympathetic nervous system (SNS). The SNS is responsible for the fight-or-flight response, which is triggered by experiences such as exercise or fear-causing situations. This response dilates pupils, increases heart rate, mobilizes energy, and diverts blood flow from non-essential organs to skeletal muscle. These effects together tend to increase physical performance momentarily.
History
By the turn of the 19th century, it was agreed that the stimulation of sympathetic nerves could cause different effects on body tissues, depending on the conditions of stimulation (such as the presence or absence of some toxin). Over the first half of the 20th century, two main proposals were made to explain this phenomenon:
- There were (at least) two different types of neurotransmitters released from sympathetic nerve terminals, or
- There were (at least) two different types of detector mechanisms for a single neurotransmitter.
The first hypothesis was championed by Walter Bradford Cannon and Arturo Rosenblueth,[1] who interpreted many experiments to then propose that there were two neurotransmitter substances, which they called sympathin E (for 'excitation') and sympathin I (for 'inhibition').
The second hypothesis found support from 1906 to 1913, when Henry Hallett Dale explored the effects of adrenaline (which he called adrenine at the time), injected into animals, on blood pressure. Usually, adrenaline would increase the blood pressure of these animals. Although, if the animal had been exposed to ergotoxine, the blood pressure decreased.[2][3] He proposed that the ergotoxine caused "selective paralysis of motor myoneural junctions" (i.e. those tending to increase the blood pressure) hence revealing that under normal conditions that there was a "mixed response", including a mechanism that would relax smooth muscle and cause a fall in blood pressure. This "mixed response", with the same compound causing either contraction or relaxation, was conceived of as the response of different types of junctions to the same compound.
This line of experiments were developed by several groups, including DT Marsh and colleagues,[4] who in February 1948 showed that a series of compounds structurally related to adrenaline could also show either contracting or relaxing effects, depending on whether or not other toxins were present. This again supported the argument that the muscles had two different mechanisms by which they could respond to the same compound. In June of that year, Raymond Ahlquist, Professor of Pharmacology at Medical College of Georgia, published a paper concerning adrenergic nervous transmission.[5] In it, he explicitly named the different responses as due to what he called α receptors and β receptors, and that the only sympathetic transmitter was adrenaline. While the latter conclusion was subsequently shown to be incorrect (it is now known to be noradrenaline), his receptor nomenclature and concept of two different types of detector mechanisms for a single neurotransmitter, remains. In 1954, he was able to incorporate his findings in a textbook, Drill's Pharmacology in Medicine,[6] and thereby promulgate the role played by α and β receptor sites in the adrenaline/noradrenaline cellular mechanism. These concepts would revolutionise advances in pharmacotherapeutic research, allowing the selective design of specific molecules to target medical ailments rather than rely upon traditional research into the efficacy of pre-existing herbal medicines.
Categories
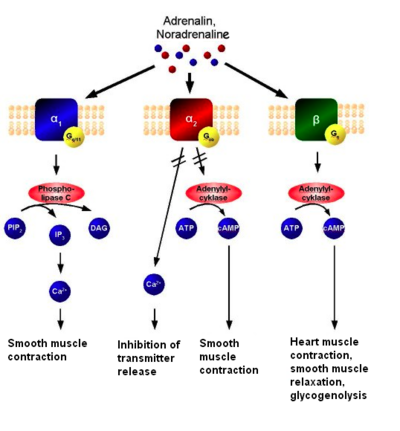
The mechanism of adrenoreceptors. Adrenaline or noradrenaline are receptor ligands to either α1, α2 or β-adrenoreceptors. The α1 couples to Gq, which results in increased intracellular Ca2+ and subsequent smooth muscle contraction. The α2, on the other hand, couples to Gi, which causes a decrease in neurotransmitter release, as well as a decrease of cAMP activity resulting in smooth muscle contraction. The β receptor couples to Gs and increases intracellular cAMP activity, resulting in e.g. heart muscle contraction, smooth muscle relaxation and glycogenolysis. There are two main groups of adrenoreceptors, α and β, with 9 subtypes in total:
- α receptors are subdivided into α1 (a Gq coupled receptor) and α2 (a Gi coupled receptor)[7]
- α1 has 3 subtypes: α1A, α1B and α1D[lower-alpha 1]
- α2 has 3 subtypes: α2A, α2B and α2C
- β receptors are subdivided into β1, β2 and β3. All 3 are coupled to Gs proteins, but β2 and β3 also couple to Gi[7]
Gi and Gs are linked to adenylyl cyclase. Agonist binding thus causes a rise in the intracellular concentration of the second messenger (Gi inhibits the production of cAMP) cAMP. Downstream effectors of cAMP include cAMP-dependent protein kinase (PKA), which mediates some of the intracellular events following hormone binding.
Roles in circulation
Epinephrine (adrenaline) reacts with both α- and β-adrenoreceptors, causing vasoconstriction and vasodilation, respectively. Although α receptors are less sensitive to epinephrine, when activated at pharmacologic doses, they override the vasodilation mediated by β-adrenoreceptors because there are more peripheral α1 receptors than β-adrenoreceptors. The result is that high levels of circulating epinephrine cause vasoconstriction. However, the opposite is true in the coronary arteries, where β2 response is greater than that of α1, resulting in overall dilation with increased sympathetic stimulation. At lower levels of circulating epinephrine (physiologic epinephrine secretion), β-adrenoreceptor stimulation dominates since epinephrine has a higher affinity for the β2 adrenoreceptor than the α1 adrenoreceptor, producing vasodilation followed by decrease of peripheral vascular resistance.[8]
Subtypes
Smooth muscle behavior is variable depending on anatomical location. Smooth muscle contraction/relaxation is generalized below. One important note is the differential effects of increased cAMP in smooth muscle compared to cardiac muscle. Increased cAMP will promote relaxation in smooth muscle, while promoting increased contractility and pulse rate in cardiac muscle.
| Receptor | Agonist potency order | Agonist action | Mechanism | Agonists | Antagonists |
|---|---|---|---|---|---|
| α1: A, B, D[lower-alpha 1] | Norepinephrine > epinephrine >> isoprenaline[9] | Smooth muscle contraction, mydriasis, vasoconstriction in the skin, mucosa and abdominal viscera & sphincter contraction of the GI tract and urinary bladder | Gq: phospholipase C (PLC) activated, IP3, and DAG, rise in calcium[7] |
|
(Alpha-1 blockers)
(TCAs)
Antihistamines (H1 antagonists) |
| α2: A, B, C | Epinephrine = norepinephrine >> isoprenaline[9] | Smooth muscle mixed effects, norepinephrine (noradrenaline) inhibition, platelet activation | Gi: adenylate cyclase inactivated, cAMP down[7] | (Alpha-2 blockers)
| |
| β1 | Isoprenaline > epinephrine > norepinephrine[9] | Positive chronotropic, dromotropic and inotropic effects, increased amylase secretion | Gs: adenylate cyclase activated, cAMP up[7] | (β1-adrenergic agonist)
|
(Beta blockers) |
| β2 | Isoprenaline > epinephrine > norepinephrine[9] | Smooth muscle relaxation (bronchodilation for example) | Gs: adenylate cyclase activated, cAMP up (also Gi, see α2)[7] | (β2-adrenergic agonist)
|
(Beta blockers)
|
| β3 | Isoprenaline > norepinephrine = epinephrine[9] | Enhance lipolysis, promotes relaxation of detrusor muscle in the bladder | Gs: adenylate cyclase activated, cAMP up (also Gi, see α2)[7] | (β3-adrenergic agonist)
|
(Beta blockers) |
α receptors
α receptors have actions in common, but also individual effects. Common (or still receptor unspecified) actions include:
- vasoconstriction[13]
- decreased flow of smooth muscle in gastrointestinal tract[14]
Subtype unspecific α agonists (see actions above) can be used to treat rhinitis (they decrease mucus secretion). Subtype unspecific α antagonists can be used to treat pheochromocytoma (they decrease vasoconstriction caused by norepinephrine).[7]
α1 receptor
α1-adrenoreceptors are members of the Gq protein-coupled receptor superfamily. Upon activation, a heterotrimeric G protein, Gq, activates phospholipase C (PLC). The PLC cleaves phosphatidylinositol 4,5-bisphosphate (PIP2), which in turn causes an increase in inositol triphosphate (IP3) and diacylglycerol (DAG). The former interacts with calcium channels of endoplasmic and sarcoplasmic reticulum, thus changing the calcium content in a cell. This triggers all other effects, including a prominent slow after depolarizing current (sADP) in neurons.[15]
Actions of the α1 receptor mainly involve smooth muscle contraction. It causes vasoconstriction in many blood vessels, including those of the skin, gastrointestinal system, kidney (renal artery)[16] and brain.[17] Other areas of smooth muscle contraction are:
- ureter
- vas deferens
- hair (arrector pili muscles)
- uterus (when pregnant)
- urethral sphincter
- urothelium and lamina propria[18]
- bronchioles (although minor relative to the relaxing effect of β2 receptor on bronchioles)
- blood vessels of ciliary body and (stimulation of dilator pupillae muscles of iris causes mydriasis)
Actions also include glycogenolysis and gluconeogenesis from adipose tissue and liver; secretion from sweat glands and Na+ reabsorption from kidney.[19]
α1 antagonists can be used to treat:[7]
- hypertension – decrease blood pressure by decreasing peripheral vasoconstriction
- benign prostate hyperplasia – relax smooth muscles within the prostate thus easing urination
α2 receptor
The α2 receptor couples to the Gi/o protein.[20] It is a presynaptic receptor, causing negative feedback on, for example, norepinephrine (NE). When NE is released into the synapse, it feeds back on the α2 receptor, causing less NE release from the presynaptic neuron. This decreases the effect of NE. There are also α2 receptors on the nerve terminal membrane of the post-synaptic adrenergic neuron.
Actions of the α2 receptor include:
- decreased insulin release from the pancreas[19]
- increased glucagon release from the pancreas
- contraction of sphincters of the GI-tract
- negative feedback in the neuronal synapses - presynaptic inhibition of norepinephrine release in CNS
- decreased platelet aggregation
- decreases peripheral vascular resistance
α2 agonists (see actions above) can be used to treat:[7]
- hypertension – decrease blood pressure-raising actions of the sympathetic nervous system
α2 antagonists can be used to treat:[7]
- impotence – relax penile smooth muscles and ease blood flow
- depression – enhance mood by increasing norepinephrine secretion
β receptors
Subtype unspecific β agonists can be used to treat:[7]
- heart failure – increase cardiac output acutely in an emergency
- circulatory shock – increase cardiac output thus redistributing blood volume
- anaphylaxis – bronchodilation
Subtype unspecific β antagonists (beta blockers) can be used to treat:[7]
- heart arrhythmia – decrease the output of sinus node thus stabilizing heart function
- coronary artery disease – reduce heart rate and hence increasing oxygen supply
- heart failure – prevent sudden death related to this condition,[7] which is often caused by ischemias or arrhythmias[21]
- hyperthyroidism – reduce peripheral sympathetic hyper-responsiveness
- migraine – reduce number of attacks
- stage fright – reduce tachycardia and tremor
- glaucoma – reduce intraocular pressure
β1 receptor
Actions of the β1 receptor include:
- increase cardiac output by increasing heart rate (positive chronotropic effect), conduction velocity (positive dromotropic effect), stroke volume (by enhancing contractility – positive inotropic effect), and rate of relaxation of the myocardium, by increasing calcium ion sequestration rate (positive lusitropic effect), which aids in increasing heart rate
- increase renin secretion from juxtaglomerular cells of the kidney[22]
- increase ghrelin secretion from the stomach[23]
β2 receptor
- Actions of the β2 receptor include:
- smooth muscle relaxation throughout many areas of the body, e.g. in bronchi (bronchodilation, see salbutamol),[19] GI tract (decreased motility), veins (vasodilation of blood vessels), especially those to skeletal muscle (although this vasodilator effect of norepinephrine is relatively minor and overwhelmed by α adrenoceptor-mediated vasoconstriction)[24]
- lipolysis in adipose tissue[25]
- anabolism in skeletal muscle[26][27]
- uptake of potassium into cells[28]
- relax non-pregnant uterus
- relax detrusor urinae muscle of bladder wall
- dilate arteries to skeletal muscle
- glycogenolysis and gluconeogenesis
- stimulates insulin secretion[29]
- contract sphincters of GI tract
- thickened secretions from salivary glands[19]
- inhibit histamine-release from mast cells
- involved in brain - immune communication[30]
β2 agonists (see actions above) can be used to treat:[7]
- asthma and COPD – reduce bronchial smooth muscle contraction thus dilating the bronchus
- hyperkalemia – increase cellular potassium intake
- preterm birth – reduce uterine smooth muscle contractions[31]
β3 receptor
Actions of the β3 receptor include:
β3 agonists could theoretically be used as weight-loss drugs, but are limited by the side effect of tremors.
See also
Notes
References
- ↑ "Studies On Conditions Of Activity In Endocrine Organs XXVI: Sympathin E and Sympathin I". American Journal of Physiology 104 (3): 557–574. 31 May 1933. doi:10.1152/ajplegacy.1933.104.3.557.
- ↑ "On some physiological actions of ergot". The Journal of Physiology 34 (3): 163–206. May 1906. doi:10.1113/jphysiol.1906.sp001148. PMID 16992821.
- ↑ "On the action of ergotoxine; with special reference to the existence of sympathetic vasodilators". The Journal of Physiology 46 (3): 291–300. Jun 1913. doi:10.1113/jphysiol.1913.sp001592. PMID 16993202.
- ↑ "The comparative pharmacology of the N-alkyl-arterenols". The Journal of Pharmacology and Experimental Therapeutics 92 (2): 108–20. Feb 1948. PMID 18903395.
- ↑ "A study of the adrenotropic receptors". The American Journal of Physiology 153 (3): 586–600. Jun 1948. doi:10.1152/ajplegacy.1948.153.3.586. PMID 18882199.
- ↑ Drill, Victor Alexander (1954). Pharmacology in medicine: a collaborative textbook. New York: McGraw-Hill. https://archive.org/details/pharmacologyinme00dril.
- ↑ 7.00 7.01 7.02 7.03 7.04 7.05 7.06 7.07 7.08 7.09 7.10 7.11 7.12 7.13 7.14 Perez, Dianne M. (2006). The adrenergic receptors in the 21st century. Totowa, New Jersey: Humana Press. pp. 54, 129–134. ISBN 978-1588294234. OCLC 58729119.
- ↑ Zwieten, Van; A, P. (1986). "Interaction Between α and β-Adrenoceptor-Mediated Cardiovascular Effects" (in en-US). Journal of Cardiovascular Pharmacology 8: S21-8. doi:10.1097/00005344-198608004-00004. ISSN 0160-2446. PMID 2427848. https://dx.doi.org/10.1097/00005344-198608004-00004.
- ↑ 9.0 9.1 9.2 9.3 9.4 Rang and Dale's pharmacology (8th ed.). United Kingdom: Elsevier. 2016. pp. 179. ISBN 9780702053627. OCLC 903083639.
- ↑ Prischich, Davia; Gomila, Alexandre M. J.; Milla-Navarro, Santiago; Sangüesa, Gemma; Diez-Alarcia, Rebeca; Preda, Beatrice; Matera, Carlo; Batlle, Montserrat et al. (2020). "Adrenergic modulation with photochromic ligands". Angewandte Chemie International Edition 60 (7): 3625–3631. doi:10.1002/anie.202010553. ISSN 1433-7851. PMID 33103317.
- ↑ "Paroxetine is a direct inhibitor of g protein-coupled receptor kinase 2 and increases myocardial contractility". ACS Chemical Biology 7 (11): 1830–1839. 2012-09-21. doi:10.1021/cb3003013. ISSN 1554-8929. PMID 22882301.
- ↑ "Functional studies of the first selective beta 3-adrenergic receptor antagonist SR 59230A in rat brown adipocytes". Molecular Pharmacology 49 (1): 7–14. 1996. PMID 8569714. http://molpharm.aspetjournals.org/cgi/content/abstract/49/1/7.
- ↑ "Alpha-adrenoceptors in equine digital veins: evidence for the presence of both alpha1 and alpha2-receptors mediating vasoconstriction". Journal of Veterinary Pharmacology and Therapeutics 20 (4): 308–17. 1997. doi:10.1046/j.1365-2885.1997.00078.x. PMID 9280371.
- ↑ "Involvement of alpha-1 and alpha-2 adrenoceptors in the postlaparotomy intestinal motor disturbances in the rat". Gut 28 (8): 955–9. 1987. doi:10.1136/gut.28.8.955. PMID 2889649.
- ↑ "Excitatory actions of noradrenaline and metabotropic glutamate receptor activation in granule cells of the accessory olfactory bulb". Journal of Neurophysiology 102 (2): 1103–14. Aug 2009. doi:10.1152/jn.91093.2008. PMID 19474170.
- ↑ "Renal alpha-1 and alpha-2 adrenergic receptors: biochemical and pharmacological correlations". The Journal of Pharmacology and Experimental Therapeutics 219 (2): 400–6. 1981. PMID 6270306. http://jpet.aspetjournals.org/cgi/content/abstract/219/2/400.
- ↑ Circulation & Lung Physiology I M.A.S.T.E.R. Learning Program, UC Davis School of Medicine
- ↑ "Adrenoceptor function and expression in bladder urothelium and lamina propria". Urology 81 (1): 211.e1–7. 2013. doi:10.1016/j.urology.2012.09.011. PMID 23200975.
- ↑ 19.0 19.1 19.2 19.3 Fitzpatrick, David; Purves, Dale; Augustine, George (2004). "Table 20:2". Neuroscience (3rd ed.). Sunderland, Mass: Sinauer. ISBN 978-0-87893-725-7.
- ↑ "Abundance and stability of complexes containing inactive G protein-coupled receptors and G proteins". FASEB Journal 22 (8): 2920–7. 2008. doi:10.1096/fj.08-105775. PMID 18434433.
- ↑ "How do heart failure patients die?". European Heart Journal Supplements 4 (Suppl D): D59–D65. 2002-04-01. doi:10.1093/oxfordjournals.ehjsupp.a000770.
- ↑ "Convergence of major physiological stimuli for renin release on the Gs-alpha/cyclic adenosine monophosphate signaling pathway". Clinical and Experimental Nephrology 16 (1): 17–24. February 2012. doi:10.1007/s10157-011-0494-1. PMID 22124804.
- ↑ "Ghrelin secretion stimulated by {beta}1-adrenergic receptors in cultured ghrelinoma cells and in fasted mice". Proceedings of the National Academy of Sciences of the United States of America 107 (36): 15868–73. Sep 2010. doi:10.1073/pnas.1011116107. PMID 20713709. Bibcode: 2010PNAS..10715868Z.
- ↑ "Adrenergic and Cholinergic Receptors in Blood Vessels". http://www.cvphysiology.com/Blood%20Pressure/BP010b.htm.
- ↑ "Human beta-2 adrenoceptor gene polymorphisms are highly frequent in obesity and associate with altered adipocyte beta-2 adrenoceptor function". The Journal of Clinical Investigation 100 (12): 3005–13. 1997. doi:10.1172/JCI119854. PMID 9399946.
- ↑ "Rapamycin inhibits the growth and muscle-sparing effects of clenbuterol". Journal of Applied Physiology 102 (2): 740–7. 2007. doi:10.1152/japplphysiol.00873.2006. PMID 17068216.
- ↑ "Clenbuterol increases lean muscle mass but not endurance in patients with chronic heart failure". The Journal of Heart and Lung Transplantation 27 (4): 457–61. 2008. doi:10.1016/j.healun.2008.01.013. PMID 18374884.
- ↑ Basic & Clinical Pharmacology. United States of America: MCGraw-Hill Education. 2018. pp. 148. ISBN 978-1-259-64115-2.
- ↑ "Age-related impairment in insulin release: the essential role of β(2)-adrenergic receptor". Diabetes 61 (3): 692–701. March 2012. doi:10.2337/db11-1027. PMID 22315324.
- ↑ "The sympathetic nerve--an integrative interface between two supersystems: the brain and the immune system". Pharmacological Reviews 52 (4): 595–638. December 2000. PMID 11121511.
- ↑ "Short-term tocolytics for preterm delivery - current perspectives". International Journal of Women's Health 6: 343–9. 2014. doi:10.2147/IJWH.S44048. PMID 24707187.
- ↑ "International Union of Pharmacology. X. Recommendation for nomenclature of alpha 1-adrenoceptors: consensus update". Pharmacological Reviews 47 (2): 267–70. June 1995. PMID 7568329.
Further reading
- "Chapter 11: Noradrenergic transmission". Rang and Dale's Pharmacology (6th ed.). Elsevier Churchill Livingstone. 2007. pp. 169–170. ISBN 978-0-443-06911-6.
External links
- Alpha receptors illustrated
- The Adrenergic Receptors
- Adrenoceptors - IUPHAR/BPS guide to pharmacology
- Basic Neurochemistry: α- and β-Adrenergic Receptors
- Theory of receptor activation
- Desensitization of β1 receptors
 |



