Medicine:Familial hemiplegic migraine
| Familial hemiplegic migraine |
|---|
Familial hemiplegic migraine (FHM) is an autosomal dominant type of hemiplegic migraine that typically includes weakness of half the body which can last for hours, days, or weeks. It can be accompanied by other symptoms, such as ataxia, coma, and paralysis. Migraine attacks may be provoked by minor head trauma. Some cases of minor head trauma in patients with hemiplegic migraine can develop into delayed cerebral edema, a life-threatening medical emergency.[1] Clinical overlap occurs in some FHM patients with episodic ataxia type 2 and spinocerebellar ataxia type 6, benign familial infantile epilepsy, and alternating hemiplegia of childhood.
Three genetic loci for FHM are known. FHM1, which accounts for about 50% of FHM patients, is caused by mutations in a gene coding for the P/Q-type calcium channel α subunit, CACNA1A. FHM1 is also associated with cerebellar degeneration. FHM2, which accounts for less than 25% of cases, is caused by mutations in the Na+/K+-ATPase gene ATP1A2. FHM3 is a rare subtype of FHM and is caused by mutations in a sodium channel α-subunit coding gene, SCN1A. These three subtypes do not account for all cases of FHM, suggesting the existence of at least one other locus (FHM4).
Also, nonfamilial cases of hemiplegic migraine are seen, termed sporadic hemiplegic migraine. These cases seem to have the same causes as the familial cases and represent de novo mutations. Sporadic cases are also clinically identical to familial cases with the exception of a lack of known family history of attacks.
Signs and symptoms
FHM signs overlap significantly with those of migraine with aura. In short, FHM is typified by migraine with aura associated with hemiparesis, and in FHM1, cerebellar degeneration, which can result in episodic or progressive ataxia. FHM can also present with the same signs as benign familial infantile convulsions and alternating hemiplegia of childhood. Other symptoms are altered consciousness (in fact, some cases seem related to head trauma), gaze-evoked nystagmus, and coma. Aura symptoms, such as numbness and blurring of vision, typically persist for 30–60 minutes, but can last for weeks to months. An attack resembles a stroke, but unlike a stroke, it resolves in time. These signs typically first manifest themselves in the first or second decade of life.[citation needed]
Causes
See the equivalent section in the main migraine article.
FHM mutations are believed to lead to migraine susceptibility by lowering the threshold for cortical-spreading-depression generation. The FHM1 and FHM3 mutations occur in ion channels expressed in neurons. These mutations may lead to both the hyper- and hypoexcitable neurons that might underlie cortical-spreading-depression. How the mutations seen in FHM2 patients might lead to FHM symptoms is even less clear, as the gene mutated in FHM2 is expressed primarily in astrocytes. One proposal states that the depolarization of astrocytes caused by haploinsufficiency of the ATP1A2 Na+/K+-ATPase causes increased release of compounds such as adenosine from astrocytes. These compounds then interact with neighboring neurons, altering their excitability and leading to cortical-spreading-depression and migraine.[citation needed]
Pathophysiology
FHM1 (CACNA1A)
The first discovered FHM locus was the CACNA1A gene (originally named CACNL1A4), which encodes the P/Q-type calcium channel CaV2.1. Currently, 17 mutations in this channel are known (table 1), and these mutations are distributed throughout the channel. Some of these mutations result in patients with notable cerebellar degeneration or other dysfunction, including one mutation (S218L), which may be related to severe responses to mild concussion, up to and including delayed cerebral edema, coma, and death.[2] Fifteen of these mutants have received at least some further analysis at the electrophysiological level to attempt to determine how they might lead to the FHM1 phenotype. Contradiction in the literature is increasing as to the end result of these mutations on channel kinetics and neuronal excitability.[citation needed]
A good example of this contradiction can be seen in the literature regarding the R192Q mutation.[3] The first investigation of this mutation, using the rabbit isoform of the channel expressed in oocytes, found that it did not alter any measured channel properties.[4] A subsequent report, using human channels expressed in HEK293 cells, found a small, hyperpolarizing shift in the midpoint for activation, a result common among FHM1 mutants.[5] This shift results in channels that open at more negative potentials, thus have a higher open probability than wild-type channels at most potentials. This report also found that the R192Q mutant produced almost twice as much whole-cell current compared to wild-type channels. This is not due to a change in single channel conductance, but to an equivalent increase in channel density. A subsequent group noticed that this mutation is in a region important for modulation by G protein-coupled receptors (GPCRs).[6] GPCR activation leads to inhibition of wild-type CaV2.1 currents. R192Q mutant channel currents are also decreased by GPCR activation, but by a smaller amount. A more recent group has confirmed some of these results by creating a R192Q knock-in mouse.[7] They confirmed that the R192Q mutant activates at more negative potentials and that neurons producing these channels have much larger whole-cell current. This resulted in a much larger quantal content (the number of neurotransmitter packets released per action potential) and generally enhanced neurotransmitter release in R192Q-expressing neurons versus wild-type. Consequently, these mutant mice were more susceptible to cortical-spreading-depression than their wild-type counterparts. The most recent experiments on this mutant, however, have contradicted some of these results.[8] In CaV2.1 knockout neurons transfected with human channels, P/Q-type currents from mutant channels are actually smaller than their wild-type counterpart. They also found a significant decrease in calcium influx during depolarization, leading to decreased quantal content, in mutant versus wild-type expressing neurons. Neurons expressing mutant channels were also less able to mediate inhibitory input and have smaller inhibitory postsynaptic currents through P/Q-type channels. Further testing with this and other mutants is required to determine their end effect on human physiology.[citation needed]
| Mutation | Position | Effect | Cerebellar signs | Reference | |
|---|---|---|---|---|---|
| Nucleotide | Amino acid | ||||
| c.G575A | R192Q | D1S4 | Decreases G-protein mediated inhibition, activates at more negative potentials, increased expression, faster recovery from inactivation. In mice: greater current, activates at more negative potentials, enhances transmitter release | ? | [3][4][5][6][7][8] |
| c.G584A | R195K | D1S4 | No | [9] | |
| c.C653T | S218L | D1S4-5 | Increases sojourns to subconductances, activates at more negative potentials, decreased slow inactivation, increased fast inactivation | Yes | [2][10] |
| c.G1748A | R583Q* | D2S4 | Activates at more negative potentials, faster current decay, faster inactivation, slower recovery from inactivation | Yes | [9][11][12][13][14] |
| c.C1997T | T666M | D2-pore | Activates at more negative potentials, faster current decay, slowed recovery from inactivation, smaller single channel conductance, higher i*Po, slower recovery from inactivation, Increased G-protein mediated inhibition, decreased gating charge (fewer channels available to open) | Yes | [3][4][5][8][9][13][15][16][17] |
| c.T2141C | V714A | D2S6 | Activates at more negative potentials, faster current decay, faster recovery from inactivation, decreases expression, faster recovery from inactivation, increases G-protein-mediated inhibition | No | [3][4][5][8][13] |
| c.C2145G | D715E | D2S6 | Activates at more negative potentials, faster current decay, faster inactivation | Yes | [9][11][15] |
| c.A4003G | K1335E | D3S3-4 | Activates at more negative potentials, inactivates at more negative potentials, slowed recovery from inactivation, increased frequency dependent rundown | No | [9][18] |
| c.G4037A | R1346Q | D3S4 | Yes | [19] | |
| c.A4151G | Y1384C | D3S5 | Yes | [9][20] | |
| c.G4366T | V1456L | D3-pore | Activates at more negative potentials, slower current decay, slower recovery from inactivation | No | [12][21] |
| c.C4636T | R1546X** | D4S1 | Decreased current | Yes | [22][23][24] |
| c.C4999T | R1667W | D4S4 | Yes | [9] | |
| c.T5047C | W1683R | D4S4-5 | Activates at more negative potentials, inactivates at more negative potentials, slowed recovery from inactivation, increased frequency dependent rundown | Yes | [9][18] |
| c.G5083A | V1695I | D4S5 | Slowed recovery from inactivation, increased frequency dependent rundown | No | [9][18] |
| c.T5126C | I1709T | D4S5 | Yes | [25][26] | |
| c.A5428C | I1810L | D4S6 | Activates at more negative potentials, faster recovery from inactivation, decreased expression, faster recovery from inactivation, Increased G-protein mediated inhibition | Yes | [3][4][5][8][13] |
*
** |
Also diagnosed as spinocerebellar ataxia type-6 Also diagnosed as episodic ataxia type-2 | ||||
| Sequence numbering according to NCBI reference sequence NM_000068.2. Cerebellar signs refers to findings of cerebellar degeneration or ataxia upon clinical examination. | |||||
FHM2 (ATP1A2)
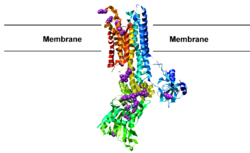
The second subtype of familial hemiplegic migraine, FHM2, is caused by mutations in the gene ATP1A2 that encodes a Na+/K+-ATPase. This Na+/K+-ATPase is heavily expressed in astrocytes and helps to set and maintain their reversal potential. Twenty-nine known mutations in this gene are associated with FHM2 (table 2), many clustering in the large intracellular loop between membrane-spanning segments 4 and 5 (figure 1). Twelve of these mutations have been studied by expression in model cells. All but one have shown either complete loss of function or more complex decreases in ATPase activity or potassium sensitivity. Astrocytes expressing these mutant ion pumps will have much higher resting potentials and are believed to lead to disease through a poorly understood mechanism.[citation needed]
| Mutation | Location | Physiological result | Reference(s) |
|---|---|---|---|
| E174K | M2-3 | No change | [27] |
| T263M | M2-3 | [28] | |
| G301R | M3 | [29] | |
| T345A | M4-5 | Decreased K influx | [30][31] |
| T376M | M4-5 | [28] | |
| R383H | M4-5 | [32] | |
| T378N | M4-5 | [33] | |
| C515Y | M4-5 | Loss of function (haploinsufficiency) | [27] |
| R548H | M4-5 | [34] | |
| R593W | M4-5 | Loss of function (haploinsufficiency) | [35] |
| A606T | M4-5 | [28] | |
| G615R | M4-5 | Loss of function (haploinsufficiency) | [36] |
| V628M | M4-5 | Loss of function (haploinsufficiency) | [35] |
| R689Q | M4-5 | Decreased catalytic turnover | [31][37][38] |
| E700K | M4-5 | [39] | |
| D718N | M4-5 | Loss of function (haploinsufficiency) | [32] |
| M731T | M4-5 | Decreased catalytic turnover | [31][37][38] |
| R763H | M4-5 | Loss of function (haploinsufficiency) | [32] |
| L764P | M4-5 | Loss of function (haploinsufficiency) | [31][40][41] |
| P796R | M5-6 | [32] | |
| M829R | M6-7 | [28] | |
| R834Q | M6-7 | [28] | |
| W887R | M7-8 | Loss of function (haploinsufficiency) | [27][31][40][41] |
| E902K | M7-8 | [32] | |
| 935K_940SdelinsI | M8-9 | [28] | |
| R937P | M8-9 | [28] | |
| S966LfsX998 | M9 | [28] | |
| P979L | M9-10 | [32] | |
| X1021RextX28 | C-Terminus | [32] | |
| Numbering according to the NCBI reference sequence NM_000702.2. | |||
FHM3 (SCN1A)
The final known locus FHM3 is the SCN1A gene, which encodes a sodium channel α subunit. The only study so far that has found mutations in this gene discovered the same Q1489K mutation in three of 20 families (15%) with 11 other kindreds (55%) already having mutations in CACNA1A or ATP1A2. This mutation is located in a highly conserved region of an intracellular loop connecting domains three and four. This mutation results in a greatly hastened (two- to four-fold) recovery from inactivation compared to wild-type.[42] As this channel is important for action potential generation in neurons, the Q1489K mutant is expected to result in hyperexcitable neurons.[citation needed]
FHM4 (1q31)
The final locus for FHM maps to the q-arm of chromosome 1. A number of attractive candidate genes occur in this area, though no mutations in them have yet been linked to FHM4.[43]
Other genetic associations
A fourth gene associated with this condition is the proline-rich transmembrane protein 2 (PRRT2 gene) - an axonal protein associated with the exocytosis complex.[44]
A fifth gene associated with this condition is SLC4A4, which encodes the electrogenic NaHCO3 cotransporter NBCe1.[45]
Diagnosis
Diagnosis of FHM is made according to these criteria:[citation needed]
- Two attacks of each of:
- Aura with motor weakness accompanied by either reversible visual symptoms (flickering lights, spots, lines, etc.), reversible sensory symptoms (pins and needles, numbness, etc.) or speech symptoms
- At least two occurrences of:
- One or more aura symptoms that develop over at least 5 minutes
- These symptoms lasting more than 5 minutes and less than 24 hours
- Headache beginning within 60 minutes of aura onset: These headaches can last 4–72 hours, occur on only one side of the head, pulsate, be of moderate to severe intensity, and may be aggravated by common physical activities such as walking. These headaches must also be accompanied by nausea/vomiting, phonophobia (avoidance of sound due to hypersensitivity), and/or photophobia (avoidance of light due to hypersensitivity).
- At least one close (first- or second-degree) relative with FHM
- No other likely cause
Sporadic forms follow the same diagnostic criteria, with the exception of family history.
In all cases, family and patient histories are used for diagnosis. Brain-imaging techniques, such as MRI, CAT scan, and SPECT,[46] are used to look for signs of other familial conditions such as CADASIL or mitochondrial disease, and for evidence of cerebellar degeneration. With the discovery of causative genes, genetic sequencing can also be used to verify diagnosis (though not all genetic loci are known).
Screening
Prenatal screening is not typically done for FHM, but it may be performed if requested. As penetrance is high, individuals found to carry mutations should be expected to develop signs of FHM at some point in life.[citation needed]
Management
See the equivalent section in the main migraine article.
People with FHM are encouraged to avoid activities that may trigger their attacks. Minor head trauma is a common attack precipitant, so FHM sufferers should avoid contact sports. Acetazolamide or standard drugs are often used to treat attacks, though those leading to vasoconstriction should be avoided due to the risk of stroke.[citation needed]
Epidemiology
Migraine itself is a very common disorder, occurring in 15–20% of the population. Hemiplegic migraine, be it familial or spontaneous, is less prevalent, at 0.01% prevalence according to one report.[47] Women are three times more likely to be affected than males.[citation needed]
See also
- Channelopathy
- Childhood absence epilepsy
- Hypokalemic periodic paralysis
- Juvenile myoclonic epilepsy
- Malignant hyperthermia
- Timothy syndrome
References
- ↑ "Early seizures and cerebral oedema after trivial head trauma associated with the CACNA1A S218L mutation". J Neurol Neurosurg Psychiatry 80 (10): 1125–1129. 2009. doi:10.1136/jnnp.2009.177279. PMID 19520699. http://dare.uva.nl/personal/pure/en/publications/early-seizures-and-cerebral-oedema-after-trivial-head-trauma-associated-with-the-cacna1a-s218l-mutation(130966e9-5712-447a-b482-f521cd45b826).html.
- ↑ 2.0 2.1 "Delayed cerebral edema and fatal coma after minor head trauma: role of the CACNA1A calcium channel subunit gene and relationship with familial hemiplegic migraine". Ann Neurol 49 (6): 753–60. 2001. doi:10.1002/ana.1031. PMID 11409427.
- ↑ 3.0 3.1 3.2 3.3 3.4 "Familial hemiplegic migraine and episodic ataxia type-2 are caused by mutations in the Ca2+ channel gene CACNL1A4.". Cell 87 (3): 543–52. 1996. doi:10.1016/S0092-8674(00)81373-2. PMID 8898206. http://repub.eur.nl/pub/57576.
- ↑ 4.0 4.1 4.2 4.3 4.4 "Familial hemiplegic migraine mutations change alpha1A Ca2+ channel kinetics.". J Biol Chem 273 (10): 5586–90. 1998. doi:10.1074/jbc.273.10.5586. PMID 9488686.
- ↑ 5.0 5.1 5.2 5.3 5.4 "Functional consequences of mutations in the human alpha1A calcium channel subunit linked to familial hemiplegic migraine.". J Neurosci 19 (5): 1610–9. 1999. doi:10.1523/JNEUROSCI.19-05-01610.1999. PMID 10024348.
- ↑ 6.0 6.1 "The familial hemiplegic migraine mutation R192q reduces G-protein-mediated inhibition of p/q-type (Cav2.1) calcium channels expressed in human embryonic kidney cells". J Physiol 546 (Pt 2): 337–47. 2003. doi:10.1113/jphysiol.2002.026716. PMID 12527722.
- ↑ 7.0 7.1 "A Cacna1a knockin migraine mouse model with increased susceptibility to cortical spreading depression". Neuron 41 (5): 701–10. 2004. doi:10.1016/S0896-6273(04)00085-6. PMID 15003170.
- ↑ 8.0 8.1 8.2 8.3 8.4 "Effects of familial hemiplegic migraine type 1 mutations on neuronal P/Q-type Ca2+ channel activity and inhibitory synaptic transmission". Proc Natl Acad Sci USA 102 (7): 2590–5. 2005. doi:10.1073/pnas.0409896102. PMID 15699344.
- ↑ 9.0 9.1 9.2 9.3 9.4 9.5 9.6 9.7 9.8 "The clinical spectrum of familial hemiplegic migraine associated with mutations in a neuronal calcium channel". N Engl J Med 345 (1): 17–24. 2001. doi:10.1056/NEJM200107053450103. PMID 11439943.
- ↑ "Specific kinetic alterations of human CaV2.1 calcium channels produced by mutation S218L causing familial hemiplegic migraine and delayed cerebral edema and coma after minor head trauma". J Biol Chem 280 (18): 17678–86. 2005. doi:10.1074/jbc.M501110200. PMID 15743764.
- ↑ 11.0 11.1 "A new CACNA1A gene mutation in acetazolamide-responsive familial hemiplegic migraine and ataxia". Neurology 53 (1): 38–43. 1999. doi:10.1212/WNL.53.1.38. PMID 10408534.
- ↑ 12.0 12.1 "Three new familial hemiplegic migraine mutants affect P/Q-type Ca(2+) channel kinetics". J Biol Chem 275 (13): 9239–43. 2000. doi:10.1074/jbc.275.13.9239. PMID 10734061.
- ↑ 13.0 13.1 13.2 13.3 "Familial hemiplegic migraine mutations increase Ca2+ influx through single human CaV2.1 channels and decrease maximal CaV2.1 current density in neurons". Proc Natl Acad Sci USA 99 (20): 13284–9. 2002. doi:10.1073/pnas.192242399. PMID 12235360.
- ↑ "Phenotypes of spinocerebellar ataxia type 6 and familial hemiplegic migraine caused by a unique CACNA1A missense mutation in patients from a large family". Arch Neurol 60 (4): 610–4. 2003. doi:10.1001/archneur.60.4.610. PMID 12707077.
- ↑ 15.0 15.1 "Recurrence of the T666M calcium channel CACNA1A gene mutation in familial hemiplegic migraine with progressive cerebellar ataxia". Am J Hum Genet 64 (1): 89–98. 1999. doi:10.1086/302192. PMID 9915947.
- ↑ "Detection of a novel missense mutation and second recurrent mutation in the CACNA1A gene in individuals with EA-2 and FHM". Hum Genet 105 (3): 261–5. 1999. doi:10.1007/s004390051099. PMID 10987655.
- ↑ "Gating deficiency in a familial hemiplegic migraine type 1 mutant P/Q-type calcium channel". J Biol Chem 280 (25): 24064–71. 2005. doi:10.1074/jbc.M502223200. PMID 15795222.
- ↑ 18.0 18.1 18.2 "Familial hemiplegic migraine type 1 mutations K1336E, W1684R, and V1696I alter Cav2.1 Ca2+ channel gating: evidence for beta-subunit isoform-specific effects". J Biol Chem 279 (50): 51844–50. 2004. doi:10.1074/jbc.M408756200. PMID 15448138.
- ↑ "A novel R1347Q mutation in the predicted voltage sensor segment of the P/Q-type calcium-channel alpha-subunit in a family with progressive cerebellar ataxia and hemiplegic migraine". Clin Genet 65 (1): 70–2. 2004. doi:10.1111/j..2004.00187.x. PMID 15032980.
- ↑ "CACNA1A gene de novo mutation causing hemiplegic migraine, coma, and cerebellar atrophy". Neurology 55 (7): 1040–2. 2000. doi:10.1212/WNL.55.7.1040. PMID 11061267.
- ↑ "Genetic heterogeneity in Italian families with familial hemiplegic migraine". Neurology 53 (1): 26–33. 1999. doi:10.1212/WNL.53.1.26. PMID 10408532.
- ↑ "High prevalence of CACNA1A truncations and broader clinical spectrum in episodic ataxia type 2". Neurology 52 (9): 1816–21. 1999. doi:10.1212/WNL.52.9.1816. PMID 10371528.
- ↑ "A novel nonsense mutation in CACNA1A causes episodic ataxia and hemiplegia". Neurology 53 (1): 34–7. 1999. doi:10.1212/WNL.53.1.34. PMID 10408533.
- ↑ "Loss-of-function EA2 mutations are associated with impaired neuromuscular transmission". Neurology 57 (10): 1843–8. 2001. doi:10.1212/WNL.57.10.1843. PMID 11723274.
- ↑ "New CACNA1A gene mutation in a case of familial hemiplegic migraine with status epilepticus". Eur Neurol 52 (1): 58–61. 2004. doi:10.1159/000079546. PMID 15240985.
- ↑ "Alternating hemiplegia of childhood: no mutations in the second familial hemiplegic migraine gene ATP1A2". Neuropediatrics 35 (5): 293–6. 2004. doi:10.1055/s-2004-821082. PMID 15534763.
- ↑ 27.0 27.1 27.2 "Rare missense variants in ATP1A2 in families with clustering of common forms of migraine". Hum Mutat 26 (4): 315–21. 2005. doi:10.1002/humu.20229. PMID 16110494.
- ↑ 28.0 28.1 28.2 28.3 28.4 28.5 28.6 28.7 "ATP1A2 mutations in 11 families with familial hemiplegic migraine". Hum Mutat 26 (3): 281. 2005. doi:10.1002/humu.9361. PMID 16088919.
- ↑ "A G301R Na+/K+-ATPase mutation causes familial hemiplegic migraine type 2 with cerebellar signs". Neurogenetics 5 (3): 177–85. 2004. doi:10.1007/s10048-004-0183-2. PMID 15459825.
- ↑ "A novel missense ATP1A2 mutation in a Finnish family with familial hemiplegic migraine type 2". Neurogenetics 5 (2): 141–6. 2004. doi:10.1007/s10048-004-0178-z. PMID 15133718.
- ↑ 31.0 31.1 31.2 31.3 31.4 "Kinetic alterations due to a missense mutation in the Na,K-ATPase alpha2 subunit cause familial hemiplegic migraine type 2". J Biol Chem 279 (42): 43692–6. 2004. doi:10.1074/jbc.M407471200. PMID 15308625.
- ↑ 32.0 32.1 32.2 32.3 32.4 32.5 32.6 "Variability of familial hemiplegic migraine with novel A1A2 Na+/K+-ATPase variants". Neurology 62 (10): 1857–61. 2004. doi:10.1212/01.WNL.0000127310.11526.FD. PMID 15159495.
- ↑ "Alternating hemiplegia of childhood or familial hemiplegic migraine? A novel ATP1A2 mutation". Ann Neurol 55 (6): 884–7. 2004. doi:10.1002/ana.20134. PMID 15174025.
- ↑ "Familial basilar migraine associated with a new mutation in the ATP1A2 gene". Neurology 65 (11): 1826–8. 2005. doi:10.1212/01.wnl.0000187072.71931.c0. PMID 16344534.
- ↑ 35.0 35.1 "Two de novo mutations in the Na,K-ATPase gene ATP1A2 associated with pure familial hemiplegic migraine". Eur J Hum Genet 14 (5): 555–60. 2006. doi:10.1038/sj.ejhg.5201607. PMID 16538223.
- ↑ "Severe episodic neurological deficits and permanent mental retardation in a child with a novel FHM2 ATP1A2 mutation". Ann Neurol 59 (2): 310–4. 2006. doi:10.1002/ana.20760. PMID 16437583.
- ↑ 37.0 37.1 "Novel mutations in the Na+, K+-ATPase pump gene ATP1A2 associated with familial hemiplegic migraine and benign familial infantile convulsions". Ann Neurol 54 (3): 360–6. 2003. doi:10.1002/ana.10674. PMID 12953268.
- ↑ 38.0 38.1 "Alterations in the α2 isoform of Na,K-ATPase associated with familial hemiplegic migraine type 2". Proc Natl Acad Sci USA 102 (31): 11106–11. 2005. doi:10.1073/pnas.0504323102. PMID 16037212. Bibcode: 2005PNAS..10211106S.
- ↑ "A novel ATP1A2 mutation in a family with FHM type II". Cephalalgia 26 (3): 324–8. 2006. doi:10.1111/j.1468-2982.2006.01002.x. PMID 16472340.
- ↑ 40.0 40.1 "Haploinsufficiency of ATP1A2 encoding the Na+/K+ pump alpha2 subunit associated with familial hemiplegic migraine type 2". Nat Genet 33 (2): 192–6. 2003. doi:10.1038/ng1081. PMID 12539047.
- ↑ 41.0 41.1 "Na,K-ATPase mutations in familial hemiplegic migraine lead to functional inactivation". Biochim Biophys Acta 1669 (1): 61–8. 2005. doi:10.1016/j.bbamem.2005.01.003. PMID 15843000.
- ↑ "Mutation in the neuronal voltage-gated sodium channel SCN1A in familial hemiplegic migraine". Lancet 366 (9483): 371–7. 2005. doi:10.1016/S0140-6736(05)66786-4. PMID 16054936.
- ↑ "A new locus for hemiplegic migraine maps to chromosome 1q31". Neurology 49 (5): 1231–8. 1997. doi:10.1212/WNL.49.5.1231. PMID 9371899.
- ↑ Ducros, A (Apr 22, 2013). "[Genetics of migraine.]". Revue Neurologique 169 (5): 360–71. doi:10.1016/j.neurol.2012.11.010. PMID 23618705.
- ↑ Suzuki, M.; Van Paesschen, W.; Stalmans, I.; Horita, S.; Yamada, H.; Bergmans, B. A.; Legius, E.; Riant, F. et al. (23 August 2010). "Defective membrane expression of the Na+-HCO3- cotransporter NBCe1 is associated with familial migraine". Proceedings of the National Academy of Sciences 107 (36): 15963–15968. doi:10.1073/pnas.1008705107. PMID 20798035. Bibcode: 2010PNAS..10715963S.
- ↑ "Familial hemiplegic migraine with prolonged global aura: follow-up findings of subtraction ictal SPECT co-registered to MRI (SISCOM)". Cephalalgia 32 (13): 1013–1014. 2012. doi:10.1177/0333102412457093. PMID 22933508.
- ↑ "An epidemiological survey of hemiplegic migraine". Cephalalgia 22 (5): 361–75. 2002. doi:10.1046/j.1468-2982.2002.00371.x. PMID 12110112.
External links
- GeneReviews/NCBI/NIH/UW entry on Familial Hemiplegic Migraine
- "The International Classification of Headache Disorders 2nd Edition". Cephalalgia 24 (s1): 8–160. May 2004. ISSN 1468-2982. https://onlinelibrary.wiley.com/toc/14682982/2004/24/s1.
| Classification | |
|---|---|
| External resources |
 |
