Medicine:Multi-drug-resistant tuberculosis
| Multi-drug-resistance tuberculosis | |
|---|---|
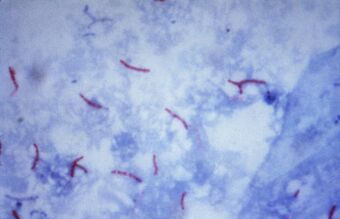 | |
| Mycobacterium tuberculosis bacteria seen by microscope | |
| Specialty | Infectious disease |
Multi-drug-resistant tuberculosis (MDR-TB) is a form of tuberculosis (TB) infection caused by bacteria that are resistant to treatment with at least two of the most powerful first-line anti-TB medications (drugs), isoniazid and rifampin. Some forms of TB are also resistant to second-line medications, and are called extensively drug-resistant TB (XDR-TB).[1]
Tuberculosis is caused by infection with the bacteria Mycobacterium tuberculosis. Almost one in four people in the world are infected with TB bacteria.[1] Only when the bacteria become active do people become ill with TB. Bacteria become active as a result of anything that can reduce the person's immunity, such as HIV, advancing age, diabetes or other immunocompromising illnesses. TB can usually be treated with a course of four standard, or first-line, anti-TB drugs (i.e., isoniazid, rifampin and any fluoroquinolone).[2]
However, beginning with the first antibiotic treatment for TB in 1943, some strains of the TB bacteria developed resistance to the standard drugs through genetic changes (see mechanisms.)[2][3][4] Currently the majority of multidrug-resistant cases of TB are due to one strain of TB bacteria called the Beijing lineage.[5][6] This process accelerates if incorrect or inadequate treatments are used, leading to the development and spread of multidrug-resistant TB (MDR-TB). Incorrect or inadequate treatment may be due to use of the wrong medications, use of only one medication (standard treatment is at least two drugs), not taking medication consistently or for the full treatment period (treatment is required for several months).[7][8][9] Treatment of MDR-TB requires second-line drugs (i.e., fluoroquinolones, aminoglycosides, and others), which in general are less effective, more toxic and much more expensive than first-line drugs.[7] Treatment schedules for MDR-TB involving fluoroquinolones and aminoglycosides can run for 2 years, compared to the 6 months of first-line drug treatment, and cost over US$100,000.[10] If these second-line drugs are prescribed or taken incorrectly, further resistance can develop leading to XDR-TB.
Resistant strains of TB are already present in the population, so MDR-TB can be directly transmitted from an infected person to an uninfected person. In this case a previously untreated person develops a new case of MDR-TB. This is known as primary MDR-TB, and is responsible for up to 75% of cases.[11] Acquired MDR-TB develops when a person with a non-resistant strain of TB is treated inadequately, resulting in the development of antibiotic resistance in the TB bacteria infecting them. These people can in turn infect other people with MDR-TB.[4][7]
MDR-TB caused an estimated 600,000 new TB cases and 240,000 deaths in 2016 and MDR-TB accounts for 4.1% of all new TB cases and 19% of previously treated cases worldwide.[12] Globally, most MDR-TB cases occur in South America, Southern Africa, India, China, and the former Soviet Union.[13]
Treatment of MDR-TB requires treatment with second-line drugs, usually four or more anti-TB drugs for a minimum of 6 months, and possibly extending for 18–24 months if rifampin resistance has been identified in the specific strain of TB with which the patient has been infected.[8] Under ideal program conditions, MDR-TB cure rates can approach 70%.[8]
Mechanism of drug resistance
The TB bacteria has natural defenses against some drugs, and can acquire drug resistance through genetic mutations. The bacteria does not have the ability to transfer genes for resistance between organisms through plasmids (see horizontal transfer). Some mechanisms of drug resistance include:[14]
- Cell wall: The cell wall of M. tuberculosis (TB) contains complex lipid molecules which act as a barrier to stop drugs from entering the cell.
- Drug modifying & inactivating enzymes: The TB genome codes for enzymes (proteins) that inactivate drug molecules. These enzymes usually phosphorylate, acetylate, or adenylate drug compounds.
- Drug efflux systems: The TB cell contains molecular systems that actively pump drug molecules out of the cell.
- Mutations: Spontaneous mutations in the TB genome can alter proteins which are the target of drugs, making the bacteria drug resistant.[15]
One example is a mutation in the rpoB gene, which encodes the beta subunit of the bacteria's RNA polymerase. In non-resistant TB, rifampin binds the beta subunit of RNA polymerase and disrupt transcription elongation. Mutation in the rpoB gene changes the sequence of amino acids and eventual conformation of the beta subunit. In this case rifampin can no longer bind or prevent transcription, and the bacteria is resistant.
Other mutations make the bacterium resistant to other drugs. For example, there are many mutations that confer resistance to isoniazid (INH), including in the genes katG, inhA, ahpC and others. Amino acid replacements in the NADH binding site of InhA apparently result in INH resistance by preventing the inhibition of mycolic acid biosynthesis, which the bacterium uses in its cell wall. Mutations in the katG gene make the enzyme catalase peroxidase unable to convert INH to its biologically active form. Hence, INH is ineffective and the bacteria is resistant.[16][17] The discovery of new molecular targets is essential to overcome drug resistant problems.[18]
In some TB bacteria, the acquisition of these mutations can be explained other mutations in the DNA recombination, recognition and repair machinery.[19] Mutations in these genes allow the bacteria to have a higher overall mutation rate and to accumulate mutations that cause drug resistance more quickly.[20][21]
Extensively drug-resistant TB
MDR-TB can become resistant to the major second-line TB drug groups: fluoroquinolones (moxifloxacin, ofloxacin) and injectable aminoglycoside or polypeptide drugs (amikacin, capreomycin, kanamycin). When MDR-TB is resistant to at least one drug from each group, it is classified as extensively drug-resistant tuberculosis (XDR-TB).[7]
In a study of MDR-TB patients from 2005 to 2008 in various countries, 43.7% had resistance to at least one second-line drug.[22] About 9% of MDR-TB cases are resistant to a drug from both classes and classified as XDR-TB.[1][23]
In the past 10 years TB strains have emerged in Italy, Iran, India, and South Africa which are resistant to all available first and second line TB drugs, classified as totally drug-resistant tuberculosis, though there is some controversy over this term.[24][25][26] Increasing levels of resistance in TB strains threaten to complicate the current global public health approaches to TB control. New drugs are being developed to treat extensively resistant forms but major improvements in detection, diagnosis, and treatment will be needed.[25]
Prevention
There are several ways that drug resistance to TB, and drug resistance in general, can be prevented:[27][28]
- Rapid diagnosis & treatment of TB: One of the greatest risk factors for drug resistant TB is problems in treatment and diagnosis, especially in developing countries. If TB is identified and treated soon, drug resistance can be avoided.
- Completion of treatment: Previous treatment of TB is an indicator of MDR TB. If the patient does not complete his/her antibiotic treatment, or if the physician does not prescribe the proper antibiotic regimen, resistance can develop. Also, drugs that are of poor quality or less in quantity, especially in developing countries, contribute to MDR TB.
- Patients with HIV/AIDS should be identified and diagnosed as soon as possible. They lack the immunity to fight the TB infection and are at great risk of developing drug resistance.
- Identify contacts who could have contracted TB: i.e. family members, people in close contact, etc.
- Research: Much research and funding is needed in the diagnosis, prevention and treatment of TB and MDR TB.
"Opponents of a universal tuberculosis treatment, reasoning from misguided notions of cost-effectiveness, fail to acknowledge that MDRTB is not a disease of poor people in distant places. The disease is infectious and airborne. Treating only one group of patients looks inexpensive in the short run, but will prove disastrous for all in the long run."— Paul Farmer [29]
DOTS-Plus
Community-based treatment programs such as DOTS-Plus, a MDR-TB-specialized treatment using the popular Directly Observed Therapy – Short Course (DOTS) initiative, have shown considerable success in the world. In these locales, these programs have proven to be a good option for proper treatment of MDR-TB in poor, rural areas. A successful example has been in Lima, Peru, where the program has seen cure rates of over 80%.[30]
However, TB clinicians[who?] have expressed concern in the DOTS program administered in the Republic of Georgia because it is anchored in a passive case finding. This means that the system depends on patients coming to health care providers, without conducting compulsory screenings. As medical anthropologists like Erin Koch have shown, this form of implementation does not suit all cultural structures. They urge that the DOTS protocol be constantly reformed in the context of local practices, forms of knowledge and everyday life.[31]
Erin Koch has used Paul Farmer's concept of "structural" violence as a perspective for understanding how "institutions, environment, poverty, and power reproduce, solidify, and naturalize the uneven distribution of disease and access to resources". She has also studied the effectiveness of the DOTS protocol in the widespread disease of tuberculosis in the Georgian prison system.[32] Unlike the DOTS passive case finding used for the general Georgian public, the multiple-level surveillance in the prison system has proven more successful in reducing the spread of tuberculosis while increasing rates of cure.[citation needed]
Koch critically notes that because the DOTS protocol aims to change the individual's behavior without addressing the need to change the institutional, political, and economic contexts, certain limitations arise, such as MDR tuberculosis.[citation needed]
Treatment
Usually, multidrug-resistant tuberculosis can be cured with long treatments of second-line drugs, but these are more expensive than first-line drugs and have more adverse effects.[33] The treatment and prognosis of MDR-TB are much more akin to those for cancer than to those for infection. MDR-TB has a mortality rate of up to 80%, which depends on a number of factors, including:
- How many drugs the organism is resistant to (the fewer the better)
- How many drugs the patient is given (patients treated with five or more drugs do better)
- The expertise and experience of the physician responsible
- How co-operative the patient is with treatment (treatment is arduous and long, and requires persistence and determination on the part of the patient)
- Whether the patient is HIV-positive or not (HIV co-infection is associated with an increased mortality).
The majority of patients suffering from multi-drug-resistant tuberculosis do not receive treatment, as they are found in underdeveloped countries or in poverty. Denial of treatment remains a difficult human rights issue, as the high cost of second-line medications often precludes those who cannot afford therapy.[34]
A study of cost-effective strategies for tuberculosis control supported three major policies. First, the treatment of smear-positive cases in DOTS programs must be the foundation of any tuberculosis control approach, and should be a basic practice for all control programs. Second, there is a powerful economic case for treating smear-negative and extra-pulmonary cases in DOTS programs along with treating smear-negative and extra-pulmonary cases in DOTS programs as a new WHO "STOP TB" approach and the second global plan for tuberculosis control. Last, but not least, the study shows that significant scaling up of all interventions is needed in the next 10 years if the millennium development goal and related goals for tuberculosis control are to be achieved. If the case detection rate can be improved, this will guarantee that people who gain access to treatment facilities are covered and that coverage is widely distributed to people who do not now have access.[35]
In general, treatment courses are measured in months to years; MDR-TB may require surgery, and death rates remain high despite optimal treatment. However, good outcomes for patients are still possible.[36]
The treatment of MDR-TB must be undertaken by physicians experienced in the treatment of MDR-TB. Mortality and morbidity in patients treated in non-specialist centers are significantly higher to those of patients treated in specialist centers. Treatment of MDR-TB must be done on the basis of sensitivity testing: it is impossible to treat such patients without this information. When treating a patient with suspected MDR-TB, pending the result of laboratory sensitivity testing, the patient could be started on SHREZ (Streptomycin+ isonicotinyl Hydrazine+ Rifampicin+Ethambutol+ pyraZinamide) and moxifloxacin with cycloserine. There is evidence that previous therapy with a drug for more than a month is associated with diminished efficacy of that drug regardless of in vitro tests indicating susceptibility.[37] Hence, a detailed knowledge of the treatment history of each patient is essential. In addition to the obvious risks (i.e., known exposure to a patient with MDR-TB), risk factors for MDR-TB include HIV infection, previous incarceration, failed TB treatment, failure to respond to standard TB treatment, and relapse following standard TB treatment.
A gene probe for rpoB is available in some countries. This serves as a useful marker for MDR-TB, because isolated RMP resistance is rare (except when patients have a history of being treated with rifampicin alone). If the results of a gene probe (rpoB) are known to be positive, then it is reasonable to omit RMP and to use SHEZ+MXF+cycloserine. The reason for maintaining the patient on INH is that INH is so potent in treating TB that it is foolish to omit it until there is microbiological proof that it is ineffective (even though isoniazid resistance so commonly occurs with rifampicin resistance).
For treatment of RR- and MDT-TB, WHO treatment guidelines are as follows: "a regimen with at least five effective TB medicines during the intensive phase is recommended, including pyrazinamide and four core second-line TB medicines – one chosen from Group A, one from Group B, and at least two from Group C3 (conditional recommendation, very low certainty in the evidence). If the minimum number of effective TB medicines cannot be composed as given above, an agent from Group D2 and other agents from Group D3 may be added to bring the total to five. It is recommended that the regimen be further strengthened with high-dose isoniazid and/or ethambutol (conditional recommendation, very low certainty in the evidence)." [38] Medicines recommended are the following:
- Group A: Fluoroquinolones (levofloxacinm moxifloxicin, gatifloxacin), linezolid, bedaquiline
- Group B: clofazimine, cycloserine/terizidone
- Group C: Other core second-line agents (ethambutol, delamanid, pyrazinamide, imipenem-cilastatin/meropenem, amikacin/streptomycin, ethionamide/prothionamide, p-aminosalicylic acid)
For patients with RR-TB or MDR-TB, "not previously treated with second-line drugs and in whom resistance to fluoroquinolones and second-line injectable agents was excluded or is considered highly unlikely, a shorter MDR-TB regimen of 9–12 months may be used instead of the longer regimens (conditional recommendation, very low certainty in the evidence)." [39]
In general, resistance to one drug within a class means resistance to all drugs within that class, but a notable exception is rifabutin: Rifampicin-resistance does not always mean rifabutin-resistance, and the laboratory should be asked to test for it. It is possible to use only one drug within each drug class. If it is difficult finding five drugs to treat then the clinician can request that high-level INH-resistance be looked for. If the strain has only low-level INH-resistance (resistance at 0.2 mg/l INH, but sensitive at 1.0 mg/l INH), then high dose INH can be used as part of the regimen. When counting drugs, PZA and interferon count as zero; that is to say, when adding PZA to a four-drug regimen, another drug must be chosen to make five. It is not possible to use more than one injectable (STM, capreomycin or amikacin), because the toxic effect of these drugs is additive: If possible, the aminoglycoside should be given daily for a minimum of three months (and perhaps thrice weekly thereafter). Ciprofloxacin should not be used in the treatment of tuberculosis if other fluoroquinolones are available. As of 2008, Cochrane reports that trials of other fluoroquinolones are ongoing.[40]
There is no intermittent regimen validated for use in MDR-TB, but clinical experience is that giving injectable drugs for five days a week (because there is no-one available to give the drug at weekends) does not seem to result in inferior results. Directly observed therapy helps to improve outcomes in MDR-TB and should be considered an integral part of the treatment of MDR-TB.[41]
Response to treatment must be obtained by repeated sputum cultures (monthly if possible). Treatment for MDR-TB must be given for a minimum of 18 months and cannot be stopped until the patient has been culture-negative for a minimum of nine months. It is not unusual for patients with MDR-TB to be on treatment for two years or more.[citation needed]
Patients with MDR-TB should be isolated in negative-pressure rooms, if possible. Patients with MDR-TB should not be accommodated on the same ward as immunosuppressed patients (HIV-infected patients, or patients on immunosuppressive drugs). Careful monitoring of compliance with treatment is crucial to the management of MDR-TB (and some physicians insist on hospitalisation if only for this reason). Some physicians will insist that these patients remain isolated until their sputum is smear-negative, or even culture-negative (which may take many months, or even years). Keeping these patients in hospital for weeks (or months) on end may be a practical or physical impossibility, and the final decision depends on the clinical judgement of the physician treating that patient. The attending physician should make full use of therapeutic drug monitoring (in particular, of the aminoglycosides) both to monitor compliance and to avoid toxic effects.
Some supplements may be useful as adjuncts in the treatment of tuberculosis, but, for the purposes of counting drugs for MDR-TB, they count as zero (if four drugs are already in the regimen, it may be beneficial to add arginine or vitamin D or both, but another drug will be needed to make five). Supplements are: arginine[42] (peanuts are a good source), vitamin D,[43] Dzherelo,[44] V5 Immunitor.[45]
The drugs listed below have been used in desperation, and it is uncertain as to whether they are effective at all. They are used when it is not possible to find five drugs from the list above. imipenem,[46] co-amoxiclav,[47][48] clofazimine,[49][50][51] prochlorperazine,[52] metronidazole.[53]
On 28 December 2012, the U.S. Food and Drug Administration (FDA) approved bedaquiline (marketed as Sirturo by Johnson & Johnson) to treat multi-drug resistant tuberculosis, the first new treatment in 40 years. Sirturo is to be used in a combination therapy for patients who have failed standard treatment and have no other options. Sirturo is an adenosine triphosphate synthase (ATP synthase) inhibitor.[54][55]
The following drugs are experimental compounds that are not commercially available, but may be obtained from the manufacturer as part of a clinical trial or on a compassionate basis. Their efficacy and safety are unknown: pretomanid[56] (manufactured by Novartis, developed in partnership with TB Alliance),[57] and delamanid.
In cases of extremely resistant disease, surgery to remove infection portions of the lung is, in general, the final option. The center with the largest experience in this is the National Jewish Medical and Research Center in Denver, Colorado. In 17 years of experience, they have performed 180 operations; of these, 98 were lobectomies and 82 were pneumonectomies. There is a 3.3% operative mortality, with an additional 6.8% dying following the operation; 12% experienced significant morbidity (in particular, extreme breathlessness). Of 91 patients who were culture-positive before surgery, only 4 were culture-positive after surgery.
The resurgence of tuberculosis in the United States, the advent of HIV-related tuberculosis, and the development of strains of TB resistant to the first-line therapies developed in recent decades—serve to reinforce the thesis that Mycobacterium tuberculosis, the causative organism, makes its own preferential option for the poor.[58] The simple truth is that almost all tuberculosis deaths result from a lack of access to existing effective therapy.[59]
Treatment success rates remain unacceptably low globally with variation between regions. 2016 data published by the WHO[60] reported treatment success rates of Multi-drug resistant TB globally. For those started on treatment for multi-drug resistant TB 56% successfully completed treatment, either treatment course completion or eradication of disease; 15% of those died while in treatment; 15% were lost to follow-up; 8% had treatment failure and there was no data on the remaining 6%. Treatment success rate was highest in the World Health Organization Mediterranean region at 65%. Treatment success rates were lower than 50% in the Ukraine, Mozambique, Indonesia and India. Areas with poor TB surveillance infrastructure had higher rates of loss to follow-up of treatment.[61]
57 countries reported outcomes for patients started on extreme-drug resistant Tuberculosis, this included 9258 patients. 39% completed treatment successfully, 26% of patients died and treatment failed for 18%. 84% of the extreme Drug resistant Cohort was made up of only three countries; India, Russian Federation and Ukraine. Shorter treatment regimes for MDR-TB have been found to be beneficial having higher treatment success rates.[62]
Epidemiology
Cases of MDR tuberculosis have been reported in every country surveyed.[34] MDR-TB most commonly develops in the course of TB treatment,[4] and is most commonly due to doctors giving inappropriate treatment, or patients missing doses or failing to complete their treatment. Because MDR tuberculosis is an airborne pathogen, persons with active, pulmonary tuberculosis caused by a multidrug-resistant strain can transmit the disease if they are alive and coughing.[34] TB strains are often less fit and less transmissible, and outbreaks occur more readily in people with weakened immune systems (e.g., patients with HIV).[63][64][65][66][67] Outbreaks among non immunocompromised healthy people do occur,[68] but are less common.[4]
As of 2013, 3.7% of new tuberculosis cases have MDR-TB. Levels are much higher in those previously treated for tuberculosis - about 20%. WHO estimates that there were about 0.5 million new MDR-TB cases in the world in 2011. About 60% of these cases occurred in Brazil, China, India, the Russian Federation and South Africa alone.[23] In Moldova, the crumbling health system has led to the rise of MDR-TB.[69] In 2013, the Mexico–United States border was noted to be "a very hot region for drug resistant TB", though the number of cases remained small.[70]
It has been known for many years that INH-resistant TB is less virulent in guinea pigs, and the epidemiological evidence is that MDR strains of TB do not dominate naturally. A study in Los Angeles, California, found that only 6% of cases of MDR-TB were clustered. Likewise, the appearance of high rates of MDR-TB in New York City in the early 1990s was associated with the explosion of AIDS in that area.[71][72] In New York City, a report issued by city health authorities states that fully 80 percent of all MDR-TB cases could be traced back to prisons and homeless shelters.[73] When patients have MDR-TB, they require longer periods of treatment—about two years of multidrug regimen. Several of the less powerful second-line drugs, which are required to treat MDR-TB, are also more toxic, with side effects such as nausea, abdominal pain, and even psychosis. The Partners in Health team had treated patients in Peru who were sick with strains that were resistant to ten and even twelve drugs. Most such patients require adjuvant surgery for any hope of a cure.[74]
Somalia
MDR-TBC is widespread in Somalia, where 8.7% of newly discovered TB cases are restistant to Rifampicin and Isoniazid, in patients which were treated previously the share was 47%.[75]
Refugees from Somalia brought an until then unknown variant of MDR tuberculosis with them to Europe. A few number of cases in four different countries were considered by the European Centre for Disease Prevention and Control to pose no risk to the native population.[76]
Russian prisons
One of the so-called "hot-spots" of drug-resistant tuberculosis is within the Russian prison system. Infectious disease researchers Nachega & Chaisson report that 10% of the one million prisoners within the system have active TB.[77] One of their studies found that 75% of newly diagnosed inmates with TB are resistant to at least one drug; 40% of new cases are multi-drug resistant.[77] In 1997, TB accounted for almost half of all Russian prison deaths, and as Bobrik et al. point out in their public health study, the 90% reduction in TB incidence contributed to a consequential fall in the prisoner death rate in the years following 1997.[78] Baussano et al. articulate that concerning statistics like these are especially worrisome because spikes in TB incidence in prisons are linked to corresponding outbreaks in surrounding communities.[79] Additionally, rising rates of incarceration, especially in Central Asian and Eastern European countries like Russia, have been correlated with higher TB rates in civilian populations.[78] Even as the DOTS program is expanded throughout Russian prisons, researchers such as Shin et al. have noted that wide-scale interventions have not had their desired effect, especially with regard to the spread of drug-resistant strains of TB.[80]
Contributing factors
There are several elements of the Russian prison system that enable the spread of MDR-TB and heighten its severity. Overcrowding in prisons is especially conducive to the spread of tuberculosis; an inmate in a prison hospital has (on average) 3 meters of personal space, and an inmate in a correctional colony has 2 meters.[78] Specialized hospitals and treatment facilities within the prison system, known as TB colonies, are intended to isolate infected prisoners to prevent transmission; however, as Ruddy et al. demonstrate, there are not enough of these colonies to sufficiently protect staff and other inmates.[81] Additionally, many cells lack adequate ventilation, which increases likelihood of transmission. Bobrik et al. have also noted food shortages within prisons, which deprive inmates of the nutrition necessary for healthy functioning.[78]
Comorbidity of HIV within prison populations has also been shown to worsen health outcomes. Nachega & Chaisson articulate that while HIV-infected prisoners are not more susceptible MDR-TB infection, they are more likely to progress to serious clinical illness if infected.[77] According to Stern, HIV infection is 75 times more prevalent in Russian prison populations than in the civilian population.[82] Therefore, prison inmates are both more likely to become infected with MDR-TB initially and to experience severe symptoms because of previous exposure to HIV.
Shin et al. emphasize another factor in MDR-TB prevalence in Russian prisons: alcohol and substance use.[80] Ruddy et al. showed that risk for MDR-TB is three times higher among recreational drug users than non-users.[81] Shin et al.'s study demonstrated that alcohol usage was linked to poorer outcomes in MDR-TB treatment; they also noted that a majority of subjects within their study (many of whom regularly used alcohol) were nevertheless cured by their aggressive treatment regimen.[80]
Non-compliance with treatment plans is often cited as a contributor to MDR-TB transmission and mortality. Indeed, of the 80 newly-released TB-infected inmates in Fry et al.'s study, 73.8% did not report visiting a community dispensary for further treatment.[83] Ruddy et al. cite release from facilities as one of the main causes of interruption in prisoner's TB treatment, in addition to non-compliance within the prison and upon reintegration into civilian life.[81] Fry et al.'s study also listed side effects of TB treatment medications (especially in HIV positive individuals), financial worries, housing insecurities, family problems, and fear of arrest as factors that prevented some prisoners from properly adhering to TB treatment.[83] They also note that some researchers have argued that the short-term gains TB-positive prisoners receive, such as better food or work exclusion, may dis-incentivize becoming cured.[83] In their World Health Organization article, Gelmanova et al. posit that non-adherence to TB treatment indirectly contributes to bacterial resistance.[84] Although ineffective or inconsistent treatment does not "create" resistant strains, mutations within the high bacterial load in non-adherent prisoners can cause resistance.
Nachega & Chaisson argue that inadequate TB control programs are the strongest driver of MDR-TB incidence.[77] They note that prevalence of MDR-TB is 2.5 times higher in areas of poorly controlled TB.[77] Russian-based therapy (i.e., not DOTS) has been criticized by Kimerling et al. as "inadequate" in properly controlling TB incidence and transmission.[85] Bobrik et al. note that treatment for MDR-TB is equally inconsistent; the second-line drugs used to treat the prisoners lack specific treatment guidelines, infrastructure, training, or follow-up protocols for prisoners reentering civilian life.[78]
Policy impacts
As Ruddy et al. note in their scholarly article, Russia's recent penal reforms will greatly reduce the number of inmates inside prison facilities and thus increase the number of ex-convicts integrated into civilian populations.[81] Because the incidence of MDR-TB is strongly predicted by past imprisonment, the health of Russian society will be greatly impacted by this change.[81] Formerly incarcerated Russians will re-enter civilian life and remain within that sphere; as they live as civilians, they will infect others with the contagions they were exposed to in prison. Researcher Vivian Stern argues that the risk of transmission from prison populations to the general public calls for an integration of prison healthcare and national health services to better control both TB and MDR-TB.[82] While second-line drugs necessary for treating MDR-TB are arguably more expensive than a typical regimen of DOTS therapy, infectious disease specialist Paul Farmer posits that the outcome of leaving infected prisoners untreated could cause a massive outbreak of MDR-TB in civilian populations, thereby inflicting a heavy toll on society.[86] Additionally, as MDR-TB spreads, the threat of the emergence of totally-drug-resistant TB becomes increasingly apparent.
See also
- 2007 tuberculosis scare
- Drug resistance
- MRSA
- Vancomycin-resistant enterococcus (VRE)
- Totally drug-resistant tuberculosis (TDR-TB)
References
- ↑ 1.0 1.1 1.2 "Diagnosis and notification of multidrug-resistant TB". World Health Organization (WHO). http://www.who.int/tb/challenges/mdr/mdr_tb_factsheet.pdf. Retrieved 7 December 2016.
- ↑ 2.0 2.1 Longo, Fausci (2012). Harrison's Principles of Internal Medicine (18th ed.). New York: McGraw Hill. pp. Chapter 165: Tuberculosis. http://accessmedicine.mhmedical.com/content.aspx?bookid=331&Sectionid=40726917. Retrieved 7 Dec 2016.
- ↑ "Chapter 168. Antimycobacterial Agents | Harrison's Principles of Internal Medicine, 18e". AccessMedicine | McGraw-Hill Medical. http://accessmedicine.mhmedical.com/content.aspx?bookid=331&Sectionid=40726917. Retrieved 2016-12-07.
- ↑ 4.0 4.1 4.2 4.3 Wood, Alastair J.J.; Iseman, Michael D. (1993). "Treatment of Multidrug-Resistant Tuberculosis". New England Journal of Medicine 329 (11): 784–91. doi:10.1056/NEJM199309093291108. PMID 8350889.
- ↑ Stoffels, Karolien; Allix-Béguec, Caroline; Groenen, Guido; Wanlin, Maryse; Berkvens, Dirk; Mathys, Vanessa; Supply, Philip; Fauville-Dufaux, Maryse (2013-05-09). "From Multidrug- to Extensively Drug-Resistant Tuberculosis: Upward Trends as Seen from a 15-Year Nationwide Study". PLOS One 8 (5): e63128. doi:10.1371/journal.pone.0063128. ISSN 1932-6203. PMID 23671662. Bibcode: 2013PLoSO...863128S.
- ↑ Parwati, Ida; Crevel, Reinout van; Soolingen, Dick van (February 2010). "Possible underlying mechanisms for successful emergence of the Mycobacterium tuberculosis Beijing genotype strains". The Lancet Infectious Diseases 10 (2): 103–111. doi:10.1016/s1473-3099(09)70330-5. PMID 20113979.
- ↑ 7.0 7.1 7.2 7.3 Millard, James; Ugarte-Gil, Cesar; Moore, David A. J. (2015-02-26). "Multidrug resistant tuberculosis". BMJ 350: h882. doi:10.1136/bmj.h882. ISSN 1756-1833. PMID 25721508. http://www.bmj.com/content/350/bmj.h882.
- ↑ 8.0 8.1 8.2 Adams and Woelke (2014). Understanding Global Health. Chapter 10: TB and HIV/AIDS (12th ed.). McGraw Hill. http://accessmedicine.mhmedical.com/content.aspx?bookid=710&Sectionid=46796911. Retrieved 9 May 2015.
- ↑ Keshavjee, Salmaan; Farmer, Paul E. (2012-09-06). "Tuberculosis, Drug Resistance, and the History of Modern Medicine". New England Journal of Medicine 367 (10): 931–936. doi:10.1056/NEJMra1205429. ISSN 0028-4793. PMID 22931261.
- ↑ Kaplan, Jeffrey. 2017. "Tuberculosis" American University. Lecture.
- ↑ Nathanson, Eva; Nunn, Paul; Uplekar, Mukund; Floyd, Katherine; Jaramillo, Ernesto; Lönnroth, Knut; Weil, Diana; Raviglione, Mario (2010-09-09). "MDR Tuberculosis — Critical Steps for Prevention and Control". New England Journal of Medicine 363 (11): 1050–1058. doi:10.1056/NEJMra0908076. ISSN 0028-4793. PMID 20825317. http://whqlibdoc.who.int/publications/2010/9789241599191_eng.pdf.
- ↑ "Drug-resistant tuberculosis" (in en-GB). http://www.who.int/tb/areas-of-work/drug-resistant-tb/en/.
- ↑ "Multi-drug-resistant tuberculosis (MDR-TB) – 2015 Update". World Health Organization (WHO). https://extranet.who.int/sree/Reports?op=vs&path=/WHO_HQ_Reports/G2/PROD/EXT/MDRTB_Indicators_map. Retrieved 7 December 2016.
- ↑ Sandhu, P; Akhter, Y (26 September 2017). "Evolution of structural fitness and multifunctional aspects of mycobacterial RND family transporters.". Archives of Microbiology 200 (1): 19–31. doi:10.1007/s00203-017-1434-6. PMID 28951954.
- ↑ Louw, G. E.; Warren, R. M.; Gey Van Pittius, N. C.; McEvoy, C. R. E.; Van Helden, P. D.; Victor, T. C. (2009). "A Balancing Act: Efflux/Influx in Mycobacterial Drug Resistance". Antimicrobial Agents and Chemotherapy 53 (8): 3181–9. doi:10.1128/AAC.01577-08. PMID 19451293.
- ↑ Gillespie, S. H. (2002). "Evolution of Drug Resistance in Mycobacterium tuberculosis: Clinical and Molecular Perspective". Antimicrobial Agents and Chemotherapy 46 (2): 267–74. doi:10.1128/AAC.46.2.267-274.2002. PMID 11796329.
- ↑ Ramaswamy, S; Musser, JM (1998). "Molecular genetic basis of antimicrobial agent resistance in Mycobacterium tuberculosis: 1998 update". Tubercle and Lung Disease 79 (1): 3–29. doi:10.1054/tuld.1998.0002. PMID 10645439.
- ↑ Baptista, Rafael; Bhowmick, Sumana; Nash, Robert J; Baillie, Les; Mur, Luis AJ (2018-03-23). "Target discovery focused approaches to overcome bottlenecks in the exploitation of antimycobacterial natural products" (in EN). Future Medicinal Chemistry 10 (7): 811–822. doi:10.4155/fmc-2017-0273. PMID 29569936. http://orca.cf.ac.uk/110455/8/Target%20discovery%20focused%20approaches%20to%20overcome%20bottlenecks%20in%20the%20exploitation%20of%20antimycobacterial%20natural%20products.pdf.
- ↑ Hanekom, M.; Pittius, N.C. Gey van; McEvoy, C.; Victor, T.C.; Helden, P.D. Van; Warren, R.M. (2011). "Mycobacterium tuberculosis Beijing genotype: A template for success". Tuberculosis 91 (6): 510–523. doi:10.1016/j.tube.2011.07.005. PMID 21835699.
- ↑ Ford, Christopher B.; Shah, Rupal R.; Maeda, Midori Kato; Gagneux, Sebastien; Murray, Megan B.; Cohen, Ted; Johnston, James C.; Gardy, Jennifer et al. (July 2013). "Mycobacterium tuberculosis mutation rate estimates from different lineages predict substantial differences in the emergence of drug resistant tuberculosis". Nature Genetics 45 (7): 784–790. doi:10.1038/ng.2656. ISSN 1061-4036. PMID 23749189.
- ↑ Mestre, Olga; Luo, Tao; Vultos, Tiago Dos; Kremer, Kristin; Murray, Alan; Namouchi, Amine; Jackson, Céline; Rauzier, Jean et al. (2011-01-20). "Phylogeny of Mycobacterium tuberculosis Beijing Strains Constructed from Polymorphisms in Genes Involved in DNA Replication, Recombination and Repair". PLOS One 6 (1): e16020. doi:10.1371/journal.pone.0016020. ISSN 1932-6203. PMID 21283803. Bibcode: 2011PLoSO...616020M.
- ↑ Dalton, Tracy; Cegielski, Peter; Akksilp, Somsak; Asencios, Luis; Caoili, Janice Campos; Cho, Sang-Nae; Erokhin, Vladislav V; Ershova, Julia et al. (2012). "Prevalence of and risk factors for resistance to second-line drugs in people with multidrug-resistant tuberculosis in eight countries: A prospective cohort study". The Lancet 380 (9851): 1406–17. doi:10.1016/S0140-6736(12)60734-X. PMID 22938757.
- ↑ 23.0 23.1 WHO. "Multidrug-resistant tuberculosis (MDR-TB) 2013 Update". World Health Organization. http://www.who.int/tb/challenges/mdr/MDR_TB_FactSheet.pdf. Retrieved 14 June 2013.
- ↑ Velayati, A; Farnia P; Masjedi M (2013). "The totally drug resistant tuberculosis (TDR-TB)". International Journal of Clinical and Experimental Medicine 6 (4): 307–309. PMID 23641309.
- ↑ 25.0 25.1 Zumla, Alimuddin; Abubakar, Ibrahim; Raviglione, Mario; Hoelscher, Michael; Ditiu, Lucica; Mchugh, Timothy D.; Squire, S. Bertel; Cox, Helen et al. (2012-05-15). "Drug-Resistant Tuberculosis—Current Dilemmas, Unanswered Questions, Challenges, and Priority Needs". Journal of Infectious Diseases 205 (suppl 2): S228–S240. doi:10.1093/infdis/jir858. ISSN 0022-1899. PMID 22476720. http://jid.oxfordjournals.org/content/205/suppl_2/S228.
- ↑ Parida, S. K.; Axelsson-Robertson, R.; Rao, M. V.; Singh, N.; Master, I.; Lutckii, A.; Keshavjee, S.; Andersson, J. et al. (2015-04-01). "Totally drug-resistant tuberculosis and adjunct therapies". Journal of Internal Medicine 277 (4): 388–405. doi:10.1111/joim.12264. ISSN 1365-2796. PMID 24809736.
- ↑ Gao, Qian; Li, Xia (2010). "Transmission of MDR tuberculosis". Drug Discovery Today: Disease Mechanisms 7: e61–5. doi:10.1016/j.ddmec.2010.09.006.
- ↑ Lobue, Philip (2009). "Extensively drug-resistant tuberculosis". Current Opinion in Infectious Diseases 22 (2): 167–73. doi:10.1097/QCO.0b013e3283229fab. PMID 19283912. https://zenodo.org/record/1234905.
- ↑ Farmer 2005, p. 133.
- ↑ Shin, Sonya; Furin, Jennifer; Bayona, Jaime; Mate, Kedar; Kim, Jim Yong; Farmer, Paul (2004). "Community-based treatment of multidrug-resistant tuberculosis in Lima, Peru: 7 years of experience". Social Science & Medicine 59 (7): 1529–39. doi:10.1016/j.socscimed.2004.01.027. PMID 15246180.
- ↑ Koch, Erin (2011). "Local Microbiologies of Tuberculosis: Insights from the Republic of Georgia". Medical Anthropology 30 (1): 81–101. doi:10.1080/01459740.2010.531064. PMID 21218357.
- ↑ Koch, Erin (2006). "Beyond suspicion". American Ethnologist 33: 50–62. doi:10.1525/ae.2006.33.1.50.
- ↑ "Scientific Facts on Drug-resistant Tuberculosis". GreenFacts. 2008-12-18. http://www.greenfacts.org/en/tuberculosis/l-2/1-mdr-tb-xdr.htm. Retrieved 2009-03-26.
- ↑ 34.0 34.1 34.2 Farmer, Paul (2001). "The Major Infectious Diseases in the World — to Treat or Not to Treat?". New England Journal of Medicine 345 (3): 208–10. doi:10.1056/NEJM200107193450310. PMID 11463018.
- ↑ Baltussen, R.; Floyd, K; Dye, C (2005). "Cost effectiveness analysis of strategies for tuberculosis control in developing countries". BMJ 331 (7529): 1364. doi:10.1136/bmj.38645.660093.68. PMID 16282379.
- ↑ Mitnick, Carole; Bayona, Jaime; Palacios, Eda; Shin, Sonya; Furin, Jennifer; Alcántara, Felix; Sánchez, Epifanio; Sarria, Madeleny et al. (2003). "Community-Based Therapy for Multidrug-Resistant Tuberculosis in Lima, Peru". New England Journal of Medicine 348 (2): 119–28. doi:10.1056/NEJMoa022928. PMID 12519922. https://researchonline.lshtm.ac.uk/9891/1/nejmoa022928.pdf.
- ↑ Goble, Marian; Iseman, Michael D.; Madsen, Lorie A.; Waite, Dennis; Ackerson, Lynn; Horsburgh Jr, C. Robert (1993). "Treatment of 171 Patients with Pulmonary Tuberculosis Resistant to Isoniazid and Rifampin". New England Journal of Medicine 328 (8): 527–32. doi:10.1056/NEJM199302253280802. PMID 8426619.
- ↑ WHO Treatment Guidelines for Drug-Resistant Tuberculosis, 2016 Update. WHO Guidelines Approved by the Guidelines Review Committee. Geneva: World Health Organization. 2016. ISBN 9789241549639. https://www.ncbi.nlm.nih.gov/books/NBK390455/.
- ↑ WHO Treatment Guidelines for Drug-Resistant Tuberculosis, 2016 Update. WHO Guidelines Approved by the Guidelines Review Committee. Geneva: World Health Organization. 2016. ISBN 9789241549639. https://www.ncbi.nlm.nih.gov/books/NBK390455/.
- ↑ Ziganshina, L. E.; Squire, S. B. (2008-01-23). Ziganshina, Lilia E. ed. "Fluoroquinolones for treating tuberculosis". The Cochrane Database of Systematic Reviews (1): CD004795. doi:10.1002/14651858.CD004795.pub3. ISSN 1469-493X. PMID 18254061.
- ↑ Leimane, Vaira; Riekstina, Vija; Holtz, Timothy H; Zarovska, Evija; Skripconoka, Vija; Thorpe, Lorna E; Laserson, Kayla F; Wells, Charles D (2005). "Clinical outcome of individualised treatment of multidrug-resistant tuberculosis in Latvia: A retrospective cohort study". The Lancet 365 (9456): 318–26. doi:10.1016/S0140-6736(05)17786-1. PMID 15664227.
- ↑ Schon, T.; Elias, D.; Moges, F.; Melese, E.; Tessema, T.; Stendahl, O.; Britton, S.; Sundqvist, T. (2003). "Arginine as an adjuvant to chemotherapy improves clinical outcome in active tuberculosis". European Respiratory Journal 21 (3): 483–8. doi:10.1183/09031936.03.00090702. PMID 12662006.
- ↑ Rockett, Kirk A.; Brookes, Roger; Udalova, Irina; Vidal, Vincent; Hill, Adrian V. S.; Kwiatkowski, Dominic (1998). "1,25-Dihydroxyvitamin D3 Induces Nitric Oxide Synthase and Suppresses Growth of Mycobacterium tuberculosis in a Human Macrophage-Like Cell Line". Infection and Immunity 66 (11): 5314–21. doi:10.1128/iai.66.11.5314-5321.1998. PMID 9784538.
- ↑ Zaitzeva, S. I.; Matveeva, S. L.; Gerasimova, T. G.; Pashkov, Y. N.; Butov, D. A.; Pylypchuk, V. S.; Frolov, V. M.; Kutsyna, G. A. (2009). "Treatment of cavitary and infiltrating pulmonary tuberculosis with and without the immunomodulator Dzherelo". Clinical Microbiology and Infection 15 (12): 1154–62. doi:10.1111/j.1469-0691.2009.02760.x. PMID 19456829.
- ↑ Butov, Dmitry A; Pashkov, Yuri N; Stepanenko, Anna L; Choporova, Aleksandra I; Butova, Tanya S; Batdelger, Dendev; Jirathitikal, Vichai; Bourinbaiar, Aldar S et al. (2011). "Phase IIb randomized trial of adjunct immunotherapy in patients with first-diagnosed tuberculosis, relapsed and multi-drug-resistant (MDR) TB". Journal of Immune Based Therapies and Vaccines 9: 3. doi:10.1186/1476-8518-9-3. PMID 21244690.
- ↑ Chambers, H. F.; Turner, J.; Schecter, G. F.; Kawamura, M.; Hopewell, P. C. (2005). "Imipenem for Treatment of Tuberculosis in Mice and Humans". Antimicrobial Agents and Chemotherapy 49 (7): 2816–21. doi:10.1128/AAC.49.7.2816-2821.2005. PMID 15980354.
- ↑ Chambers, Henry F.; Kocagöz, Tanil; Sipit, Tugrul; Turner, Joan; Hopewell, Philip C. (1998). "Activity of Amoxicillin/Clavulanate in Patients with Tuberculosis". Clinical Infectious Diseases 26 (4): 874–7. doi:10.1086/513945. PMID 9564467.
- ↑ Peter r. Donald, Frederick a. Sirge; Sirgel, FA; Venter, A; Parkin, DP; Van De Wal, BW; Barendse, A; Smit, E; Carman, D et al. (2001). "Early Bactericidal Activity of Amoxicillin in Combination with Clavulanic Acid in Patients with Sputum Smear-positive Pulmonary Tuberculosis". Scandinavian Journal of Infectious Diseases 33 (6): 466–9. doi:10.1080/00365540152029954. PMID 11450868.
- ↑ Jagannath, C; Reddy, M V; Kailasam, S; O'Sullivan, J F; Gangadharam, P R (1995). "Chemotherapeutic activity of clofazimine and its analogues against Mycobacterium tuberculosis. In vitro, intracellular, and in vivo studies". American Journal of Respiratory and Critical Care Medicine 151 (4): 1083–6. doi:10.1164/ajrccm.151.4.7697235. PMID 7697235.
- ↑ Adams, Linda B.; Sinha, Indu; Franzblau, Scott G.; Krahenbuhl, James L. Krahenbuhl; Mehta, Reeta T. Mehta (1999). "Effective Treatment of Acute and Chronic Murine Tuberculosis with Liposome-Encapsulated Clofazimine". Antimicrobial Agents and Chemotherapy 43 (7): 1638–43. doi:10.1128/AAC.43.7.1638. PMID 10390215.
- ↑ Janulionis, E.; Sofer, C.; Song, H.-Y.; Wallis, R. S. (2004). "Lack of Activity of Orally Administered Clofazimine against Intracellular Mycobacterium tuberculosis in Whole-Blood Culture". Antimicrobial Agents and Chemotherapy 48 (8): 3133–5. doi:10.1128/AAC.48.8.3133-3135.2004. PMID 15273133.
- ↑ Shubin, H; Sherson, J; Pennes, E; Glaskin, A; Sokmensuer, A (1958). "Prochlorperazine (compazine) as an aid in the treatment of pulmonary tuberculosis". Antibiotic Medicine and Clinical Therapy 5 (5): 305–9. PMID 13521769.
- ↑ Wayne, L G; Sramek, H A (1994). "Metronidazole is bactericidal to dormant cells of Mycobacterium tuberculosis". Antimicrobial Agents and Chemotherapy 38 (9): 2054–8. doi:10.1128/AAC.38.9.2054. PMID 7811018.
- ↑ "FDA Press Release". U.S. Food and Drug Administration. 31 December 2012. https://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm333695.htm.
- ↑ Carroll, John (31 December 2012). "J&J wins accelerated OK for first new TB drug in 40 years". fiercebiotech.com. http://www.fiercebiotech.com/story/jj-wins-accelerated-ok-first-new-tb-drug-40-years/2012-12-31. Retrieved 3 January 2013.
- ↑ Stover, C. Kendall; Warrener, Paul; Vandevanter, Donald R.; Sherman, David R.; Arain, Taraq M.; Langhorne, Michael H.; Anderson, Scott W.; Towell, J. Andrew et al. (2000). "A small-molecule nitroimidazopyran drug candidate for the treatment of tuberculosis". Nature 405 (6789): 962–6. doi:10.1038/35016103. PMID 10879539. Bibcode: 2000Natur.405..962S.
- ↑ Chase, Marilyn (27 October 2004). "Novartis Sets Deal to Seek New Drugs for Fighting TB". TB Alliance. Archived from the original on 6 May 2007. https://web.archive.org/web/20070506175858/http://new.tballiance.org/newscenter/view-innews.php?id=520. Retrieved 3 January 2013.
- ↑ Farmer 1999, p. [page needed].
- ↑ Farmer 2005, p. 148.
- ↑ https://apps.who.int/iris/bitstream/handle/10665/329368/9789241565714-eng.pdf?ua=1
- ↑ https://apps.who.int/iris/bitstream/handle/10665/329368/9789241565714-eng.pdf?ua=1
- ↑ https://apps.who.int/iris/bitstream/handle/10665/329368/9789241565714-eng.pdf?ua=1
- ↑ Centers for Disease Control (CDC) (August 1991). "Nosocomial transmission of multidrug-resistant tuberculosis among HIV-infected persons—Florida and New York, 1988–1991". Morbidity and Mortality Weekly Report 40 (34): 585–91. PMID 1870559.
- ↑ Edlin, Brian R.; Tokars, Jerome I.; Grieco, Michael H.; Crawford, Jack T.; Williams, Julie; Sordillo, Emelia M.; Ong, Kenneth R.; Kilburn, James O. et al. (1992). "An Outbreak of Multidrug-Resistant Tuberculosis among Hospitalized Patients with the Acquired Immunodeficiency Syndrome". New England Journal of Medicine 326 (23): 1514–21. doi:10.1056/NEJM199206043262302. PMID 1304721.
- ↑ Pitchenik, Arthure; Burr, Janice; Laufer, Marla; Miller, Gary; Cacciatore, Robert; Bigler, Williamj.; Witte, Johnj.; Cleary, Timothy (1990). "Outbreaks of drug-resistant tuberculosis at AIDS centre". The Lancet 336 (8712): 440–1. doi:10.1016/0140-6736(90)91987-L. PMID 1974967.
- ↑ Centers for Disease Control (CDC) (March 1991). "Transmission of multidrug-resistant tuberculosis from an HIV-positive client in a residential substance-abuse treatment facility—Michigan". Morbidity and Mortality Weekly Report 40 (8): 129–31. PMID 1900098.
- ↑ Fischl, Margaret A.; Uttamchandani, RB; Daikos, GL; Poblete, RB; Moreno, JN; Reyes, RR; Boota, AM; Thompson, LM et al. (1992). "An Outbreak of Tuberculosis Caused by Multiple-Drug-resistant Tubercle Bacilli among Patients with HIV Infection". Annals of Internal Medicine 117 (3): 177–83. doi:10.7326/0003-4819-117-3-177. PMID 1616211.
- ↑ Centers for Disease Control (1990). "Outbreak of multidrug-resistant tuberculosis—Texas, California, and Pennsylvania". Morbidity and Mortality Weekly Report 39 (22): 369–72. PMID 2111434. https://www.cdc.gov/mmwr/preview/mmwrhtml/00001636.htm.
- ↑ Rochkind, David (2010-08-09). "Moldova: Fighting a Deadly Disease". Pulitzer Center on Crisis Reporting. http://pulitzercenter.org/projects/eastern-europe/moldova-fighting-deadly-disease. Retrieved 23 September 2012.
- ↑ McKay, Betsy (March 9–10, 2013). "Risk of Deadly TB Exposure Grows Along U.S.—Mexico Border". The Wall Street Journal: p. A1.
- ↑ Frieden, Thomas R.; Sterling, Timothy; Pablos-Mendez, Ariel; Kilburn, James O.; Cauthen, George M.; Dooley, Samuel W. (1993). "The Emergence of Drug-Resistant Tuberculosis in New York City". New England Journal of Medicine 328 (8): 521–6. doi:10.1056/NEJM199302253280801. PMID 8381207.
- ↑ Garrett 2000, p. 266ff.
- ↑ Garrett 1994, p. 524.
- ↑ Farmer 2005, p. 118.
- ↑ Ärzteblatt, Deutscher Ärzteverlag GmbH, Redaktion Deutsches (2016-12-27). "MDR-Tuberkulose unter Migranten aus Somalia" (in de). https://www.aerzteblatt.de/nachrichten/72186/MDR-Tuberkulose-unter-Migranten-aus-Somalia.
- ↑ Ärzteblatt, Deutscher Ärzteverlag GmbH, Redaktion Deutsches (2016-12-27). "MDR-Tuberkulose unter Migranten aus Somalia" (in de). https://www.aerzteblatt.de/nachrichten/72186/MDR-Tuberkulose-unter-Migranten-aus-Somalia.
- ↑ 77.0 77.1 77.2 77.3 77.4 Nachega J., Chaisson R. (2003). "Tuberculosis Drug Resistance: A Global Threat". Clinical Infectious Diseases 36 (1): S24–S30. doi:10.1086/344657. PMID 12516027.
- ↑ 78.0 78.1 78.2 78.3 78.4 Bobrik A.; Danishevski K.; Eroshina K.; McKee M. (2005). "Prison Health in Russia: The Larger Picture". Journal of Public Health Policy 26 (1): 30–59. doi:10.1057/palgrave.jphp.3200002. PMID 15906874.
- ↑ Baussano I.; Williams B.; Nunn P.; Beggiato M.; Fedeli U. (2010). "Tuberculosis Incidence in Prisons: A Systematic Review". PLOS Medicine 7 (12): e1000381. doi:10.1371/journal.pmed.1000381. PMID 21203587.
- ↑ 80.0 80.1 80.2 Shin S. S.; Pasechnikov A.; Gelmanova I.; Peremitin G.; Strelis A.; Andreev Y.; Golubchikova V.; Tonkel T. et al. (2006). "Treatment outcomes in an integrated civilian and prison MDR-TB treatment program in Russia". The International Journal of Tuberculosis and Lung Disease 10 (4): 402–407. PMID 16602404.
- ↑ 81.0 81.1 81.2 81.3 81.4 Ruddy M.; Balabanova Y.; Graham C.; Fedorin I.; Malomanova N.; Elisarova E.; Kuznetznov S.; Gusarova G. et al. (2005). "Rates of drug resistance and risk factor analysis in civilian and prison patients with tuberculosis in Samar Region, Russia". Thorax 60 (2): 130–135. doi:10.1136/thx.2004.026922. PMID 15681501.
- ↑ 82.0 82.1 Stern, V. (2001). Problems in Prisons Worldwide, with a Particular Focus on Russia. Annals of the New York Academy of Sciences, 953b, 113-119.
- ↑ 83.0 83.1 83.2 Fry R.; Khoshnood K.; Vdovichenko E.; Granskaya J.; Sazhin V.; Shpakovskaya L; Zhemkov V.; Zhemkova M. et al. (2005). "Barriers to completion of tuberculosis treatment among prisoners and former prisoners in St. Petersburg, Russia". The International Journal of Tuberculosis and Lung Disease 9 (9): 1027–1033. PMID 16158896.
- ↑ Gelmanova I.; Keshavjee S.; Golubchikova V.; Berezina V.; Strelis A.; Yanova G.; Atwood S.; Murray M. (2007). "Barriers to successful tuberculosis treatment in Tomsk, Russian Federation: non-adherence, default and the acquisition of multidrug resistance". Bulletin of the World Health Organization 85 (9): 703–11. doi:10.2471/BLT.06.038331. PMID 18026627.
- ↑ Kimerling M.E.; Kluge H.; Vezhnina N.; Iacovazzi T.; Demeulenaere T.; Portaels F.; Matthys F. (1999). "Inadequacy of the current WHO re-treatment regimen in a central Siberian prison: treatment failure and MDR-TB.". The International Journal of Tuberculosis and Lung Disease 3 (5): 451–453. PMID 10331736.
- ↑ Farmer P (1999). "Pathologies of power: rethinking health and human rights". American Journal of Public Health 89 (10): 1486–1496. doi:10.2105/ajph.89.10.1486. PMID 10511828.
- Notes
- Farmer, Paul (1999). Infections and inequalities : the modern plagues. Berkeley, California, United States: University of California Press. ISBN 978-0-520-22913-6. https://archive.org/details/infectionsinequa0000farm.
- Farmer, Paul (2005). Pathologies of Power: health, human rights, and the new war on the poor. Berkeley, California, United States: University of California Press. ISBN 978-0-520-93147-3.
- Garrett, Laurie (1994). The coming plague : newly emerging diseases in a world out of balance. New York, New York, United States: Farrar, Straus and Giroux. ISBN 978-0-374-12646-9. https://archive.org/details/comingplaguenew000garr.
- Garrett, Laurie (2000). Betrayal of trust: the collapse of global public health. New York, New York, United States: Hyperion Books. ISBN 978-0-7868-6522-2. https://archive.org/details/betrayaloftrustc00garr_0.
External links
| Classification |
|---|
- Video: Drug-Resistant TB in Russia 24 July 2007, Woodrow Wilson Center event featuring Salmaan Keshavjee and Murray Feshbach
- TB Drug Resistance Mutation Database
- MDR-TB : a story of Hope, Struggle & Triumph
- MDR-TB (DOTS Plus) protocol followed under RNTCP in India (PDF)
- "The Strange, Isolated Life of a Tuberculosis Patient in the 21st Century", Buzzfeed
