Medicine:Chromoblastomycosis
| Chromoblastomycosis | |
|---|---|
| Other names | Chromomycosis,[1] Cladosporiosis,[1] Fonseca's disease,[1] Pedroso's disease,[1] Phaeosporotrichosis,[1] or Verrucous dermatitis[1] |
| Specialty | Infectious disease, Dermatology |
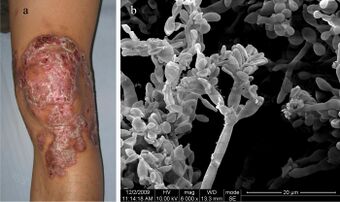
Chromoblastomycosis is a long-term fungal infection of the skin[2] and subcutaneous tissue (a chronic subcutaneous mycosis).[3]
It can be caused by many different types of fungi which become implanted under the skin, often by thorns or splinters.[4] Chromoblastomycosis spreads very slowly.[citation needed]
It is rarely fatal and usually has a good prognosis, but it can be very difficult to cure. The several treatment options include medication and surgery.[5]
The infection occurs most commonly in tropical or subtropical climates, often in rural areas.[6]
Symptoms and signs
The initial trauma causing the infection is often forgotten or not noticed. The infection builds at the site over a period of years, and a small red papule (skin elevation) appears. The lesion is usually not painful, with few, if any symptoms. Patients rarely seek medical care at this point.[citation needed]
Several complications may occur. Usually, the infection slowly spreads to the surrounding tissue while still remaining localized to the area around the original wound. However, sometimes the fungi may spread through the blood vessels or lymph vessels, producing metastatic lesions at distant sites. Another possibility is secondary infection with bacteria. This may lead to lymph stasis (obstruction of the lymph vessels) and elephantiasis. The nodules may become ulcerated, or multiple nodules may grow and coalesce, affecting a large area of a limb.[citation needed]
Cause
Chromoblastomycosis is believed to originate in minor trauma to the skin, usually from vegetative material such as thorns or splinters; this trauma implants fungi in the subcutaneous tissue. In many cases, the patient will not notice or remember the initial trauma, as symptoms often do not appear for years. The fungi most commonly observed to cause chromoblastomycosis are:
- Fonsecaea pedrosoi[8][9]
- Cladophialophora bantiana causes both cutaneous chromoblastomycosis and systemic phaeohyphomycosis
- Phialophora verrucosa[10]
- Cladophialophora carrionii
- Fonsecaea compacta[11]
Mechanism
Over months to years, an erythematous papule appears at the site of inoculation. Although the mycosis slowly spreads, it usually remains localized to the skin and subcutaneous tissue. Hematogenous and/or lymphatic spread may occur. Multiple nodules may appear on the same limb, sometimes coalescing into a large plaque. Secondary bacterial infection may occur, sometimes inducing lymphatic obstruction. The central portion of the lesion may heal, producing a scar, or it may ulcerate.[citation needed]
Diagnosis
The most informative test is to scrape the lesion and add potassium hydroxide (KOH), then examine under a microscope. (KOH scrapings are commonly used to examine fungal infections.) The pathognomonic finding is observing medlar bodies (also called muriform bodies or sclerotic cells). Scrapings from the lesion can also be cultured to identify the organism involved. Blood tests and imaging studies are not commonly used. On histology, chromoblastomycosis manifests as pigmented yeasts resembling "copper pennies". Special stains, such as periodic acid schiff and Gömöri methenamine silver, can be used to demonstrate the fungal organisms if needed.[citation needed]
Prevention
No preventive measure is known aside from avoiding the traumatic inoculation of fungi. At least one study found a correlation between walking barefoot in endemic areas and occurrence of chromoblastomycosis on the foot.[citation needed]
Treatment
Chromoblastomycosis is very difficult to cure. The primary treatments of choice are:[citation needed]
- Itraconazole, an antifungal azole, is given orally, with or without flucytosine.
- Alternatively, cryosurgery with liquid nitrogen has also been shown to be effective.
Other treatment options are the antifungal drug terbinafine,[12] another antifungal azole posaconazole, and heat therapy.
Antibiotics may be used to treat bacterial superinfections.[citation needed]
Amphotericin B has also been used.[13]
Photodynamic therapy is a newer type of therapy used to treat Chromblastomycosis.[14]
Prognosis
The prognosis for chromoblastomycosis is very good for small lesions. Severe cases are difficult to cure, although the prognosis is still quite good. The primary complications are ulceration, lymphedema, and secondary bacterial infection. A few cases of malignant transformation to squamous cell carcinoma have been reported. Chromoblastomycosis is very rarely fatal.[citation needed]
Epidemiology
Chromoblastomycosis occurs around the world, most commonly in rural areas in tropical or subtropical climates.[6]
It is most common in rural areas between approximately 30°N and 30°S latitude. Over two-thirds of patients are male, and usually between the ages of 30 and 50. A correlation with HLA-A29 suggests genetic factors may play a role, as well.[15]
Social and cultural
Chromoblastomycosis is considered a neglected tropical disease, affects mainly people living in poverty, and causes considerable morbidity, stigma and discrimination.[6]
See also
- List of cutaneous conditions
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 Rapini, Ronald P.; Bolognia, Jean L.; Jorizzo, Joseph L. (2007). Dermatology: 2-Volume Set. St. Louis: Mosby. ISBN 978-1-4160-2999-1.
- ↑ "chromoblastomycosis" at Dorland's Medical Dictionary
- ↑ "Chromoblastomycosis". Clin. Dermatol. 25 (2): 188–94. 2007. doi:10.1016/j.clindermatol.2006.05.007. PMID 17350498.
- ↑ "Chromoblastomycosis | Genetic and Rare Diseases Information Center (GARD) – an NCATS Program" (in en). https://rarediseases.info.nih.gov/diseases/1319/chromoblastomycosis.
- ↑ "Chromoblastomycosis | DermNet New Zealand" (in en). https://www.dermnetnz.org/topics/chromoblastomycosis/.
- ↑ 6.0 6.1 6.2 Santos, Daniel Wagner C. L.; de Azevedo, Conceição de Maria Pedrozo E. Silva; Vicente, Vania Aparecida; Queiroz-Telles, Flávio; Rodrigues, Anderson Messias; de Hoog, G. Sybren; Denning, David W.; Colombo, Arnaldo Lopes (August 2021). "The global burden of chromoblastomycosis". PLOS Neglected Tropical Diseases 15 (8): e0009611. doi:10.1371/journal.pntd.0009611. ISSN 1935-2735. PMID 34383752.
- ↑ Ran Yuping (2016). "Observation of Fungi, Bacteria, and Parasites in Clinical Skin Samples Using Scanning Electron Microscopy". in Janecek, Milos. Modern Electron Microscopy in Physical and Life Sciences. InTech. doi:10.5772/61850. ISBN 978-953-51-2252-4.
- ↑ "Chromoblastomycosis: clinical and mycologic experience of 51 cases". Mycoses 44 (1–2): 1–7. 2001. doi:10.1046/j.1439-0507.2001.00613.x. PMID 11398635.
- ↑ "Rapid identification of Fonsecaea by duplex polymerase chain reaction in isolates from patients with chromoblastomycosis". Diagn. Microbiol. Infect. Dis. 57 (3): 267–72. March 2007. doi:10.1016/j.diagmicrobio.2006.08.024. PMID 17338941.
- ↑ "A case of chromoblastomycosis with an unusual clinical manifestation caused by Phialophora verrucosa on an unexposed area: treatment with a combination of amphotericin B and 5-flucytosine". Br. J. Dermatol. 152 (3): 560–4. March 2005. doi:10.1111/j.1365-2133.2005.06424.x. PMID 15787829.
- ↑ Attapattu MC (1997). "Chromoblastomycosis--a clinical and mycological study of 71 cases from Sri Lanka". Mycopathologia 137 (3): 145–51. doi:10.1023/A:1006819530825. PMID 9368408.
- ↑ "Treatment of chromoblastomycosis with terbinafine: experience with four cases". J Dermatolog Treat 16 (1): 47–51. February 2005. doi:10.1080/09546630410024538. PMID 15897168. https://zenodo.org/record/894429.
- ↑ "Extensive chromoblastomycosis caused by Fonsecaea pedrosoi successfully treated with a combination of amphotericin B and itraconazole". Med. Mycol. 46 (2): 179–84. March 2008. doi:10.1080/13693780701721856. PMID 18324498.
- ↑ Queiroz-Telles, Flavio; de C L Santos, Daniel Wagner (2013-06-01). "Challenges in the Therapy of Chromoblastomycosis" (in en). Mycopathologia 175 (5): 477–488. doi:10.1007/s11046-013-9648-x. ISSN 1573-0832. PMID 23636730. https://doi.org/10.1007/s11046-013-9648-x.
- ↑ Queiroz-Telles, Flavio; de Hoog, Sybren; Santos, Daniel Wagner C. L.; Salgado, Claudio Guedes; Vicente, Vania Aparecida; Bonifaz, Alexandro; Roilides, Emmanuel; Xi, Liyan et al. (January 2017). "Chromoblastomycosis". Clinical Microbiology Reviews 30 (1): 233–276. doi:10.1128/CMR.00032-16. ISSN 1098-6618. PMID 27856522.
External links
| Classification | |
|---|---|
| External resources |
 |

