Medicine:Cryptococcosis
| Cryptococcosis | |
|---|---|
| Other names | Busse-Buschke disease, cryptococcic meningitis, cryptococcosis lung, cryptococcosis skin, European Blastomycosis, torular meningitis, torulosis[1] |
 | |
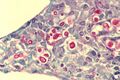
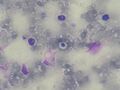
| Micrograph of cryptococcosis showing the characteristically thick capsule of cryptococcus. Field stain. | |
| Pronunciation | |
| Specialty | Infectious disease[4] |
| Symptoms |
|
| Causes | Cryptococcus neoformans,[7] Cryptococcus gattii[8] |
| Risk factors | HIV/AIDS,[9] Aviculture |
| Diagnostic method | Biopsy, culture[9] |
| Treatment | Antifungal medication |
| Medication | |
Cryptococcosis is a potentially fatal fungal infection of mainly the lungs, presenting as a pneumonia, and brain, where it appears as a meningitis.[4][9] Cough, difficulty breathing, chest pain and fever are seen when the lungs are infected.[5] When the brain is infected, symptoms include headache, fever, neck pain, nausea and vomiting, light sensitivity and confusion or changes in behavior.[5] It can also affect other parts of the body including skin, where it may appear as several fluid-filled nodules with dead tissue.[6]
It is caused by the fungi Cryptococcus neoformans or less commonly Cryptococcus gattii, and is acquired by breathing in the spores from the air.[4] These fungi are found around the world in soil, decaying wood, pigeon droppings, and in the hollows of some species of trees.[9][11] Whereas C. neoformans generally infects people with HIV/AIDS and those on immunosuppressant drugs and does not usually affect fit and healthy people, C. gattii (found in some parts of Canada and the US) does.[9][11] Once breathed in, the dried yeast cells colonize the lungs, where they are either cleared by immune cells, lie dormant, or cause infection and spread.[12]
Diagnosis is by isolating Cryptococcus from a sample of affected tissue or direct observation of the fungus by using staining of body fluids.[9] It can be cultured from a cerebrospinal fluid, sputum, and skin biopsy.[9] Treatment is with fluconazole or amphotericin B.[9][10]
Data from 2009 estimated that of the almost one million cases of cryptococcal meningitis that occurred worldwide annually, 700,000 occurred in sub-Saharan Africa and 600,000 per year died.[13] Cryptococcosis was rare before the 1970s which saw an increase in at-risk groups such as people with organ transplant or on immunosuppressant medications.[9] The number of cases escalated in the mid-1980s with over 80% occurring in people with HIV/AIDS.[9] Pigeon breeders (or otherwise people who spend significant time with pigeons) are known to have a high incidence of cryptococcal infections including PCC due to Cryptococcus' association with pigeon droppings.[14][15]
Classification
Cryptococcus is generally classified according to how it is acquired and its site.[16] It typically begins in the lungs before spreading to other parts of the body, particularly the brain and nervous system.[1] The skin type is less common.[1]
Signs and symptoms
Cough, shortness of breath, chest pain and fever are seen when the lungs are infected, appearing like a pneumonia.[5] There may also be feeling of tiredness.[4] When the brain is infected, symptoms include headache, fever, neck pain, nausea and vomiting, light sensitivity, confusion or changes in behaviour.[5] It can also affect other parts of the body including skin, eyes, bones and prostate.[9] In the skin, it may appear as several fluid-filled nodules with dead tissue.[6] Depending on the site of infection, other features may include loss of vision, blurred vision, inability to move an eye and memory loss.[9]
Symptom onset is often sudden when lungs are infected and gradual over several weeks when the central nervous system is affected.[9]
Cause
Cryptococcosis is a common opportunistic infection for AIDS, and is particularly common among people living with AIDS in Africa. Other conditions that pose an increased risk include certain malignancies (such as lymphoma), liver cirrhosis, organ transplants, and long-term corticosteroid therapy.[17]
Distribution is worldwide in soil.[18] The prevalence of cryptococcosis has been increasing over the past 50 years for many reasons, including the increase in incidence of AIDS and the expanded use of immunosuppressive drugs.[19]
In humans, C. neoformans chiefly infects the skin, lungs, and central nervous system (causing meningitis).[19] Less commonly it may affect other organs such as the eye or prostate.[19]
Primary cutaneous cryptococcosis
Primary cutaneous cryptococcosis (PCC) is a distinct clinical diagnosis separate from the secondary cutaneous cryptococcosis that is spread from systematic infection. Males are more likely to develop the infection and a 2020 study showed that the sex bias may be due to a growth hormone, produced by C. neoformans called gibberellic acid (GA) that is upregulated by testosterone.[20] The upper limbs account for a majority of infections. Isolates found in PCC include Cryptococcus neoformans (most common), Cryptococcus gattii, and Cryptococcus laurentii. Prognosis for PCC is generally good outside of disseminated infection.[21]
Morphologic description of the lesions show umbilicated papules, nodules, and violaceous plaques that can mimic other cutaneous diseases like molluscum contagiosum and Kaposi's sarcoma. These lesions may be present months before other signs of system infection in patients with AIDS.[22]
Pulmonary cryptococcosis
Cryptococcus (both C. neoformans and C. gattii) plays a common role in pulmonary invasive mycosis seen in adults with HIV and other immunocompromised conditions.[23] It also affects healthy adults at a much lower frequency and severity as healthy hosts may have no or mild symptoms.[24] Immune-competent hosts may not seek or require treatment, but careful observation may be important.[25] Cryptococcal pneumonia has a potential to disseminate to the central nervous system (CNS) especially in immunocompromised individuals.[26]
Pulmonary cryptococcosis has a worldwide distribution and is commonly underdiagnosed due to limitations in diagnostic capabilities. Since pulmonary nodules are its most common radiological feature, it can clinically and radiologically mimic lung cancer, TB, and other pulmonary mycoses. The sensitivity of cultures and the Cryptococcal (CrAg) antigen with lateral flow device on serum are rarely positive in the absence of disseminated disease.[23] Moreover, pulmonary cryptococcosis worsen the prognosis of cryptococcal meningitis.[23]
Cryptococcal meningitis
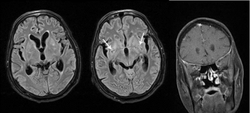
Cryptococcal meningitis (infection of the meninges, the tissue covering the brain) is believed to result from dissemination of the fungus from either an observed or unappreciated pulmonary infection. Often there is also silent dissemination throughout the brain when meningitis is present. People with defects in their cell-mediated immunity, for example, people with AIDS, are especially susceptible to disseminated cryptococcosis. Cryptococcosis is often fatal, even if treated. It is estimated that the three-month case-fatality rate is 9% in high-income regions, 55% in low/middle-income regions, and 70% in sub-Saharan Africa. As of 2009 there were globally approximately 958,000 annual cases and 625,000 deaths within three months after infection.[27]
Although C. neoformans infection most commonly occurs as an opportunistic infection in immunocompromised people (such as those living with AIDS), C. gattii often infects immunocompetent people as well.[28]
Cryptococcus (both C. neoformans and C. gattii) is the dominant and leading[29] etiologic agent of meningitis in adults with HIV and is considered an "emerging" disease in healthy adults.[30] Though the rate of infection is clearly higher with immunocompromised individuals, some studies suggest a higher mortality rate in patients with non-HIV cryptococcal meningitis secondary to the role of T-cell mediated reaction and injury.[31] CD4+ T cells have proven roles in the defense against Cryptococcus, but it can also contribute to clinical deterioration due its inflammatory response.[32]
Diagnosis
Dependent on the infectious syndrome, symptoms include fever, fatigue, dry cough, headache, blurred vision, and confusion.[33] Symptom onset is often subacute, progressively worsened over several weeks. The two most common presentations are meningitis (an infection in and around the brain) and pulmonary (lung) infection.[19]
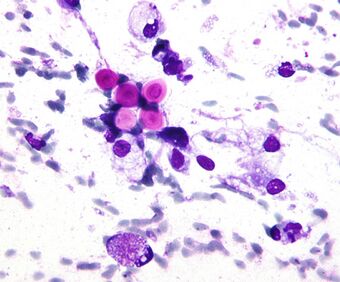
Any person who is found to have cryptococcosis at a site outside of the central nervous system (e.g., pulmonary cryptococcosis), a lumbar puncture is indicated to evaluate the cerebrospinal fluid (CSF) for evidence of cryptococcal meningitis, even if they do not have signs or symptoms of CNS disease. Detection of cryptococcal antigen (capsular material) by culture of CSF, sputum and urine provides definitive diagnosis.[34] Blood cultures may be positive in heavy infections. India ink of the CSF is a traditional microscopic method of diagnosis,[35] although the sensitivity is poor in early infection, and may miss 15–20% of patients with culture-positive cryptococcal meningitis.[36] Unusual morphological forms are rarely seen.[37] Cryptococcal antigen from cerebrospinal fluid is the best test for diagnosis of cryptococcal meningitis in terms of sensitivity.[38] Apart from conventional methods of detection like direct microscopy and culture, rapid diagnostic methods to detect cryptococcal antigen by latex agglutination test, lateral flow immunochromatographic assay (LFA), or enzyme immunoassay (EIA). A new cryptococcal antigen LFA was FDA approved in July 2011.[36][39] Polymerase chain reaction (PCR) has been used on tissue specimens.
Cryptococcosis can rarely occur in the non-immunosuppressed people, particularly with Cryptococcus gattii.[citation needed]
Prevention
Cryptococcosis is a very subacute infection with a prolonged subclinical phase lasting weeks to months in persons with HIV/AIDS before the onset of symptomatic meningitis. In Sub-Saharan Africa, the prevalence rates of detectable cryptococcal antigen in peripheral blood is often 4–12% in persons with CD4 counts lower than 100 cells/mcL.[40][41] Cryptococcal antigen screen and preemptive treatment with fluconazole is cost saving to the healthcare system by avoiding cryptococcal meningitis.[42] The World Health Organization recommends cryptococcal antigen screening in HIV-infected persons entering care with CD4<100 cells/μL.[43] This undetected subclinical cryptococcal (if not preemptively treated with anti-fungal therapy) will often go on to develop cryptococcal meningitis, despite receiving HIV therapy.[41][44] Cryptococcosis accounts for 20–25% of the mortality after initiating HIV therapy in Africa. What is effective preemptive treatment is unknown, with the current recommendations on dose and duration based on expert opinion. Screening in the United States is controversial, with official guidelines not recommending screening, despite cost-effectiveness and a 3% U.S. cryptococcal antigen prevalence in CD4<100 cells/μL.[45][46]
Antifungal prophylaxis such as fluconazole and itraconazole reduces the risk of contracting cryptococcosis in those with low CD4 cell count and high risk of developing such disease in a setting of cryptococcal antigen screening tests are not available.[47]
Treatment
Treatment options in persons without HIV-infection have not been well studied. Intravenous Amphotericin B combined with flucytosine by mouth is recommended for initial treatment (induction therapy).[48]
People living with AIDS often have a greater burden of disease and higher mortality (30–70% at 10-weeks), but recommended therapy is with amphotericin B and flucytosine. Where flucytosine is not available (many low and middle income countries), fluconazole should be used with amphotericin.[43] Amphotericin-based induction therapy has much greater microbiologic activity than fluconazole monotherapy with 30% better survival at 10 weeks.[34][49] Based on a systematic review of existing data, the most cost-effective induction treatment in resource-limited settings appears to be one week of amphotericin B coupled with high-dose fluconazole.[49] After initial induction treatment as above, typical consolidation therapy is with oral fluconazole for at least 8 weeks used with secondary prophylaxis with fluconazole thereafter.[43]
The decision on when to start treatment for HIV appears to be very different than other opportunistic infections. A large multi-site trial supports deferring ART for 4–6 weeks was overall preferable with 15% better 1-year survival than earlier ART initiation at 1–2 weeks after diagnosis.[50] A 2018 Cochrane review also supports the delayed starting of treatment until cryptococcosis starts improving with antifungal treatment.[51]
IRIS
The immune reconstitution inflammatory syndrome (IRIS) has been described in those with normal immune function with meningitis caused by C. gattii and C. grubii. The increasing inflammation can cause brain injury or be fatal.[52][53][54]
Epidemiology
Cryptococcosis is usually associated with immunosuppressed patients, such as AIDs, corticosteroid use, diabetes, and organ transplant patients.[55] Cryptococcus is found in two species, Cryptococcus neoformans and Cryptococcus gattii.[56] C. gattii was previously thought to only be found in tropical climates and in immunocompetent persons, but recent findings of C. gattii in regions such as Canada and Western regions of North America have challenged this initial presumption of the geographic patterns.[57]
Data from 2009 estimated that of the almost one million cases of cryptococcal meningitis that occurred worldwide annually, 700,000 occurred in sub-Saharan Africa and 600,000 per year died.[13] In 2014, amongst people who had low CD4+ cell count, the annual incidence rate was estimated to be 278,000 cases. Of those, 223,100 resulted in cryptococcal meningitis.[58] About 73% of cryptococcal meningitis cases occurred in Sub-Saharan Africa. More than 180,000 fatalities are attributed to cryptococcal meningitis, 135,000 of which occur in sub-Saharan Africa. Case fatality of cryptococcal meningitis varies widely depending on what country the infection occurs. In low-income countries the case fatality from cryptococcal meningitis is 70%. This differs from middle income countries where the case fatality rate is 40%. Lastly, in wealthy countries the case fatality is 20%.[58] Cryptococcosis is the second most common cause of death for patients with AIDs (about 15%), behind tuberculosis.[59] In sub-Saharan Africa approximately 1/3 of HIV patients will develop cryptococcosis.[60]
In the United States
In the United States there are between 2–7 cases of cryptococcosis per 1,000 per year. Since 1990 the incidence of AIDs associated cryptococcosis fell by 90% due to the proliferation of antiretroviral therapy.[61][62] The estimated prevalence of cryptococcosis cases amongst HIV patients in the U.S. is 2.8%.[63] In immunocompetent patients cryptococcus typically presents itself as Cryptococcus gattii.[62] Despite its rarity cryptococcus has been more commonly seen, with upwards of 20% of cases in immunocompetent people.[64] Over 50% of cryptococcosis infections in North America are caused by C. gattii. Though C. gattii was originally thought to be restricted to subtropical and tropical regions it has become more prevalent worldwide.[65] C. gattii has been found in over 90 people in the United States, most of these cases originating in Washington or Oregon.[66]
In sub-Saharan Africa
Sub-Saharan Africa is the main hub for HIV/AIDS worldwide. HIV/AIDS accounts for about 0.5% of the world's population.[67] Remarkably, sub-Saharan Africa holds 71% of HIV/AIDs cases.[68] Cryptococcal meningitis is a primary contributor to mortality among individuals with HIV/AIDS in sub-Saharan Africa.[69] Approximately 160,000 cases of cryptococcal meningitis are reported in West Africa, resulting in 130,000 deaths in sub-Saharan Africa.[70] Uganda is reported to have the highest occurrence of cryptococcus meningitis.[71] Reflecting that, Ethiopia has the least occurrence.[71] Presently, treatment options involve either a 7 or 14-day regimen of amphotericin-B, coupled with oral antifungal tablets or oral fluconazole. It is important to note, amphotericin-B is not considered a treatment, as it showed not a significant reduction in the mortality rate.[72]
Other animals
Cryptococcosis is also seen in cats and occasionally dogs. It is the most common deep fungal disease in cats, usually leading to chronic infection of the nose and sinuses, and skin ulcers. Cats may develop a bump over the bridge of the nose from local tissue inflammation. It can be associated with FeLV infection in cats. Cryptococcosis is most common in dogs and cats but cattle, sheep, goats, horses, wild animals, and birds can also be infected. Soil, fowl manure, and pigeon droppings are among the sources of infection.[73][74]
References
- ↑ 1.0 1.1 1.2 "Cryptococcosis". https://rarediseases.org/rare-diseases/cryptococcosis/.
- ↑ "Cryptococcosis". Cryptococcosis. Oxford University Press. http://www.lexico.com/definition/Cryptococcosis.
- ↑ "Cryptococcosis". Merriam-Webster Dictionary. https://www.merriam-webster.com/dictionary/Cryptococcosis. Retrieved 2016-01-21.
- ↑ 4.0 4.1 4.2 4.3 "ICD-11 - ICD-11 for Mortality and Morbidity Statistics". https://icd.who.int/browse11/l-m/en#/http%3a%2f%2fid.who.int%2ficd%2fentity%2f390527954.
- ↑ 5.0 5.1 5.2 5.3 5.4 5.5 "Symptoms of C. neoformans Infection | Fungal Diseases | CDC" (in en-us). 14 January 2021. https://www.cdc.gov/fungal/diseases/cryptococcosis-neoformans/symptoms.html.
- ↑ 6.0 6.1 6.2 Johnstone, Ronald B. (2017). "25. Mycoses and Algal infections". Weedon's Skin Pathology Essentials (2nd ed.). Elsevier. p. 446. ISBN 978-0-7020-6830-0. https://books.google.com/books?id=NTE_DAAAQBAJ.
- ↑ "C. neoformans Infection | Fungal Diseases | CDC" (in en-us). 29 December 2020. https://www.cdc.gov/fungal/diseases/cryptococcosis-neoformans/index.html.
- ↑ "Where C. gattii Infection Comes From | Fungal Disease | CDC" (in en-us). 29 January 2021. https://www.cdc.gov/fungal/diseases/cryptococcosis-gattii/causes.html.
- ↑ 9.00 9.01 9.02 9.03 9.04 9.05 9.06 9.07 9.08 9.09 9.10 9.11 9.12 9.13 Maziarz, Eileen K.; Perfect, John R. (2016). "Cryptococcosis". Infectious Disease Clinics of North America 30 (1): 179–206. doi:10.1016/j.idc.2015.10.006. ISSN 0891-5520. PMID 26897067.
- ↑ 10.0 10.1 "Treatment for C. neoformans Infection | Fungal Diseases | CDC" (in en-us). 14 January 2021. https://www.cdc.gov/fungal/diseases/cryptococcosis-neoformans/treatment.html.
- ↑ 11.0 11.1 "Where C. neoformans Infection Comes From | Fungal Diseases | CDC" (in en-us). 2 February 2021. https://www.cdc.gov/fungal/diseases/cryptococcosis-neoformans/causes.html.
- ↑ Sabiiti, Wilber; May, Robin C. (November 2012). "Mechanisms of infection by the human fungal pathogen Cryptococcus neoformans". Future Microbiology 7 (11): 1297–1313. doi:10.2217/fmb.12.102. ISSN 1746-0921. PMID 23075448. https://pubmed.ncbi.nlm.nih.gov/23075448/.
- ↑ 13.0 13.1 Vallabhaneni, Snigdha; Mody, Rajal K.; Walker, Tiffany; Chiller, Tom (2016). "1. The global burden of fungal disease". in Sobel, Jack; Ostrosky-Zeichner, Luis (in en). Fungal Infections, An Issue of Infectious Disease Clinics of North America. Philadelphia: Elsevier. pp. 3–4. ISBN 978-0-323-41649-8. https://books.google.com/books?id=uwndCwAAQBAJ&pg=PA3.
- ↑ Walter JE, Atchison RW. Epidemiological and immunological studies of Cryptococcus neoformans. J Bacteriol. 1966 Jul;92(1):82-7. doi: 10.1128/JB.92.1.82-87.1966. PMID 5328755; PMCID: PMC276199.
- ↑ Beatson M, Harwood M, Reese V, Robinson-Bostom L. Primary cutaneous cryptococcosis in an elderly pigeon breeder. JAAD Case Rep. 2019 May 7;5(5):433-435. doi: 10.1016/j.jdcr.2019.03.006. PMID 31192987; PMCID: PMC6510938.
- ↑ Alanazi, Abdulaziz H.; Adil, Mir S.; Lin, Xiaorong; Chastain, Daniel B.; Henao-Martínez, Andrés F.; Franco-Paredes, Carlos; Somanath, Payaningal R. (July 2022). "Elevated Intracranial Pressure in Cryptococcal Meningoencephalitis: Examining Old, New, and Promising Drug Therapies". Pathogens 11 (7): 783. doi:10.3390/pathogens11070783. PMID 35890028.
- ↑ "Pulmonary cryptococcosis: A review of pathobiology and clinical aspects". Medical Mycology 57 (2): 133–150. February 2019. doi:10.1093/mmy/myy086. PMID 30329097. https://academic.oup.com/mmy/article/57/2/133/5133472. Retrieved 2022-08-18.
- ↑ "Meningitis: cryptococcal: Overview". Medical Reference: Encyclopedia. University of Maryland Medical Center. September 2010. http://www.umm.edu/ency/article/000642.htm. Retrieved 2011-04-26.
- ↑ 19.0 19.1 19.2 19.3 "Cryptococcosis". Infectious Disease Clinics 35 (2): 493–514. June 2021. doi:10.1016/j.idc.2021.03.012. PMID 34016288.
- ↑ Tucker JS, Guess TE, McClelland EE. The Role of Testosterone and Gibberellic Acid in the Melanization of Cryptococcus neoformans. Front. Microbiol. 2020 Aug 13;11:1921. doi: 10.3389/fmicb.2020.01921. PMID 32922377; PMCID: PMC7456850.
- ↑ Du L, Yang Y, Gu J, Chen J, Liao W, Zhu Y. Systemic Review of Published Reports on Primary Cutaneous Cryptococcosis in Immunocompetent Patients. Mycopathologia. 2015 Aug;180(1-2):19-25. doi: 10.1007/s11046-015-9880-7. Epub 2015 Mar 4. PMID 25736173.
- ↑ Murakawa GJ, Kerschmann R, Berger T. Cutaneous Cryptococcus infection and AIDS. Report of 12 cases and review of the literature. Arch Dermatol. 1996 May;132(5):545-8. PMID 8624151.
- ↑ 23.0 23.1 23.2 Setianingrum F, Rautemaa-Richardson R, Denning DW. Pulmonary cryptococcosis: A review of pathobiology and clinical aspects. Med Mycol. 2019 Feb 1;57(2):133-150. doi: 10.1093/mmy/myy086. PMID 30329097.
- ↑ Choi KH, Park SJ, Min KH, Kim SR, Lee MH, Chung CR, Han HJ, Lee YC. Treatment of asymptomatic pulmonary cryptococcosis in immunocompetent hosts with oral fluconazole. Scand J Infect Dis. 2011 May;43(5):380-5. doi: 10.3109/00365548.2011.552521. Epub 2011 Jan 28. PMID 21271944.
- ↑ Saag MS, Graybill RJ, Larsen RA, Pappas PG, Perfect JR, Powderly WG, Sobel JD, Dismukes WE. Practice guidelines for the management of cryptococcal disease. Infectious Diseases Society of America. Clin Infect Dis. 2000 Apr;30(4):710-8. doi: 10.1086/313757. Epub 2000 Apr 20. PMID 10770733.
- ↑ Brizendine KD, Baddley JW, Pappas PG. Pulmonary cryptococcosis. Semin Respir Crit Care Med. 2011 Dec;32(6):727-34. doi: 10.1055/s-0031-1295720. Epub 2011 Dec 13. PMID 22167400.
- ↑ "Estimation of the current global burden of cryptococcal meningitis among persons living with HIV/AIDS". AIDS 23 (4): 525–30. 2009-02-20. doi:10.1097/QAD.0b013e328322ffac. PMID 19182676.
- ↑ "Genome Variation in Cryptococcus gattii, an Emerging Pathogen of Immunocompetent Hosts". mBio (American Society for Microbiology) 2 (1): e00342-10. 2011-02-08. doi:10.1128/mBio.00342-10. PMID 21304167.
- ↑ Traoré FA, Cissoko Y, Tounkara TM, Sako FB, Mouelle AD, Kpami DO, Traoré M, Doumbouya M. Étiologies des méningites lymphocytaires chez les personnes vivant avec le VIH suivies dans le service des maladies infectieuses de Conakry [Causes of lymphocytic meningitis in people with HIV admitted to the Infectious Disease department of Conakry]. Med Sante Trop. 2015 Jan-Mar;25(1):52-5. French. doi: 10.1684/mst.2014.0391. PMID 25466555.
- ↑ Pasquier E, Kunda J, De Beaudrap P, Loyse A, Temfack E, Molloy SF, Harrison TS, Lortholary O. Long-term Mortality and Disability in Cryptococcal Meningitis: A Systematic Literature Review. Clin Infect Dis. 2018 Mar 19;66(7):1122-1132. doi: 10.1093/cid/cix870. PMID 29028957.
- ↑ Anjum S, Williamson PR. Clinical Aspects of Immune Damage in Cryptococcosis. Curr Fungal Infect Rep. 2019 Sep;13(3):99-108. doi: 10.1007/s12281-019-00345-7. Epub 2019 Jul 22. PMID 33101578; PMCID: PMC7580832.
- ↑ Neal LM, Xing E, Xu J, Kolbe JL, Osterholzer JJ, Segal BM, Williamson PR, Olszewski MA. CD4+ T Cells Orchestrate Lethal Immune Pathology despite Fungal Clearance during Cryptococcus neoformans Meningoencephalitis. mBio. 2017 Nov 21;8(6):e01415-17. doi: 10.1128/mBio.01415-17. PMID 29162707; PMCID: PMC5698549.
- ↑ "Opportunistic Fungal Infections, Part 3: Cryptococcosis, Histoplasmosis, Coccidioidomycosis, and Emerging Mould Infections". Infections in Medicine. November 18, 2008. http://www.consultantlive.com/infection/article/1145625/1404367?pageNumber=1.
- ↑ 34.0 34.1 Rhein, J; Boulware DR (2012). "Prognosis and management of cryptococcal meningitis in patients with HIV infection". Neurobehavioral HIV Medicine 4: 45. doi:10.2147/NBHIV.S24748.
- ↑ Zerpa, R; Huicho, L; Guillén, A (September 1996). "Modified India ink preparation for Cryptococcus neoformans in cerebrospinal fluid specimens.". Journal of Clinical Microbiology 34 (9): 2290–1. doi:10.1128/JCM.34.9.2290-2291.1996. PMID 8862601.
- ↑ 36.0 36.1 Boulware, DR; Rolfes, MA; Rajasingham, R; von Hohenberg, M; Qin, Z; Taseera, K; Schutz, C; Kwizera, R et al. (Jan 2014). "Multisite validation of cryptococcal antigen lateral flow assay and quantification by laser thermal contrast.". Emerging Infectious Diseases 20 (1): 45–53. doi:10.3201/eid2001.130906. PMID 24378231.
- ↑ Shashikala; Kanungo, R; Srinivasan, S; Mathew, R; Kannan, M (Jul–Sep 2004). "Unusual morphological forms of Cryptococcus neoformans in cerebrospinal fluid". Indian Journal of Medical Microbiology 22 (3): 188–90. doi:10.1016/S0255-0857(21)02835-8. PMID 17642731.
- ↑ Antinori, Spinello; Radice, Anna; Galimberti, Laura; Magni, Carlo; Fasan, Marco; Parravicini, Carlo (November 2005). "The role of cryptococcal antigen assay in diagnosis and monitoring of cryptococcal meningitis.". Journal of Clinical Microbiology 43 (11): 5828–9. doi:10.1128/JCM.43.11.5828-5829.2005. PMID 16272534. PMC 1287839. https://air.unimi.it/bitstream/2434/6221/2/Antinori.pdf.
- ↑ "Evaluation of a novelpoint-of-care cryptococcal antigen test on serum, plasma, and urine frompatients with HIV-associated cryptococcal meningitis". Clin Infect Dis 53 (10): 1019–23. 2011. doi:10.1093/cid/cir613. PMID 21940419.
- ↑ "FIGURE 1. Prevalence of asymptomatic antigenemia with corresponding cost per life saved based on LFA cost of $2.50 per test.". http://journals.lww.com/jaids/_layouts/oaks.journals/ImageView.aspx?k=jaids:2012:04150:00011&i=FF1&year=2012&issue=04150&article=00011.
- ↑ 41.0 41.1 "Cost-effectiveness of serum cryptococcal antigen screening to prevent deaths among HIV-infected persons with a CD4+ cell count < or = 100 cells/microL who start HIV therapy in resource-limited settings". Clin. Infect. Dis. 51 (4): 448–55. August 2010. doi:10.1086/655143. PMID 20597693.
- ↑ Rajasingham, R; Meya, DB; Boulware, DR (Apr 15, 2012). "Integrating cryptococcal antigen screening and pre-emptive treatment into routine HIV care". Journal of Acquired Immune Deficiency Syndromes 59 (5): e85–91. doi:10.1097/QAI.0b013e31824c837e. PMID 22410867.
- ↑ 43.0 43.1 43.2 World Health Organization. "Rapid advice: Diagnosis, prevention and management of cryptococcal disease in HIV-infected adults, adolescents, and children". https://www.who.int/hiv/pub/cryptococcal_disease2011/en/.
- ↑ Jarvis, JN; Harrison, TS; Govender, N; Lawn, SD; Longley, N; Bicanic, T; Maartens, G; Venter, F et al. (2011). "Routine cryptococcal antigen screening for HIV-infected patients with low CD4+ T-lymphocyte counts—time to implement in South Africa?". South African Medical Journal 101 (4): 232–4. doi:10.7196/samj.4752. PMID 21786721. https://open.uct.ac.za/bitstream/11427/24418/1/Jarvis_Article_2011.pdf.
- ↑ Rajasingham, R; Boulware, DR (Dec 2012). "Reconsidering cryptococcal antigen screening in the U.S. among persons with CD4 <100 cells/mcL.". Clinical Infectious Diseases 55 (12): 1742–4. doi:10.1093/cid/cis725. PMID 22918997.
- ↑ "Prevalence and correlates of cryptococcal antigen positivity among AIDS patients—United States, 1986–2012". MMWR Morb. Mortal. Wkly. Rep. 63 (27): 585–7. July 2014. PMID 25006824.
- ↑ Awotiwon, Ajibola A; Johnson, Samuel; Rutherford, George W; Meintjes, Graeme; Eshun-Wilson, Ingrid (2018-08-29). Cochrane Infectious Diseases Group. ed. "Primary antifungal prophylaxis for cryptococcal disease in HIV-positive people" (in en). Cochrane Database of Systematic Reviews 2018 (8): CD004773. doi:10.1002/14651858.CD004773.pub3. PMID 30156270.
- ↑ "Practice Guidelines for the Management of Cryptococcal Disease". Infectious Disease Society of America. 2010. http://www.idsociety.org/Organism/#CryptococcalDisease.
- ↑ 49.0 49.1 Rajasingham, Radha; Rolfes, M.A.; Birkenkamp, K.E.; Meya, D.B.; Boulware, D.R. (2012). Farrar, Jeremy. ed. "Cryptococcal Meningitis Treatment Strategies in Resource-Limited Settings: A Cost-Effectiveness Analysis". PLOS Medicine 9 (9): e1001316. doi:10.1371/journal.pmed.1001316. PMID 23055838.
- ↑ Boulware, DR; Meya, DB; Muzoora, Conrad; Rolfes, MA; Huppler Hullsiek, K; Musubire, Abdu; Taseera, Kabanda; Nabeta, HW et al. (26 June 2014). "Timing of Antiretroviral Therapy after Diagnosis of Cryptococcal Meningitis". New England Journal of Medicine 370 (26): 2487–2498. doi:10.1056/NEJMoa1312884. PMID 24963568.
- ↑ Eshun-Wilson, Ingrid; Okwen, Mbah P.; Richardson, Marty; Bicanic, Tihana (24 July 2018). "Early versus delayed antiretroviral treatment in HIV-positive people with cryptococcal meningitis". The Cochrane Database of Systematic Reviews 2018 (7): CD009012. doi:10.1002/14651858.CD009012.pub3. ISSN 1469-493X. PMID 30039850.
- ↑ "Steroid responsive late deterioration in Cryptococcus neoformans variety gattii meningitis". Neurology 63 (4): 713–4. August 2004. doi:10.1212/01.WNL.0000134677.29120.62. PMID 15326249.
- ↑ "Paradoxical inflammatory reaction during treatment of Cryptococcus neoformans var. gattii meningitis in an HIV-seronegative woman". Clin. Infect. Dis. 39 (8): e78–82. October 2004. doi:10.1086/424746. PMID 15486830.
- ↑ "The poor prognosis of central nervous system cryptococcosis among nonimmunosuppressed patients: a call for better disease recognition and evaluation of adjuncts to antifungal therapy". Clin. Infect. Dis. 42 (10): 1443–7. May 2006. doi:10.1086/503570. PMID 16619158.
- ↑ Mada, Pradeep Kumar; Jamil, Radia T.; Alam, Mohammed U. (2023), "Cryptococcus", StatPearls (Treasure Island (FL): StatPearls Publishing), PMID 28613714, http://www.ncbi.nlm.nih.gov/books/NBK431060/, retrieved 2023-11-15
- ↑ "Error: no
|title=specified when using {{Cite web}}". https://academic.oup.com/femsyr/article/10/6/769/539826. - ↑ Harris, Julie; Lockhart, Shawn; Chiller, Tom (February 2012). "Cryptococcus gattii : where do we go from here?" (in en). Medical Mycology 50 (2): 113–129. doi:10.3109/13693786.2011.607854. ISSN 1369-3786. PMID 21939343. https://academic.oup.com/mmy/article-lookup/doi/10.3109/13693786.2011.607854.
- ↑ 58.0 58.1 Rajasingham, Radha; Smith, Rachel M; Park, Benjamin J; Jarvis, Joseph N; Govender, Nelesh P; Chiller, Tom M; Denning, David W; Loyse, Angela et al. (August 2017). "Global burden of disease of HIV-associated cryptococcal meningitis: an updated analysis" (in en). The Lancet Infectious Diseases 17 (8): 873–881. doi:10.1016/S1473-3099(17)30243-8. PMID 28483415.
- ↑ Akaihe, Chidinma Lynda; Nweze, Emeka Innocent (January 2021). "Epidemiology of Cryptococcus and cryptococcosis in Western Africa" (in en). Mycoses 64 (1): 4–17. doi:10.1111/myc.13188. ISSN 0933-7407. PMID 32969547. https://onlinelibrary.wiley.com/doi/10.1111/myc.13188.
- ↑ Alemayehu, Tsegaye; Ayalew, Sosina; Buzayehu, Temesgen; Daka, Deresse (2020-04-20). "Magnitude of Cryptococcosis among HIV patients in sub-Saharan Africa countries: a systematic review and meta-analysis" (in en). African Health Sciences 20 (1): 114–121. doi:10.4314/ahs.v20i1.16. ISSN 1729-0503. PMID 33402899. PMC 7750036. https://www.ajol.info/index.php/ahs/article/view/194953.
- ↑ "C. neoformans Infection Statistics | Fungal Diseases | CDC" (in en-us). 2022-11-02. https://www.cdc.gov/fungal/diseases/cryptococcosis-neoformans/statistics.html.
- ↑ 62.0 62.1 Mada, Pradeep Kumar; Jamil, Radia T.; Alam, Mohammed U. (2023), "Cryptococcus", StatPearls (Treasure Island (FL): StatPearls Publishing), PMID 28613714, http://www.ncbi.nlm.nih.gov/books/NBK431060/, retrieved 2023-11-15
- ↑ Alemayehu, Tsegaye; Ayalew, Sosina; Buzayehu, Temesgen; Daka, Deresse (2020-04-20). "Magnitude of Cryptococcosis among HIV patients in sub-Saharan Africa countries: a systematic review and meta-analysis" (in en). African Health Sciences 20 (1): 114–121. doi:10.4314/ahs.v20i1.16. ISSN 1729-0503. PMID 33402899. PMC 7750036. https://www.ajol.info/index.php/ahs/article/view/194953.
- ↑ "Error: no
|title=specified when using {{Cite web}}". https://academic.oup.com/ofid/article/10/8/ofad420/7241483. - ↑ Howard-Jones, Annaleise R.; Sparks, Rebecca; Pham, David; Halliday, Catriona; Beardsley, Justin; Chen, Sharon C.-A. (November 2022). "Pulmonary Cryptococcosis" (in en). Journal of Fungi 8 (11): 1156. doi:10.3390/jof8111156. ISSN 2309-608X. PMID 36354923.
- ↑ Harris, Julie; Lockhart, Shawn; Chiller, Tom (February 2012). "Cryptococcus gattii : where do we go from here?" (in en). Medical Mycology 50 (2): 113–129. doi:10.3109/13693786.2011.607854. ISSN 1369-3786. PMID 21939343. https://academic.oup.com/mmy/article-lookup/doi/10.3109/13693786.2011.607854.
- ↑ "HIV and AIDS Epidemic Global Statistics" (in en). https://www.hiv.gov/hiv-basics/overview/data-and-trends/global-statistics.
- ↑ Kharsany, Ayesha B.M.; Karim, Quarraisha A. (2016-04-08). "HIV Infection and AIDS in Sub-Saharan Africa: Current Status, Challenges and Opportunities". The Open AIDS Journal 10: 34–48. doi:10.2174/1874613601610010034. ISSN 1874-6136. PMID 27347270.
- ↑ "C. neoformans Infection Statistics | Fungal Diseases | CDC" (in en-us). 2022-11-02. https://www.cdc.gov/fungal/diseases/cryptococcosis-neoformans/statistics.html.
- ↑ Akaihe, Chidinma Lynda; Nweze, Emeka Innocent (January 2021). "Epidemiology of Cryptococcus and cryptococcosis in Western Africa" (in en). Mycoses 64 (1): 4–17. doi:10.1111/myc.13188. ISSN 0933-7407. PMID 32969547. https://onlinelibrary.wiley.com/doi/10.1111/myc.13188.
- ↑ 71.0 71.1 Alemayehu, Tsegaye; Ayalew, Sosina; Buzayehu, Temesgen; Daka, Deresse (2020-04-20). "Magnitude of Cryptococcosis among HIV patients in sub-Saharan Africa countries: a systematic review and meta-analysis". African Health Sciences 20 (1): 114–121. doi:10.4314/ahs.v20i1.16. ISSN 1680-6905. PMID 33402899. PMC 7750036. https://www.ajol.info/index.php/ahs/article/view/194953.
- ↑ Patel, Raju K K; Leeme, Tshepo; Azzo, Caitlin; Tlhako, Nametso; Tsholo, Katlego; Tawanana, Ephraim O; Molefi, Mooketsi; Mosepele, Mosepele et al. (2018-11-01). "High Mortality in HIV-Associated Cryptococcal Meningitis Patients Treated With Amphotericin B–Based Therapy Under Routine Care Conditions in Africa" (in en). Open Forum Infectious Diseases 5 (11): ofy267. doi:10.1093/ofid/ofy267. ISSN 2328-8957. PMID 30488038.
- ↑ "Deep Fungal Infections". http://www.cathealth.com/FungalINFXdeep.htm.
- ↑ Akira Takeuchi, D. V. M. (July 2014). Feline Cryptococcosis – WSAVA 2003 Congress – VIN. http://www.vin.com/proceedings/Proceedings.plx?CID=WSAVA2003&PID=6653&O=Generic.
Further reading
- "Clinical practice guidelines for the management of cryptococcal disease: 2010 update by the infectious diseases society of america". Clinical Infectious Diseases 50 (3): 291–322. 2010. doi:10.1086/649858. PMID 20047480.
- "Cryptococcosis: epidemiology, fungal resistance, and new alternatives for treatment". European Journal of Clinical Microbiology & Infectious Diseases 32 (11): 1377–1391. 2013. doi:10.1007/s10096-013-1915-8. PMID 24141976.
- "Cryptococcus neoformans: a sugar-coated killer with designer genes". FEMS Immunology and Medical Microbiology 45 (11): 395–404. 2005. doi:10.1016/j.femsim.2005.06.005. PMID 16055314. (Review)
External links
| Classification | |
|---|---|
| External resources |
 |