Medicine:Postmenopausal confusion
| Postmenopausal confusion | |
|---|---|
| Other names | Postmenopausal brain fog, menopause brain fog |
| Specialty | Gynecology, Midwifery, Neuroscience |
| Symptoms | Forgetfulness, difficulty concentrating |
| Usual onset | Menopause |
Postmenopausal confusion, also commonly referred to as postmenopausal brain fog, is a group of symptoms of menopause in which women report problems with cognition at a higher frequency during postmenopause than before.[1][2]
Multiple studies on cognitive performance following menopause have reported noticeable declines of greater than 60%.[3][4] The common issues presented included impairments in reaction time and attention, difficulty recalling numbers or words, and forgetting reasons for involvement in certain behaviors. Association between subjective cognitive complaints and objective measures of performance show a significant impact on health-related quality of life for postmenopausal women.[5]
Treatment primarily involves symptom management through non-pharmacological treatment strategies. This includes involvement in physical activity and following medically supervised diets, especially those that contain phytoestrogens or resveratrol.[6][7][8][9] Pharmacological interventions in treating postmenopausal confusion are currently being researched. Hormone replacement therapy (HRT) is currently not indicated for the treatment of postmenopausal confusion due to inefficacy.[10][11] The use of HRT for approved indications has identified no significant negative effect on postmenopausal cognition.[10]
Although much of the literature references women, all people who undergo menopause, including those who do not self-identify as women, may experience symptoms of postmenopausal confusion.
History
Research on menopause as a whole declined with the end of the Women's Health Initiative (WHI) studies, but research on the treatment of symptoms associated with menopause—especially the treatment of cognitive decline—continues. The Study of Women's Health Across the Nation (SWAN), first started in 1996, continues to publish progress reports which include cognitive symptoms associated with menopausal transition, including those in postmenopause.[4] As of 2019[update], SWAN indicated, "Approximately 60% of midlife women report problems with memory during the [menopause transition], yet studies of measured cognitive performance during the transition are rare."[4]
Although there are many relationships between hormone levels in postmenopause and cognitive function, the previously favored HRT therapies (estrogen therapies) have been shown to be ineffective in specifically treating postmenopausal confusion.[12][10][13] The use of hormone replacement therapies, once considered detrimental to cognition in postmenopausal women, has now been shown to have no negative effect when used properly for approved indications.[10][13][14] There are no conclusive studies to support any pharmacological agents, but several potential drug candidates are still being explored.
Presentation
Menopause is a natural decline in the ovarian function of women who reach the age between 45 and 54 years. "About 25 million women pass through menopause worldwide each year, and it has been estimated that, by the year 2030, the world population of menopausal and postmenopausal women will be 1.2 billion, with 47 million new entrants each year."[15]
Postmenopause begins immediately following menopause (one year after the final menstrual cycle).[16] Postmenopausal confusion is often manifested through the following cognitive symptoms: memory problems, forgetfulness, and poor concentration.[17] Confusion which is otherwise unexplained and coincides with the onset of postmenopause may be postmenopausal confusion.[18]
Causes
Risk factors
Hypertension
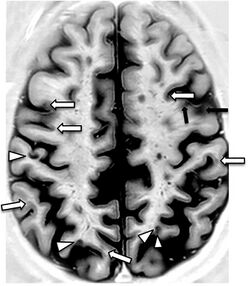
A 2019 literature review identified hypertension and history of pre-eclampsia as significant risk factors for the accelerated decline of cognitive function in women during midlife. Although the mechanism remains unclear, neuroimaging studies included in the review found that those with hypertension have evident structural changes in their brains; specifically, gray matter brain volume decreased and white matter hyperintensity volume increased.[18]
Atherosclerosis and comorbidities
Atherosclerosis and comorbidities such as hyperlipidemia and diabetes mellitus have long been considered risk factors for cognitive decline because they have the propensity to cause the formation of amyloid plaques (aggregates of misfolded, deleterious proteins) in the brain.[19]
Insomnia
Many postmenopausal women report insomnia. Studies have shown "associations between poor sleep quality and cognitive decline" in postmenopausal women as those with insufficient sleep, or with difficulty falling or staying asleep, reported decreased cognitive performance including "verbal memory, attention, and general cognition."[3]
Depression
There is evidence linking depression and cognitive decline in postmenopausal women. Research suggests that increased cortisol levels from depressive episodes may affect the hippocampus, area of the brain responsible for episodic memory. Studies have also shown a correlation between depression and decreased cognitive performance including "processing speed, verbal memory, and working memory" in postmenopausal women.[3]
Hot flashes
There are studies indicating a correlation between frequency of hot flashes in postmenopausal women and a deficit in verbal memory performance. It is suggested that faster blood flow in the brain or higher cortisol levels from hot flashes may cause changes in the brain and affect information processing and memory.[3]
Surgical menopause
A 2019 systematic review and meta-analysis identified surgical menopause, especially when performed at or before the age of 45, as a substantial risk factor for cognitive decline and dementia.[20]
Cardiac procedures
Cardiac procedures such as invasive cerebral and coronary angiography, coronary artery bypass graft surgery (CABG), surgical aortic valve replacement, and transcatheter aortic valve replacement (TAVR) have been found to increase the risk of cognitive decline in females as they been found to increase the incidence of brain lesions.[19]
Mechanism
The mechanism of postmenopausal confusion is poorly understood due to simultaneous aging-related physiological changes, as well as differential diagnoses presenting with similar symptoms.[2] Research remains ongoing.
Treatment
Overview
There are pharmacological and non-pharmacological considerations in improving the symptoms of postmenopausal confusion. Currently, no pharmacological agents are indicated to treat postmenopausal confusion, but research remains ongoing. Non-pharmacological strategies to manage postmenopausal confusion symptoms are utilized, with focus on diet and exercise.
Pharmacological
Hormone therapy
Hormone therapy, also known as estrogen therapy, was previously a common treatment for postmenopausal confusion. However, more recent research indicates that hormone therapy is not an effective treatment for postmenopausal cognitive symptoms.[10][11] A 2008 Cochrane review of 16 trials concluded that there is a body of evidence that suggests that hormone replacement therapy is unable to prevent cognitive decline or maintain cognitive function in healthy postmenopausal women when given over a short or long period of time.[11] Conversely, studies have also suggested that the use of hormone replacement therapy are unlikely to have negative cognitive effects when used for their approved indications.[10]
Previous research suggested that increases in blood flow to the hippocampus and temporal lobe occurred from hormone therapy, improving postmenopausal confusion symptoms.[21] More recent research no longer supports this, and is inconclusive as to the true effects of estrogen on hippocampal volume as studies show results differing from improved cognition and maintained hippocampal volume when hormone therapy is administered during menopause to results showing no obvious beneficial results.[22]
Research focusing on adiponectin (ADPN) has yielded positive results in the development of possible treatments for postmenopausal confusion. A study has shown an association between higher levels of ADPN and increased cognitive performance in postmenopausal women. However, an ADPN receptor agonist has yet to be discovered.[23]
Psychostimulant therapy
There is ongoing research regarding the efficacy of psychostimulant drugs such as lisdexamphetamine (Vyvanse) and atomoxetine (Strattera) in treating postmenopausal and menopausal confusion.[24][25]
Non-pharmacological
Diet

Individuals play an important role in maintaining their cognitive health. One way to achieve this is by the promotion of healthy nutrition. In particular, the Mediterranean diet, defined as being low in saturated fat and high in vegetable oils, showed improvement in aspects of cognitive function. This diet consists of low intake of sweets and eggs, moderate intakes of meat and fish, dairy products and red wine, and high intake of leafy green vegetables, pulses/legumes and nuts, fruits, cereal, and cold pressed extra virgin olive oil.[7] Further analysis concluded that the Mediterranean diet supplemented by olive oil resulted in better cognition and memory as compared to the Mediterranean diet plus mixed nuts combination.[26]
Supplementation
Soy isoflavones (SIF), a type of phytoestrogen which can be found in soybeans, fruits and nuts, has been shown to improve cognitive outcomes in recent postmenopausal women of less than 10 years. This suggests that the initiation of SIF may have a critical margin of opportunity when used at a younger age in postmenopausal women. In addition to improved cognitive functions and visual memory, no evidence of harm from SIF supplementation was revealed with the dose ranges tested in multiple trials.[8]
Analysis of multiple randomized controlled trials have brought attention to black cohosh and red clover (which contain phytoestrogen) and its potential as an efficacious treatment of menopausal symptoms. Black cohosh did not reveal any evidence of risk of harm, but lack of good evidence cannot firmly conclude its safety.[27] Overall, the results suggested that neither botanical treatments provided any cognitive benefits.[28]
Resveratrol, another bioactive compound derived from plants, has also shown to improve cognitive performance in postmenopausal women. There are ongoing trials studying the cognitive benefits of resveratrol in early versus late postmenopausal women.[9]
Chronic ginkgo biloba supplementation has been shown to improve "mental flexibility" in "older and more cognitively impaired" postmenopausal women. However, a combined ginkgo biloba and ginger supplementation had no effect on memory or cognitive performance in postmenopausal women.[29]
Dehydroepiandrosterone (DHEA) supplementation may improve cognition in women with postmenopausal confusion but does not benefit those without cognitive impairment.[30] More long-term studies are required to study the efficacy of DHEA and its role in cognition and postmenopausal women.[31]
Exercise
Regular physical exercise may prevent symptoms of postmenopausal confusion. Studies have shown an association between exercise and "lower rates of cognitive decline" in postmenopausal women. On the other hand, an inactive lifestyle has been strongly associated with "higher rates of cognitive decline" in postmenopausal women.[6]
Mind-body therapy
Studies have shown benefits of mind-body therapies in women with postmenopausal symptoms including cognitive impairment. Mindfulness, hypnosis, and yoga may help decrease symptoms of insomnia, depression, or hot flashes in postmenopausal women which leads to better cognitive performance.[3]
See also
References
- ↑ Norton, Amy. "More Evidence Menopause 'Brain Fog' Is Real" (in en). https://www.webmd.com/menopause/news/20161012/more-evidence-menopause-brain-fog-is-real.
- ↑ 2.0 2.1 Dalal, PronobK; Agarwal, Manu (2015). "Postmenopausal syndrome" (in en). Indian Journal of Psychiatry 57 (6): S222-32. doi:10.4103/0019-5545.161483. ISSN 0019-5545. PMID 26330639. PMC 4539866. http://www.indianjpsychiatry.org/text.asp?2015/57/6/222/161483.
- ↑ 3.0 3.1 3.2 3.3 3.4 Sliwinski, Jim R; Johnson, Aimee K; Elkins, Gary R (2014). "Memory Decline in Peri- and Post-menopausal Women: The Potential of Mind–Body Medicine to Improve Cognitive Performance". Integrative Medicine Insights 9: 17–23. doi:10.4137/IMI.S15682. ISSN 1177-3936. PMID 25125972.
- ↑ 4.0 4.1 4.2 El Khoudary, Samar R.; Greendale, Gail; Crawford, Sybil L.; Avis, Nancy E.; Brooks, Maria M.; Thurston, Rebecca C.; Karvonen-Gutierrez, Carrie; Waetjen, L. Elaine et al. (2019). "The menopause transition and women's health at midlife: a progress report from the Study of Women's Health Across the Nation (SWAN)" (in en). Menopause 26 (10): 1213–1227. doi:10.1097/GME.0000000000001424. ISSN 1530-0374. PMID 31568098.
- ↑ Maki, Pauline M.; Henderson, Victor W. (2016). "Cognition and the menopause transition" (in en). Menopause 23 (7): 803–805. doi:10.1097/GME.0000000000000681. ISSN 1072-3714. PMID 27272226. https://dx.doi.org/10.1097/GME.0000000000000681.
- ↑ 6.0 6.1 Anderson, Debra; Seib, Charlotte; Rasmussen, Laura (2014). "Can physical activity prevent physical and cognitive decline in postmenopausal women?" (in en). Maturitas 79 (1): 14–33. doi:10.1016/j.maturitas.2014.06.010. PMID 25008420. https://linkinghub.elsevier.com/retrieve/pii/S0378512214002060.
- ↑ 7.0 7.1 Davis, Courtney; Bryan, Janet; Hodgson, Jonathan; Murphy, Karen (2015). "Definition of the Mediterranean Diet; A Literature Review" (in en). Nutrients 7 (11): 9139–9153. doi:10.3390/nu7115459. PMID 26556369.
- ↑ 8.0 8.1 Cheng, Peng-Fei; Chen, Jian-Jun; Zhou, Xin-Yu; Ren, Yi-Fei; Huang, Wen; Zhou, Jing-Jing; Xie, Peng (2015). "Do soy isoflavones improve cognitive function in postmenopausal women? A meta-analysis" (in en-US). Menopause 22 (2): 198–206. doi:10.1097/GME.0000000000000290. ISSN 1530-0374. PMID 25003621. https://dx.doi.org/10.1097/GME.0000000000000290.
- ↑ 9.0 9.1 Thaung Zaw, Jay Jay; Howe, Peter Ranald Charles; Wong, Rachel Heloise Xiwen (2018). "Postmenopausal health interventions: Time to move on from the Women's Health Initiative?" (in en). Ageing Research Reviews 48: 79–86. doi:10.1016/j.arr.2018.10.005. ISSN 1568-1637. PMID 30355506. https://www.sciencedirect.com/science/article/pii/S1568163718301612.
- ↑ 10.0 10.1 10.2 10.3 10.4 10.5 Sheikh, Knvul. "Hormone Therapy May Not Prevent Postmenopausal Brain Fog" (in en). https://www.scientificamerican.com/article/hormone-therapy-may-not-prevent-postmenopausal-brain-fog/.
- ↑ 11.0 11.1 11.2 Lethaby, Anne; Hogervorst, Eva; Richards, Marcus; Yesufu, Amina; Yaffe, Kristine (2008). "Hormone replacement therapy for cognitive function in postmenopausal women". Cochrane Database of Systematic Reviews 2008 (1): CD003122. doi:10.1002/14651858.CD003122.pub2. PMID 18254016.
- ↑ Mott, Natasha N.; Toni R. Pak (2013). "Estrogen Signaling and the Aging Brain: Context-Dependent Consideration for Postmenopausal Hormone Therapy". ISRN Endocrinology 2013: 1–16. doi:10.1155/2013/814690. PMID 23936665.
- ↑ 13.0 13.1 Gava, Giulia; Orsili, Isabella; Alvisi, Stefania; Mancini, Ilaria; Seracchioli, Renato; Meriggiola, Maria Cristina (2019). "Cognition, Mood and Sleep in Menopausal Transition: The Role of Menopause Hormone Therapy" (in en). Medicina 55 (10): 668. doi:10.3390/medicina55100668. ISSN 1648-9144. PMID 31581598.
- ↑ Grimm, A.; Y. Lim; A.G. Mensah-Nyagan; J. Götz; A. Eckert (2012). "Alzheimer's disease, oestrogen and mitochondria: an ambiguous relationship". Molecular Neurobiology 46 (1): 151–160. doi:10.1007/s12035-012-8281-x. PMID 22678467.
- ↑ Borrelli, Francesca; Ernst, Edzard (2008). "Black cohosh (Cimicifuga racemosa) for menopausal symptoms: A systematic review of its efficacy" (in en). Pharmacological Research 58 (1): 8–14. doi:10.1016/j.phrs.2008.05.008. ISSN 1043-6618. PMID 18585461. https://www.sciencedirect.com/science/article/abs/pii/S1043661808000996.
- ↑ "Postmenopause" (in en). 6 April 2021. https://healthcare.utah.edu/womenshealth/gynecology/menopause/postmenopause.php.
- ↑ Henderson, Victor W. (2008). "Cognitive Changes After Menopause: Influence of Estrogen". Clinical Obstetrics and Gynecology 51 (3): 618–626. doi:10.1097/GRF.0b013e318180ba10. ISSN 0009-9201. PMID 18677155.
- ↑ 18.0 18.1 Miller, Kathleen B.; Miller, Virginia M.; Barnes, Jill N. (2019). "Pregnancy History, Hypertension, and Cognitive Impairment in Postmenopausal Women". Current Hypertension Reports 21 (12): 93. doi:10.1007/s11906-019-0997-9. PMID 31741134.
- ↑ 19.0 19.1 Volgman, Annabelle Santos; Bairey Merz, C. Noel; Aggarwal, Neelum T.; Bittner, Vera; Bunch, T. Jared; Gorelick, Philip B.; Maki, Pauline; Patel, Hena N. et al. (2019). "Sex Differences in Cardiovascular Disease and Cognitive Impairment: Another Health Disparity for Women?". Journal of the American Heart Association 8 (19): e013154. doi:10.1161/JAHA.119.013154. PMID 31549581.
- ↑ Georgakisa, Marios; Beskou-Konto, Theano; Theodoridis, Ioannis; Skalkidou, Alkistis; Petridou, Eleni (2019). "Surgical menopause in association with cognitive function and risk of dementia: A systematic review and meta-analysis". Psychoneuroendocrinology 106: 9–19. doi:10.1016/j.psyneuen.2019.03.013. PMID 30928686.
- ↑ Maki, PM (2005). "Estrogen effects on the hippocampus and frontal lobes". International Journal of Fertility and Women's Medicine 50 (2): 67–71. PMID 16334413.
- ↑ Wnuk, A.; D.L. Korol; K.I. Erickson (2012). "Estrogens, hormone therapy, and hippocampal volume in postmenopausal women". Maturitas 73 (3): 186–190. doi:10.1016/j.maturitas.2012.07.001. PMID 22858056.
- ↑ Rizzo, Maria Rosaria; Fasano, Renata; Paolisso, Giuseppe (2020). "Adiponectin and Cognitive Decline". International Journal of Molecular Sciences 21 (6): 2010. doi:10.3390/ijms21062010. ISSN 1422-0067. PMID 32188008.
- ↑ University of Pennsylvania (2017). Attention & Memory Impairments in Menopausal Women: A Possible Role for Vyvanse?. Shire. https://clinicaltrials.gov/ct2/show/study/NCT01324024.
- ↑ Epperson, C. Neill; Pittman, Brian; Czarkowski, Kathryn A.; Bradley, Jeanette; Quinlan, Donald M.; Brown, Thomas E. (2015). "Impact of atomoxetine on subjective attention and memory difficulties in perimenopausal and postmenopausal women" (in en). Menopause 18 (5): 542–548. doi:10.1097/gme.0b013e3181fcafd6. ISSN 1072-3714. PMID 21293309. PMC 4076798. https://dx.doi.org/10.1097/gme.0b013e3181fcafd6.
- ↑ Lehert, P.; Villaseca, P.; Hogervorst, E.; Maki, P. M.; Henderson, V. W. (2015). "Individually modifiable risk factors to ameliorate cognitive aging: a systematic review and meta-analysis". Climacteric 18 (5): 678–689. doi:10.3109/13697137.2015.1078106. ISSN 1369-7137. PMID 26361790.
- ↑ Leach, Matthew J; Moore, Vivienne (2012). "Black cohosh (Cimicifuga spp.) for menopausal symptoms". The Cochrane Database of Systematic Reviews 2012 (9): CD007244. doi:10.1002/14651858.CD007244.pub2. ISSN 1469-493X. PMID 22972105.
- ↑ Maki, Pauline M.; Rubin, Leah H.; Fornelli, Deanne; Drogos, Lauren; Banuvar, Suzanne; Shulman, Lee P.; Geller, Stacie E. (2009). "Effects of botanicals and combined hormone therapy on cognition in postmenopausal women" (in en). Menopause 16 (6): 1167–1177. doi:10.1097/gme.0b013e3181ace484. ISSN 1072-3714. PMID 19590458. PMC 2783198. https://dx.doi.org/10.1097/gme.0b013e3181ace484.
- ↑ Clement, Yuri N.; Onakpoya, Igho; Hung, Shao K.; Ernst, Edzard (2011). "Effects of herbal and dietary supplements on cognition in menopause: A systematic review" (in en). Maturitas 68 (3): 256–263. doi:10.1016/j.maturitas.2010.12.005. ISSN 0378-5122. PMID 21237589. https://www.sciencedirect.com/science/article/abs/pii/S0378512210004536.
- ↑ Goel, Rachna M.; Cappola, Anne R. (2011). "Dehydroepiandrosterone sulfate and postmenopausal women" (in en-US). Current Opinion in Endocrinology, Diabetes and Obesity 18 (3): 171–176. doi:10.1097/MED.0b013e3283461818. ISSN 1752-296X. PMID 21478748. https://dx.doi.org/10.1097/MED.0b013e3283461818.
- ↑ Pluchino, N.; Drakopoulos, P.; Bianchi-Demicheli, F.; Wenger, J.M.; Petignat, P.; Genazzani, A.R. (2015). "Neurobiology of DHEA and effects on sexuality, mood and cognition" (in en). The Journal of Steroid Biochemistry and Molecular Biology 145: 273–280. doi:10.1016/j.jsbmb.2014.04.012. ISSN 0960-0760. PMID 24892797. https://www.sciencedirect.com/science/article/abs/pii/S0960076014000983.
Further reading
- Rao, Y.S.; Mott, N.N.; Wang, Y.; Chung, W.C.; Pak, T.R. (2013). "MicroRNAs in the aging female brain: a putative mechanism for age-specific estrogen effects". Endocrinology 154 (8): 2795–2806. doi:10.1210/en.2013-1230. PMID 23720423.
- Shafin, N.; Zakaria, R.; Hussain, N.H.; Othman, Z. (2013). "Association of oxidative stress and memory performance in postmenopausal women receiving estrogen progestin therapy". Menopause 20 (6): 661–666. doi:10.1097/GME.0b013e31827758c6. PMID 23715378. http://eprints.usm.my/44480/1/10.1097%40gme.0b013e31827758c6.pdf.
- Epperson, C.N.; Sammel, M.D.; Freeman, E.W. (2013). "Menopause effects on verbal memory: findings from a longitudinal community cohort". Journal of Clinical Endocrinology and Metabolism 98 (9): 3829–3838. doi:10.1210/jc.2013-1808. PMID 23836935.
- Sherwin, Barbara B.; Miglena Grigorova (2011). "Differential effects of estrogen and micronized progesterone or medroxyprogesterone acetate on cognition in postmenopausal women". Fertility and Sterility 96 (2): 399–403. doi:10.1016/j.fertnstert.2011.05.079. PMID 21703613.
- Epperson, C.N.; Amin, Z.; Ruparel, K.; Gur, R.; Loughead, J. (2012). "Interactive effects of estrogen and serotonin on brain activation during working memory and affective processing in menopausal women". Psychoneuroendocrinology 37 (3): 372–382. doi:10.1016/j.psyneuen.2011.07.007. PMID 21820247.
- Hampson, Elizabeth; E.E. Morley (2013). "Estradiol concentrations and working memory performance in women of reproductive age". Psychoneuroendocrinology 38 (12): 2897–2904. doi:10.1016/j.psyneuen.2013.07.020. PMID 24011502.
- Hunter, Myra S.; Joseph Chilcot (2013). "Testing a cognitive model of menopausal hot flushes and night sweats". Journal of Psychosomatic Research 74 (4): 307–312. doi:10.1016/j.jpsychores.2012.12.005. PMID 23497832.
