Biology:Human serum albumin
 Generic protein structure example |
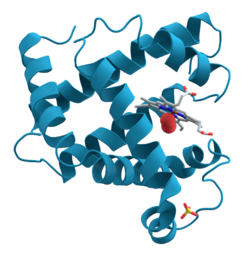
Human serum albumin is the serum albumin found in human blood. It is the most abundant protein in human blood plasma; it constitutes about half of serum protein. It is produced in the liver. It is soluble in water, and it is monomeric.[citation needed]
Albumin transports hormones, fatty acids, and other compounds, buffers pH, and maintains oncotic pressure, among other functions.
Albumin is synthesized in the liver as preproalbumin, which has an N-terminal peptide that is removed before the nascent protein is released from the rough endoplasmic reticulum. The product, proalbumin, is in turn cleaved in the Golgi apparatus to produce the secreted albumin.
The reference range for albumin concentrations in serum is approximately 35–50 g/L (3.5–5.0 g/dL).[1] It has a serum half-life of approximately 21 days.[2] It has a molecular mass of 66.5 kDa.
The gene for albumin is located on chromosome 4 in locus 4q13.3 and mutations in this gene can result in anomalous proteins. The human albumin gene is 16,961 nucleotides long from the putative 'cap' site to the first poly(A) addition site. It is split into 15 exons that are symmetrically placed within the 3 domains thought to have arisen by triplication of a single primordial domain.
Human serum albumin (HSA) is a highly water-soluble globular monomeric plasma protein with a relative molecular weight of 67 KDa, consisting of 585 amino acid residues, one sulfhydryl group and 17 disulfide bridges. Among nanoparticulate carriers, HSA nanoparticles have long been the center of attention in the pharmaceutical industry due to their ability to bind to various drug molecules, great stability during storage and in vivo usage, no toxicity and antigenicity, biodegradability, reproducibility, scale up of the production process and a better control over release properties. In addition, significant amounts of drug can be incorporated into the particle matrix because of the large number of drug binding sites on the albumin molecule.[3]
Function
- Maintains oncotic pressure
- Transports thyroid hormones
- Transports other hormones, in particular, ones that are fat-soluble
- Transports fatty acids ("free" fatty acids) to the liver and to myocytes for utilization of energy
- Transports unconjugated bilirubin
- Transports many drugs; serum albumin levels can affect the half-life of drugs. Competition between drugs for albumin binding sites may cause drug interaction by increasing the free fraction of one of the drugs, thereby affecting potency.
- Competitively binds calcium ions (Ca2+)
- Serum albumin, as a negative acute-phase protein, is down-regulated in inflammatory states. As such, it is not a valid marker of nutritional status; rather, it is a marker of an inflammatory state
- Prevents photodegradation of folic acid
- Prevent pathogenic effects of Clostridioides difficile toxins[4]
Measurement
Serum albumin is commonly measured by recording the change in absorbance upon binding to a dye such as bromocresol green or bromocresol purple.[5]
Reference ranges
The normal range of human serum albumin in adults (> 3 y.o.) is 3.5–5.0 g/dL (35–50 g/L). For children less than three years of age, the normal range is broader, 2.9–5.5 g/dL.[6]
Low albumin (hypoalbuminemia) may be caused by liver disease, nephrotic syndrome, burns, protein-losing enteropathy, malabsorption, malnutrition, late pregnancy, artefact, genetic variations and malignancy.[citation needed]
High albumin (hyperalbuminemia) is almost always caused by dehydration. In some cases of retinol (Vitamin A) deficiency, the albumin level can be elevated to high-normal values (e.g., 4.9 g/dL) because retinol causes cells to swell with water. (This is also the reason too much Vitamin A is toxic.)[7] This swelling also likely occurs during treatment with 13-cis retinoic acid (isotretinoin), a pharmaceutical for treating severe acne, amongst other conditions. In lab experiments it has been shown that all-trans retinoic acid down regulates human albumin production.[8]
Pathology
Hypoalbuminemia
Hypoalbuminemia means low blood albumin levels.[9] This can be caused by:
- Liver disease; cirrhosis of the liver is most common
- Excess excretion by the kidneys (as in nephrotic syndrome)
- Excess loss in bowel (protein-losing enteropathy, e.g., Ménétrier's disease)
- Burns (plasma loss in the absence of skin barrier)
- Redistribution (hemodilution [as in pregnancy], increased vascular permeability or decreased lymphatic clearance)
- Acute disease states (referred to as a negative acute-phase protein)[10]
- Malnutrition and wasting[11]
- Mutation causing analbuminemia (very rare)
- Anorexia nervosa (most common cause in adolescents)
In clinical medicine, hypoalbuminemia significantly correlates with a higher mortality rates in several conditions such as heart failure, post-surgery, COVID-19.[12][13][14]
Hyperalbuminemia
Hyperalbuminemia is an increased concentration of albumin in the blood.[15] Typically, this condition is due to dehydration.[15] Hyperalbuminemia has also been associated with high protein diets.[16]
Medical use
Human albumin solution (HSA) is available for medical use, usually at concentrations of 5–25%.
Human albumin is often used to replace lost fluid and help restore blood volume in trauma, burns and surgery patients. There is no strong medical evidence that albumin administration (compared to saline) saves lives for people who have hypovolaemia or for those who are critically ill due to burns or hypoalbuminaemia.[17] It is also not known if there are people who are critically ill that may benefit from albumin.[17] Therefore, the Cochrane Collaboration recommends that it should not be used, except in clinical trials.[17][18]
In acoustic droplet vaporization (ADV), albumin is sometimes used as a surfactant. ADV has been proposed as a cancer treatment by means of occlusion therapy.[19]
Human serum albumin may be used to potentially reverse drug/chemical toxicity by binding to free drug/agent.[20]
Human albumin may also be used in treatment of decompensated cirrhosis.[21]
Human serum albumin has been used as a component of a frailty index.[11]
Glycation
It has been known for a long time that human blood proteins like hemoglobin[22] and serum albumin[23][24] may undergo a slow non-enzymatic glycation, mainly by formation of a Schiff base between ε-amino groups of lysine (and sometimes arginine) residues and glucose molecules in blood (Maillard reaction). This reaction can be inhibited in the presence of antioxidant agents.[25] Although this reaction may happen normally,[23] elevated glycoalbumin is observed in diabetes mellitus.[24]
Glycation has the potential to alter the biological structure and function of the serum albumin protein.[26][27][28][29]
Moreover, the glycation can result in the formation of Advanced Glycation End-Products (AGE), which result in abnormal biological effects. Accumulation of AGEs leads to tissue damage via alteration of the structures and functions of tissue proteins, stimulation of cellular responses, through receptors specific for AGE-proteins, and generation of reactive oxygen intermediates. AGEs also react with DNA, thus causing mutations and DNA transposition. Thermal processing of proteins and carbohydrates brings major changes in allergenicity. AGEs are antigenic and represent many of the important neoantigens found in cooked or stored foods.[30] They also interfere with the normal product of nitric oxide in cells.[31]
Although there are several lysine and arginine residues in the serum albumin structure, very few of them can take part in the glycation reaction.[24][32]
Oxidation
The albumin is the predominant protein in most body fluids, its Cys34 represents the largest fraction of free thiols within the body. The albumin Cys34 thiol exists in both reduced and oxidized forms.[33] In plasma of healthy young adults, 70–80% of total HSA contains the free sulfhydryl group of Cys34 in a reduced form or mercaptoalbumin (HSA-SH).[34] However, in pathological states characterized by oxidative stress such as kidney disease, liver disease and diabetes the oxidized form, or non-mercaptoalbumin (HNA), could predominate.[35][36] The albumin thiol reacts with radical hydroxyl (.OH), hydrogen peroxide (H2O2) and the reactive nitrogen species as peroxynitrite (ONOO.), and have been shown to oxidize Cys34 to sulfenic acid derivate (HSA-SOH), it can be recycled to mercapto-albumin; however at high concentrations of reactive species leads to the irreversible oxidation to sulfinic (HSA-SO2H) or sulfonic acid (HSA-SO3H) affecting its structure.[37] Presence of reactive oxygen species (ROS), can induce irreversible structural damage and alter protein activities.[citation needed]
Loss via kidneys
In the healthy kidney, albumin's size and negative electric charge exclude it from excretion in the glomerulus. This is not always the case, as in some diseases including diabetic nephropathy, which can sometimes be a complication of uncontrolled or of longer term diabetes in which proteins can cross the glomerulus. The lost albumin can be detected by a simple urine test.[38] Depending on the amount of albumin lost, a patient may have normal renal function, microalbuminuria, or albuminuria.
Interactions
Human serum albumin has been shown to interact with FCGRT.[39]
It might also interact with a yet-unidentified albondin (gp60), a certain pair of gp18/gp30, and some other proteins like osteonectin, hnRNPs, calreticulin, cubilin, and megalin.[40]
See also
References
- ↑ "Harmonisation of Reference Intervals". pathologyharmony.co.uk. Pathology Harmony. http://www.acb.org.uk/docs/Pathology%20Harmony%20for%20web.pdf.
- ↑ Hypoalbuminemia: Background, Pathophysiology, Etiology. 2019-11-10. https://emedicine.medscape.com/article/166724-overview. Retrieved 2019-12-22.
- ↑ "Efficient loading and entrapment of tamoxifen in human serum albumin based nanoparticulate delivery system by a modified desolvation technique". Chemical Engineering Research and Design 92 (9): 1681–1692. September 2014. doi:10.1016/j.cherd.2013.11.024.
- ↑ "Human Serum Albumin Is an Essential Component of the Host Defense Mechanism Against Clostridium difficile Intoxication". The Journal of Infectious Diseases 218 (9): 1424–1435. September 2018. doi:10.1093/infdis/jiy338. PMID 29868851.
- ↑ "Albumin: analyte monograph". Association for Clinical Biochemistry and Laboratory Medicine. http://www.acb.org.uk/docs/NHLM/Albumin.pdf.
- ↑ "Normal Ranges for Common Laboratory Tests.". http://www.rush.edu/webapps/rml/RMLRangesCMP.jsp. Rush University
- ↑ "Protective effect of taurine, zinc and tocopherol on retinol-induced damage in human lymphoblastoid cells". The Journal of Nutrition 114 (12): 2256–2261. December 1984. doi:10.1093/jn/114.12.2256. PMID 6502269.
- ↑ "All-trans retinoic acid down-regulates human albumin gene expression through the induction of C/EBPbeta-LIP". The Biochemical Journal 397 (2): 345–353. July 2006. doi:10.1042/BJ20051863. PMID 16608438.
- ↑ Dorland's illustrated medical dictionary (29th ed.). Philadelphia [u.a.]: Saunders. 2000. p. 860. ISBN 978-0721682617. https://archive.org/details/trent_0116404640520/page/860.
- ↑ "The Impact of Serum Albumin Levels on COVID-19 Mortality" (in en). Infectious Disease Reports 14 (3): 278–286. 2022-04-20. doi:10.3390/idr14030034. ISSN 2036-7449. PMID 35645213.
- ↑ 11.0 11.1 "The impact of frailty status on survival after transcatheter aortic valve replacement in older adults with severe aortic stenosis: a single-center experience". JACC. Cardiovascular Interventions 5 (9): 974–981. September 2012. doi:10.1016/j.jcin.2012.06.011. PMID 22995885.
- ↑ "Serum albumin and mortality in acutely decompensated heart failure". American Heart Journal 160 (6): 1149–1155. December 2010. doi:10.1016/j.ahj.2010.09.004. PMID 21146671.
- ↑ "Preoperative hypoalbuminemia in patients undergoing cardiac surgery: a meta-analysis". Surgery Today 53 (8): 861–872. August 2022. doi:10.1007/s00595-022-02566-9. PMID 35933630.
- ↑ "The Impact of Serum Albumin Levels on COVID-19 Mortality". Infectious Disease Reports 14 (3): 278–286. April 2022. doi:10.3390/idr14030034. PMID 35645213.
- ↑ 15.0 15.1 "Chapter 101: Serum Albumin and Globulin". Clinical methods : the history, physical, and laboratory examinations (3rd ed.). Boston: Butterworths. 1990. ISBN 978-0409900774. https://www.ncbi.nlm.nih.gov/books/NBK204/#_A3173_.
- ↑ "Hyperalbuminemia and elevated transaminases associated with high-protein diet". Scandinavian Journal of Gastroenterology 41 (6): 759–760. June 2006. doi:10.1080/00365520500442625. PMID 16716979.
- ↑ 17.0 17.1 17.2 "Human albumin solution for resuscitation and volume expansion in critically ill patients". The Cochrane Database of Systematic Reviews 2011 (11): CD001208. November 2011. doi:10.1002/14651858.CD001208.pub4. PMID 22071799.
- ↑ "Expert consensus on the use of human serum albumin in critically ill patients". Chinese Medical Journal 134 (14): 1639–1654. July 2021. doi:10.1097/CM9.0000000000001661. PMID 34397592.
- ↑ "Acoustic droplet vaporization threshold: effects of pulse duration and contrast agent". IEEE Transactions on Ultrasonics, Ferroelectrics, and Frequency Control 54 (5): 933–946. May 2007. doi:10.1109/tuffc.2007.339. PMID 17523558.
- ↑ "Fipronil recognition by the FA1 site of human serum albumin". Journal of Molecular Recognition 31 (8): e2713. August 2018. doi:10.1002/jmr.2713. PMID 29656610.
- ↑ "Long-term albumin administration in decompensated cirrhosis (ANSWER): an open-label randomised trial". Lancet 391 (10138): 2417–2429. June 2018. doi:10.1016/S0140-6736(18)30840-7. PMID 29861076.
- ↑ "An abnormal hemoglobin in red cells of diabetics". Clinica Chimica Acta; International Journal of Clinical Chemistry 22 (2): 296–298. October 1968. doi:10.1016/0009-8981(68)90372-0. PMID 5687098.
- ↑ 23.0 23.1 "Nonenzymatically glucosylated albumin. In vitro preparation and isolation from normal human serum". The Journal of Biological Chemistry 254 (3): 595–597. February 1979. doi:10.1016/S0021-9258(17)37845-6. PMID 762083.
- ↑ 24.0 24.1 24.2 "Nonenzymatic glycosylation of albumin in vivo. Identification of multiple glycosylated sites". The Journal of Biological Chemistry 261 (29): 13542–13545. October 1986. doi:10.1016/S0021-9258(18)67052-8. PMID 3759977.
- ↑ "Inhibition of nonenzymatic protein glycation and lipid peroxidation by drugs with antioxidant activity". Life Sciences 65 (18–19): 1991–1993. 1999. doi:10.1016/S0024-3205(99)00462-2. PMID 10576452.
- ↑ "Thermodynamic analysis of human serum albumin interactions with glucose: insights into the diabetic range of glucose concentration". The International Journal of Biochemistry & Cell Biology 34 (9): 1115–1124. September 2002. doi:10.1016/S1357-2725(02)00031-6. PMID 12009306.
- ↑ "Nonenzymatic glycosylation of human serum albumin alters its conformation and function". The Journal of Biological Chemistry 259 (6): 3812–3817. March 1984. doi:10.1016/S0021-9258(17)43168-1. PMID 6706980.
- ↑ "The effect of non-enzymatic glycation on the unfolding of human serum albumin". Archives of Biochemistry and Biophysics 444 (2): 92–99. December 2005. doi:10.1016/j.abb.2005.10.019. PMID 16309624.
- ↑ "The thermal analysis of nonezymatic glycosylation of human serum albumin: differential scanning calorimetry and circular dichroism studies". Thermochimica Acta 389 (1–2): 141–151. July 2002. doi:10.1016/S0040-6031(02)00006-0.
- ↑ "Thermal glycation of proteins by D-glucose and D-fructose". Archivum Immunologiae et Therapiae Experimentalis 50 (1): 61–66. 2002. PMID 11916310.
- ↑ "Regulation of endothelial nitric oxide synthase expression by albumin-derived advanced glycosylation end products". Circulation Research 86 (3): E50–E54. February 2000. doi:10.1161/01.RES.86.3.e50. PMID 10679490.
- ↑ "The principal site of nonenzymatic glycosylation of human serum albumin in vivo". The Journal of Biological Chemistry 258 (10): 6142–6146. May 1983. doi:10.1016/S0021-9258(18)32384-6. PMID 6853480.
- ↑ "Identification and characterization of oxidized human serum albumin. A slight structural change impairs its ligand-binding and antioxidant functions". The FEBS Journal 273 (14): 3346–3357. July 2006. doi:10.1111/j.1742-4658.2006.05341.x. PMID 16857017.
- ↑ "Oxidation of the albumin thiol to sulfenic acid and its implications in the intravascular compartment". Brazilian Journal of Medical and Biological Research = Revista Brasileira de Pesquisas Medicas e Biologicas 42 (4): 305–311. April 2009. doi:10.1590/s0100-879x2009000400001. PMID 19330257.
- ↑ "Antioxidant capacity and structural changes of human serum albumin from patients in advanced stages of diabetic nephropathy and the effect of the dialysis". Molecular and Cellular Biochemistry 404 (1–2): 193–201. June 2015. doi:10.1007/s11010-015-2378-2. PMID 25758354.
- ↑ "Clinical Implications Associated With the Posttranslational Modification-Induced Functional Impairment of Albumin in Oxidative". Journal of Pharmaceutical Sciences 106 (9): 2195-2203. 2017. doi:10.1016/j.xphs.2017.03.002. PMID 28302542.
- ↑ "Albumin thiol oxidation and serum protein carbonyl formation are progressively enhanced with advancing stages of chronic kidney disease". Clinical and Experimental Nephrology 13 (4): 308–315. August 2009. doi:10.1007/s10157-009-0161-y. PMID 19363646.
- ↑ "Microalbumin Urine Test". WebMD. http://www.webmd.com/hw/diabetes_1_2/tu6440.asp.
- ↑ "The major histocompatibility complex-related Fc receptor for IgG (FcRn) binds albumin and prolongs its lifespan". The Journal of Experimental Medicine 197 (3): 315–322. February 2003. doi:10.1084/jem.20021829. PMID 12566415.
- ↑ "Unraveling the mysteries of serum albumin-more than just a serum protein". Frontiers in Physiology 5: 299. 2014. doi:10.3389/fphys.2014.00299. PMID 25161624.
Further reading
- "The role of an amino acid triad at the entrance of the heme pocket in human serum albumin for O(2) and CO binding to iron protoporphyrin IX". Organic & Biomolecular Chemistry 7 (18): 3836–3841. September 2009. doi:10.1039/b909794e. PMID 19707690.
- "Human serum albumin inhibits Abeta fibrillization through a "monomer-competitor" mechanism". Biophysical Journal 97 (9): 2585–2594. November 2009. doi:10.1016/j.bpj.2009.08.028. PMID 19883602. Bibcode: 2009BpJ....97.2585M.
- "Influence of non-enzymatic post-translation modifications on the ability of human serum albumin to bind iron. Implications for non-transferrin-bound iron speciation". Biochimica et Biophysica Acta 1794 (10): 1449–1458. October 2009. doi:10.1016/j.bbapap.2009.06.003. PMID 19505594.
- "Multiple conformational state of human serum albumin around single tryptophan residue at various pH revealed by time-resolved fluorescence spectroscopy". Journal of Biochemistry 147 (2): 191–200. February 2010. doi:10.1093/jb/mvp175. PMID 19884191.
- "Structure, properties, and engineering of the major zinc binding site on human albumin". The Journal of Biological Chemistry 284 (34): 23116–23124. August 2009. doi:10.1074/jbc.M109.003459. PMID 19520864.
- "Influence of electrostatic interactions on the fibrillation process of human serum albumin". The Journal of Physical Chemistry B 113 (30): 10521–10529. July 2009. doi:10.1021/jp902224d. PMID 19572666.
- "[Advanced glycation end products induce expression of PAI-1 in cultured human proximal tubular epithelial cells through NADPH oxidase dependent pathway]". Xi Bao Yu Fen Zi Mian Yi Xue Za Zhi = Chinese Journal of Cellular and Molecular Immunology 25 (8): 674–677. August 2009. PMID 19664386.
- "Ibuprofen impairs allosterically peroxynitrite isomerization by ferric human serum heme-albumin". The Journal of Biological Chemistry 284 (45): 31006–31017. November 2009. doi:10.1074/jbc.M109.010736. PMID 19734142.
- "Defining the human deubiquitinating enzyme interaction landscape". Cell 138 (2): 389–403. July 2009. doi:10.1016/j.cell.2009.04.042. PMID 19615732.
- "Beyond expansion: structural studies on the transport roles of human serum albumin". Vox Sanguinis 83 (Suppl 1): 315–319. August 2002. doi:10.1111/j.1423-0410.2002.tb05326.x. PMID 12617161.
- "Structural basis of transport of lysophospholipids by human serum albumin". The Biochemical Journal 423 (1): 23–30. September 2009. doi:10.1042/BJ20090913. PMID 19601929.
- "Focus on microalbuminuria to improve cardiac and renal protection". Nephron Clinical Practice 111 (3): c204-10; discussion c211. 2009. doi:10.1159/000201568. PMID 19212124.
- "Dynamics of loop 1 of domain I in human serum albumin when dissolved in ionic liquids". The Journal of Physical Chemistry B 113 (38): 12825–12830. September 2009. doi:10.1021/jp904475v. PMID 19711930.
- "The antioxidant properties of serum albumin". FEBS Letters 582 (13): 1783–1787. June 2008. doi:10.1016/j.febslet.2008.04.057. PMID 18474236.
- "Identification of human plasma proteins as major clients for the extracellular chaperone clusterin". The Journal of Biological Chemistry 285 (6): 3532–3539. February 2010. doi:10.1074/jbc.M109.079566. PMID 19996109.
- "A study on the interaction between 5-Methyluridine and human serum albumin using fluorescence quenching method and molecular modeling". Journal of Molecular Modeling 16 (2): 255–262. February 2010. doi:10.1007/s00894-009-0548-4. PMID 19588173.
- "Albumin Benkovac (c.1175 A > G; p.Glu392Gly): a novel genetic variant of human serum albumin". Translational Research 155 (3): 118–119. March 2010. doi:10.1016/j.trsl.2009.10.001. PMID 20171595.
- "Exploration of human serum albumin binding sites by docking and molecular dynamics flexible ligand-protein interactions". Biopolymers 93 (2): 161–170. February 2010. doi:10.1002/bip.21314. PMID 19785033.
- "Ischemia-modified albumin reduction after coronary bypass surgery is associated with the cardioprotective efficacy of cold-blood cardioplegia enriched with N-acetylcysteine: a preliminary study". European Surgical Research 44 (1): 30–36. 2010. doi:10.1159/000262324. PMID 19955769.
- "Association of serum glycated albumin, C-reactive protein and ICAM-1 levels with diffuse coronary artery disease in patients with type 2 diabetes mellitus". Clinica Chimica Acta; International Journal of Clinical Chemistry 408 (1–2): 45–49. October 2009. doi:10.1016/j.cca.2009.07.003. PMID 19615354.
External links
- Human Albumin structure in the Protein data bank
- Human Serum Albumin on the Human Protein Reference Database
- Albumin binding prediction
- Albumin at Lab Tests Online
- Albumin: analyte monograph from the Association for Clinical Biochemistry and Laboratory Medicine
- Overview of all the structural information available in the PDB for UniProt: P02768 (Serum albumin) at the PDBe-KB.
 |