Medicine:Intrauterine device
| Intrauterine device | |
|---|---|
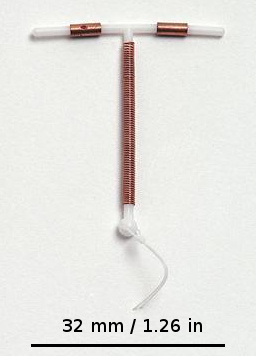 Copper IUD (Paragard T 380A) | |
| Background | |
| Type | Intrauterine |
| First use | 1800s[1] |
| Synonyms | Intrauterine system |
| Failure rates (first year) | |
| Perfect use | <1%[2] |
| Typical use | <1%[2] |
| Usage | |
| User reminders | None |
| Advantages and disadvantages | |
| STI protection | No |
| Periods | Depends on the type |
| Weight | No effect |
An intrauterine device (IUD), also known as an intrauterine contraceptive device (IUCD or ICD) or coil,[3] is a small, often T-shaped birth control device that is inserted into the uterus to prevent pregnancy. IUDs are a form of long-acting reversible contraception (LARC).[4]
The use of IUDs as a form of birth control dates from the 1800s.[1] A previous model known as the Dalkon shield was associated with an increased risk of pelvic inflammatory disease (PID). However, current models do not affect PID risk in women without sexually transmitted infections during the time of insertion.[5]
Although copper IUDs may increase menstrual bleeding and result in painful cramps,[6] hormonal IUDs may reduce menstrual bleeding or stop menstruation altogether.[7][8] However, women can have daily spotting for several months after insertion. It can take up to three months for there to be a 90% decrease in bleeding with hormonal IUDs.[9] Cramping can be treated with NSAIDs.[10] More serious potential complications include expulsion (2–5%), uterus perforation (less than 0.7%), and bladder perforation.[7][11][10] Levonorgestrel intrauterine devices (LNG-IUDs) may be associated with psychiatric symptoms such as depression, anxiety, and suicidal ideation, particularly in younger users. Evidence remains mixed, and further research is needed.[12] IUDs do not affect breastfeeding and can be inserted immediately after delivery.[7] They may also be used immediately after an abortion.[13][14]
IUDs are safe and effective in adolescents as well as those who have not previously had children.[15][16] Once an IUD is removed, even after long-term use, fertility returns to normal rapidly.[17] Copper devices have a failure rate of about 0.8%, while hormonal (levonorgestrel) devices fail about 0.2% of the time within the first year of use.[18] In comparison, male sterilization and male condoms have a failure rate of about 0.15% and 15%, respectively.[19] Copper IUDs can also be used as emergency contraception within five days of unprotected sex.[20] Globally, 14.3% of women of reproductive age and 22.8% of women using contraception use intrauterine contraception according to 2011 data,[21] with high variance in use rates among different countries, such as 34.1% of women in China in 2017.[22] Among birth control methods, IUDs, along with other contraceptive implants, result in the greatest satisfaction among users.[15]
History
The history of intrauterine devices dates back to the early 20th century. Unlike modern intrauterine devices, early interuterine (from Latin inter-, meaning "between", as opposed to intra-) devices crossed both the vagina and the uterus, causing a high rate of pelvic inflammatory disease. The first IUD was developed in 1909 by the German physician Richard Richter of Waldenburg. His device was made of silkworm gut and was not widely used.[23]
Ernst Gräfenberg, another German physician (after whom the G-spot is named), created the first Ring IUD, Gräfenberg's ring, made of silver filaments. His work was suppressed during the Nazi regime, when contraception was considered a threat to Aryan women.[23] He moved to the United States, where his colleagues H. Hall and M. Stone took up his work after his death and created the stainless steel Hall-Stone Ring. A Japanese doctor named Tenrei Ota also developed a silver or gold IUD called the Precea ring () or Ōta ring.[23]
Jack Lippes helped begin the increase of IUD use in the United States in the late 1950s. In this time, thermoplastics, which can bend for insertion and retain their original shape, became the material used for first-generation IUDs. Lippes also devised the addition of the monofilament nylon string, which facilitates IUD removal. His trapezoid-shaped Lippes Loop IUD became one of the most popular first-generation IUDs. In the following years, many different-shaped plastic IUDs were invented and marketed.[23] These included the infamous Dalkon Shield, whose poor design caused bacterial infection and led to thousands of lawsuits. Although the Dalkon shield was removed from the market, it had a lasting, negative impact on IUD use and reputation in the United States.[24] Lazar C. Margulies developed the first plastic IUD using thermoplastics in the 1960s.[25] His innovation allowed insertion of the IUD into the uterus without the need to dilate the cervix.[26]
The invention of the copper IUD in the 1960s brought with it the capital T-shaped design used by most modern IUDs. U.S. physician Howard Tatum determined that the 'T' shape would work better with the shape of the uterus, which forms a 'T' when contracted. He predicted this would reduce rates of IUD expulsion.[23] Together, Tatum and Chilean physician Jaime Zipper discovered that copper could be an effective spermicide and developed the first copper IUD, TCu200. Improvements by Tatum led to the creation of the TCu380A (ParaGard), which is currently the preferred copper IUD.[23]
The hormonal IUD was also invented in the 1960s and 1970s; initially, the goal was to mitigate the increased menstrual bleeding associated with copper and inert IUDs. The first model, Progestasert, was conceived by Antonio Scommegna and created by Tapani J. V. Luukkainen. The device only lasted for one year of use,[24] due to this it was discontinued.[27] One commercial hormonal IUD which is currently available, Mirena, was also developed by Luukkainen and released in 1976.[23] The manufacturer of the Mirena, Bayer AG, became the target of multiple lawsuits over allegations that Bayer failed to adequately warn users that the IUD could pierce the uterus and migrate to other parts of the body.[28]
China
In China, the use of IUDs by state health services was part of the government's efforts to limit birth rates. From 1980 to 2014, 324 million women were inserted with IUDs, in addition to the 107 million who had tubal ligation. Women who refused could lose their government employment. Their children could lose access to public schools. The IUDs inserted in this way were modified such that they could not be removed in a doctor's office (meant to be left indefinitely), and surgical removal is usually needed.[29] Until the mid-1990s, the state-preferred IUD was a stainless steel ring,[30][31] which had a higher rate of complications compared to other types of IUD. It gave rise to the idiom 上环; shànghuán, meaning "insert a loop". Nowadays, the IUDs include T and V shapes, the former being the most common and easiest to remove.
To implement the two-child policy, the government announced that IUD removals would be paid for by the government.[29] IUD removals are free for women "who are allowed to have another child" (see one-child policy) or "who cannot continue to have the IUD for health reasons."[32]
Mechanism

The main mechanisms of action of IUDs occur before fertilization, by preventing sperm from ever reaching the egg.[33]
The copper-bearing IUD acts as a spermicide, killing or impairing sperm so they cannot reach the egg. Copper IUDs do not contain any hormones, but release copper ions, which are toxic to sperm. They also cause the uterus and fallopian tubes to produce a fluid that contains white blood cells, copper ions, enzymes, and prostaglandins, which is also toxic to sperm.[34] The very high effectiveness of copper-containing IUDs as emergency contraceptives implies they may also act by preventing implantation of the blastocyst.[35][36]
The progestogen released from hormonal IUDs mainly works by thickening the cervical mucus, preventing sperm from reaching the fallopian tubes. Hormonal IUDs may also sometimes prevent ovulation.[34][37]
Types
The types of intrauterine devices available, and the names they go by, differ by location. In the United States, there are two types available:[38]
- Nonhormonal: Copper-containing IUD (ParaGard and others)
- Hormonal: Progestogen-releasing IUD (Mirena and others)
The WHO ATC labels both copper and hormonal devices as IUDs. In the United Kingdom, there are more than 10 different types of copper IUDs available. In the United Kingdom, the term IUD refers only to these copper devices. Hormonal intrauterine contraception is labeled with the term intrauterine system (IUS).[39][40]
| Copper[41] | Mirena[42] | Skyla[43] | Liletta[44] | Kyleena[45] | |
|---|---|---|---|---|---|
| Hormone (total in device) | None | 52 mg
levonorgestrel |
13.5 mg
levonorgestrel |
52 mg
levonorgestrel |
19.5 mg levonorgestrel |
| Initial amount released | None | 20 μg/day | 14 μg/day | 18.6 μg/day | 16 μg/day |
| Approved effectiveness | 10 years (12 years) | 5 years (10 years) | 3 years | 3 years (5 years) | 5 years |
| Mechanism of action | Copper toxic to sperm | -Levonorgestrel thickens cervical mucus to prevent sperm from reaching egg
-Prevents ovulation at times | |||
| Advantages among IUDs | -No hormones
-Emergency contraception |
-Various hormone level options
-Lighter periods after 3 months; some users experience amenorrhea | |||
| Disadvantages among IUDs | Heavier menstrual flow and cramps | Ovarian cysts (although they can be asymptomatic) | |||
Non-hormonal
Copper


Most copper IUDs have a T-shaped frame that is wound around with pure electrolytic copper wire and/or have copper collars (sleeves). The arms of the frame hold the IUD in place near the top of the uterus. The Paragard TCu 380a measures 32 mm (1.26") horizontally (top of the T), and 36 mm (1.42") vertically (leg of the T). Copper IUDs have a first-year failure rate ranging from 0.1 to 2.2%.[46] They work by damaging sperm and disrupting their motility so that they are not able to fertilize an egg. Specifically, copper acts as a spermicide within the uterus by increasing levels of copper ions, prostaglandins, and white blood cells within the uterine and tubal fluids.[6][47] The increased copper ions in the cervical mucus inhibit the sperm's motility and viability, preventing sperm from traveling through the cervical mucus, or destroying it as it passes through.[48] Copper can also alter the endometrial lining, and while studies show that this alteration can prevent implantation of a fertilized egg ("blastocyst"), it cannot disrupt one that has already been implanted.[49]
Advantages of the copper IUD include its ability to provide emergency contraception up to five days after unprotected sex. It is the most effective form of emergency contraception available.[50] It works by preventing fertilization or implantation but does not affect already implanted embryos.[49] It contains no hormones, so it can be used while breastfeeding, and fertility returns quickly after removal.[51] Copper IUDs also last longer and are available in a wider range of sizes and shapes than hormonal IUDs.[9] Disadvantages include the possibility of heavier menstrual periods and more painful cramps.[6]
IUDs that contain gold or silver also exist.[39][52] Other shapes of IUD include the so-called U-shaped IUDs, such as the Load and Multiload, and the frameless IUD that holds several hollow cylindrical minuscule copper beads. It is held in place by a suture (knot) to the fundus of the uterus. It is mainly available in China and Europe. A framed copper IUD called the IUB SCu300 coils, when deployed and forms a three-dimensional spherical shape. It is based on a nickel titanium shape memory alloy core.[53] In addition to copper, noble metal, and progestogen IUDs, women in China can get copper IUDs with indomethacin. This non-hormonal compound reduces the severity of menstrual bleeding, and these coils are popular.[54]
Inert
Inert IUDs do not have a bioactive component. They are made of inert materials like stainless steel (such as the stainless steel ring (SSR), a flexible ring of steel coils that can deform to be inserted through the cervix) or plastic (such as the Lippes Loop, which can be inserted through the cervix in a cannula and takes a trapezoidal shape within the uterus). They are less effective than copper or hormonal IUDs, with a side effect profile similar to copper IUDs. Their primary mechanism of action is inducing a local foreign body reaction, which makes the uterine environment hostile both to sperm and to implantation of an embryo.[48] They may have higher rates of preventing pregnancy after fertilization, instead of before fertilization, compared to copper or hormonal IUDs.[55]
Inert IUDs are not yet approved for use in the United States, UK, or Canada. In China, where IUDs are the most common form of contraception, copper IUD production replaced inert IUD production in 1993.[56] However, as of 2008, the most common IUD used by immigrants presenting to Canadian clinics for removal of IUDs placed in China was still the SSR. Because the SSR has no string for removal, it can present a challenge to healthcare providers unfamiliar with IUD types not available in their region.[57]
Hormonal

Hormonal IUDs (referred to as intrauterine systems in the UK) work by releasing a small amount of levonorgestrel, a progestin. Each type varies in size, amount of levonorgestrel released, and duration. The primary mechanism of action is making the inside of the uterus uninhabitable for sperm.[58] They can also thin the endometrial lining and potentially impair implantation, but this is not their usual function.[59][60] Because they thin the endometrial lining, they can also reduce or even prevent menstrual bleeding. As a result, they are used to treat menorrhagia (heavy menses), once pathologic causes of menorrhagia (such as uterine polyps) have been ruled out.[61] In a 10-year study, the levonorgestrel coil was found to be as effective as oral medicines (tranexamic acid, mefenamic acid, combined oestrogen–progestogen or progesterone alone); the same proportion of women had not had surgery for heavy bleeding and had similar improvements in their quality of life.[62][63]
The progestin released by hormonal IUDs primarily acts locally; use of Mirena results in much lower systemic progestin levels than other very-low-dose progestogen only contraceptives.[64]
Insertion and removal

It is difficult to predict what a woman will experience during IUD insertion or removal. Some women describe the insertion as cramps, some as a pinch, and others do not feel anything. Only 9% of nulliparous women considered the procedure painless, 72% moderately painful, and 17% experienced substantial pain with insertion that needed active management.[65] Approximately 11% of parous women feel similar pain.[66] In such cases, NSAIDs can be effective when given in response to post-insertion pain, but have no significant effect when given prophylactically.[66] Topical lidocaine is an effective pain management drug when applied before the procedure.[67] The use of intrauterine lidocaine (paracervical block) is underutilized in the United States as an effective method to reduce pain associated with insertion.[68]
IUD insertion can occur at multiple timepoints in a woman's reproductive lifespan:
- interval insertion, the most common, occurs remote from pregnancy;
- post-abortion or post-miscarriage insertion occurs following an abortion or miscarriage when the uterus is known to be empty;
- postpartum insertion occurs after a woman gives birth either immediately, while the woman is still in the hospital, or delayed, up to 6 weeks following delivery, following either vaginal delivery or cesarean delivery. Insertion timing changes the risk of IUD expulsion.[69][70][71][72][73]
Procedure
During the insertion procedure, health care providers use a speculum to find the cervix (the opening to the uterus), pinch the cervix to stabilize it open with a tenaculum,[74] and then use an insertion device to place the IUD in the uterus. The insertion device goes through the cervix. The procedure itself, if uncomplicated, should take no more than five to ten minutes.[75]
A suction cervical stabilizer can be used in place of the standard tenaculum to hold the cervix open during the IUD insertion procedure.[76] Suction cervical stabilizers, such as The Carevix™ Suction Cervical Stabilizer,[77] may reduce pain associated with the insertion procedure.[78]
For immediate postpartum insertion, the IUD is inserted following the removal of the placenta from the uterus. The uterus is larger than baseline following birth, which has important implications for insertion. After vaginal deliveries, insertions can be done using placental forceps, a longer inserter specialized for postpartum insertions, or manually, where the provider uses their hand to insert the IUD in the uterus. After cesarean deliveries, the IUD is placed in the uterus with forceps or manually during surgery prior to suturing the uterine incision.[73][70][79]
Generally, the removal is uncomplicated and reported to be not as painful as the insertion because no instrument needs to go through the cervix.[80] This process requires the health care provider to find the cervix with a speculum and then use ring forceps, which only go into the vagina, to grasp the IUD strings and then pull the IUD out.
Manufacturers and other training facilities can teach IUD placement and removal.[81]
Adverse effects
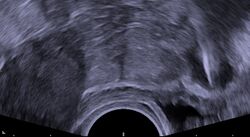
Regardless of the IUD type, some potential side effects are similar for all IUDs. Some of these side effects include bleeding pattern changes, expulsion, and pelvic inflammatory disease (especially in the first 21 days after insertion). The occurrence of IUD migration is rare, with reported rates in medical literature varying between 0.1% and 0.9%. However, when migration occurs, it can lead to serious complications such as uterine perforation and, in rare cases, bladder perforation. Bladder perforation, while uncommon (affecting only 2% of displaced IUDs), can result in symptoms like urinary frequency, hematuria, and stone formation, often necessitating surgical intervention for removal.[82] Regular monitoring and imaging, such as ultrasound or CT scans, are recommended to detect such complications early and ensure timely treatment. A small probability of pregnancy remains after IUD insertion, and when it occurs, there is a greater risk of ectopic pregnancy.[83]
IUDs with progestogen confer an increased risk of ovarian cysts,[84] and IUDs with copper confer an increased risk of heavier periods. Mirena lists common (less than 1 in 10 women) side effects as including ovarian cysts, painful periods, increased vaginal discharge, headaches and depression. More than 1 in 10 women experience light, infrequent or absent periods or spotting.[85][86]
Menstrual cup companies recommend that women with IUDs who are considering using menstrual cups should consult with their gynecologists before use. There have been rare cases in which women using IUDs dislodged them when removing their menstrual cups, however, this can also happen with tampon use.[87] Despite reports, as of 2023, there is no scientific agreement on whether using a menstrual cup increases the risk of IUD expulsion; more rigorous studies are needed.[88]
Unlike condoms, the IUD does not protect against sexually transmitted infections.[89]
Modern IUDs do not lead to infertility or make it harder for a woman to become pregnant, and fertility typically returns within days of removal. Some prior studies found an association between infertility and the Dalkon Shield, an early IUD design which is no longer available.[90]
Modern IUDs do not cause increased infection, though the earlier Dalkon Shield may have, because it contained multifilament strings, which provided bacteria a space to grow and move up the string. IUDs manufactured after 2008 use monofilament strings to prevent this from happening.[91] However, as with any medical intervention, IUDs can lead to increased risk of infection immediately after the insertion.
According to the U.S. Medical Eligibility Criteria for Contraceptive Use, published by the CDC, women and adolescents under the age of 20 and women who have not given birth are classified in category 2 for IUD use, mainly due to "the risk for expulsion from nulliparity and STIs from sexual behavior in younger age groups." According to the CDC, benefits generally outweigh the risks, and IUDs are recommended for young and nulliparous women, although more careful attention may be required. Women over age 20 and those who have previously given birth are placed in category 1, meaning no special concerns are placed on use.[92][93]
Some women experience amenorrhea, or lack of menstruation, while using an IUD. Menstruation occurs when a woman has not become pregnant and the uterus sheds its lining in preparation for the next cycle. IUDs tend to thin the lining of the uterus, leading to less menses by volume or a lack of menstruation altogether. There is a condition known as polycystic ovarian syndrome (PCOS) which causes women to miss their periods and can lead to an increased risk of endometrial cancer.[94] However, an IUD causes the endometrial lining of a uterus to thin, which is the opposite of what occurs with PCOS.
Levonorgestrel intrauterine devices (LNG-IUDs) have been associated with psychiatric symptoms, including depression, anxiety, and suicidal ideation, particularly in adolescents and young women, though evidence remains mixed. Some studies report increased depressive symptoms and anxiety, potentially linked to the sensitization of the hypothalamic-pituitary-adrenal (HPA) axis and elevated cortisol levels. Others find no association or even reduced symptoms.[12]
Prevalence and popularity
Globally, 14.3% of married or partnered women of reproductive age (15–49) use intrauterine contraception as their preferred method of family planning. And a study found that female family planning providers choose LARC methods more often (41.7%) than the general public (12.1%).[95] However, the adoption of IUC varies significantly across different regions. In Asia, IUC is particularly popular, with 27% of contraceptive users relying on it, while in Oceania, the usage rate is much lower at 1.8%. Geographically, the majority of IUC users—over 80% worldwide—are concentrated in Asia, with nearly two-thirds (64%) of these users living in China, according to a 2011 United Nations review.[21]
IUC use is more prevalent in less developed regions (15.1% of women) compared to more developed regions (9.2% of women). Within continents, there are significant variations. For instance, in Europe, IUC usage ranges from 5% in Southern Europe to 16–28% in countries like France and Scandinavia. In Africa, IUC use is relatively low in sub-Saharan regions (less than 2%) but higher in Northern Africa, particularly in countries such as Egypt (36.1%) and Tunisia (27.8%).[21] In the United States, the use of IUDs increased from 0.8% in 1995 to 7.2% from the period of 2006 to 2014[96][97] and to 10.5% in a 2017-2019 survey.[22] IUC usage rates are also influenced by ethnicity within the United States, with Hispanic women more likely to use IUC compared to Caucasian women.[21]
Among birth control methods, IUDs, along with other contraceptive implants, result in the greatest satisfaction among users.[15]
Cost
In the United States, intrauterine devices (IUDs) typically cost between $0 and $1,300, with prices covering medical exams, insertion, and follow-up visits.[98] Under the Affordable Care Act, most insurance plans must cover all FDA-approved birth control methods, including IUDs. Coverage for specific brands may vary.[99]
References
- ↑ 1.0 1.1 (in en) Blueprints Obstetrics and Gynecology. Lippincott Williams & Wilkins. 2013. p. 320. ISBN 978-1-4511-1702-8. https://books.google.com/books?id=eKC1B3BhlxUC&pg=PA320.
- ↑ 2.0 2.1 "ParaGard (copper IUD)". 7 September 2019. https://www.drugs.com/mcp/paragard-copper-iud.
- ↑ "IUD (intrauterine device)". Contraception guide. NHS Choices. http://www.nhs.uk/Conditions/contraception-guide/Pages/iud-coil.aspx. "the intrauterine device, or IUD (sometimes called a coil)"
- ↑ "Effectiveness of long-acting reversible contraception". The New England Journal of Medicine 366 (21): 1998–2007. May 2012. doi:10.1056/NEJMoa1110855. PMID 22621627.
- ↑ "Popularity Disparity: Attitudes About the IUD in Europe and the United States". Guttmacher Policy Review. Guttmacher Institute. Fall 2007. http://www.guttmacher.org/pubs/gpr/10/4/gpr100419.html.
- ↑ 6.0 6.1 6.2 "Intrauterine Devices (IUDs)". Contraceptive Technology. 2007.
- ↑ 7.0 7.1 7.2 Obstetrics: Normal and Problem Pregnancies. Elsevier Health Sciences. 2012. p. 527. ISBN 978-1-4557-3395-8. https://books.google.com/books?id=x3mJpT2PkEUC&pg=PA527.
- ↑ Gemzell-Danielsson, Kristina; Kubba, Ali; Caetano, Cecilia; Faustmann, Thomas; Lukkari-Lax, Eeva; Heikinheimo, Oskari (23 Feb 2021). "Thirty years of mirena: A story of innovation and change in women's healthcare". Acta Obstetricia et Gynecologica Scandinavica 100 (4): 614–618. doi:10.1111/aogs.14110. ISSN 1600-0412. PMID 33544887.
- ↑ 9.0 9.1 (in en) Contraception. John Wiley & Sons. 2011. p. 96. ISBN 978-1-4443-4263-5. https://books.google.com/books?id=ksjJcx1CeKcC&pg=PA96.
- ↑ 10.0 10.1 "Current issues in contraception". Mayo Clinic Proceedings 88 (3): 295–299. March 2013. doi:10.1016/j.mayocp.2013.01.007. PMID 23489454.
- ↑ Liu, Guangtao; Li, Feifei; Ao, Min; Huang, Guimin (2021-08-16). "Intrauterine devices migrated into the bladder: two case reports and literature review" (in en). BMC Women's Health 21 (1): 301. doi:10.1186/s12905-021-01443-w. ISSN 1472-6874. PMID 34399735.
- ↑ 12.0 12.1 Elsayed, Mohamed; Dardeer, Khaled T.; Khehra, Nimrat; Padda, Inderbir; Graf, Heiko; Soliman, Amr; Makram, Abdelrahman M.; Zeiss, René et al. (2023-07-03). "The potential association between psychiatric symptoms and the use of levonorgestrel intrauterine devices (LNG-IUDs): A systematic review". The World Journal of Biological Psychiatry 24 (6): 457–475. doi:10.1080/15622975.2022.2145354. ISSN 1562-2975. PMID 36426589.
- ↑ "Intrauterine contraceptive insertion postabortion: a systematic review". Contraception 84 (5): 447–464. November 2011. doi:10.1016/j.contraception.2011.03.007. PMID 22018119. https://zenodo.org/record/1258857.
- ↑ "Society of Family Planning clinical recommendations: contraception after surgical abortion". Contraception 99 (1): 2–9. January 2019. doi:10.1016/j.contraception.2018.08.016. PMID 30195718.
- ↑ 15.0 15.1 15.2 "Committee opinion no. 539: adolescents and long-acting reversible contraception: implants and intrauterine devices". Obstetrics and Gynecology 120 (4): 983–988. October 2012. doi:10.1097/AOG.0b013e3182723b7d. PMID 22996129.
- ↑ "A review of barriers and myths preventing the more widespread use of intrauterine contraception in nulliparous women". The European Journal of Contraception & Reproductive Health Care 17 (5): 340–350. October 2012. doi:10.3109/13625187.2012.700744. PMID 22834648.
- ↑ Clinical reproductive medicine and surgery. Philadelphia: Mosby. 2007. p. 409. ISBN 978-0-323-03309-1. https://books.google.com/books?id=fOPtaEIKvcIC&pg=PA409.
- ↑ The Johns Hopkins manual of gynecology and obstetrics. (4th ed.). Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins. 2012-03-28. p. 232. ISBN 978-1-60547-433-5. https://books.google.com/books?id=4Sg5sXyiBvkC&pg=PR232.
- ↑ "Contraception Editorial January 2008: Reducing Unintended Pregnancy in the United States". January 2008. http://www.arhp.org/Publications-and-Resources/Contraception-Journal/January-2008.
- ↑ "Emergency Contraception - ACOG". https://www.acog.org/Clinical-Guidance-and-Publications/Practice-Bulletins/Committee-on-Practice-Bulletins-Gynecology/Emergency-Contraception.
- ↑ 21.0 21.1 21.2 21.3 Buhling, Kai J.; Zite, Nikki B.; Lotke, Pamela; Black, Kirsten (2014-03-01). "Worldwide use of intrauterine contraception: a review". Contraception 89 (3): 162–173. doi:10.1016/j.contraception.2013.11.011. ISSN 0010-7824. PMID 24369300.
- ↑ 22.0 22.1 Kamiya, Yumiko; Molitoris, Joseph; Roldán, Rocío Peinador; Zhang, Guangyu (April 2024). "World Contraceptive Use 2024". United Nations Department of Economic and Social Affairs, Population Division. https://www.un.org/development/desa/pd/data/world-contraceptive-use.
- ↑ 23.0 23.1 23.2 23.3 23.4 23.5 23.6 "Pioneers of the intrauterine device". The European Journal of Contraception & Reproductive Health Care 2 (1): 15–23. March 1997. doi:10.1080/13625189709049930. PMID 9678105. http://www.contrel.be/Articles%20and%20videos/Pioneers%20of%20the%20intrauterine%20device.pdf.
- ↑ 24.0 24.1 "Intrauterine contraception: from silver ring to intrauterine contraceptive implant". European Journal of Obstetrics, Gynecology, and Reproductive Biology 90 (2): 145–152. June 2000. doi:10.1016/s0301-2115(00)00262-1. PMID 10825633.
- ↑ "Pioneers of the intrauterine device". The European Journal of Contraception & Reproductive Health Care 2 (1): 15–23. March 1997. doi:10.1080/13625189709049930. PMID 9678105. http://www.contrel.be/Articles%20and%20videos/Pioneers%20of%20the%20intrauterine%20device.pdf. Retrieved 24 March 2016.
- ↑ The Birth Control Movement and American Society: From Private Vice to Public Virtue. Princeton University Press. 1984. p. 306. ISBN 978-1-4008-5659-6. https://books.google.com/books?id=aNn_AwAAQBAJ&q=%22Lazar%20C.%20Margulies%22&pg=PA306.
- ↑ Bürger, Zoé; Bucher, Anna Magdalena; Comasco, Erika; Henes, Melanie; Hübner, Stephanie; Kogler, Lydia; Derntl, Birgit (2021-10-01). "Association of levonorgestrel intrauterine devices with stress reactivity, mental health, quality of life and sexual functioning: A systematic review". Frontiers in Neuroendocrinology 63. doi:10.1016/j.yfrne.2021.100943. ISSN 0091-3022. PMID 34425187. https://www.sciencedirect.com/science/article/pii/S0091302221000455.
- ↑ "Legal Current Events | Westlaw Practitioner Insights". http://newsandinsight.thomsonreuters.com/Legal/News/2013/05_-_May/Judge_calls_for_female_lawyers_on_plaintiffs__committee_in_Mirena_MDL/.
- ↑ 29.0 29.1 "After One-Child Policy, Outrage at China's Offer to Remove IUDs". The New York Times. 7 January 2017. https://www.nytimes.com/2017/01/07/world/asia/after-one-child-policy-outrage-at-chinas-offer-to-remove-iuds.html.
- ↑ "Chinese ring". July 14, 2011. http://www.obgyn.net/obgyn-ultrasound/chinese-ring.
- ↑ "Intrauterine Devices (IUDs)". https://www.fhi360.org/sites/default/files/webpages/Modules/IUD/s1pg6.htm.
- ↑ "One Child Policy Leaves Millions of Chinese Women With Unwanted IUDs" (in en). January 13, 2017. http://www.rfa.org/english/women/onechild-iud-01132017173100.html.
- ↑ "Myths and facts about... the Intra-Uterine Device (IUD)" (in en). 2012-02-17. https://www.ippf.org/blogs/myths-and-facts-about-intra-uterine-devices.
- ↑ 34.0 34.1 "Understanding the IUD | Center for Research". National Center For Health Research. 15 July 2013. http://center4research.org/medical-care-for-adults/birth-control/understanding-the-iud/.
- ↑ "Emergency contraception". Contraceptive technology (20th revised ed.). New York: Ardent Media. 2011. pp. 113–145. ISBN 978-1-59708-004-0. OCLC 781956734. p. 121:
Mechanism of action
Copper-releasing IUCs
When used as a regular or emergency method of contraception, copper-releasing IUCs act primarily to prevent fertilization. Emergency insertion of a copper IUC is significantly more effective than the use of ECPs, reducing the risk of pregnancy following unprotected intercourse by more than 99%.2,3 This very high level of effectiveness implies that emergency insertion of a copper IUC must prevent some pregnancies after fertilization.
Emergency contraceptive pills
To make an informed choice, women must know that ECPs—like the birth control pill, patch, ring, shot, and implant,76and even like breastfeeding77—prevent pregnancy primarily by delaying or inhibiting ovulation and inhibiting fertilization, but may at times inhibit implantation of a fertilized egg in the endometrium. However, women should also be informed that the best available evidence indicates that ECPs prevent pregnancy by mechanisms that do not involve interference with post-fertilization events.
ECPs do not cause abortion78 or harm an established pregnancy. Pregnancy begins with implantation according to medical authorities such as the US FDA, the National Institutes of Health79 and the American College of Obstetricians and Gynecologists (ACOG).80
Ulipristal acetate (UPA). One study has demonstrated that UP can delay ovulation.81... Another study found that UPA altered the endometrium, but whether this change would inhibit implantation is unknown.82
p. 122:
Progestin-only emergency contraceptive pills. Early treatment with ECPs containing only the progestin levonorgestrel has been shown to impair the ovulatory process and luteal function.83–87
p. 123:
Combined emergency contraceptive pills. Several clinical studies have shown that combined ECPs containing ethinyl estradiol and levonorgestrel can inhibit or delay ovulation.107–110 - ↑ RCOG Faculty of Sexual; Reproductive Healthcare; Clinical Effectiveness Unit (January 2012). "Clinical guidance: emergency contraception". Clinical Guidance (London: Royal College of Obstetricians and Gynaecologists). ISSN 1755-103X. http://www.fsrh.org/pdfs/CEUguidanceEmergencyContraception11.pdf. Retrieved 2012-04-30.p.3:
How does EC work?
In 2002, a judicial review ruled that pregnancy begins at implantation, not fertilisation.8 The possible mechanisms of action should be explained to the patient, as some methods may not be acceptable, depending on individual beliefs about the onset of pregnancy and abortion.
Copper-bearing intrauterine device (Cu-IUD). Copper is toxic to the ovum and sperm, and thus the copper-bearing intrauterine device (Cu-IUD) is effective immediately after insertion and works primarily by inhibiting fertilisation.9–11 A systematic review on the mechanisms of action of IUDs showed that both pre- and post-fertilization effects contribute to efficacy.11If fertilisation has already occurred, it is accepted that there is an anti-implantation effect,12,13
Levonorgestrel (LNG). The precise mode of action of levonorgestrel (LNG) is incompletely understood, but it is thought to work primarily by inhibition of ovulation.16,17
Ulipristal acetate (UPA). UPA's primary mechanism of action is thought to be inhibition or delay of ovulation.2 - ↑ "Mirena (DIU hormonal) - Mayo Clinic". http://www.mayoclinic.org/tests-procedures/mirena/basics/definition/prc-20012867.
- ↑ "IUDs--an update". Population Reports. Series B, Intrauterine Devices (6): 1–35. December 1995. PMID 8724322. http://www.infoforhealth.org/pr/b6/b6.pdf. Retrieved 2006-01-01.
- ↑ 39.0 39.1 "Contraceptive coils (IUDs)". NetDoctor.co.uk. 2006. http://www.netdoctor.co.uk/sex_relationships/facts/contraceptivecoil.htm.
- ↑ "Hormonally impregnated intrauterine systems (IUSs) versus other forms of reversible contraceptives as effective methods of preventing pregnancy". The Cochrane Database of Systematic Reviews 2004 (3). 2004. doi:10.1002/14651858.CD001776.pub2. PMID 15266453.
- ↑ "ParaGard intrauterine copper contraceptive". https://www.paragard.com/pdf/PARAGARD-PI.pdf#page=4.
- ↑ "Mirena: Levonorgestrel-releasing intrauterine system". https://www.accessdata.fda.gov/drugsatfda_docs/label/2008/021225s019lbl.pdf.
- ↑ "Syla: levonorgestrel-releasing intrauterine system". https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/203159s007lbl.pdf.
- ↑ "Liletta: levonorgestrel-releasing intrauterine system". https://www.fda.gov/downloads/drugs/developmentapprovalprocess/developmentresources/ucm446653.pdf.
- ↑ "Kyleena: Levonorgestrel-releasing intrauterine system". https://www.accessdata.fda.gov/drugsatfda_docs/nda/2016/208224Orig1s000SumR.pdf.
- ↑ "Copper containing, framed intra-uterine devices for contraception". The Cochrane Database of Systematic Reviews (4). October 2007. doi:10.1002/14651858.CD005347.PUB3. PMID 17943851.
- ↑ "Mechanisms of the Contraceptive Action of Hormonal Methods and Intrauterine Devices (IUDs)". Family Health International. 2006. http://www.fhi.org/en/RH/Pubs/booksReports/methodaction.htm.
- ↑ 48.0 48.1 "Copper-T intrauterine device and levonorgestrel intrauterine system: biological bases of their mechanism of action". Contraception 75 (6 Suppl): S16–S30. June 2007. doi:10.1016/j.contraception.2007.01.020. PMID 17531610.
- ↑ 49.0 49.1 "Facts are Important: Emergency Contraception (EC) and Intrauterine Devices (IUDs) are Not Abortifacients" (PDF). American Congress of Obstetricians and Gynecologists. June 12, 2014. http://www.acog.org/-/media/Departments/Government-Relations-and-Outreach/FactsAreImportantEC.pdf?dmc=1&ts=20150127T1149330103. "Copper ions released from the IUD create an environment that is toxic to sperm, preventing fertilization.14 Copper can also alter the endometrial lining, but studies show that this alteration can prevent implantation, but not disrupt implantation"
- ↑ "The efficacy of intrauterine devices for emergency contraception: a systematic review of 35 years of experience". Human Reproduction 27 (7): 1994–2000. July 2012. doi:10.1093/humrep/des140. PMID 22570193.
- ↑ "Recovery of fertility after use of the levonorgestrel 20 mcg/d or Copper T 380 Ag intrauterine device". Contraception 34 (3): 261–267. September 1986. doi:10.1016/0010-7824(86)90007-7. PMID 3098498.
- ↑ Schering (May 13, 2003). "Nova T380 Patient information leaflet (PIL)". http://emc.medicines.org.uk/emc/assets/c/html/displaydoc.asp?documentid=3641.
- ↑ "The IUB, a newly invented IUD: a brief report". Contraception 89 (2): 139–141. February 2014. doi:10.1016/j.contraception.2013.10.017. PMID 24309220.
- ↑ "[A multi-center randomized controlled trial of intrauterine device use in Chinese women]" (in zh). Zhonghua Yi Xue Za Zhi 91 (45): 3172–3175. December 2011. PMID 22333096.
- ↑ ESHRE Capri Workshop Group (April 2008). "Intrauterine devices and intrauterine systems". Human Reproduction Update 14 (3): 197–208. doi:10.1093/humupd/dmn003. PMID 18400840.
- ↑ "Chinese experience with intrauterine devices". Contraception 75 (6 Suppl): S31–S34. June 2007. doi:10.1016/j.contraception.2006.12.007. PMID 17531613.
- ↑ "A 10-year experience in removing Chinese intrauterine devices". International Journal of Gynaecology and Obstetrics 109 (3): 219–222. June 2010. doi:10.1016/j.ijgo.2009.12.018. PMID 20219193.
- ↑ "Intrauterine contraception". A clinical guide for contraception (5th ed.). Philadelphia: Lippincott Williams & Wilkins. 2011. pp. 239–280. ISBN 978-1-60831-610-6. pp. 246–247:
Mechanism of action
The contraceptive action of all IUDs is mainly in the intrauterine cavity. Ovulation is not affected, and the IUD is not an abortifacient.58–60 It is currently believed that the mechanism of action for IUDs is the production of an intrauterine environment that is spermicidal.
Nonmedicated IUDs depend for contraception on the general reaction of the uterus to a foreign body. It is believed that this reaction, a sterile inflammatory response, produces tissue injury of a minor degree but sufficient to be spermicidal. Very few, if any, sperm reach the ovum in the fallopian tube.
The progestin-releasing IUD adds the endometrial action of the progestin to the foreign body reaction. The endometrium becomes decidualized with atrophy of the glands.65 The progestin IUD probably has two mechanisms of action: inhibition of implantation and inhibition of sperm capacitation, penetration, and survival. - ↑ ESHRE Capri Workshop Group (2008). "Intrauterine devices and intrauterine systems". Human Reproduction Update 14 (3): 197–208. doi:10.1093/humupd/dmn003. PMID 18400840. "Both copper IUDs and levonorgestrel releasing IUSs may interfere with implantation".
- ↑ Contraceptive technology (20th rev. ed.). [New York, N.Y.]: Ardent Media. 2011. p. 162. ISBN 978-1-59708-004-0. "Although the precise mechanism of action is not known, currently available IUCs work primarily by preventing sperm from fertilizing ova.26 IUCs are not abortifacients: they do not interrupt an implanted pregnancy.27 Pregnancy is prevented by a combination of the "foreign body effect" of the plastic or metal frame and the specific action of the medication (copper or levonorgestrel) that is released. Exposure to a foreign body causes a sterile inflammatory reaction in the intrauterine environment that is toxic to sperm and ova and impairs implantation.28,29 The production of cytotoxic peptides and activation of enzymes lead to inhibition of sperm motility, reduced sperm capacitation and survival, and increased phagocytosis of sperm.30,31… The progestin in the LNg IUC enhances the contraceptive action of the device by thickening cervical mucus, suppressing the endometrium, and impairing sperm function. In addition, ovulation is often impaired as a result of systemic absorption of levonorgestrel"
- ↑ "Levonorgestrel-releasing intrauterine system: uses and controversies". Expert Review of Medical Devices 5 (4): 437–445. July 2008. doi:10.1586/17434440.5.4.437. PMID 18573044.
- ↑ "Rates of medical or surgical treatment for women with heavy menstrual bleeding: the ECLIPSE trial 10-year observational follow-up study" (in EN). Health Technology Assessment 27 (17): 1–50. October 2023. doi:10.3310/JHSW0174. PMID 37924269.
- ↑ "The coil and medicines are both effective long-term treatments for heavy periods". NIHR Evidence. 8 March 2024. doi:10.3310/nihrevidence_62335. https://evidence.nihr.ac.uk/alert/the-coil-and-medicines-are-both-effective-long-term-treatments-for-heavy-periods/.
- ↑ "Levonorgestrel-IUS system and endometrial manipulation". Journal of Mid-Life Health 4 (1): 6–7. January 2013. doi:10.4103/0976-7800.109625. PMID 23833526.
- ↑ "Use of the levonorgestrel releasing-intrauterine system in nulliparous women--a non-interventional study in Sweden". The European Journal of Contraception & Reproductive Health Care 16 (2): 126–134. April 2011. doi:10.3109/13625187.2011.558222. PMID 21417562.
- ↑ 66.0 66.1 "Management of pain associated with the insertion of intrauterine contraceptives". Human Reproduction Update 19 (4): 419–427. 2013. doi:10.1093/humupd/dmt022. PMID 23670222.
- ↑ "Lidocaine for pain control during intrauterine device insertion". The Journal of Obstetrics and Gynaecology Research 43 (6): 1061–1066. June 2017. doi:10.1111/jog.13308. PMID 28503818.
- ↑ "Why haven't we figured out how to make IUDs less excruciating?" (in en-US). https://www.motherjones.com/politics/2022/06/why-are-iuds-so-painful-treatment-contraception-roe-dobbs-supreme-court/.
- ↑ "Long-Acting Reversible Contraception: Implants and Intrauterine Devices" (in en). https://www.acog.org/en/Clinical/Clinical%20Guidance/Practice%20Bulletin/Articles/2017/11/Long-Acting%20Reversible%20Contraception%20Implants%20and%20Intrauterine%20Devices.
- ↑ 70.0 70.1 "Immediate postabortal insertion of intrauterine devices". The Cochrane Database of Systematic Reviews 2014 (7). July 2014. doi:10.1002/14651858.cd001777.pub4. PMID 25101364.
- ↑ "Early Pregnancy Loss" (in en). https://www.acog.org/en/Clinical/Clinical%20Guidance/Practice%20Bulletin/Articles/2018/11/Early%20Pregnancy%20Loss.
- ↑ "Immediate postpartum insertion of intrauterine device for contraception". The Cochrane Database of Systematic Reviews 2015 (6). June 2015. doi:10.1002/14651858.cd003036.pub3. PMID 26115018.
- ↑ 73.0 73.1 "Intrauterine Device Expulsion After Postpartum Placement: A Systematic Review and Meta-analysis". Obstetrics and Gynecology 132 (4): 895–905. October 2018. doi:10.1097/aog.0000000000002822. PMID 30204688.
- ↑ "Insertion and removal of intrauterine devices". American Family Physician 71 (1): 95–102. January 2005. PMID 15663031. https://www.aafp.org/afp/2005/0101/p95.html.
- ↑ "What's an IUD insertion like?" (in en). https://www.plannedparenthood.org/learn/birth-control/iud/whats-an-iud-insertion-like.
- ↑ Yaron, Michal; Legardeur, Hélène; Barcellini, Bastien; Akhoundova, Farida; Mathevet, Patrice (2023-07-01). "Safety and efficacy of a suction cervical stabilizer for intrauterine contraceptive device insertion: Results from a randomized, controlled study". Contraception 123. doi:10.1016/j.contraception.2023.110004. ISSN 0010-7824. PMID 36914147. https://www.sciencedirect.com/science/article/pii/S0010782423000665.
- ↑ "510(k) Premarket Notification". https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfPMN/pmn.cfm?ID=K223866.
- ↑ Ansanay-Alex, Sandra (2023-02-07). "Aspivix receives U.S. FDA Clearance for Carevix™, Their Novel Cervical Stabilizer" (in en-US). https://bioalps.org/aspivix-receives-fda-clearance-carevix-cervical-stabilizer/.
- ↑ "Society of Family Planning Guidelines: Postplacental insertion of intrauterine devices". Contraception 97 (1): 2–13. January 2018. doi:10.1016/j.contraception.2017.09.014. PMID 28987293.
- ↑ "This Is What to Expect After Getting Your IUD Removed" (in en). SELF. https://www.self.com/story/iud-removal-facts.
- ↑ "Clinical Education and Training" (in en). https://www.acog.org/About-ACOG/ACOG-Departments/Long-Acting-Reversible-Contraception/LARC-Clinician-Education-and-Training.
- ↑ Liu, Guangtao; Li, Feifei; Ao, Min; Huang, Guimin (2021-08-16). "Intrauterine devices migrated into the bladder: two case reports and literature review". BMC Women's Health 21 (1): 301. doi:10.1186/s12905-021-01443-w. ISSN 1472-6874. PMID 34399735.
- ↑ "ParaGard (copper IUD)". https://www.mayoclinic.org/tests-procedures/paragard/about/pac-20391270.
- ↑ "Enlarged ovarian follicles in users of a levonorgestrel-releasing intrauterine system and contraceptive implant". The Journal of Reproductive Medicine 48 (8): 637–640. August 2003. PMID 12971147.
- ↑ "Mirena: Consumer Medicine Information". Bayer. March 2014. http://www.bayerresources.com.au/resources/uploads/CMI/file9398.pdf.
- ↑ "Mirena 20 micrograms/24 hours intrauterine delivery system - Patient Information Leaflet (PIL) - (emc) | 1132". https://www.medicines.org.uk/emc/product/1132/pil.
- ↑ "Menstrual Cup use and IUDs". Feminine Wear. http://www.femininewear.co.uk/cup-use-and-iuds-24-w.asp.
- ↑ "Menstrual cup and risk of IUD expulsion - a systematic review". Contraception and Reproductive Medicine 8 (1). January 2023. doi:10.1186/s40834-022-00203-x. PMID 36670496.
- ↑ "What Are the Side Effects & Complications of the IUD?" (in en). https://www.plannedparenthood.org/learn/birth-control/iud/what-are-the-disadvantages-of-iuds.
- ↑ (in en) The Handbook of Contraception: A Guide for Practical Management. Humana Press. 2015-09-28. ISBN 978-3-319-20185-6. https://books.google.com/books?id=ZQehCgAAQBAJ&q=infertility+and+iud&pg=PA273.
- ↑ (in en) Danforth's Obstetrics and Gynecology. Lippincott Williams & Wilkins. 2008. ISBN 978-0-7817-6937-2. https://books.google.com/books?id=v4krPhqFG8sC&q=COPPER+AND+MIRENA+MONOFILAMENT&pg=PA529.
- ↑ "Classifications for Intrauterine Devices". 9 April 2020. https://www.cdc.gov/reproductivehealth/contraception/mmwr/mec/appendixb.html.
- ↑ "U.S. Medical Eligibility Criteria for Contraceptive Use, 2016" (in en-us). MMWR. Recommendations and Reports 65 (3): 1–103. July 2016. doi:10.15585/mmwr.rr6503a1. PMID 27467196.
- ↑ "Cancer risk and PCOS". Steroids 78 (8): 782–785. August 2013. doi:10.1016/j.steroids.2013.04.004. PMID 23624028.
- ↑ "New Study Finds Women's Health Providers Use IUDs More Than Any Other Method of Birth Control" (in en). https://www.plannedparenthood.org/about-us/newsroom/press-releases/new-study-finds-womens-health-providers-use-iuds-more-than-any-other-method-of-birth-control.
- ↑ "Products - Data Briefs - Number 188 - February 2015" (in en-us). https://www.cdc.gov/nchs/data/databriefs/db188.htm.
- ↑ "Contraceptive Use in the United States" (in en). 2004-08-04. https://www.guttmacher.org/fact-sheet/contraceptive-use-united-states.
- ↑ "IUD Birth Control | Info About Mirena & ParaGard IUDs" (in en). https://www.plannedparenthood.org/learn/birth-control/iud.
- ↑ "Where Can I Buy the IUD & How Much Will It Cost?" (in en). https://www.plannedparenthood.org/learn/birth-control/iud/how-can-i-get-an-iud.
 |






