Medicine:Shoulder problems
| Shoulder problems | |
|---|---|
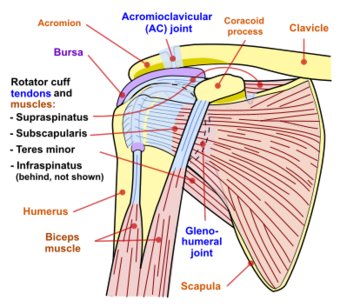 | |
| Diagram of the human shoulder joint |
Shoulder problems, including pain, are one of the more common reasons for physician visits for musculoskeletal symptoms. The shoulder is the most movable joint in the body. However, it is an unstable joint because of the range of motion allowed. This instability increases the likelihood of joint injury, often leading to a degenerative process in which tissues break down and no longer function well.
Shoulder pain may be localized or may be referred to areas around the shoulder or down the arm. Other regions within the body (such as gallbladder, liver, or heart disease, or disease of the cervical spine of the neck) also may generate pain that the brain may interpret as arising from the shoulder.[1]
Shoulder structures and functions
The rotator cuff is a structure composed of tendons that, with associated muscles, holds the ball at the top of the humerus in the glenoid socket and provides mobility and strength to the shoulder joint.[2]
Diagnosis
Following are some of the ways doctors diagnose shoulder problems:
Medical history and physical exam
- Medical history (the patient tells the doctor about an injury). For shoulder problems the medical history includes the patient's age, dominant hand, if injury affects normal work/activities as well as details on the actual shoulder problem including acute versus chronic and the presence of shoulder catching, instability, locking, pain, paresthesias (burning sensation), stiffness, swelling, and weakness.[3] Other salutary information includes OPQRST (onset, palliation/provocation, quality, radiation, severity, timing) and a history of issues that could lead to referred pain (pain felt at the shoulder but actually coming from another part of the body) including cervical spine disorders, heart attacks, peptic ulcer disease, and pneumonia. Standardized questionnaires like the Penn Shoulder Score that assess shoulder pain and function can aid in eliciting the required history to make a diagnosis and monitor condition progression.[4]
- Physical examination of the shoulder to feel for injury and discover the limits of movement, location of pain, and extent of joint instability. The steps to elicit this information are inspection (looking), palpation (feeling), testing range of motion, and performing special maneuvers.[3] Information collected on inspection are asymmetry, atrophy, ecchymosis, scars, swelling, and venous distention. Palpation can help find pain and deformities, and should specifically include the anterior glenohumeral joint, acromioclavicular joint, biceps tendon, cervical spine, coracoid process, scapula, and sternoclavicular joint. Range of motion tests external and internal rotation, abduction and adduction, passive and active weakness, and true weakness versus weakness due to pain. The Apley scratch test is the most useful: touch opposite scapular by reaching behind the head for adduction and external rotation and behind the back for abduction and internal rotation. Finally, there are more specific maneuvers that can home in on a diagnosis, however their accuracy is limited.[5]
Diagnostic tests
- X-ray
- Arthrogram—Diagnostic record that can be seen on an X-ray after injection of a contrast fluid into the shoulder joint to outline structures such as the rotator cuff. In disease or injury, this contrast fluid may either leak into an area where it does not belong, indicating a tear or opening, or be blocked from entering an area where there normally is an opening.
- MRI (magnetic resonance imaging)--A non-invasive procedure in which a machine produces a series of cross-sectional images of the shoulder.
- Other diagnostic tests, such as injection of an anesthetic into and around the shoulder joint.
Dislocation
Description
Signs and diagnosis
Treatment
Separation
Description
Signs and diagnosis
Treatment
Sternoclavicular separation
Description
Signs and diagnosis
Treatment
Rotator cuff tendinopathy (tendinitis, bursitis, impingement syndrome, and rotator cuff tears)
Anatomy
Pathology
The rotator cuff tendons degenerate with age.[6][7][8][9] A group of respected scientists wrote in a review of existing evidence that, the theory that this degeneration is related to pinching (or impingement) between the head of the humerus and the acromion is now considered inaccurate.[10] Rotator cuff pathology is similar in non-dominant compared to dominant and symptomatic compared to asymptomatic shoulder.[7][8][11][12][13][14] About two-thirds of all humans develop rotator cuff tendinopathy if they live to 70 years of age.[6] The pathology is mucoid degeneration, not inflammation.[10] The process can involve the intra-articular part of the long head of biceps in addition to the supraspinatus, infraspinatus, and subscapularis tendons.[15]
Rotator cuff tear
Signs
Diagnosis
Diagnosis of tendinitis and bursitis begins with a medical history and physical examination. X-rays do not show tendons or the bursae but may be helpful in ruling out bony abnormalities or arthritis. The doctor may remove and test fluid from the inflamed area to rule out infection. Ultrasound scans are frequently used to confirm a suspected tendinitis or bursitis as well as rule out a tear in the rotator cuff muscles.
Treatment
Anti-inflammatory medicines such as aspirin, naproxen or ibuprofen among others can be taken to help with pain. In some cases the physical therapist will use ultrasound and electrical stimulation, as well as manipulation. Gentle stretching and strengthening exercises are added gradually. If there is no improvement, the doctor may inject a corticosteroid medicine into the space under the acromion. However, recent level one evidence showed limited efficacy of corticosteroid injections for pain relief.[16] While steroid injections are a common treatment, they must be used with caution because they may lead to tendon rupture. If there is still no improvement after six to 12 months, the doctor may perform either arthroscopic or open surgery to repair damage and relieve pressure on the tendons and bursae. In those with calcific tendinitis of the shoulder high energy extracorporeal shock-wave therapy can be useful.[17] It is not useful in other types of tendonitis.[17] For a rotator cuff tear, tentative evidence suggests exercise may reduce pain in the short-term.[18] Combination of exercise and joint mobilization can result in long term benefits.[18] Other evidence demonstrates the use of corticosteroids injections to be more effective.[18]
SLAP tear (lesion)
Symptoms
Diagnosis
The best diagnosis for a SLAP tear is a clinical exam
Treatment
Recovery
Frozen shoulder (adhesive capsulitis)
Fracture
Description
Signs and diagnosis
A shoulder fracture that occurs after a major injury is usually accompanied by severe pain. Within a short time, there may be redness and bruising around the area. Sometimes a fracture is obvious because the bones appear out of position.
Treatment
Arthritis of the shoulder (glenohumeral joint)
Description
In arthritis of the shoulder, the cartilage of the ball and socket (glenohumeral joint) is lost so that bone rubs on bone.
Signs and diagnosis

Treatment
Early on arthritis of the shoulder can be managed with mild analgesics and gentle exercises.[19] Known gentle exercises include warm water therapy pool exercises that are provided by a trained and licensed physical therapist; approved land exercises to assure free movement of the arthritic area; cortisone injections (administered at the minimum of every six months according to orthopedic physicians) to reduce inflammation; ice and hot moist pact application are very effective. Moist heat is preferred over ice whereas ice is preferred if inflammation occurs during the daytime hours. Local analgesics along with ice or moist heat are adequate treatments for acute pain.
In young and active patients a partial shoulder replacement with a non-prosthetic glenoid arthroplasty may also be a consideration
Arthritis or osteolysis of the AC (acromioclavicular) joint
Description
Signs and diagnosis
Pain is perceived on shoulder motion, especially on certain movements. Often a crossover arm test is utilized in diagnosis because this compresses the AC joint, exacerbating the symptoms. X-rays of the shoulder joint may show either arthritic changes of the ac joint or osteolysis.
Treatment
Treatment
- Protection: Guard the shoulder to prevent further injury.
- Rest: Reduce or stop using the injured area for 48 hours.
- Ice: Put an ice pack on the injured area for 20 minutes at a time, 4 to 8 times per day. Use a cold pack, ice bag, or a plastic bag filled with crushed ice that has been wrapped in a towel.
- Compression: Compress the area with bandages, such as an elastic wrap, to help stabilize the shoulder.
- Elevation: Keep the injured area elevated above the level of the heart. Use a pillow to help elevate the injury.
If pain and stiffness persist, see a doctor.
According to the American Academy of Orthopaedic Surgeons (AAOS) visits to orthopedic specialists for shoulder pain has been rising since 1998 and in 2005 over 13 million patients sought medical care for shoulder pain, of which only 34 percent were related to injury.[20]
References
- ↑ "Referred Shoulder Pain - Topic Overview". WebMD, LLC.. 14 November 2014. http://www.webmd.com/pain-management/tc/referred-shoulder-pain-topic-overview.
- ↑ Zadro, Joshua; Rischin, Adam; Johnston, Renea V; Buchbinder, Rachelle (2021-08-26). Cochrane Musculoskeletal Group. ed. "Image-guided glucocorticoid injection versus injection without image guidance for shoulder pain" (in en). Cochrane Database of Systematic Reviews 2021 (9). doi:10.1002/14651858.CD009147.pub3. PMID 34435661.
- ↑ 3.0 3.1 Woodward, T. W.; Best, T. M. (15 May 2000). "The painful shoulder: part I. Clinical evaluation.". American Family Physician 61 (10): 3079–88. PMID 10839557.
- ↑ "Penn Shoulder Score description and calculator – orthotoolkit". http://www.orthotoolkit.com/index.php/penn-shoulder-score/.
- ↑ E. J. Hegedus; A. Goode; S. Campbell; A. Morin; M. Tamaddoni; C. T. Moorman III; C. Cook (2007). "Physical Examination Tests of the Shoulder: A Systematic Review with Meta-analysis of Individual Tests". Br J Sports Med 42 (2): 80–92. doi:10.1136/bjsm.2007.038406. PMID 17720798.
- ↑ 6.0 6.1 Teunis, Teun; Lubberts, Bart; Reilly, Brian T.; Ring, David (December 2014). "A systematic review and pooled analysis of the prevalence of rotator cuff disease with increasing age". Journal of Shoulder and Elbow Surgery 23 (12): 1913–1921. doi:10.1016/j.jse.2014.08.001. ISSN 1532-6500. PMID 25441568.
- ↑ 7.0 7.1 Yamaguchi, Ken; Ditsios, Konstantinos; Middleton, William D.; Hildebolt, Charles F.; Galatz, Leesa M.; Teefey, Sharlene A. (August 2006). "The demographic and morphological features of rotator cuff disease. A comparison of asymptomatic and symptomatic shoulders". The Journal of Bone and Joint Surgery. American Volume 88 (8): 1699–1704. doi:10.2106/JBJS.E.00835. ISSN 0021-9355. PMID 16882890.
- ↑ 8.0 8.1 Liu, Tiffany C.; Leung, Nina; Edwards, Leonard; Ring, David; Bernacki, Edward; Tonn, Melissa D. (October 2017). "Patients Older Than 40 Years With Unilateral Occupational Claims for New Shoulder and Knee Symptoms Have Bilateral MRI Changes". Clinical Orthopaedics and Related Research 475 (10): 2360–2365. doi:10.1007/s11999-017-5401-y. ISSN 1528-1132. PMID 28600690.
- ↑ Vincent, Karl; Leboeuf-Yde, Charlotte; Gagey, Olivier (May 2017). "Are degenerative rotator cuff disorders a cause of shoulder pain? Comparison of prevalence of degenerative rotator cuff disease to prevalence of nontraumatic shoulder pain through three systematic and critical reviews". Journal of Shoulder and Elbow Surgery 26 (5): 766–773. doi:10.1016/j.jse.2016.09.060. ISSN 1532-6500. PMID 28089260.
- ↑ 10.0 10.1 McFarland, Edward G.; Maffulli, Nicola; Del Buono, Angelo; Murrell, George A. C.; Garzon-Muvdi, Juan; Petersen, Steve A. (July 2013). "Impingement is not impingement: the case for calling it "Rotator Cuff Disease"". Muscles, Ligaments and Tendons Journal 3 (3): 196–200. doi:10.32098/mltj.03.2013.11. ISSN 2240-4554. PMID 24367779.
- ↑ Barreto, Rodrigo Py Gonçalves; Braman, Jonathan P.; Ludewig, Paula M.; Ribeiro, Larissa Pechincha; Camargo, Paula Rezende (September 2019). "Bilateral magnetic resonance imaging findings in individuals with unilateral shoulder pain". Journal of Shoulder and Elbow Surgery 28 (9): 1699–1706. doi:10.1016/j.jse.2019.04.001. ISSN 1532-6500. PMID 31279721.
- ↑ Eliason, Anna; Harringe, Marita; Engström, Björn; Sunding, Kerstin; Werner, Suzanne (2021-08-17). "Bilateral ultrasound findings in patients with unilateral subacromial pain syndrome". Physiotherapy Theory and Practice 38 (13): 2568–2579. doi:10.1080/09593985.2021.1962462. ISSN 1532-5040. PMID 34402715.
- ↑ Yamaguchi, K.; Tetro, A. M.; Blam, O.; Evanoff, B. A.; Teefey, S. A.; Middleton, W. D. (May 2001). "Natural history of asymptomatic rotator cuff tears: a longitudinal analysis of asymptomatic tears detected sonographically". Journal of Shoulder and Elbow Surgery 10 (3): 199–203. doi:10.1067/mse.2001.113086. ISSN 1058-2746. PMID 11408898.
- ↑ Ranebo, Mats C.; Björnsson Hallgren, Hanna C.; Adolfsson, Lars E. (March 2018). "Patients with a long-standing cuff tear in one shoulder have high rates of contralateral cuff tears: a study of patients with arthroscopically verified cuff tears 22 years ago". Journal of Shoulder and Elbow Surgery 27 (3): e68–e74. doi:10.1016/j.jse.2017.10.007. ISSN 1532-6500. PMID 29249548.
- ↑ Ahrens, P. M.; Boileau, P. (August 2007). "The long head of biceps and associated tendinopathy". The Journal of Bone and Joint Surgery. British Volume 89 (8): 1001–1009. doi:10.1302/0301-620X.89B8.19278. ISSN 0301-620X. PMID 17785735.
- ↑ Mohamadi, Amin; Chan, Jimmy J.; Claessen, Femke M. A. P.; Ring, David; Chen, Neal C. (January 2017). "Corticosteroid Injections Give Small and Transient Pain Relief in Rotator Cuff Tendinosis: A Meta-analysis". Clinical Orthopaedics and Related Research 475 (1): 232–243. doi:10.1007/s11999-016-5002-1. ISSN 1528-1132. PMID 27469590.
- ↑ 17.0 17.1 Bannuru, R. R.; Flavin, N. E.; Vaysbrot, E.; Harvey, W.; McAlindon, T. (15 April 2014). "High-energy extracorporeal shock-wave therapy for treating chronic calcific tendinitis of the shoulder: a systematic review.". Annals of Internal Medicine 160 (8): 542–9. doi:10.7326/m13-1982. PMID 24733195.
- ↑ 18.0 18.1 18.2 Green, Sally; Buchbinder, Rachelle; Hetrick, Sarah E (2003-04-22). "Physiotherapy interventions for shoulder pain". Cochrane Database of Systematic Reviews 2013 (2). doi:10.1002/14651858.cd004258. ISSN 1465-1858. PMID 12804509.
- ↑ "Introduction - Home Exercises for the Rough Shoulder". Orthop.washington.edu. 2006-10-09. http://www.orthop.washington.edu/?q=patient-care/articles/shoulder/home-exercises-for-the-rough-shoulder.html.
- ↑ American Academy of Orthopaedic Surgeons Physician Visits for Musculoskeletal Symptoms http://www.aaos.org/Research/stats/Common%20Orthopaedic%20Symptoms%20Seen%20by%20a%20Physician.pdf
This article contains and extends text from the public domain document "Questions and Answers about Shoulder Problems", NIH Publication No. 01-4865, available from URL [1]
External links
| Classification |
|---|
 |
