Medicine:Blood sugar level
The blood sugar level, blood sugar concentration, blood glucose level, or glycemia, is the measure of glucose concentrated in the blood. The body tightly regulates blood glucose levels as a part of metabolic homeostasis.[2]
For a 70 kg (154 lb) human, approximately four grams of dissolved glucose (also called "blood glucose") is maintained in the blood plasma at all times.[2] Glucose that is not circulating in the blood is stored in skeletal muscle and liver cells in the form of glycogen;[2] in fasting individuals, blood glucose is maintained at a constant level by releasing just enough glucose from these glycogen stores in the liver and skeletal muscle in order to maintain homeostasis.[2] Glucose can be transported from the intestines or liver to other tissues in the body via the bloodstream.[2] Cellular glucose uptake is primarily regulated by insulin, a hormone produced in the pancreas.[2] Once inside the cell, the glucose can now act as an energy source as it undergoes the process of glycolysis.
In humans, properly maintained glucose levels are necessary for normal function in a number of tissues, including the human brain, which consumes approximately 60% of blood glucose in fasting, sedentary individuals.[2] A persistent elevation in blood glucose leads to glucose toxicity, which contributes to cell dysfunction and the pathology grouped together as complications of diabetes.[2]
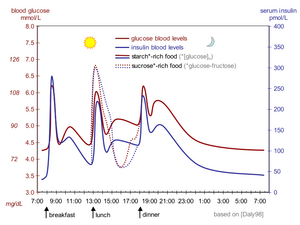
Glucose levels are usually lowest in the morning, before the first meal of the day, and rise after meals for an hour or two by a few millimoles.
Abnormal persistently high glycemia is referred to as hyperglycemia; low levels are referred to as hypoglycemia. Diabetes mellitus is characterized by persistent hyperglycemia from a variety of causes, and it is the most prominent disease related to the failure of blood sugar regulation. There are different methods of testing and measuring blood sugar levels.
Drinking alcohol causes an initial surge in blood sugar and later tends to cause levels to fall. Also, certain drugs can increase or decrease glucose levels.[3]
Units
There are two ways of measuring blood glucose levels: In the United Kingdom and Commonwealth countries (Australia, Canada, India, etc.) and ex-USSR countries molar concentration, measured in mmol/L (millimoles per litre, or millimolar, abbreviated mM). In the United States, Germany, Japan and many other countries mass concentration is measured in mg/dL (milligrams per decilitre).[4]
Since the molecular weight of glucose C6H12O6 is 180, the difference between the two units is a factor of 18, so 1 mmol/L of glucose is equivalent to 18 mg/dL.[5]Template:BSN
Normal value range
Humans
Normal value ranges may vary slightly between laboratories. Glucose homeostasis, when operating normally, restores the blood sugar level to a narrow range of about 4.4 to 6.1 mmol/L (79 to 110 mg/dL) (as measured by a fasting blood glucose test).[6]
Normal blood glucose level (tested while fasting) for non-diabetics is between 3.9 and 7.1 mmol/L (70 and 130 mg/dL). The global mean fasting plasma blood glucose level in humans is about 5.5 mmol/L (100 mg/dL);[7][5] however, this level fluctuates throughout the day. Blood sugar levels for those without diabetes and who are not fasting should be below 6.9 mmol/L (125 mg/dL).[8] The blood glucose target range for diabetics, according to the American Diabetes Association, should be 5.0–7.2 mmol/L (90–130 mg/dL) before meals and less than 10 mmol/L (180 mg/dL) two hours after meals (as measured by a blood glucose monitor).[9][10]
Despite widely variable intervals between meals or the occasional consumption of meals with a substantial carbohydrate load, human blood glucose levels tend to remain within the normal range. However, shortly after eating, the blood glucose level may rise, in non-diabetics, temporarily up to 7.8 mmol/L (140 mg/dL) or slightly more. For people with diabetes maintaining "tight diabetes control", the American Diabetes Association recommends a post-meal glucose level of less than 10 mmol/L (180 mg/dL) and a fasting plasma glucose of 3.9 to 7.2 mmol/L (70–130 mg/dL).[11]
The actual amount of glucose in the blood and body fluids is very small. In a healthy adult male of 75 kg (165 lb) with a blood volume of 5 L, a blood glucose level of 5.5 mmol/L (100 mg/dL) amounts to 5 g, equivalent to about a teaspoonful of sugar.[12] Part of the reason why this amount is so small is that, to maintain an influx of glucose into cells, enzymes modify glucose by adding phosphate or other groups to it.[citation needed]
Other animals
In general, ranges of blood sugar in common domestic ruminants are lower than in many monogastric mammals.[13] However this generalization does not extend to wild ruminants or camelids. For serum glucose in mg/dL, reference ranges of 42 to 75 for cows, 44 to 81 for sheep, and 48 to 76 for goats, but 61 to 124 for cats; 62 to 108 for dogs, 62 to 114 for horses, 66 to 116 for pigs, 75 to 155 for rabbits, and 90 to 140 for llamas have been reported.[14] A 90 percent reference interval for serum glucose of 26 to 181 mg/dL has been reported for captured mountain goats (Oreamnos americanus), where no effects of the pursuit and capture on measured levels were evident.[15] For beluga whales, the 25–75 percent range for serum glucose has been estimated to be 94 to 115 mg/dL.[16] For the white rhinoceros, one study has indicated that the 95 percent range is 28 to 140 mg/dL.[17] For harp seals, a serum glucose range of 4.9 to 12.1 mmol/L [i.e. 88 to 218 mg/dL] has been reported; for hooded seals, a range of 7.5 to 15.7 mmol/L [i.e. about 135 to 283 mg/dL] has been reported.[18]
Regulation
The body's homeostatic mechanism keeps blood glucose levels within a narrow range. It is composed of several interacting systems, of which hormone regulation is the most important.[19]
There are two types of mutually antagonistic metabolic hormones affecting blood glucose levels:
- catabolic hormones (such as glucagon, cortisol and catecholamines) which increase blood glucose;[20]
- and one anabolic hormone (insulin), which decreases blood glucose.
These hormones are secreted from pancreatic islets (bundles of endocrine tissues), of which there are four types: alpha (A) cells, beta (B) cells, Delta (D) cells and F cells. Glucagon is secreted from alpha cells, while insulin is secreted by beta cells. Together they regulate the blood-glucose levels through negative feedback, a process where the end product of one reaction stimulates the beginning of another reaction. In blood-glucose levels, insulin lowers the concentration of glucose in the blood. The lower blood-glucose level (a product of the insulin secretion) triggers glucagon to be secreted, and repeats the cycle.[21]
In order for blood glucose to be kept stable, modifications to insulin, glucagon, epinephrine and cortisol are made. Each of these hormones has a different responsibility to keep blood glucose regulated; when blood sugar is too high, insulin tells muscles to take up excess glucose for storage in the form of glycogen. Glucagon responds to too low of a blood glucose level; it informs the tissue to release some glucose from the glycogen stores. Epinephrine prepares the muscles and respiratory system for activity in the case of a "fight or flight" response. Lastly, cortisol supplies the body with fuel in times of heavy stress.[22]
Abnormalities
High blood sugar
If blood sugar levels remain too high the body suppresses appetite over the short term. Long-term hyperglycemia causes many health problems including heart disease, cancer,[23] eye, kidney, and nerve damage.[24]
Blood sugar levels above 16.7 mmol/L (300 mg/dL) can cause fatal reactions. Ketones will be very high (a magnitude higher than when eating a very low carbohydrate diet) initiating ketoacidosis. The ADA (American Diabetes Association) recommends seeing a doctor if blood glucose reaches 13.3 mmol/L (240 mg/dL),[25] and it is recommended to seek emergency treatment at 15 mmol/L (270 mg/dL) blood glucose if Ketones are present.[26] The most common cause of hyperglycemia is diabetes. When diabetes is the cause, physicians typically recommend an anti-diabetic medication as treatment. From the perspective of the majority of patients, treatment with an old, well-understood diabetes drug such as metformin will be the safest, most effective, least expensive, and most comfortable route to managing the condition. Treatment will vary for the distinct forms of Diabetes and can differ from person to person based on how they are reacting to treatment.[27] Diet changes and exercise implementation may also be part of a treatment plan for diabetes.[28]
Some medications may cause a rise in blood sugars of diabetics, such as steroid medications, including cortisone, hydrocortisone, prednisolone, prednisone, and dexamethasone.[29]
Low blood sugar
When the blood sugar level is below 70 mg/dL, this is referred to as having low blood sugar. Low blood sugar is very frequent among type 1 diabetics. There are several causes of low blood sugar, including, taking an excessive amount of insulin, not consuming enough carbohydrates, drinking alcohol, spending time at a high elevation, puberty, and menstruation.[30] If blood sugar levels drop too low, a potentially fatal condition called hypoglycemia develops. Symptoms may include lethargy, impaired mental functioning; irritability; shaking, twitching, weakness in arm and leg muscles; pale complexion; sweating; loss of consciousness.[citation needed]
Mechanisms that restore satisfactory blood glucose levels after extreme hypoglycemia (below 2.2 mmol/L or 40 mg/dL) must be quick and effective to prevent extremely serious consequences of insufficient glucose: confusion or unsteadiness and, in the extreme (below 0.8 mmol/L or 15 mg/dL) loss of consciousness and seizures. Without discounting the potentially quite serious conditions and risks due to or oftentimes accompanying hyperglycemia, especially in the long-term (diabetes or pre-diabetes, obesity or overweight, hyperlipidemia, hypertension, etc.), it is still generally more dangerous to have too little glucose – especially if levels are very low – in the blood than too much, at least temporarily, because glucose is so important for metabolism and nutrition and the proper functioning of the body's organs. This is especially the case for those organs that are metabolically active or that require a constant, regulated supply of blood sugar (the liver and brain are examples). Symptomatic hypoglycemia is most likely associated with diabetes and liver disease (especially overnight or postprandial), without treatment or with wrong treatment, possibly in combination with carbohydrate malabsorption, physical over-exertion or drugs. Many other less likely illnesses, like cancer, could also be a reason. Starvation, possibly due to eating disorders, like anorexia, will also eventually lead to hypoglycemia. Hypoglycemic episodes can vary greatly between persons and from time to time, both in severity and swiftness of onset. For severe cases, prompt medical assistance is essential, as damage to brain and other tissues and even death will result from sufficiently low blood-glucose levels.[citation needed]
Glucose measurement
In the past to measure blood glucose it was necessary to take a blood sample, as explained below, but since 2015 it has also been possible to use a continuous glucose monitor, which involves an electrode placed under the skin. Both methods, as of 2023, cost hundreds of dollars or euros per year for supplies needed.[citation needed]
Sample source
Glucose testing in a fasting individual shows comparable levels of glucose in arterial, venous, and capillary blood. But following meals, capillary and arterial blood glucose levels can be significantly higher than venous levels. Although these differences vary widely, one study found that following the consumption of 50 grams of gluten, "the mean capillary blood glucose concentration is higher than the mean venous blood glucose concentration by 35%."[31][32]
Sample type
Glucose is measured in whole blood, plasma or serum. Historically, blood glucose values were given in terms of whole blood, but most laboratories now measure and report plasma or serum glucose levels. Because red blood cells (erythrocytes) have a higher concentration of protein (e.g., hemoglobin) than serum, serum has a higher water content and consequently more dissolved glucose than does whole blood. To convert from whole-blood glucose, multiplication by 1.14[33] has been shown to generally give the serum/plasma level.
To prevent contamination of the sample with intravenous fluids, particular care should be given to drawing blood samples from the arm opposite the one in which an intravenous line is inserted. Alternatively, blood can be drawn from the same arm with an IV line after the IV has been turned off for at least 5 minutes, and the arm has been elevated to drain infused fluids away from the vein. Inattention can lead to large errors, since as little as 10% contamination with a 5% glucose solution (D5W) will elevate glucose in a sample by 500 mg/dL or more. The actual concentration of glucose in blood is very low, even in the hyperglycemic.[citation needed]
Measurement techniques
Two major methods have been used to measure glucose. The first, still in use in some places, is a chemical method exploiting the nonspecific reducing property of glucose in a reaction with an indicator substance that changes color when reduced. Since other blood compounds also have reducing properties (e.g., urea, which can be abnormally high in uremic patients), this technique can produce erroneous readings in some situations (5–15 mg/dL has been reported). The more recent technique, using enzymes specific to glucose, is less susceptible to this kind of error. The two most common employed enzymes are glucose oxidase and hexokinase.[34] Average blood glucose concentrations can also be measured. This method measures the level of glycated hemoglobin, which is representative of the average blood glucose levels over the last, approximately, 120 days.[34]
In either case, the chemical system is commonly contained on a test strip which is inserted into a meter, and then has a blood sample applied. Test-strip shapes and their exact chemical composition vary between meter systems and cannot be interchanged. Formerly, some test strips were read (after timing and wiping away the blood sample) by visual comparison against a color chart printed on the vial label. Strips of this type are still used for urine glucose readings, but for blood glucose levels they are obsolete. Their error rates were, in any case, much higher. Errors when using test strips were often caused by the age of the strip or exposure to high temperatures or humidity.[35] More precise blood glucose measurements are performed in a medical laboratory, using hexokinase, glucose oxidase, or glucose dehydrogenase enzymes.
Urine glucose readings, however taken, are much less useful. In properly functioning kidneys, glucose does not appear in urine until the renal threshold for glucose has been exceeded. This is substantially above any normal glucose level, and is evidence of an existing severe hyperglycemic condition. However, as urine is stored in the bladder, any glucose in it might have been produced at any time since the last time the bladder was emptied. Since metabolic conditions change rapidly, as a result of any of several factors, this is delayed news and gives no warning of a developing condition.[36] Blood glucose monitoring is far preferable, both clinically and for home monitoring by patients. Healthy urine glucose levels were first standardized and published in 1965[37] by Hans Renschler.
A noninvasive method of sampling to monitor glucose levels has emerged using an exhaled breath condensate. However this method does need highly sensitive glucose biosensors.[38]
| I. Chemical methods | ||
|---|---|---|
| A. Oxidation-reduction reaction | ||
| [math]\displaystyle{ \mathrm{Glucose} + \mathrm{Alkaline\ copper\ tartarate}\xrightarrow{\mathrm{Reduction}} \mathrm{Cuprous\ oxide} }[/math] | ||
| 1. Alkaline copper reduction | ||
| Folin-Wu method | [math]\displaystyle{ \mathrm{Cu}^{2+} + \mathrm{Phosphomolybdic\ acid}\xrightarrow{\mathrm{Oxidation}} \mathrm{Phosphomolybdenum\ oxide} }[/math] | Blue end-product |
| Benedict's method |
| |
| Nelson–Somogyi method | [math]\displaystyle{ \mathrm{Cu}^{2+} + \mathrm{Arsenomolybdic\ acid}\xrightarrow{\mathrm{Oxidation}} \mathrm{Arsenomolybdenum\ oxide} }[/math] | Blue end-product. |
| Neocuproine method | [math]\displaystyle{ \mathrm{Cu}^{2+} + \mathrm{Neocuproine}\xrightarrow{\mathrm{Oxidation}} \mathrm{Cu}^{2+} \mathrm{neocuproine\ complex} }[/math]* | Yellow-orange color neocuproine[39] |
| Shaeffer–Hartmann–Somogyi |
| |
| 2. Alkaline Ferricyanide reduction | ||
| Hagedorn–Jensen | [math]\displaystyle{ \mathrm{Glucose} + \mathrm{Alkaline\ ferricyanide}\longrightarrow \mathrm{Ferrocyanide} }[/math] | Colorless end product; other reducing substances interfere with reaction. |
| B. Condensation | ||
| Ortho-toluidine method |
| |
| Anthrone (phenols) method |
| |
| II. Enzymatic methods | ||
| A. Glucose oxidase | ||
| [math]\displaystyle{ \mathrm{Glucose} + \mathrm{O}_{2}\xrightarrow[\mathrm{Oxidation}] {\mathrm{glucose\ oxidase}}\textrm{D-glucono-1,5-lactone} + \mathrm{H_{2}O_{2}} }[/math] | ||
| Saifer–Gerstenfeld method | [math]\displaystyle{ \mathrm{H_{2}O_2} + \textit{O}\text{-dianisidine}\xrightarrow[\mathrm{Oxidation}] {\mathrm{peroxidase}} \mathrm{H_2O} + \mathrm{oxidized\ chromogen} }[/math] | Inhibited by reducing substances like BUA, bilirubin, glutathione, ascorbic acid. |
| Trinder method |
| |
| Kodak Ektachem |
| |
| Glucometer |
| |
| B. Hexokinase | ||
|
[math]\displaystyle{ \begin{alignat}{2} & \mathrm{Glucose} + \mathrm{ATP}\xrightarrow[\mathrm{Phosphorylation}] {\mathrm{Hexokinase} + \mathrm{Mg}^{2+}} \textrm{G-6PO}_4 + \mathrm{ADP} \\ & \textrm{G-6PO}_4 + \mathrm{NADP}\xrightarrow[\mathrm{Oxidation}] {\textrm{G-6PD}} \textrm{6-Phosphogluconate} + \mathrm{NADPH} + \mathrm{H}^{+} \\ \end{alignat} }[/math] | ||
| ||
Clinical correlation
The fasting blood glucose level, which is measured after a fast of 8 hours, is the most commonly used indication of overall glucose homeostasis, largely because disturbing events such as food intake are avoided. Conditions affecting glucose levels are shown in the table below. Abnormalities in these test results are due to problems in the multiple control mechanism of glucose regulation.[citation needed]
The metabolic response to a carbohydrate challenge is conveniently assessed by a postprandial glucose level drawn 2 hours after a meal or a glucose load. In addition, the glucose tolerance test, consisting of several timed measurements after a standardized amount of oral glucose intake, is used to aid in the diagnosis of diabetes.[citation needed]
Error rates for blood glucose measurements systems vary, depending on laboratories, and on the methods used. Colorimetry techniques can be biased by color changes in test strips (from airborne or finger-borne contamination, perhaps) or interference (e.g., tinting contaminants) with light source or the light sensor. Electrical techniques are less susceptible to these errors, though not to others. In home use, the most important issue is not accuracy, but trend. Thus if a meter / test strip system is consistently wrong by 10%, there will be little consequence, as long as changes (e.g., due to exercise or medication adjustments) are properly tracked. In the US, home use blood test meters must be approved by the federal Food and Drug Administration before they can be sold.[citation needed]
Finally, there are several influences on blood glucose level aside from food intake. Infection, for instance, tends to change blood glucose levels, as does stress either physical or psychological. Exercise, especially if prolonged or long after the most recent meal, will have an effect as well. In the typical person, maintenance of blood glucose at near constant levels will nevertheless be quite effective.[clarification needed]
| Persistent hyperglycemia | Transient hyperglycemia | Persistent hypoglycemia | Transient hypoglycemia |
|---|---|---|---|
| Reference range, fasting blood glucose (FBG): 70–110 mg/dL | |||
| Diabetes mellitus | Pheochromocytoma | Insulinoma | Acute alcohol intoxication or ingestion |
| Adrenal cortical hyperactivity Cushing's syndrome | Severe liver disease | Adrenal cortical insufficiency Addison's disease | Drugs: salicylates, antituberculosis agents |
| Hyperthyroidism | Acute stress reaction | Hypopituitarism | Severe liver disease |
| Acromegaly | Shock | Galactosemia | Several glycogen storage diseases |
| Obesity | Convulsions | Ectopic hormone production from tumors | Hereditary fructose intolerance |
See also
References
- ↑ "Acute effects on insulin sensitivity and diurnal metabolic profiles of a high-sucrose compared with a high-starch diet". The American Journal of Clinical Nutrition 67 (6): 1186–96. June 1998. doi:10.1093/ajcn/67.6.1186. PMID 9625092. http://www.ajcn.org/content/67/6/1186.full.pdf.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 2.7 "Four grams of glucose". American Journal of Physiology. Endocrinology and Metabolism 296 (1): E11–21. January 2009. doi:10.1152/ajpendo.90563.2008. PMID 18840763.
- ↑ Walker, Rosemary and Rodgers, Jill (2006) Type 2 Diabetes – Your Questions Answered. Dorling Kindersley. ISBN:1-74033-550-3.
- ↑ "Blood Glucose Monitor and Blood Glucose Meter - Blood Glucose Measurement Units FAQ". 6 July 2011. http://www.abbottdiabetescare.com.au/diabetes-faq-measure-units.php.
- ↑ 5.0 5.1 What are mg/dL and mmol/L? How to convert? Glucose? Cholesterol? Advameg, Inc.
- ↑ "Screening for Type 2 Diabetes". Clinical Diabetes 18 (2). 2000. http://journal.diabetes.org/clinicaldiabetes/v18n22000/pg69.htm.
- ↑ Danaei, G (2 July 2011). "National, regional, and global trends in fasting plasma glucose and diabetes prevalence since 1980: systematic analysis of health examination surveys and epidemiological studies with 370 country-years and 2·7 million participants.". The Lancet 378 (9785): 31–40. doi:10.1016/S0140-6736(11)60679-X. PMID 21705069.
- ↑ Glucose test – blood. NIH – National Institutes of Health.
- ↑ Davidson, Nancy Klobassa; Moreland, Peggy (26 July 2011). "Living with diabetes blog". Mayo Clinic. http://www.mayoclinic.com/health/blood-glucose-target-range/MY00494.
- ↑ Schuster, Dara (14 August 2008). "What Does 'Post-Meal (Or Post-Prandial) Blood Sugar' Mean And What Does It Tell You?". Ohio State University. https://abcnews.go.com/Health/DiabetesScreening/story?id=3812972.
- ↑ American Diabetes Association (January 2006). "Standards of medical care in diabetes--2006". Diabetes Care 29 Suppl 1 (Supplement 1): S4–42. doi:10.2337/diacare.29.s1.06.s4. PMID 16373931. http://care.diabetesjournals.org/content/29/suppl_1/s4.full. "Standards of Medical Care – Table 6 and Table 7, Correlation between A1C level and Mean Plasma Glucose Levels on Multiple Testing over 2–3 months".
- ↑ USDA National Nutrient Database for Standard Reference, Release 22 (2009)
- ↑ "Endocrine glands". Dukes' Physiology of Domestic Animals (12th ed.). Ithaca, NY: Comstock. 2004. pp. 621–69. ISBN 978-0801442384. https://archive.org/details/dukesphysiologyo0012duke.
- ↑ Merck Veterinary Manual (9th ed.). Whitehouse Station: Merck & Co.. 2005. ISBN 978-0911910506. https://archive.org/details/merckveterinarym09edunse.
- ↑ Rice, C. G.; Hall, B. (2007). "Hematologic and biochemical reference intervals for mountain goats (Oreamnos americanus): effects of capture conditions". Northwest Science 81 (3): 206. doi:10.3955/0029-344X-81.3.206.
- ↑ "Hematology and serum chemistry values in the beluga (Delphinapterus leucas)". Journal of Wildlife Diseases 24 (2): 220–4. April 1988. doi:10.7589/0090-3558-24.2.220. PMID 3373628.
- ↑ Seal, U. S.; Barton, R.; Mather, L.; Gray, C. W. (1976). "Baseline Laboratory Data for the White Rhinoceros (Ceratotherium simum simum)". The Journal of Zoo Animal Medicine 7 (1): 11–17. http://www.rhinoresourcecenter.com/pdf_files/123/1239956678.pdf.
- ↑ "Hematology and serum chemistry of harp (Phoca groenlandica) and hooded seals (Cystophora cristata) during the breeding season, in the Gulf of St. Lawrence, Canada". Journal of Wildlife Diseases 42 (1): 115–32. January 2006. doi:10.7589/0090-3558-42.1.115. PMID 16699154.
- ↑ Felig, PHILIP; Sherwin, ROBERT S.; Soman, VIJAY; Wahren, JOHN; Hendler, ROSA; Sacca, LUIGI; Eigler, NEIL; Goldberg, DAVID et al. (1979-01-01), Greep, ROY O., ed., "Hormonal Interactions in the Regulation of Blood Glucose" (in en), Proceedings of the 1978 Laurentian Hormone Conference, Recent Progress in Hormone Research (Boston: Academic Press) 35: pp. 501–532, ISBN 978-0-12-571135-7, https://www.sciencedirect.com/science/article/pii/B9780125711357500163, retrieved 2023-04-09
- ↑ Lehninger, Albert; Nelson, David; Cox, Michael (2017). Lehininger Principles of Biochemistry. New York: W.H. Freedom. p. 934. ISBN 9781319117689.
- ↑ Tortora, Gerard (December 2016). Principles Anatomy and Physiology (15 ed.). New York: John Wiley & Sons, Inc.. pp. Chapter 18. ISBN 9781119343738.
- ↑ Lehninger, Albert; Nelson, David; Cox, Michael (2017). Lehninger Principles of Biochemistry (7th ed.). New York: W.H.Freeman. p. 930. ISBN 9781319117689.
- ↑ "Excess sugar linked to cancer" (in en). Science Daily. https://www.sciencedaily.com/releases/2013/02/130201100149.htm.
- ↑ "Diabetic ketoacidosis - Symptoms and causes" (in en). Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/diabetic-ketoacidosis/symptoms-causes/syc-20371551.
- ↑ "Diabetic emergencies: Warning signs and what to do" (in en). 2019-03-28. https://www.medicalnewstoday.com/articles/317436.
- ↑ Australia, Healthdirect (2023-11-28). "Hyperglycaemia (high blood sugar)" (in en-AU). https://www.healthdirect.gov.au/hyperglycaemia-high-blood-sugar.
- ↑ Consumer Reports Health Best Buy Drugs. "The Oral Diabetes Drugs: Treating Type 2 Diabetes". Best Buy Drugs: 2. http://www.consumerreports.org/health/resources/pdf/best-buy-drugs/DiabetesUpdate-FINAL-Feb09.pdf. Retrieved 18 September 2012.
- ↑ Fowler, Michael J. (2007-06-22). "Diet and exercise." (in English). Clinical Diabetes 25 (3): 105–110. https://go.gale.com/ps/i.do?p=AONE&sw=w&issn=08918929&v=2.1&it=r&id=GALE%7CA167029985&sid=googleScholar&linkaccess=abs.
- ↑ "Steroid medications and diabetes fact sheet – NDSS". https://www.ndss.com.au/about-diabetes/resources/find-a-resource/steroid-medications-and-diabetes-fact-sheet/.
- ↑ "Low blood sugar - self-care: MedlinePlus Medical Encyclopedia" (in en). medlineplus.gov. https://medlineplus.gov/ency/patientinstructions/000085.htm.
- ↑ "Studies of arteriovenous differences in blood sugar; effect of alimentary hyperglycemia on the rate of extrahepatic glucose assimilation". The Journal of Biological Chemistry 174 (1): 189–200. May 1948. doi:10.1016/S0021-9258(18)57386-5. PMID 18914074. http://www.jbc.org/content/174/1/189.full.pdf.
- ↑ Roe, Jeffrey. "Glucose Concentration Difference Between Arterial, Capillary, and Venous Blood". Best Thinking. http://www.bestthinking.com/articles/medicine/internal_medicine/hematology/glucose-concentration-difference-between-arterial-capillary-and-venous-blood.
- ↑ Cox, David L; Nelson, Michael M. (2013). Lehninger principles of biochemistry (6th ed.). New York: W.H. Freeman. pp. 950. ISBN 9781429234146.
- ↑ 34.0 34.1 Cox, Michael M.; Lehninger, Albert L.; Nelson, David L. (2017). Lehninger Principles of Biochemistry. New York: W.H. Freeman. pp. 248–49. ISBN 9781319117689.
- ↑ "Factors affecting blood glucose monitoring: sources of errors in measurement". Journal of Diabetes Science and Technology 3 (4): 903–13. July 2009. doi:10.1177/193229680900300438. PMID 20144340.
- ↑ Singer, D. E.; Coley, C. M.; Samet, J. H.; Nathan, D. M. (1989-01-15). "Tests of glycemia in diabetes mellitus. Their use in establishing a diagnosis and in treatment". Annals of Internal Medicine 110 (2): 125–137. doi:10.7326/0003-4819-110-2-125. ISSN 0003-4819. PMID 2642375. https://pubmed.ncbi.nlm.nih.gov/2642375.
- ↑ "[The upper limit of glucose concentration in the urine of healthy subjects]". Deutsche Medizinische Wochenschrift 90 (53): 2349–53. December 1965. PMID 5851934.
- ↑ Tankasala, D; Linnes, JC (November 2019). "Noninvasive glucose detection in exhaled breath condensate.". Translational Research 213: 1–22. doi:10.1016/j.trsl.2019.05.006. PMID 31194942.
- ↑ "Neocuproine MSDS". http://hazard.com/msds/mf/baker/baker/files/d6824.htm.
Further reading
- Henry, John Bernard (2001). Clinical diagnosis and Management by Laboratory Methods (20th ed.). Philadelphia: Saunders. ISBN 978-0721688640.
- "Monosaccharides in health and disease". Annual Review of Nutrition 6: 211–24. 1986. doi:10.1146/annurev.nu.06.070186.001235. PMID 3524617.
- "Pancreatic regulation of glucose homeostasis". Experimental & Molecular Medicine 48 (3, March): e219. March 2016. doi:10.1038/emm.2016.6. PMID 26964835.
External links
- Glucose (blood, serum, plasma): analyte monograph – The Association for Clinical Biochemistry and Laboratory Medicine
 |