Biology:Alanine transaminase
| Alanine transaminase | |||||||||
|---|---|---|---|---|---|---|---|---|---|
 | |||||||||
| Identifiers | |||||||||
| EC number | 2.6.1.2 | ||||||||
| CAS number | 9000-86-6 | ||||||||
| Databases | |||||||||
| IntEnz | IntEnz view | ||||||||
| BRENDA | BRENDA entry | ||||||||
| ExPASy | NiceZyme view | ||||||||
| KEGG | KEGG entry | ||||||||
| MetaCyc | metabolic pathway | ||||||||
| PRIAM | profile | ||||||||
| PDB structures | RCSB PDB PDBe PDBsum | ||||||||
| Gene Ontology | AmiGO / QuickGO | ||||||||
| |||||||||
Alanine transaminase (ALT) is a transaminase enzyme (EC 2.6.1.2). It is also called alanine aminotransferase (ALT or ALAT) and was formerly called serum glutamate-pyruvate transaminase or serum glutamic-pyruvic transaminase (SGPT) and was first characterized in the mid-1950s by Arthur Karmen and colleagues.[1] ALT is found in plasma and in various body tissues but is most common in the liver. It catalyzes the two parts of the alanine cycle. Serum ALT level, serum AST (aspartate transaminase) level, and their ratio (AST/ALT ratio) are routinely measured clinically as biomarkers for liver health.[citation needed]
The half-life of ALT in the circulation approximates 47 hours.[2] Aminotransferase is cleared by sinusoidal cells in the liver.[2]
Function
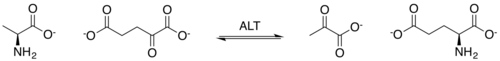
ALT catalyzes the transfer of an amino group from L-alanine to α-ketoglutarate, the products of this reversible transamination reaction being pyruvate and L-glutamate.[citation needed]
- L-alanine + α-ketoglutarate ⇌ pyruvate + L-glutamate
ALT (and all aminotransferases) require the coenzyme pyridoxal phosphate, which is converted into pyridoxamine in the first phase of the reaction, when an amino acid is converted into a keto acid.[citation needed]
Clinical significance
ALT is commonly measured clinically as part of liver function tests and is a component of the AST/ALT ratio.[3] When used in diagnostics, it is almost always measured in international units/liter (IU/L)[4] or µkat. While sources vary on specific reference range values for patients, 0-40 IU/L is the standard reference range for experimental studies.[3]
Elevated levels
Test results should always be interpreted using the reference range from the laboratory that produced the result. However typical reference intervals for ALT are:
| Patient type | Reference ranges[5] |
| Male | ≤ 45 IU/L |
| Female | ≤ 34 IU/L |
Significantly elevated levels of ALT (SGPT) often suggest the existence of other medical problems such as viral hepatitis, diabetes, congestive heart failure, liver damage, bile duct problems, infectious mononucleosis, or myopathy, so ALT is commonly used as a way of screening for liver problems.[citation needed] Elevated ALT may also be caused by dietary choline deficiency.[citation needed] However, elevated levels of ALT do not automatically mean that medical problems exist. Fluctuation of ALT levels is normal over the course of the day, and they can also increase in response to strenuous physical exercise.[6]
When elevated ALT levels are found in the blood, the possible underlying causes can be further narrowed down by measuring other enzymes. For example, elevated ALT levels due to hepatocyte damage can be distinguished from bile duct problems by measuring alkaline phosphatase. Also, myopathy-related elevations in ALT should be suspected when the aspartate transaminase (AST) is greater than ALT; the possibility of muscle disease causing elevations in liver tests can be further explored by measuring muscle enzymes, including creatine kinase. Many drugs may elevate ALT levels, including zileuton, omega-3 acid ethyl esters (Lovaza),[7] anti-inflammatory drugs, antibiotics, cholesterol medications, some antipsychotics such as risperidone, and anticonvulsants.[citation needed] Paracetamol (acetaminophen) may also elevate ALT levels.[8]
For years, the American Red Cross used ALT testing as part of the battery of tests to ensure the safety of its blood supply by deferring donors with elevated ALT levels. The intent was to identify donors potentially infected with hepatitis C because no specific test for that disease was available at the time. Prior to July 1992, widespread blood donation testing in the US for hepatitis C was not carried out by major blood banks. With the introduction of second-generation ELISA antibody tests for hepatitis C, the Red Cross changed the ALT policy. (As of July 2003), donors previously disqualified for elevated ALT levels and no other reason may be reinstated as donors when they contact the donor-counseling department of their regional Red Cross organization.[9]
In 2000, the American Association for Clinical Chemistry determined that the appropriate terminology for AST and ALT are aspartate aminotransferase and alanine aminotransferase. The term transaminase is outdated and no longer used in liver disease.[10]
See also
References
- ↑ "Transaminase activity in human blood". The Journal of Clinical Investigation 34 (1): 126–31. January 1955. doi:10.1172/JCI103055. PMID 13221663.
- ↑ 2.0 2.1 "Liver enzyme alteration: a guide for clinicians". Canadian Medical Association Journal 172 (3): 367–79. February 2005. doi:10.1503/cmaj.1040752. PMID 15684121. "Aminotransferase clearance is carried out within the liver by sinusoidal cells. The half-life in the circulation is about 47 hours for ALT, about 17 hours for total AST and, on average, 87 hours for mitochondrial AST.".
- ↑ 3.0 3.1 "Liver Function Tests". Stat Pearls (Treasure Island (FL): StatPearls Publishing). July 2020. PMID 29494096.
- ↑ "Liver enzymes, nonalcoholic fatty liver disease, and incident cardiovascular disease: a narrative review and clinical perspective of prospective data". Hepatology 52 (3): 1156–61. September 2010. doi:10.1002/hep.23789. PMID 20658466.
- ↑ "Alanine aminotransferase: analyte monograph". Association for Clinical Biochemistry and Laboratory Medicine. 2012. pp. 3–7. http://www.acb.org.uk/Nat%20Lab%20Med%20Hbk/ALT.pdf.
- ↑ "Mildly elevated liver transaminase levels in the asymptomatic patient". American Family Physician 71 (6): 1105–10. March 2005. PMID 15791889. http://www.aafp.org/afp/20050315/1105.html.
- ↑ "Pieter Dullemeijer, professor of animal morphology". Acta Morphologica Neerlando-Scandinavica 27 (1–2): 9–16. 2008. PMID 2683599.
- ↑ "Aminotransferase elevations in healthy adults receiving 4 grams of acetaminophen daily: a randomized controlled trial". JAMA 296 (1): 87–93. July 2006. doi:10.1001/jama.296.1.87. PMID 16820551.
- ↑ Van Ostrand, Darla. "Red Cross Donor Requirements". American Red Cross of Tompkins County. http://www.tompkins-redcross.org/donor_req.htm.
- ↑ "Diagnosis and monitoring of hepatic injury. I. Performance characteristics of laboratory tests". Clinical Chemistry 46 (12): 2027–49. December 2000. doi:10.1093/clinchem/46.12.2027. PMID 11106349.
External links
- Alanine+transaminase at the US National Library of Medicine Medical Subject Headings (MeSH)
- ALT: analyte monograph; The Association for Clinical Biochemistry and Laboratory Medicine
- Alanine aminotransferase (ALT) at Lab Tests Online
{{Navbox
| name = Glycolysis enzymes | title = Metabolism: carbohydrate metabolism: [[Biology:Glycoglycolysis/gluconeogenesis enzymes | state = autocollapse | listclass = hlist
| group1 = Glycolysis
| list1 =
| |
| group2 = Gluconeogenesis only| list2 =
| to oxaloacetate: | |
|---|---|
| from lactate (Cori cycle): | |
| from alanine (Alanine cycle): | |
| from glycerol: |
| group4 = Regulatory | list4 =
}}
 |