Medicine:Kabuki syndrome
| Kabuki syndrome | |
|---|---|
| Other names | Niikawa–Kuroki syndrome |
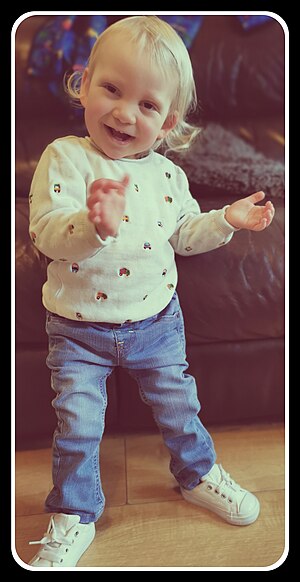 | |
| A child with kabuki syndrome displaying the “scrunchy face” | |
| Symptoms | Vary widely among patients but may include: Long eyelashes, depressed nasal tip, atypical fingerprints, ear deformity (macrotia or microtia), hypotonia, joint hyperflexibility, ptosis, blue sclera, cafe au lait spot, GU anomalies (e.g. hypospadias or horseshoe kidney), gi anomalies (e.g. anal atresia or intestinal malformation), hearing loss, immune deficiencies (e.g. hypogammaglobinemia), feeding difficulty (infants), obesity (adulthood), short stature, poor sleep, hyperinsulinemia (hypoglycemia), epilepsy, cardiac defects (e.g. coarctation of the aorta), vertebral anamolies (e.g. butterfly vertebrae), sparse lateral eyelash, finger anomaly (e.g. short 5th finger), cleft palate, dental issues, precocious puberty, scoliosis, hip dysplasia |
| Usual onset | Conception |
| Types | Type 1 (KMT2D), type 2 (KDM6A); other rare mutations unrecognized for now |
| Causes | Loss-of-function mutations in KMT2D or KDM6A genes |
| Diagnostic method | Clinical findings; genetic testing |
| Frequency | 1 in 32,000 births |
Kabuki syndrome (also previously known as Kabuki-makeup syndrome (KMS) or Niikawa–Kuroki syndrome) is a congenital disorder of genetic origin.[1][2] It affects multiple parts of the body, with varying symptoms and severity, although the most common is the characteristic facial appearance.[3]
It is quite rare, affecting roughly one in 32,000 births.[4] It was first identified and described in 1981 by two Japanese groups, led by scientists Norio Niikawa and Yoshikazu Kuroki.[5] It is named Kabuki syndrome because of the facial resemblance of affected individuals to stage makeup used in kabuki, a Japanese traditional theatrical form.[4]
Signs and symptoms
Specific symptoms for Kabuki syndrome vary, with large differences between affected individuals.[3] Most people with Kabuki syndrome have distinctive facial features that include arched eyebrows, long eyelashes, elongated eyelids with lower lids that turn out, prominent ears, a flat tip of the nose and a downward slant to the mouth.[3][4]
Overlapping phenotypic features for patients between KDM6A and KDM6B variations include prominent ears, abnormal dentition, congenital heart disease, feeding difficulties, cryptorchidism, joint hypermobility, developmental delay, hypotonia, and behavioral difficulties.
Other common symptoms are skeletal abnormalities, short stature, heart defects, feeding difficulties and a failure to thrive, vision and hearing difficulties, weak muscle tone (hypotonia), small head size (microcephaly), and frequent infections.[3]
Mild to moderate intellectual disability and mild to severe developmental delay are often associated with Kabuki syndrome.[3][4][6] Infants and young children often experience difficulties relating to hypotonia, feeding issues/failure to thrive, infections, surgical repair of heart and palate defects and developmental delays.[citation needed]
Young children with Kabuki syndrome benefit from early intervention services. School age children tend to have fewer medical issues requiring hospitalization, though frequent infections, hearing loss and feeding issues occur. In addition, intellectual impairment, difficulty with visuospatial tasks and maintaining attention usually require an IEP (individualized education plan) if the child attends public school. Older children and adults report difficulties with anxiety. Endocrine abnormalities and immune system abnormalities such as ITP (idiopathic thrombocytopenia) and CVID (common variable immune deficiency) are medical issues that tend to present in older children, adolescents and adults.[7]
Causes
Type 1 Kabuki syndrome is caused by germline heterozygous loss of function variants in KMT2D (formerly known as the MLL2), located on human chromosome 12.[2] It is estimated that between 55 and 80% of cases of Kabuki syndrome are of Type 1.[8][9][10][11] Type 1 Kabuki syndrome demonstrates an autosomal dominant pattern of inheritance.
Type 2 Kabuki syndrome is caused by germline hemizygous (in males) or heterozygous (in females) chromosome deletions[12] or loss of function point variants[13] involving KDM6A, located on the X chromosome. Approximately 5% of cases of Kabuki syndrome are of Type 2. Type 2 Kabuki syndrome demonstrates an X-linked dominant pattern of inheritance.[14]
Most cases of Kabuki syndrome occur de novo, that is, the parents are unaffected and the gene was mutated early in embryological development. However, several cases of inherited mutations causing Type 1 or Type 2 Kabuki syndrome are now known.[10][14]
Some cases of Kabuki syndrome have no identifiable causative mutation.[4] These may represent individuals with types of mutations that are challenging to detect via current routine investigations or patients who have disorders that share some features with Kabuki syndrome.
Pathophysiology
The KMT2D and KDM6A genes belong to a family of genes called chromatin-modifying enzymes. Specifically, these genes code for a histone methyltransferase (KMT2D) and a histone demethylase (KDM6A), and play a part in the regulation of gene expression.[15] Under normal circumstances, these enzymes transfer methyl groups on and off histones to regulate genes via epigenetic pathways. When the genes that encode these enzymes are mutated, epigenetic activation of certain developmental genes is impaired and developmental abnormalities occur, leading to the characteristics of Kabuki syndrome patients.[15] The specific developmental genes that are affected by the impaired epigenetic mechanisms in Kabuki syndrome are not yet fully known.[15]
There are hundreds of different mutations that have been identified in Kabuki syndrome patients. Most of these mutations are in the KMT2D gene and involve a change in amino acid sequence that creates a shortened and nonfunctional chromatin-modifying enzyme.[11]
Diagnosis
A consensus on clinical diagnostic criteria for Kabuki syndrome (KS) was defined in December 2018 by an international group of experts.[10] The authors propose that a definitive diagnosis can be made in an individual of any age with a history of infantile hypotonia, developmental delay and/or intellectual disability, and one or both of the following major criteria: (1) a pathogenic or likely pathogenic variant in KMT2D or KDM6A; and (2) typical dysmorphic features (defined below) at some point of life. Typical dysmorphic features include long palpebral fissures with eversion of the lateral third of the lower eyelid and two or more of the following: (1) arched and broad eyebrows with the lateral third displaying notching or sparseness; (2) short columella with depressed nasal tip; (3) large, prominent or cupped ears; and (4) persistent fingertip pads. Further criteria for a probable and possible diagnosis, including a table of suggestive clinical features, were included in the publication.[10]
The original description of Kabuki syndrome by Niikawa et al.[16] defined five cardinal manifestations, although some of these “cardinal manifestations” may or may not be present in a patient with Kabuki syndrome.
- Typical facial features: Elongated palpebral fissures with eversion of the lateral third of the lower eyelid; arched and broad eyebrows with the lateral third displaying sparseness or notching; short columella with depressed nasal tip; large, prominent, or cupped ears[16][17][9][18][19]
- Skeletal anomalies: Spinal column abnormalities, including sagittal cleft vertebrae, butterfly vertebrae, narrow intervertebral disc space, and/or scoliosis, Brachydactyly V Brachymesophalangy Clinodactyly of fifth digits
- Dermatoglyphic abnormalities: persistence of fetal fingertip pads
- Mild to moderate intellectual disability
- Postnatal growth deficiency
Kabuki syndrome is diagnosed with genetic testing (targeted, whole exome or whole genome sequencing).[3] When genetic testing is not available, Kabuki syndrome is diagnosed clinically (through identifying symptoms, physical exams, and lab results), most commonly by a geneticist.
Diagnosis can be difficult given the large spectrum of disease. The fact that some patients do not carry one of the two known mutations or can carry multiple mutations complicates the diagnosis further.[citation needed]
Screening
Due to its rarity, Kabuki syndrome is not screened for in routine prenatal testing including blood tests, chorionic villus sampling (CVS), or amniocentesis. Although not routine for the general population, if Kabuki syndrome is a specific concern (i.e. expectant mother who has been diagnosed with Kabuki syndrome or sibling with KS), it is possible to test for one of the specific mutations.[4] This prenatal testing does require a CVS or amniocentesis. However Kabuki syndrome is usually not inherited and therefore most cases do not have a positive family history.[3][4] Kabuki syndrome can have positive screening tests, such as cystic hygroma seen on nuchal translucency ultrasound screening, although these findings are non-specific and have a wide differential diagnosis.[20][21]
Management
Newly diagnosed patients with Kabuki syndrome will often undergo tests that are aimed at detecting common abnormalities associated with the syndrome. They include an echocardiogram (ultrasound of the heart) for detection of structural heart defects, kidney ultrasound for detection of structural renal abnormalities, immunoglobulin levels, pneumococcal titers and a hearing screening test. Further evaluation and testing by specialists may be indicated in addition to cardiology, nephrology, allergy/immunology, audiology-mentioned above. This may include orthopedics (such as hip dysplasia), pulmonary (sleep study to rule out obstructive sleep apnea due to hypotonia), ophthalmology evaluation (vision screen), ENT evaluation (hearing evaluation), Neurology evaluation (i.e. if seizures present), Hematology evaluation (if bleeding disorder), GI evaluation (if gi abnormalities), or others as needed. A summary of recommended evaluations can be found here.
There is no specific treatment for Kabuki syndrome. Treatment plans are customized to address the symptoms the individual is experiencing.[15] For example, someone experiencing seizures will be treated with the standard anti-epilepsy therapies.[15] Additionally, patients with Kabuki syndrome are routinely evaluated and monitored to address problems that may develop, such as vision or hearing problems, or cognitive difficulties.[15] If congenital heart disease is present, prophylactic antibiotics may be recommended before any procedures such as dental work that might cause infection.[15]
Prognosis
Life expectancy is not shortened in most cases of Kabuki syndrome. Some patients have coexisting conditions which may shorten life expectancy, such as hypoplastic left heart syndrome or kidney dysfunction. It is important that patients with cardiac, renal, or immunologic issues are identified and well-managed.[3]
Epidemiology
Kabuki syndrome occurs about once in every 32,000 births.[4][16] The disease appears to affect all population groups equally, with no differences based on sex, race, or environment.[22]
Research
Research on Kabuki syndrome is extremely limited due to its low incidence.[4] Despite this, several groups around the world are studying Kabuki syndrome. In the United States, these include the Epigenetics and Chromatin Clinic at Johns Hopkins University (led by Dr. Hans Bjornsson), The Roya Kabuki Program at Boston Children's Hospital, Dr. Mark Hannibal at the University of Michigan, groups at University of Colorado, University of Utah, University of South Florida and others.[23][24] In the UK, Prof Siddharth Banka's group at the University of Manchester and Manchester University Hospitals has a research program for Kabuki syndrome. Several European groups based in Italy, France, Germany and the Netherlands are also actively working on improving understanding of the condition and to identifying potential treatments. The Kabuki Syndrome Foundation was established in 2018 to accelerate research efforts to treat or cure Kabuki syndrome.
History
In 1969, Norio Niikawa MD, a geneticist in Japan was treating a child patient presenting with unique facial characteristics and various health problems. Never having seen this constellation of symptoms before, Dr Niikawa wondered if he was faced with an undiagnosed condition, a disorder with a genetic basis. Over the next several years, this physician treated several other patients with the same symptoms in his outpatient genetics clinic, furthering support for a disorder never before diagnosed.[25]
In 1979, Dr Niikawa presented his findings and hypothesis at the first Japan Dysmorphology Conference. A fellow physician at this conference, Yoshikazu Kuroki, recognized the symptoms, and realized that he had also seen several paediatric patients with this presentation; he presented two of his own cases at the second annual conference the following year. In 1981, the two doctors separately submitted articles on this new diagnosis to the Journal of Pediatrics.[5][25][26]
Dr Niikawa coined the term 'Kabuki syndrome' (also known as Kabuki make-up syndrome or Niikawa–Kuroki syndrome) as a reference to traditional Japanese theatre which he respected greatly. Many of the children presenting with this diagnosis had unusual, elongated lower eyelids, and this feature was reminiscent of the theatrical make-up worn by actors in Kabuki theatre.[27][28]
As reported by Dr. Niikawa "The name, 'Kabuki make-up', of the syndrome was given by myself, because the facial appearance of patients, especially eversion of their lower eyelids, is reminiscent of the makeup of actors in Kabuki, the traditional form of Japanese theater. Kabuki was founded early in the 17th century in Japan and over the next 300 years developed into a sophisticated form of theater. Kabuki actors usually apply traditional makeup to strengthen their eyes, especially in a hero play, and they are very proud of their performing art."[29]
The individual kanji, from left to right, mean sing (歌), dance (舞), and skill (伎). Kabuki is therefore sometimes translated as "the art of singing and dancing".
In popular culture
Television and Film
- The Good Doctor is an American medical drama television series that airs on ABC. Season five's ninth episode features Matthew Horner, an actor with Kabuki syndrome. Horner is likely the first actor with Kabuki syndrome to be cast in a major network TV drama.[30]
- Nineteen Paper Cranes is a short documentary by Michael Joseph McDonald. The film follows a deaf Japanese papermaker with Kabuki syndrome as she memorializes the nineteen victims of the Sagamihara stabbings.[31]
References
- ↑ "Kabuki Syndrome Gene Identified". National Institutes of Health (NIH). 2015-05-20. http://www.nih.gov/researchmatters/august2010/08232010kabuki.htm.
- ↑ 2.0 2.1 "Exome sequencing identifies MLL2 mutations as a cause of Kabuki syndrome". Nature Genetics 42 (9): 790–793. September 2010. doi:10.1038/ng.646. PMID 20711175.
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 3.6 3.7 "Kabuki syndrome". Genetic and Rare Diseases Information Center (GARD) – an NCATS Program. https://rarediseases.info.nih.gov/diseases/6810/kabuki-syndrome.
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 4.6 4.7 4.8 "Kabuki syndrome". Genetics Home Reference, U.S. National Library of Medicine. http://ghr.nlm.nih.gov/condition/kabuki-syndrome.
- ↑ 5.0 5.1 "A new malformation syndrome of long palpebral fissures, large ears, depressed nasal tip, and skeletal anomalies associated with postnatal dwarfism and mental retardation". The Journal of Pediatrics 99 (4): 570–573. October 1981. doi:10.1016/S0022-3476(81)80256-9. PMID 7277097.
- ↑ "Developmental outcome in Kabuki syndrome". American Journal of Medical Genetics. Part A 132A (3): 263–264. January 2005. doi:10.1002/ajmg.a.30338. PMID 15523636.
- ↑ (in en) Kabuki Syndrome. University of Washington, Seattle. 2019-10-21. https://www.ncbi.nlm.nih.gov/sites/books/NBK62111/.
- ↑ "How genetically heterogeneous is Kabuki syndrome?: MLL2 testing in 116 patients, review and analyses of mutation and phenotypic spectrum". European Journal of Human Genetics 20 (4): 381–388. April 2012. doi:10.1038/ejhg.2011.220. PMID 22126750.
- ↑ 9.0 9.1 "Spectrum of MLL2 (ALR) mutations in 110 cases of Kabuki syndrome". American Journal of Medical Genetics. Part A 155A (7): 1511–1516. July 2011. doi:10.1002/ajmg.a.34074. PMID 21671394.
- ↑ 10.0 10.1 10.2 10.3 "Kabuki syndrome: international consensus diagnostic criteria". Journal of Medical Genetics 56 (2): 89–95. February 2019. doi:10.1136/jmedgenet-2018-105625. PMID 30514738.
- ↑ 11.0 11.1 "Unmasking Kabuki syndrome". Clinical Genetics 83 (3): 201–211. March 2013. doi:10.1111/cge.12051. PMID 23131014.
- ↑ "Deletion of KDM6A, a histone demethylase interacting with MLL2, in three patients with Kabuki syndrome". American Journal of Human Genetics 90 (1): 119–124. January 2012. doi:10.1016/j.ajhg.2011.11.021. PMID 22197486.
- ↑ "Novel KDM6A (UTX) mutations and a clinical and molecular review of the X-linked Kabuki syndrome (KS2)". Clinical Genetics 87 (3): 252–258. March 2015. doi:10.1111/cge.12363. PMID 24527667.
- ↑ 14.0 14.1 "Clinical delineation, sex differences, and genotype-phenotype correlation in pathogenic KDM6A variants causing X-linked Kabuki syndrome type 2". Genetics in Medicine 23 (7): 1202–1210. July 2021. doi:10.1038/s41436-021-01119-8. PMID 33674768.
- ↑ 15.0 15.1 15.2 15.3 15.4 15.5 15.6 Adam, M. P.; Everman, D. B.; Mirzaa, G. M.; Pagon, R. A.; Wallace, S. E.; Bean LJH; Gripp, K. W.; Amemiya, A. et al. (16 May 2013). "Kabuki Syndrome". GeneReviews [Internet]. PMID 21882399. https://www.ncbi.nlm.nih.gov/books/NBK62111/.
- ↑ 16.0 16.1 16.2 "Kabuki make-up syndrome: a syndrome of mental retardation, unusual facies, large and protruding ears, and postnatal growth deficiency". The Journal of Pediatrics 99 (4): 565–569. October 1981. doi:10.1016/S0022-3476(81)80255-7. PMID 7277096.
- ↑ "Thirteen cases of Niikawa-Kuroki syndrome: report and review with emphasis on medical complications and preventive management". American Journal of Medical Genetics 79 (2): 112–120. September 1998. doi:10.1002/(SICI)1096-8628(19980901)79:2<112::AID-AJMG7>3.0.CO;2-S. PMID 9741469.
- ↑ "Kabuki syndrome: Clinical data in 20 patients, literature review, and further guidelines for preventive management". American Journal of Medical Genetics. Part A 132A (3): 234–243. January 2005. doi:10.1002/ajmg.a.30331. PMID 15690368.
- ↑ "Further delineation of Kabuki syndrome in 48 well-defined new individuals". American Journal of Medical Genetics. Part A 132A (3): 265–272. January 2005. doi:10.1002/ajmg.a.30340. PMID 15690370.
- ↑ "Kabuki syndrome as a cause of non-immune fetal hydrops/ascites". American Journal of Medical Genetics. Part A 170 (12): 3333–3337. December 2016. doi:10.1002/ajmg.a.37956. PMID 27568880.
- ↑ "[First-trimester cystic hygroma: prenatal diagnosis and fetal outcome]". Journal de Gynécologie, Obstétrique et Biologie de la Reproduction 43 (6): 455–462. June 2014. doi:10.1016/j.jgyn.2013.04.005. PMID 23747217.
- ↑ "Kabuki Syndrome - NORD (National Organization for Rare Disorders)". NORD (National Organization for Rare Disorders). https://rarediseases.org/rare-diseases/kabuki-syndrome/.
- ↑ "Kabuki Syndrome | Boston Children's Hospital". http://www.childrenshospital.org/conditions-and-treatments/conditions/k/kabuki-syndrome.
- ↑ Johns Hopkins Medicine (2015-10-07), #TomorrowsDiscoveries: Intellectual Disability Treatments — Dr. Hans Bjornsson, https://www.youtube.com/watch?v=BVLSJvYYaGA, retrieved 2018-04-24
- ↑ 25.0 25.1 "Kabuki make-up syndrome: a review". American Journal of Medical Genetics. Part C, Seminars in Medical Genetics 117C (1): 57–65. February 2003. doi:10.1002/ajmg.c.10020. PMID 12561059.
- ↑ "Kabuki make-up syndrome: a syndrome of mental retardation, unusual facies, large and protruding ears, and postnatal growth deficiency". The Journal of Pediatrics 99 (4): 565–569. October 1981. doi:10.1016/s0022-3476(81)80255-7. PMID 7277096.
- ↑ "Kabuki syndrome: Clinical data in 20 patients, literature review, and further guidelines for preventive management". American Journal of Medical Genetics. Part A 132A (3): 234–243. January 2005. doi:10.1002/ajmg.a.30331. PMID 15690368.
- ↑ "Kabuki syndrome: diagnostic and treatment considerations". Mental Health in Family Medicine 9 (3): 171–179. September 2012. PMID 23997823.
- ↑ "Niikawa Presentation". http://istituti.unicatt.it/genetica-medica-Niikawa_Kabuki.pdf.
- ↑ https://www.wmar2news.com/brittney-verner+(2022-03-07).+"Local doctor and patient featured on ABC's The Good Doctor" (in en). https://www.wmar2news.com/news/local-news/local-doctor-and-patient-featured-on-abcs-the-good-doctor.
- ↑ "19 Paper Cranes – Global Justice Film Festival" (in en). http://globaljusticefilmfestival.ca/films/detail/19-paper-cranes.
External links
| Website | |
|---|---|
| Patient Advocacy | All Things Kabuki |
| Kabuki UK | |
| Supporting Aussie Kids with Kabuki Syndrome (SAKKS) | |
| Association Syndrome Kabuki | |
| Research | Kabuki Syndrome Foundation |
| Roya Kabuki Program | |
| Conferences/Gatherings | Texas Kabuki Gathering |
| Classification | |
|---|---|
| External resources |
 |



