Medicine:Microcephaly
Microcephaly (from Neo-Latin microcephalia, from Ancient Greek μικρός mikrós "small" and κεφαλή kephalé "head"[1]) is a medical condition involving a smaller-than-normal head.[2] Microcephaly may be present at birth or it may develop in the first few years of life.[2] Brain development is often affected; people with this disorder often have an intellectual disability, poor motor function, poor speech, abnormal facial features, seizures and dwarfism.[2]
The disorder is caused by a disruption to the genetic processes that form the brain early in pregnancy,[2] though the cause is not identified in most cases.[3] Many genetic syndromes can result in microcephaly, including chromosomal and single-gene conditions, though almost always in combination with other symptoms. Mutations that result solely in microcephaly (primary microcephaly) exist but are less common.[4] External toxins to the embryo, such as alcohol during pregnancy or vertically transmitted infections, can also result in microcephaly.[2] Microcephaly serves as an important neurological indication or warning sign, but no uniformity exists in its definition. It is usually defined as a head circumference (HC) more than two standard deviations below the mean for age and sex.[5][6] Some academics advocate defining it as head circumference more than three standard deviations below the mean for the age and sex.[7]
There is no specific treatment that returns the head size to normal.[2] In general, life expectancy for individuals with microcephaly is reduced, and the prognosis for normal brain function is poor. Occasional cases develop normal intelligence and grow normally (apart from persistently small head circumference).[2][8] It is reported that in the United States, microcephaly occurs in 1 in 800-5,000 births.[3]
Signs and symptoms
There are a variety of symptoms that can occur in children. Infants with microcephaly are born with either a normal or reduced head size.[9] Subsequently, the head fails to grow, while the face continues to develop at a normal rate, producing a child with a small head and a receding forehead, and a loose, often wrinkled scalp.[10] As the child grows older, the smallness of the skull becomes more obvious, although the entire body also is often underweight and dwarfed.[9]
Severely impaired intellectual development is common, but disturbances in motor functions may not appear until later in life.[9] Affected newborns generally have striking neurological defects and seizures.[9] Development of motor functions and speech may be delayed. Hyperactivity and intellectual disability are common occurrences, although the degree of each varies. Convulsions may also occur. Motor ability varies, ranging from clumsiness in some to spastic quadriplegia in others.[11]
Causes
Microcephaly is a type of cephalic disorder. It has been classified in two types based on the onset:[12]
Congenital
- Isolated
- Familial (autosomal recessive) microcephaly[13]
- Autosomal dominant microcephaly[14][15]
- X-linked microcephaly[13]
- Chromosomal (balanced rearrangements and ring chromosome)
- Syndromes
- Chromosomal
- Poland syndrome[16]
- Down syndrome[17]
- Edward syndrome[18]
- Patau syndrome[19]
- Unbalanced rearrangements
- Contiguous gene deletion
- 4p deletion (Wolf–Hirschhorn syndrome)
- 5p deletion (Cri-du-chat)
- 7q11.23 deletion (Williams syndrome)
- 22q11 deletion (DiGeorge syndrome)
- Chromosomal
- Single gene defects
- Smith–Lemli–Opitz syndrome
- Seckel syndrome
- Cornelia de Lange syndrome
- Dihydropteridine reductase deficiency - in up to 25% of patients[20]
- 5,10-methenyltetrahydrofolate synthetase deficiency
- Holoprosencephaly
- Primary microcephaly[21]
- Wiedemann-Steiner syndrome
- Acquired
- Disruptive injuries
- Vertically transmitted infections
- Congenital cytomegalovirus infection[23]
- Toxoplasmosis[23]
- Congenital rubella syndrome[23]
- Congenital varicella syndrome[23]
- Zika virus (see Zika fever)[24]
- Drugs
- Fetal hydantoin syndrome[23]
- Fetal alcohol syndrome[23]
- Other
- Radiation exposure to mother
- Maternal malnutrition[23]
- Maternal phenylketonuria[23]
- Poorly controlled gestational diabetes
- Hyperthermia
- Maternal hypothyroidism
- Placental insufficiency
- Craniosynostosis[23]
Postnatal onset
- Genetic
- Inborn errors of metabolism
- Congenital disorder of glycosylation[25]
- Mitochondrial disorders[26]
- Peroxisomal disorder[27]
- Glucose transporter defect[28]
- Menkes disease
- Congenital disorders of amino acid metabolism[29]
- Organic acidemia[30]
- Inborn errors of metabolism
- Syndromes
- Contiguous gene deletion
- 17p13.3 deletion (Miller–Dieker syndrome)[31]
- Single gene defects
- Rett syndrome (primarily girls)
- Nijmegen breakage syndrome
- X-linked lissencephaly with abnormal genitalia
- Aicardi–Goutières syndrome
- Ataxia telangiectasia
- Cohen syndrome
- Cockayne syndrome
- Contiguous gene deletion
- Acquired
- Disruptive injuries
- Traumatic brain injury[32]
- Hypoxic-ischemic encephalopathy[23]
- Ischemic stroke[22]
- Hemorrhagic stroke[22]
- Infections
- Congenital HIV encephalopathy[33]
- Meningitis[34]
- Encephalitis[35]
- Toxins
- Chronic kidney failure[36]
- Deprivation
- Hypothyroidism[37]
- Anemia[38]
- Congenital heart disease[39]
- Malnutrition[40]
- Disruptive injuries
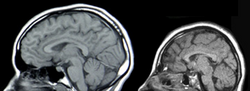
Genetic mutations cause most cases of microcephaly.[2] Relationships have been found between autism, duplications of genes and macrocephaly on one side. On the other side, a relationship has been found between schizophrenia, deletions of genes and microcephaly.[41][42][43] Several genes have been designated "MCPH" genes, after microcephalin (MCPH1), based on their role in brain size and primary microcephaly syndromes when mutated. In addition to microcephalin, these include WDR62 (MCPH2), CDK5RAP2 (MCPH3), KNL1 (MCPH4), ASPM (MCPH5), CENPJ (MCPH6), STIL (MCPH7), CEP135 (MCPH8), CEP152 (MCPH9), ZNF335 (MCPH10), PHC1 (MCPH11) and CDK6 (MCPH12).[4] Moreover, an association has been established between common genetic variants within known microcephaly genes (such as MCPH1 and CDK5RAP2) and normal variation in brain structure as measured with magnetic resonance imaging (MRI)—i.e., primarily brain cortical surface area and total brain volume.[44]
Arbovirus
Bites and stings from Arthropods can often be a cause of vector-borne diseases. These include mosquitoes, fleas, sand flies, lice, ticks, and mites that are hematophagous vectors. The Centers for Disease Control (CDC) stated that "mosquitoes kill more people than any other creature and considers that mosquitoes are "the most dangerous animals on earth".[45]
The spread of Aedes mosquito-borne Zika virus has been implicated in increasing levels of congenital microcephaly by the International Society for Infectious Diseases and the US Centers for Disease Control and Prevention.[46] Zika can spread from a pregnant woman to her fetus. This can result in other severe brain malformations and birth defects.[47][48][49][50] A study published in The New England Journal of Medicine has documented a case in which they found evidence of the Zika virus in the brain of a fetus that displayed the morphology of microcephaly.[51]
Microlissencephaly
Microlissencephaly is microcephaly combined with lissencephaly (smooth brain surface due to absent sulci and gyri). Most cases of microlissencephaly are described in consanguineous families, suggesting an autosomal recessive inheritance.[52][53][54]
Historical causes of microcephaly
After the dropping of atomic bombs "Little Boy" on Hiroshima and "Fat Man" on Nagasaki, several women close to ground zero who had been pregnant at the time gave birth to children with microcephaly.[55] Microcephaly was present in 7 children from a group of 11 pregnant women at 11–17 weeks of gestation who survived the blast at less than 1.2 km (0.75 mi) from ground zero.[56] Due to their proximity to the bomb, the pregnant women's in utero children received a biologically significant radiation dose that was relatively high due to the massive neutron output of the lower explosive-yielding Little Boy.[56] Researchers studied 286 additional children who were in utero during the atomic bombings, and after a year they found these children had a higher incidence of microcephaly and mental retardation.[57][56]
Other relations
Intracranial volume also affects this pathology, as it is related with the size of the brain.[58]
Pathophysiology
Microcephaly generally is due to the diminished size of the largest part of the human brain, the cerebral cortex, and the condition can arise during embryonic and fetal development due to insufficient neural stem cell proliferation, impaired or premature neurogenesis, the death of neural stem cells or neurons, or a combination of these factors.[59] Research in animal models such as rodents has found many genes that are required for normal brain growth. For example, the Notch pathway genes regulate the balance between stem cell proliferation and neurogenesis in the stem cell layer known as the ventricular zone, and experimental mutations of many genes can cause microcephaly in mice,[60] similar to human microcephaly.[61][62] Mutations of the abnormal spindle-like microcephaly-associated (ASPM) gene are associated with microcephaly in humans and a knockout model has been developed in ferrets that exhibits severe microcephaly.[63] In addition, viruses such as cytomegalovirus (CMV) or Zika have been shown to infect and kill the primary stem cell of the brain—the radial glial cell, resulting in the loss of future daughter neurons.[64][65] The severity of the condition may depend on the timing of infection during pregnancy. Microcephaly is a feature common to several different genetic disorders arising from a deficiency in the cellular DNA damage response.[66] Individuals with the following DNA damage response disorders exhibit microcephaly: Nijmegen breakage syndrome, ATR-Seckel syndrome, MCPH1-dependent primary microcephaly disorder, xeroderma pigmentosum complementation group A deficiency, Fanconi anemia, ligase 4 deficiency syndrome and Bloom syndrome. These findings suggest that a normal DNA damage response is critical during brain development, perhaps to protect against induction of apoptosis by DNA damage occurring in neurons.[67]
Treatment

There is no known cure for microcephaly.[2] Treatment is symptomatic and supportive.[2] Because some cases of microcephaly and its associated symptoms may be a result of amino acid deficiencies, treatment with amino acids in these cases has been shown to improve symptoms such as seizures and motor function delays.[68]
History
People with small heads were displayed as a public spectacle in ancient Rome.[69]
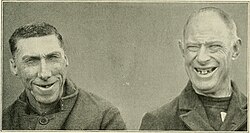
People with microcephaly were sometimes sold to freak shows in North America and Europe in the 19th and early 20th centuries, where they were known by the name "pinheads". Many of them were presented as different species (e.g., "monkey man") and described as being the missing link.[70] Famous examples include Zip the Pinhead (although he may not have had microcephaly), Maximo and Bartola and Schlitzie the Pinhead.[71] Stars of the 1932 film Freaks were cited as influences on the development of the long-running comic strip character Zippy the Pinhead, created by Bill Griffith.[72]
-
Triboulet, a French court jester, 1461
-
18-year-old Emil R., 1868
-
Elderly female, 1888/89
-
52-year-old female, 1900
-
10-year-old male, 1904
-
20-year-old female, 1906/07
-
3 relatives, 1913
-
18-year-old sister and 9-year-old brother, 1917
-
55-year-old female, 1920 (linear descendant of Pocahontas)
-
6 siblings, 1920
Notable cases
- A 'dwarf' of Punt (ancient Somalia) was given by the Chief clans as partial tribute to the last ruler of Ancient Egypt's Old Kingdom, Pepi II Neferkare (6th Dynasty, circa 2125–2080 BC); it could be inferred that this person was also microcephalic. In a letter preserved at the British Museum, the young king gives instructions by letter, "Harkhuf! The men in your service [escorts; soldiers; sailors; guards, etc.] ought pay sincere care with the dwarf's head while sleeping during the voyage to the palace" (so that it does not fall off). At the same time, it could be for other reasons unrelated to microcephaly, etc.[73]
- Triboulet, a jester of duke René of Anjou (not to be confused with the slightly later Triboulet at the French court).
- Jenny Lee Snow and Elvira Snow, whose stage names were Pip and Flip, respectively, were sisters with microcephaly who acted in the 1932 film Freaks.
- Schlitze "Schlitzie" Surtees, possibly born Simon Metz, was a widely known sideshow performer and actor, who also appeared in Freaks.
- Lester "Beetlejuice" Green, a member of radio host Howard Stern's Wack Pack.
- William Henry Johnson, an African American man from New Jersey who performed in freak shows under stage names What is It? and Zip the Pinhead.[74]
See also
- Anencephaly (Usually rapidly fatal)
- Cerebral rubicon
- Hydrocephaly
- Macrocephaly
- Seckel syndrome
- Achalasia microcephaly
- Oropouche orthobunyavirus
References
- ↑ "Microcephaly - Definition of Microcephaly by Merriam-Webster". http://www.merriam-webster.com/dictionary/microcephaly.
- ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 "NINDS Microcephaly Information Page". June 30, 2015. http://www.ninds.nih.gov/disorders/Microcephaly/microcephaly.htm.
- ↑ 3.0 3.1 "Facts about Microcephaly | Birth Defects | National Center on Birth Defects and Developmental Disabilities". 2016-12-07. https://www.cdc.gov/ncbddd/birthdefects/microcephaly.html.
- ↑ 4.0 4.1 Faheem, Muhammad; Naseer, Muhammad Imran; Rasool, Mahmood; Chaudhary, Adeel G; Kumosani, Taha A; Ilyas, Asad Muhammad; Pushparaj, Peter Natesan; Ahmed, Farid et al. (2015). "Molecular genetics of human primary microcephaly: an overview". BMC Medical Genomics 8 (Suppl 1): S4. doi:10.1186/1755-8794-8-S1-S4. PMID 25951892.
- ↑ Leviton, A.; Holmes, L.B.; Allred, E.N.; Vargas, J. (2002). "Methodologic issues in epidemiologic studies of congenital microcephaly". Early Hum Dev 69 (1): 91–105. doi:10.1016/S0378-3782(02)00065-8. PMID 12324187.
- ↑ Opitz, J. M.; Holt, M. C. (1990). "Microcephaly: general considerations and aids to nosology". Journal of Craniofacial Genetics and Developmental Biology 10 (2): 75–204. PMID 2211965.
- ↑ Behrman, R.E.; Kligman, R. M.; Jensen, H.B. (2000). Nelson's Textbook of Pediatrics (16th ed.). Philadelphia: WB Saunders. ISBN 978-0-7216-7767-5. OCLC 44552900. https://archive.org/details/nelsontextbookof00behr.
- ↑ Stoler-Poria, S.; Lev, D.; Schweiger, A.; Lerman-Sagie, T.; Malinger, G. (2010-01-12). "Developmental outcome of isolated fetal microcephaly". Ultrasound in Obstetrics and Gynecology (Wiley) 36 (2): 154–8. doi:10.1002/uog.7556. ISSN 0960-7692. PMID 20069548.
- ↑ 9.0 9.1 9.2 9.3 "Microcephaly". https://www.stanfordchildrens.org/en/topic/default?id=microcephaly-90-P02610.
- ↑ "Cephalic Disorders Fact Sheet". https://www.ninds.nih.gov/Disorders/Patient-Caregiver-Education/Fact-Sheets/Cephalic-Disorders-Fact-Sheet.
- ↑ "Microcephaly with Spastic Quadriplegia disease: Malacards - Research Articles, Drugs, Genes, Clinical Trials". https://www.malacards.org/card/microcephaly_with_spastic_quadriplegia.
- ↑ Ashwal, S.; Michelson, D.; Plawner, L.; Dobyns, W. B. (2009). "Practice Parameter: Evaluation of the child with microcephaly (an evidence-based review)". Neurology 73 (11): 887–897. doi:10.1212/WNL.0b013e3181b783f7. PMID 19752457.
- ↑ 13.0 13.1 "Microcephaly in Children". Health Encyclopedia. University of Rochester Medical Center. https://www.urmc.rochester.edu/encyclopedia/content.aspx?ContentTypeID=90&ContentID=P02610. Retrieved 2019-07-30.
- ↑ "Microcephaly autosomal dominant". Genetic and Rare Diseases Information Center. https://rarediseases.info.nih.gov/diseases/3605/microcephaly-autosomal-dominant.
- ↑ Online Mendelian Inheritance in Man (OMIM) Microcephaly 18, Primary, Autosomal Dominant; MCPH18 -617520
- ↑ "Poland syndrome". Genetic and Rare Diseases Information Center. https://rarediseases.info.nih.gov/diseases/7412/poland-syndrome.
- ↑ "Microcephaly". World Health Organization. https://www.who.int/news-room/fact-sheets/detail/microcephaly.
- ↑ "Trisomy 18: MedlinePlus Medical Encyclopedia" (in en). https://medlineplus.gov/ency/article/001661.htm.
- ↑ "Trisomy 13 | Genetic and Rare Diseases Information Center (GARD) – an NCATS Program". https://rarediseases.info.nih.gov/diseases/7341/trisomy-13.
- ↑ "Consensus guideline for the diagnosis and treatment of tetrahydrobiopterin (BH4) deficiencies". Orphanet Journal of Rare Diseases 15 (1): 126. May 2020. doi:10.1186/s13023-020-01379-8. PMID 32456656.
- ↑ Szczepanski, Sandra; Hussain, MuhammadSajid; Sur, Ilknur; Altmüller, Janine; Thiele, Holger; Abdullah, Uzma; Waseem, SyedaSeema; Moawia, Abubakar et al. (30 November 2015). "A novel homozygous splicing mutation of CASC5 causes primary microcephaly in a large Pakistani family". Human Genetics 135 (2): 157–170. doi:10.1007/s00439-015-1619-5. PMID 26621532.
- ↑ 22.0 22.1 22.2 22.3 "Microcephaly in infants and children: Etiology and evaluation". UpToDate. https://www.uptodate.com/contents/microcephaly-in-infants-and-children-etiology-and-evaluation.
- ↑ 23.00 23.01 23.02 23.03 23.04 23.05 23.06 23.07 23.08 23.09 "Microcephaly - Symptoms and causes". https://www.mayoclinic.org/diseases-conditions/microcephaly/symptoms-causes/syc-20375051.
- ↑ Emily E. Petersen; Erin Staples; Dana Meaney-Delman; Marc Fischer; Sascha R. Ellington; William M. Callaghan; Denise J. Jamieson (January 22, 2016). "Interim Guidelines for Pregnant Women During a Zika Virus Outbreak — United States, 2016". Morbidity and Mortality Weekly Report 65 (2): 30–33. doi:10.15585/mmwr.mm6502e1. PMID 26796813.
- ↑ "Congenital Disorders of Glycosylation". https://rarediseases.org/rare-diseases/congenital-disorders-of-glycosylation/.
- ↑ "Mito Info". https://www.mito.org.au/mito-info/.
- ↑ "Zellweger syndrome". https://www.orpha.net/consor/cgi-bin/OC_Exp.php?Lng=GB&Expert=912.
- ↑ Reference, Genetics Home. "GLUT1 deficiency syndrome". https://medlineplus.gov/genetics/condition/glut1-deficiency-syndrome/.
- ↑ "Maternal phenylketonuria". https://www.orpha.net/consor/cgi-bin/OC_Exp.php?Expert=2209&lng=EN.
- ↑ Reddy, Nihaal; Calloni, Sonia F.; Vernon, Hilary J.; Boltshauser, Eugen; Huisman, Thierry A. G. M.; Soares, Bruno P. (2018-05-01). "Neuroimaging Findings of Organic Acidemias and Aminoacidopathies". RadioGraphics 38 (3): 912–931. doi:10.1148/rg.2018170042. ISSN 0271-5333. PMID 29757724.
- ↑ Online Mendelian Inheritance in Man (OMIM) Miller-Dieker Lissencephaly Syndrome; MDLS -247200
- ↑ Joyce, Tina; Huecker, Martin R. (2019), "Pediatric Abusive Head Trauma (Shaken Baby Syndrome)", National Center for Biotechnology Information (AU.S. National Library of Medicine), PMID 29763011, https://www.ncbi.nlm.nih.gov/books/NBK499836/, retrieved 2019-07-30
- ↑ Donald, Kirsten A.; Walker, Kathleen G.; Kilborn, Tracy; Carrara, Henri; Langerak, Nelleke G; Eley, Brian; Wilmshurst, Jo M (2015). "HIV Encephalopathy: pediatric case series description and insights from the clinic coalface". AIDS Research and Therapy 12 (1): 2. doi:10.1186/s12981-014-0042-7. ISSN 1742-6405. PMID 25598835.
- ↑ Tibussek, Daniel; Sinclair, Adriane; Yau, Ivanna; Teatero, Sarah; Fittipaldi, Nahuel; Richardson, Susan E.; Mayatepek, Ertan; Jahn, Peter et al. (2015). "Late-Onset Group B Streptococcal Meningitis Has Cerebrovascular Complications". The Journal of Pediatrics 166 (5): 1187–92.e1. doi:10.1016/j.jpeds.2015.02.014. PMID 25919727.
- ↑ Ramos, Regina; Viana, Rafaela; Brainer-Lima, Alessandra; Florêncio, Telma; Carvalho, Maria Durce; van Der Linden, Vanessa; Amorim, Antonio; Rocha, Maria Ângela et al. (2017). "Perinatal Chikungunya Virus-Associated Encephalitis Leading to Postnatal-Onset Microcephaly and Optic Atrophy". The Pediatric Infectious Disease Journal 37 (1): 94–95. doi:10.1097/INF.0000000000001690. ISSN 0891-3668. PMID 28737626.
- ↑ "Galloway-Mowat Syndrome". https://rarediseases.org/rare-diseases/galloway-mowat-syndrome/.
- ↑ Kurian, Manju A; Jungbluth, Heinz (July 2014). "Genetic disorders of thyroid metabolism and brain development". Developmental Medicine and Child Neurology 56 (7): 627–634. doi:10.1111/dmcn.12445. ISSN 0012-1622. PMID 24665922.
- ↑ Reference, Genetics Home. "Fanconi anemia". https://medlineplus.gov/genetics/condition/fanconi-anemia/.
- ↑ Damlich, Jennifer; Qato, Roa; Cruz, Meredith; Colon, Maria; Wilkins, Isabelle (2009-07-01). "Discussion: 'Microcephaly associated with congenital heart defect' by Barbu et al" (in en). American Journal of Obstetrics & Gynecology 201 (1): e7–e12. doi:10.1016/j.ajog.2009.05.042. ISSN 0002-9378. PMID 19576365. https://www.ajog.org/article/S0002-9378(09)00556-0/abstract.
- ↑ "Facts about Microcephaly". Centers for Disease Control and Prevention. 2016-12-07. https://www.cdc.gov/ncbddd/birthdefects/microcephaly.html.
- ↑ Crespi, B.; Stead, P.; Elliot, M. (January 2010). "Evolution in health and medicine Sackler colloquium: Comparative genomics of autism and schizophrenia". Proceedings of the National Academy of Sciences of the United States of America 107 (Suppl 1): 1736–41. doi:10.1073/pnas.0906080106. PMID 19955444. Bibcode: 2010PNAS..107.1736C.
- ↑ Stone, Jennifer L.; O'Donovan, Michael C.; Gurling, Hugh; Kirov, George K.; Blackwood, Douglas H. R.; Corvin, Aiden et al. (September 2008). "Rare chromosomal deletions and duplications increase risk of schizophrenia". Nature 455 (7210): 237–241. doi:10.1038/nature07239. PMID 18668038. Bibcode: 2008Natur.455..237S.
- ↑ "DUF1220 domains, cognitive disease, and human brain evolution". Cold Spring Harb. Symp. Quant. Biol. 74: 375–382. 2009. doi:10.1101/sqb.2009.74.025. PMID 19850849.
- ↑ Rimol, Lars M.; Agartz, Ingrid; Djurovic, Srdjan; Brown, Andrew A.; Roddey, J. Cooper; Kahler, Anna K. et al. (2010). "Sex-dependent association of common variants of microcephaly genes with brain structure". Proceedings of the National Academy of Sciences 107 (1): 384–8. doi:10.1073/pnas.0908454107. PMID 20080800. Bibcode: 2010PNAS..107..384R.
- ↑ "Mosquitos kill more people than any other creature, the CDC warns". NPR Morning Edition. 8 July 2024. https://www.npr.org/2024/07/08/nx-s1-5026612/mosquitos-kill-more-people-than-any-other-creature-the-cdc-warns.
- ↑ "Zika virus - Brazil: confirmed Archive Number: 20150519.3370768". International Society for Infectious Diseases. http://www.promedmail.org/direct.php?id=3370768.
- ↑ Rasmussen, Sonja A.; Jamieson, Denise J.; Honein, Margaret A.; Petersen, Lyle R. (13 April 2016). "Zika Virus and Birth Defects — Reviewing the Evidence for Causality". New England Journal of Medicine 374 (20): 1981–7. doi:10.1056/NEJMsr1604338. PMID 27074377.
- ↑ "CDC Concludes Zika Causes Microcephaly and Other Birth Defects". 13 April 2016. https://www.cdc.gov/media/releases/2016/s0413-zika-microcephaly.html.
- ↑ "CDC issues interim travel guidance related to Zika virus for 14 Countries and Territories in Central and South America and the Caribbean". Centers for Disease Control and Prevention. 2016-01-15. https://www.cdc.gov/media/releases/2016/s0315-zika-virus-travel.html.
- ↑ Beth Mole (2016-01-17). "CDC issues travel advisory for 14 countries with alarming viral outbreaks". Ars Technica. Condé Nast. http://arstechnica.co.uk/science/2016/01/cdc-issues-travel-advisory-for-14-countries-with-alarming-viral-outbreaks/.
- ↑ Mlakar, Jernej; Korva, Misa; Tul, Nataša; Popović, Mara; Poljšak-Prijatelj, Mateja; Mraz, Jerica; Kolenc, Marko; Resman Rus, Katarina et al. (2016-03-10). "Zika Virus Associated with Microcephaly". New England Journal of Medicine 374 (10): 951–8. doi:10.1056/NEJMoa1600651. ISSN 0028-4793. PMID 26862926.
- ↑ Cavallin, Mara; Rujano, Maria A.; Bednarek, Nathalie; Medina-Cano, Daniel; Bernabe Gelot, Antoinette; Drunat, Severine; Maillard, Camille; Garfa-Traore, Meriem et al. (2017-10-01). "WDR81 mutations cause extreme microcephaly and impair mitotic progression in human fibroblasts and Drosophila neural stem cells". Brain 140 (10): 2597–2609. doi:10.1093/brain/awx218. ISSN 1460-2156. PMID 28969387.
- ↑ Coley, Brian D. (2013). [[[:Template:GBUrl]] Caffey's Pediatric Diagnostic Imaging E-Book] (12th ed.). Elsevier Health Sciences. ISBN 978-1-4557-5360-4. OCLC 847214216. Template:GBUrl.
- ↑ Martin, Richard J.; Fanaroff, Avroy A.; Walsh, Michele C. (2014). [[[:Template:GBUrl]] Fanaroff and Martin's Neonatal-Perinatal Medicine E-Book: Diseases of the Fetus and Infant]. Elsevier Health Sciences. ISBN 978-0-323-29537-6. OCLC 909892605. Template:GBUrl.
- ↑ "Aftereffects". http://www.pcf.city.hiroshima.jp/kids/KPSH_E/hiroshima_e/sadako_e/subcontents_e/13kousyougai_1_e.html#.
- ↑ 56.0 56.1 56.2 Kalter, Harold (2010). [[[:Template:GBUrl]] "Pioneering Studies §Atomic Radiation §Microcephaly and Mental Retardation"]. Teratology in the Twentieth Century Plus Ten. Springer. p. 21. doi:10.1007/978-90-481-8820-8_2. ISBN 978-90-481-8820-8. Template:GBUrl.
- ↑ Burrow, Gerard N.; Hamilton, Howard B.; Hrubec, Zdenek (June 1964). "Study of Adolescents Exposed in Utero to the Atomic Bomb, Nagasaki, Japan". Yale Journal of Biology and Medicine 36 (6): 430–444. PMID 14173443.
- ↑ Adams, Hieab H. H.; Hibar, Derrek P.; Chouraki, Vincent; Stein, Jason L.; Nyquist, Paul A.; Rentería, Miguel E.; Trompet, Stella; Arias-Vasquez, Alejandro et al. (2016). "Novel genetic loci underlying human intracranial volume identified through genome-wide association". Nature Neuroscience 19 (12): 1569–82. doi:10.1038/nn.4398. PMID 27694991.
- ↑ Jamuar, SS; Walsh, CA (June 2015). "Genomic variants and variations in malformations of cortical development.". Pediatric Clinics of North America 62 (3): 571–85. doi:10.1016/j.pcl.2015.03.002. PMID 26022163.
- ↑ Rash, BG; Lim, HD; Breunig, JJ; Vaccarino, FM (26 October 2011). "FGF signaling expands embryonic cortical surface area by regulating Notch-dependent neurogenesis.". The Journal of Neuroscience 31 (43): 15604–17. doi:10.1523/jneurosci.4439-11.2011. PMID 22031906.
- ↑ Shen, J; Gilmore, EC; Marshall, CA; Haddadin, M; Reynolds, JJ; Eyaid, W; Bodell, A; Barry, B et al. (March 2010). "Mutations in PNKP cause microcephaly, seizures and defects in DNA repair.". Nature Genetics 42 (3): 245–9. doi:10.1038/ng.526. PMID 20118933.
- ↑ Alkuraya, FS; Cai, X; Emery, C; Mochida, GH; Al-Dosari, MS; Felie, JM; Hill, RS; Barry, BJ et al. (13 May 2011). "Human mutations in NDE1 cause extreme microcephaly with lissencephaly [corrected."]. American Journal of Human Genetics 88 (5): 536–47. doi:10.1016/j.ajhg.2011.04.003. PMID 21529751.
- ↑ Johnson, Matthew B.; Sun, Xingshen; Kodani, Andrew; Borges-Monroy, Rebeca; Girskis, Kelly M.; Ryu, Steven C.; Wang, Peter P.; Patel, Komal et al. (2018). "Aspm knockout ferret reveals an evolutionary mechanism governing cerebral cortical size". Nature 556 (7701): 370–5. doi:10.1038/s41586-018-0035-0. PMID 29643508. Bibcode: 2018Natur.556..370J.
- ↑ Nowakowski, TJ; Pollen, AA; Di Lullo, E; Sandoval-Espinosa, C; Bershteyn, M; Kriegstein, AR (5 May 2016). "Expression Analysis Highlights AXL as a Candidate Zika Virus Entry Receptor in Neural Stem Cells.". Cell Stem Cell 18 (5): 591–6. doi:10.1016/j.stem.2016.03.012. PMID 27038591.
- ↑ Li, C; Xu, D; Ye, Q; Hong, S; Jiang, Y; Liu, X; Zhang, N; Shi, L et al. (7 July 2016). "Zika Virus Disrupts Neural Progenitor Development and Leads to Microcephaly in Mice.". Cell Stem Cell 19 (1): 120–6. doi:10.1016/j.stem.2016.04.017. PMID 27179424.
- ↑ "The role of the DNA damage response pathways in brain development and microcephaly: insight from human disorders". DNA Repair (Amst) 7 (7): 1039–50. July 2008. doi:10.1016/j.dnarep.2008.03.018. PMID 18458003.
- ↑ "DNA damage and repair: underlying mechanisms leading to microcephaly". Front Cell Dev Biol 11. 2023. doi:10.3389/fcell.2023.1268565. PMID 37881689.
- ↑ de Koning, T. J. (2006). "Treatment with amino acids in serine deficiency disorders". Journal of Inherited Metabolic Disease 29 (2–3): 347–351. doi:10.1007/s10545-006-0269-0. ISSN 0141-8955. PMID 16763900.
- ↑ Stories, Wander (4 February 2015). [[[:Template:GBUrl]] Colosseum in Rome: a travel guide and tour as with the best local guide]. WanderStories. ISBN 978-9-949-51606-3. Template:GBUrl.
- ↑ Mateen, F.J.; Boes, C.J. (2010). "'Pinheads': the exhibition of neurologic disorders at 'The Greatest Show on Earth'". Neurology 75 (22): 2028–32. doi:10.1212/WNL.0b013e3181ff9636. PMID 21115959.
- ↑ "Zip the Pinhead: What is it?". The Human Marvels. 16 October 2010. http://www.thehumanmarvels.com/zip-the-pinhead-what-is-it/.
- ↑ "Interview with Bill Griffith". Goblin Magazine. 1995. http://www.zippythepinhead.com/pages/aaishehavingfunyet.html.
- ↑ Kozma, Chahira (10 October 2005). "Historical Review - Dwarfs in Ancient Egypt". American Journal of Medical Genetics 140 (4): 303–311. doi:10.1002/ajmg.a.31068. PMID 16380966. http://www.academia.dk/MedHist/Biografier/PDF/DwarfsInAncientEgypt.pdf. Retrieved 17 February 2018.
- ↑ Cook, Jr., James W., 'Of Men, Missing Links, and Nondescripts: The Strange Career of P. T. Barnum's "What is It?" Exhibition', in Rosemarie Garland-Thomson (ed.), Freakery: Cultural Spectacles of the Extraordinary Body, (New York: New York University Press, 1996), pp. 139-157.
External links
| Classification | |
|---|---|
| External resources |
|
Template:Congenital malformations and deformations of nervous system
 |









