Philosophy:Sexual motivation and hormones
Sexual motivation is influenced by hormones such as testosterone, estrogen, progesterone, oxytocin, and vasopressin. In most mammalian species, sex hormones control the ability and motivation to engage in sexual behaviours.
Measuring sexual motivation
Sexual motivation can be measured using a variety of different techniques. Self-report measures, such as the Sexual Desire Inventory, are commonly used to detect levels of sexual motivation in humans. Self-report techniques such as the bogus pipeline can be used to ensure individuals do not falsify their answers to represent socially desirable results. Sexual motivation can also be implicitly examined through frequency of sexual behaviour, including masturbation.
Hormones
Testosterone
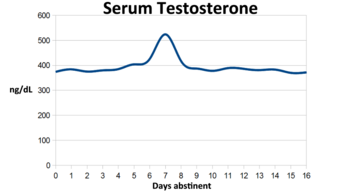
Testosterone appears to be a major contributing factor to sexual motivation in male primates, including humans. The elimination of testosterone in adulthood has been shown to reduce sexual motivation in both male humans and male primates.[1] Male humans who had their testicular function suppressed with a GnRH antagonist displayed decreases in sexual desire and masturbation two weeks following the procedure.[2] Research from male rhesus monkeys suggests testosterone functions to increase sexual motivation, thereby motivating males to compete for access to sexual partners. It is postulated that the motivating effects of testosterone in male rhesus monkeys promotes successful sexual competition and may be particularly important motivating tools for low ranking males.[2] It is important to note that elimination of testosterone in primates does not reduce the ability to copulate; rather, it reduces the motivation to copulate.
Testosterone levels in males have been shown to vary according to the ovulating state of females. Males who were exposed to scents of ovulating women recorded higher testosterone levels than males who were exposed to scents of nonovulating women.[3] Being exposed to female ovulating cues may increase testosterone, which in turn may increase males' motivation to engage in, and initiate, sexual behaviour. Ultimately, these higher levels of testosterone may increase the reproductive success of males exposed to female ovulation cues.
The relationship between testosterone and female sexual motivation is somewhat ambiguous. Research suggests androgens, such as testosterone, are not sufficient by themselves to prompt sexual motivation in females. In particular, studies with rhesus macaques have observed testosterone was not significantly associated with variations in level of sexual motivation in females.[2] However, some research with nonhuman primates suggests a role for androgens in female sexual behaviour. Adrenalectomized female rhesus monkeys displayed diminished female sexual receptivity.[4] Later studies revealed this diminished sexual receptivity was specific to the elimination of androgens that can be converted to estrogen.[5]
It is also suggested that levels of testosterone are related to the type of relationship in which one is involved. Men involved in polyamorous relationships display higher levels of testosterone than men involved in either a single partner relationship or single men.[6] Polyamorous women have both higher levels of testosterone and score higher on measures of sexual desire than women who are single or women who are in single-partner relationships.[6]
Estrogens and progesterone
Estrogens and progesterone typically regulate motivation to engage in sexual behaviour for females in mammalian species, though the relationship between hormones and female sexual motivation is not as well understood. In particular, estrogens have been shown to correlate positively with increases in female sexual motivation, and progesterone has been associated with decreases in female sexual motivation.[7][8] The periovulatory period of the female menstrual cycle is often associated with increased female receptivity and sexual motivation.[8] During this stage in the cycle, estrogens are elevated in the female and progesterone levels are low. At this time, mating is more likely to result in female pregnancy.
Females at different stages of their menstrual cycle have been shown to display differences in sexual attraction. Heterosexual females not using birth control pills who are ovulating (high levels of estrogens) have a preference for the scent of males with low levels of fluctuating asymmetry.[9] Ovulating heterosexual females also display preferences toward masculine faces and report greater sexual attraction to males other than their current partner.[10] From an evolutionary perspective, increases in estrogens during fertile periods in females may direct sexual motivation toward males with preferential genes (the good genes hypothesis).
Following natural or surgically induced menopause, many women experience declines in sexual motivation.[11] Menopause is associated with a rapid decline of estrogen, as well as a steady rate of decline of androgens.[12] The decline of estrogen and androgen levels is believed to account for the lowered levels of sexual desire and motivation in postmenopausal women, although the direct relationship is not well understood.
Oxytocin and vasopressin
The hormones oxytocin and vasopressin are implicated in regulating both male and female sexual motivation. Oxytocin is released at orgasm and is associated with both sexual pleasure and the formation of emotional bonds.[13] Based on the pleasure model of sexual motivation, the increased sexual pleasure that occurs following oxytocin release may encourage motivation to engage in future sexual activities. Emotional closeness can be an especially strong predictor of sexual motivation in females and insufficient oxytocin release may subsequently diminish sexual arousal and motivation in females.
High levels of vasopressin can lead to decreases in sexual motivation for females.[13] A link between vasopressin release and aggression has been observed in females, which may impair female sexual arousal and sexual motivation by leading to feelings of neglect and hostility toward a sexual partner.[14] In males, vasopressin is involved in the arousal phase. Vasopressin levels have been shown to increase during erectile response in male sexual arousal, and decrease back to baseline following ejaculation.[15] The increase of vasopressin during erectile response may be directly associated with increased motivation to engage in sexual behaviour.[13]
Nonprimate species
The hormonal influences of sexual motivation are much more clearly understood for nonprimate females. Suppression of estrogen receptors in the ventromedial nucleus of the hypothalamus in female rats has been observed to reduce female proceptivity and receptivity.[16] Proceptivity and receptivity in the female rat are indicators of sexual motivation, thus indicating a direct relationship between estrogen levels and sexual motivation. In addition, female rats receiving doses of estrogen and progesterone were more likely to exert effort at gaining sexual attention from a male rat.[17] The willingness of the female rats to access males was considered a direct measure of the females' levels of sexual motivation.
An increase in vasopressin has been observed in female rats which have just given birth. Vasopressin is associated with aggressive and hostile behaviours, and is postulated to decrease sexual motivation in females. Vasopressin administered in the female rat brain has been observed to result in an immediate decrease in sexual motivation.[13]
Sexual orientation
Little research has been conducted on the effect of hormones on sexual motivation for same-sex sexual contact. One study observed the relationship between sexual motivation in lesbian and bisexual women and period-related changes in circulating estrogen concentrations.[18] Lesbian women who were at the estrogen peak of their fertile cycle reported increased sexual motivation for sexual contact with women, whereas bisexual women reported only a slight increase in same-sex motivated sexual contact during peak estrogen levels.[citation needed]
Both lesbian and bisexual women showed decreases in sexual motivation for other-sex sexual contact at peak estrogen levels, with greater changes in the bisexual group than the lesbian group.[citation needed]
Clinical research
Men
- Testosterone is critical for sexual desire, function, and arousal in men.[19][20] Aromatization of testosterone into the estrogen estradiol appears to be partially responsible for the effects of testosterone on sexual desire and function in men.[21][22][23] 5α-Reduction of testosterone into the more potent androgen dihydrotestosterone (DHT) may have a small contribution to the effects of testosterone on sexual desire and function in men.[24] Based on animal research, metabolites of DHT including the neurosteroids and weak estrogens 3α-androstanediol and 3β-androstanediol may be involved in sexual function in men.[25][26][27]
- Men experience sexual dysfunction at testosterone levels of below 300 ng/dL, with men that have levels of testosterone of approximately 200 ng/dL often experiencing such problems.[28] Complete loss of testicular testosterone production resulting in testosterone levels within the castrate range (95% decrease, to 15 ng/dL on average) with surgical or medical castration causes profound sexual dysfunction in men.[29][30] Combined marked suppression of testicular testosterone production resulting in testosterone levels of just above the castrate/female range (70 to 80% decrease, to 100 ng/dL on average) and marked androgen receptor antagonism with high-dosage cyproterone acetate monotherapy causes profound sexual dysfunction in men.[29][31] Treatment of men with medical castration and add-back of multiple dosages of testosterone to restore testosterone levels (to a range of about 200 to 900 ng/dL) showed that testosterone dose-dependently restored sexual desire and erectile function in men.[32] High-dosage monotherapy with an androgen receptor antagonist such as bicalutamide or enzalutamide, which preserves testosterone and estradiol levels, has a minimal to moderate negative effect on sexual desire and erectile function in men in spite of strong blockade of the androgen receptor.[29][33][34][35]
- Estradiol supplementation maintains greater sexual desire in men with surgical or medical castration.[23] High-dose estrogen therapy, which results in marked or complete suppression of testicular testosterone production such that testosterone levels are within the castrate range (95% decrease, to less than 50 ng/dL), causes decreased sexual desire and function.[23][36][37] However, sexual function and activity appear to be significantly better with high-dose estrogen therapy than with surgical castration.[21][22][23] Treatment of men with medical castration and add-back testosterone to restore testosterone levels, with or without the aromatase inhibitor anastrozole, showed that prevention of the conversion of testosterone into estradiol partially prevented restoration of sexual desire and erectile dysfunction by testosterone in men.[32] However, this was not the case in another study with a similar design that used the aromatase inhibitor testolactone.[22] Men with aromatase deficiency and estrogen insensitivity syndrome, and hence estrogen deficiency, appear to have normal sexual desire, function, and activity.[22][21] However, estradiol supplementation in some men with aromatase deficiency increased sexual desire and activity but not in other men with aromatase deficiency.[22][21][38] Treatment with the antiestrogenic selective estrogen receptor modulator (SERM) tamoxifen has been found to decrease sexual desire in men treated with it for male breast cancer.[39] However, other studies have not found or reported decreased sexual function in men treated with SERMs including tamoxifen, clomifene, raloxifene, and toremifene.[22][40]
- 5α-Reductase inhibitors, which block the conversion of testosterone into DHT, result in a slightly increased risk of sexual dysfunction with an incidence of decreased libido and erectile dysfunction of about 3 to 16%.[41][42][24] Treatment of healthy men with multiple dosages of testosterone enanthate, with or without the 5α-reductase inhibitor dutasteride, showed that dutasteride did not significantly influence changes in sexual desire and function.[43][24] Treatment of men with high-dosage bicalutamide therapy, with or without the 5α-reductase inhibitor dutasteride, showed that dutasteride did not significantly influence sexual function.[44] Combined high-dosage bicalutamide therapy plus dutasteride showed less sexual dysfunction than medical castration similarly to high-dosage bicalutamide monotherapy.[45]
- Treatment of men with very high-dosage DHT (a non-aromatizable androgen), which resulted in an increase in DHT levels by approximately 10-fold and complete suppression of testosterone and estradiol levels, showed that none of the measures of sexual function were significantly changed with the exception of a mild but significant decrease in sexual desire.[40][46][24] Treatment of hypogonadal men with the aromatizable testosterone undecanoate and the non-aromatizable mesterolone showed that testosterone undecanoate produced better improvements in mood, libido, erection, and ejaculation than did mesterolone.[21][40] However, the dosage of mesterolone could have been suboptimal.[40]
Women
- Estradiol seems to be the most important hormone for sexual desire in women.[47][28][48] Periovulatory levels of estradiol increase sexual desire in women.[47] Based on animal research, progesterone may also be involved in sexual function in women.[49][50][51] Very limited clinical research suggests that progesterone does not increase sexual desire and may decrease it.[52] There is little support for the notion that physiological levels of testosterone are important for sexual desire in women, although supraphysiological levels of testosterone can increase sexual desire in women similarly to the high levels in men.[47][28]
- There is little to no correlation between total testosterone levels within the normal physiological range and sexual desire in premenopausal women.[28] Sexual desire is not increased in women with polycystic ovary syndrome (PCOS) in spite of high testosterone levels.[28] Women with PCOS actually experience an improvement in sexual desire following treatment of their condition, likely due improved psychological functioning (e.g., body image).[28]
- Sexual desire is not decreased in women with complete androgen insensitivity syndrome (CAIS) relative to unaffected women in spite of a completely non-functional androgen receptor.[28] Sexual desire is increased or unchanged in most women taking a combined birth control pill.[28][53][54] This is in spite of the fact that almost all combined birth control pills contain the potently hepatotropic estrogen ethinylestradiol, and the typical doses of ethinylestradiol present in combined birth control pills increase sex hormone-binding globulin (SHBG) levels by 2- to 4-fold and consequently decrease free testosterone levels by 40 to 80%.[55] However, there are some conflicting reports on the effects of combined birth control pills on sexual function in women.[56] Progestogen-only birth control, such as with depot medroxyprogesterone acetate or the etonogestrel birth control implant, has shown mixed effects on sexual desire and function.[52][57] Androgen receptor antagonists such as flutamide and bicalutamide cause little to no decrease in sexual desire in women.[58][59][60]
- Low dosages of testosterone that result in physiological levels of testosterone (< 50 ng/dL) do not increase sexual desire in women.[47][28] High dosages of testosterone that result in supraphysiological levels of testosterone (> 50 ng/dL) significantly increase sexual desire in women, with levels of testosterone of 80 to 150 ng/dL "slightly" increasing sexual desire.[47][28] Further higher dosages of testosterone may result in greater effects on sexual desire in women.[47][28] High dosages of testosterone (with levels of > 50 ng/dL) have a risk of masculinization (e.g., acne, hair growth, voice changes) with long-term therapy in women.[47][28] High dosages of testosterone but not low dosages of testosterone enhance the effects of low dosages of estrogens on sexual desire.[47][28] Tibolone, a combined estrogen, progestin, and androgen, may increase sex drive to a greater extent than standard estrogen–progestogen therapy in postmenopausal women.[61][62][63][64]
Transgender individuals
- Testosterone therapy increases sexual desire and arousal in transgender men.[65][66] Estradiol and antiandrogen therapy decreases sexual desire and arousal in transgender women.[65] However, treatment with estradiol in transgender women who have undergone surgical castration appears to maintain significantly greater sexual desire and activity than would be expected for surgical castration alone.[21][22][23]
See also
- Body odour and sexual attraction
- Hypoactive sexual desire disorder
- Sexual desire and intimate relationships
- Menopause
- Menstrual cycle
- Pheromone
References
- ↑ Wallen K (2001). "Sex and context: hormones and primate sexual motivation.". Hormones and Behavior 40 (2): 339–357. doi:10.1006/hbeh.2001.1696. PMID 11534996.
- ↑ 2.0 2.1 2.2 Wallen K (2001). "Sex and context: hormones and primate sexual motivation". Hormones and Behavior 40 (2): 339–57. doi:10.1006/hbeh.2001.1696. PMID 11534996.
- ↑ Miller S. L.; Maner J. K. (2009). "Scent of a woman: Men's testosterone responses to olfactory ovulation cues". Psychological Science 21 (2): 276–283. doi:10.1177/0956797609357733. PMID 20424057.
- ↑ Johnson D. F.; Phoenix C. H. (1976). "Hormonal control of female sexual attractiveness, proceptivity, and receptivity in rhesus monkeys". Journal of Comparative and Physiological Psychology 90 (5): 473–483. doi:10.1037/h0077216. PMID 977822.
- ↑ Veney S. L.; Rissman E. F. (2000). "Steroid implants in the medial preoptic area or ventromedial nucleus of the hypothalamus activate female sexual behaviour in the musk shrew". Journal of Neuroendocrinology 12 (11): 1124–1132. doi:10.1046/j.1365-2826.2000.00567.x. PMID 11069128.
- ↑ 6.0 6.1 Van Anders S. M.; Hamilton L. D.; Watson N. V. (2007). "Multiple partners are associated with higher testosterone in North American men and women". Hormones and Behavior 51 (3): 454–459. doi:10.1016/j.yhbeh.2007.01.002. PMID 17316638. https://deepblue.lib.umich.edu/bitstream/2027.42/83914/1/multiple_partners_are_associated_with_higher_testosterine_in_North_American_men_and_women.pdf.
- ↑ "General sexual desire, but not desire for uncommitted sexual relationships, tracks changes in women's hormonal status". Psychoneuroendocrinology 88: 153–157. February 2018. doi:10.1016/j.psyneuen.2017.12.015. PMID 29287282. http://eprints.gla.ac.uk/154251/7/154251.pdf.
- ↑ 8.0 8.1 Ziegler T. E. (2007). "Female sexual motivation during non-fertile periods: a primate phenomenon". Hormones and Behavior 51 (1): 1–2. doi:10.1016/j.yhbeh.2006.09.002. PMID 17069815.
- ↑ Gangestad S. W.; Thornhill R. (1998). "Menstrual cycle variation in women's preferences for the scent of symmetrical men". Proceedings of the Royal Society of London 265 (1399): 927–933. doi:10.1098/rspb.1998.0380. PMID 9633114.
- ↑ Gangestad S. W.; Thornhill R.; Garver-Apgar C. E. (2005). "Adaptations to ovulation implications for sexual and social behaviour". Current Directions in Psychological Science 14 (6): 312–316. doi:10.1111/j.0963-7214.2005.00388.x.
- ↑ Giles (2008). "Sex hormones and sexual desire". Journal for the Theory of Social Behaviour 38 (1): 45–66. doi:10.1111/j.1468-5914.2008.00356.x.
- ↑ "Nonsteroidal selective androgen receptor modulators enhance female sexual motivation". The Journal of Pharmacology and Experimental Therapeutics 334 (2): 439–448. 2010. doi:10.1124/jpet.110.168880. PMID 20444881.
- ↑ 13.0 13.1 13.2 13.3 Hiller, J. (2005). Gender differences in sexual motivation. The journal of men's health & gender, 2(3), 339-345.
- ↑ Keverne E. B.; Curley J. P. (2004). "Vasopressin, oxytocin and social behaviour". Neurobiology 14 (6): 777–783. doi:10.1016/j.conb.2004.10.006. PMID 15582383.
- ↑ Carter C. S. (1992). "Oxytocin and sexual behaviour". Neuroscience & Biobehavioral Reviews 16 (2): 131–144. doi:10.1016/s0149-7634(05)80176-9. PMID 1630727.
- ↑ "Estrogen-induced sexual incentive motivation, proceptivity and receptivity depend on a functional estrogen receptor [alpha in the ventromedial nucleus of the hypothalamus but not in the amygdala"]. Neuroendocrinology 91 (2): 142–154. 2010. doi:10.1159/000255766. PMID 19887773.
- ↑ Cummings J. A.; Becker J. B. (2012). "Quantitative assessment of female sexual motivation in the rat: Hormonal control of motivation". Journal of Neuroscience Methods 204 (2): 227–233. doi:10.1016/j.jneumeth.2011.11.017. PMID 22120688.
- ↑ Diamond L. M.; Wallen K. (2011). "Sexual minority women's sexual motivation around the time of ovulation". Archives of Sexual Behavior 40 (2): 237–246. doi:10.1007/s10508-010-9631-2. PMID 20464467.
- ↑ "Translational Perspective on the Role of Testosterone in Sexual Function and Dysfunction". J Sex Med 13 (8): 1183–98. August 2016. doi:10.1016/j.jsxm.2016.06.004. PMID 27436075.
- ↑ "Testosterone and sexual function in men". Maturitas 112: 46–52. June 2018. doi:10.1016/j.maturitas.2018.04.004. PMID 29704917.
- ↑ 21.0 21.1 21.2 21.3 21.4 21.5 "Role of estrogen in normal male function: clinical implications for patients with prostate cancer on androgen deprivation therapy". J. Urol. 185 (1): 17–23. January 2011. doi:10.1016/j.juro.2010.08.094. PMID 21074215.
- ↑ 22.0 22.1 22.2 22.3 22.4 22.5 22.6 "Estrogens in men: clinical implications for sexual function and the treatment of testosterone deficiency". J Sex Med 9 (6): 1681–96. June 2012. doi:10.1111/j.1743-6109.2012.02726.x. PMID 22512993.
- ↑ 23.0 23.1 23.2 23.3 23.4 "The effect of estrogen on the sexual interest of castrated males: Implications to prostate cancer patients on androgen-deprivation therapy". Crit. Rev. Oncol. Hematol. 87 (3): 224–38. September 2013. doi:10.1016/j.critrevonc.2013.01.006. PMID 23484454.
- ↑ 24.0 24.1 24.2 24.3 "Dihydrotestosterone: Biochemistry, Physiology, and Clinical Implications of Elevated Blood Levels". Endocr. Rev. 38 (3): 220–254. June 2017. doi:10.1210/er.2016-1067. PMID 28472278.
- ↑ "Mechanisms regulating male sexual behavior in the rat: role of 3 alpha- and 3 beta-androstanediols". Biol. Reprod. 51 (3): 562–71. September 1994. doi:10.1095/biolreprod51.3.562. PMID 7803627.
- ↑ "Non-genomic actions of androgens". Front Neuroendocrinol 29 (2): 169–81. May 2008. doi:10.1016/j.yfrne.2007.10.005. PMID 18093638.
- ↑ "Dissociating behavioral, autonomic, and neuroendocrine effects of androgen steroids in animal models". Psychiatric Disorders. Methods in Molecular Biology. 829. 2012. pp. 397–431. doi:10.1007/978-1-61779-458-2_26. ISBN 978-1-61779-457-5.
- ↑ 28.00 28.01 28.02 28.03 28.04 28.05 28.06 28.07 28.08 28.09 28.10 28.11 28.12 "Has testosterone passed the test in premenopausal women with low libido? A systematic review". Int J Women's Health 8: 599–607. 2016. doi:10.2147/IJWH.S116212. PMID 27785108.
- ↑ 29.0 29.1 29.2 "Nonsteroidal antiandrogens: a therapeutic option for patients with advanced prostate cancer who wish to retain sexual interest and function". BJU Int. 87 (1): 47–56. January 2001. doi:10.1046/j.1464-410x.2001.00988.x. PMID 11121992.
- ↑ "Treatment of Paraphilic Disorders in Sexual Offenders or Men With a Risk of Sexual Offending With Luteinizing Hormone-Releasing Hormone Agonists: An Updated Systematic Review". J Sex Med 15 (1): 77–93. January 2018. doi:10.1016/j.jsxm.2017.11.013. PMID 29289377.
- ↑ "Cyproterone acetate in the treatment of sexual disorders: pharmacological base and clinical experience". Exp. Clin. Endocrinol. 98 (2): 71–80. 1991. doi:10.1055/s-0029-1211103. PMID 1838080.
- ↑ 32.0 32.1 "Gonadal steroids and body composition, strength, and sexual function in men". N. Engl. J. Med. 369 (11): 1011–22. September 2013. doi:10.1056/NEJMoa1206168. PMID 24024838.
- ↑ "The role of antiandrogen monotherapy in the treatment of prostate cancer". BJU Int. 91 (5): 455–61. March 2003. doi:10.1046/j.1464-410X.2003.04026.x. PMID 12603397.
- ↑ "Bicalutamide 150mg: a review of its use in the treatment of locally advanced prostate cancer". Drugs 66 (6): 837–50. 2006. doi:10.2165/00003495-200666060-00007. PMID 16706554.
- ↑ "Enzalutamide monotherapy in hormone-naive prostate cancer: primary analysis of an open-label, single-arm, phase 2 study". Lancet Oncol. 15 (6): 592–600. May 2014. doi:10.1016/S1470-2045(14)70129-9. PMID 24739897.
- ↑ "The World Federation of Societies of Biological Psychiatry (WFSBP) guidelines for the biological treatment of paraphilias". World J. Biol. Psychiatry 11 (4): 604–55. 2010. doi:10.3109/15622971003671628. PMID 20459370.
- ↑ "Flutamide. A preliminary review of its pharmacodynamic and pharmacokinetic properties, and therapeutic efficacy in advanced prostatic cancer". Drugs 38 (2): 185–203. August 1989. doi:10.2165/00003495-198938020-00003. PMID 2670515. "A favourable feature of flutamide therapy has been its lesser effect on libido and sexual potency; fewer than 20% of patients treated with flutamide alone reported such changes. In contrast, nearly all patients treated with oestrogens or estramustine phosphate reported loss of sexual potency. [...] In comparative therapeutic trials, loss of potency has occurred in all patients treated with stilboestrol or estramustine phosphate compared with 0 to 20% of those given flutamide alone (Johansson et al. 1987; Lund & Rasmussen 1988).".
- ↑ "Of mice and men: the many guises of estrogens". Tissue-Specific Estrogen Action. Ernst Schering Foundation Symposium Proceedings. 2006/1. 2006. 45–67. doi:10.1007/2789_2006_016. ISBN 978-3-540-49547-5.
- ↑ "Preliminary study with bicalutamide in heterosexual and homosexual patients with prostate cancer: a possible implication of androgens in male homosexual arousal". BJU Int. 108 (1): 110–5. July 2011. doi:10.1111/j.1464-410X.2010.09764.x. PMID 20955264.
- ↑ 40.0 40.1 40.2 40.3 "Long-term effects of dihydrotestosterone treatment on prostate growth in healthy, middle-aged men without prostate disease: a randomized, placebo-controlled trial". Ann. Intern. Med. 153 (10): 621–32. November 2010. doi:10.7326/0003-4819-153-10-201011160-00004. PMID 21079217.
- ↑ "Adverse Effects and Safety of 5-alpha Reductase Inhibitors (Finasteride, Dutasteride): A Systematic Review". J Clin Aesthet Dermatol 9 (7): 56–62. 2016. PMID 27672412.
- ↑ "Effects of 5-alpha reductase inhibitors on erectile function, sexual desire and ejaculation". Expert Opin Drug Saf 12 (1): 81–90. January 2013. doi:10.1517/14740338.2013.742885. PMID 23173718.
- ↑ "Effect of testosterone supplementation with and without a dual 5α-reductase inhibitor on fat-free mass in men with suppressed testosterone production: a randomized controlled trial". JAMA 307 (9): 931–9. March 2012. doi:10.1001/jama.2012.227. PMID 22396515.
- ↑ "The AVOCAT study: Bicalutamide monotherapy versus combined bicalutamide plus dutasteride therapy for patients with locally advanced or metastatic carcinoma of the prostate-a long-term follow-up comparison and quality of life analysis". SpringerPlus 5: 653. 2016. doi:10.1186/s40064-016-2280-8. PMID 27330919.
- ↑ "Randomized non-inferiority trial of Bicalutamide and Dutasteride versus LHRH agonists for prostate volume reduction prior to I-125 permanent implant brachytherapy for prostate cancer". Radiother Oncol 118 (1): 141–7. January 2016. doi:10.1016/j.radonc.2015.11.022. PMID 26702991. "Dutasteride and Bicalutamide is a regimen of non-inferior efficacy to LHRH agonist based regimens for prostate volume reduction prior to permanent implant prostate brachytherapy. D + B has less sexual toxicity compared to LHRH agonists prior to implant and for the first 6 months after implant. D + B is therefore an option to be considered for prostate volume reduction prior to PIPB.".
- ↑ "Male sexual function can be maintained without aromatization: randomized placebo-controlled trial of dihydrotestosterone (DHT) in healthy, older men for 24 months". J Sex Med 11 (10): 2562–70. October 2014. doi:10.1111/jsm.12550. PMID 24751323.
- ↑ 47.0 47.1 47.2 47.3 47.4 47.5 47.6 47.7 "Increasing women's sexual desire: The comparative effectiveness of estrogens and androgens". Horm Behav 78: 178–93. February 2016. doi:10.1016/j.yhbeh.2015.11.003. PMID 26589379.
- ↑ "Sexual medicine: Transdermal oestrogen is effective". Nat Rev Urol 14 (11): 638. November 2017. doi:10.1038/nrurol.2017.152. PMID 28895561.
- ↑ "Novel perspectives for progesterone in hormone replacement therapy, with special reference to the nervous system". Endocr. Rev. 28 (4): 387–439. June 2007. doi:10.1210/er.2006-0050. PMID 17431228.
- ↑ "Progesterone receptors: form and function in brain". Front Neuroendocrinol 29 (2): 313–39. May 2008. doi:10.1016/j.yfrne.2008.02.001. PMID 18374402.
- ↑ "Role of Estrogens and Estrogen-Like Compounds in Female Sexual Function and Dysfunction". J Sex Med 13 (3): 305–16. March 2016. doi:10.1016/j.jsxm.2015.11.015. PMID 26944462.
- ↑ 52.0 52.1 "Hormones and Female Sexual Dysfunction: Beyond Estrogens and Androgens--Findings from the Fourth International Consultation on Sexual Medicine". J Sex Med 13 (3): 283–90. March 2016. doi:10.1016/j.jsxm.2015.12.014. PMID 26944460.
- ↑ "The influence of combined oral contraceptives on female sexual desire: a systematic review". Eur J Contracept Reprod Health Care 18 (1): 27–43. February 2013. doi:10.3109/13625187.2012.728643. PMID 23320933.
- ↑ "The effects of hormonal contraceptives on female sexuality: a review". J Sex Med 9 (9): 2213–23. September 2012. doi:10.1111/j.1743-6109.2012.02848.x. PMID 22788250.
- ↑ IARC Working Group on the Evaluation of Carcinogenic Risks to Humans; World Health Organization; International Agency for Research on Cancer (2007). Combined Estrogen-progestogen Contraceptives and Combined Estrogen-progestogen Menopausal Therapy. World Health Organization. pp. 157, 433–. ISBN 978-92-832-1291-1. https://books.google.com/books?id=aGDU5xibtNgC&pg=PA433.
- ↑ "Impact of Contraception on Female Sexual Function". J Womens Health (Larchmt) 26 (3): 207–213. March 2017. doi:10.1089/jwh.2015.5703. PMID 27622561.
- ↑ "Contraception and sexuality". Minerva Ginecol 62 (4): 331–47. August 2010. PMID 20827250.
- ↑ "Combined Oral Contraception and Bicalutamide in Polycystic Ovary Syndrome and Severe Hirsutism: A Double-Blind Randomized Controlled Trial". J. Clin. Endocrinol. Metab. 103 (3): 824–838. March 2018. doi:10.1210/jc.2017-01186. PMID 29211888.
- ↑ "Retrospective, observational study on the effects and tolerability of flutamide in a large population of patients with acne and seborrhea over a 15-year period". Gynecol. Endocrinol. 27 (10): 823–9. October 2011. doi:10.3109/09513590.2010.526664. PMID 21117864. "Among the slight and temporary adverse events [of flutamide], most frequently reported and not requesting treatment discontinuation were headache (7.8%), respiratory tract disorders (7.0%), nausea and/or vomiting (4.0%), diarrhea (4.0%), dry skin (9.5%), and reduction of libido (4.5%).".
- ↑ "Low-dose flutamide (125 mg/day) as maintenance therapy in the treatment of hirsutism". Horm. Res. 56 (1–2): 25–31. 2001. doi:10.1159/000048086. PMID 11815724. "[...] changes in serum levels of the aminotransferases [11] or side effects (stomach pain, headache, dry skin, nausea, increased appetite, decrease of libido) are only occasionally seen [with flutamide] [10, 11].".
- ↑ "Tibolone and climacteric symptoms". Maturitas 21 (2): 127–36. February 1995. doi:10.1016/0378-5122(94)00888-E. PMID 7752950.
- ↑ "Tibolone: a review". Maturitas 30 (3): 295–305. November 1998. doi:10.1016/S0378-5122(98)00059-0. PMID 9881330.
- ↑ "The effects of tibolone on mood and libido". Menopause 9 (3): 162–70. 2002. doi:10.1097/00042192-200205000-00004. PMID 11973439.
- ↑ "Role of androgens, progestins and tibolone in the treatment of menopausal symptoms: a review of the clinical evidence". Clin Interv Aging 3 (1): 1–8. 2008. doi:10.2147/CIA.S1043. PMID 18488873.
- ↑ 65.0 65.1 "Endocrine Treatment of Gender-Dysphoric/Gender-Incongruent Persons: An Endocrine Society Clinical Practice Guideline". J. Clin. Endocrinol. Metab. 102 (11): 3869–3903. November 2017. doi:10.1210/jc.2017-01658. PMID 28945902.
- ↑ "Testosterone therapy for transgender men". Lancet Diabetes Endocrinol 5 (4): 301–311. April 2017. doi:10.1016/S2213-8587(16)00036-X. PMID 27084565.

