Medicine:Paediatric multisystem inflammatory syndrome
| Paediatric multi-system inflammatory syndrome (PMIS)[1] | |
|---|---|
| Other names | |
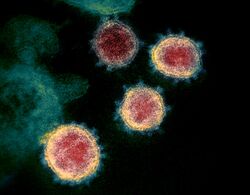 | |
TEM image of SARS-CoV-2, the coronavirus responsible for COVID-19: PMIS / MIS-C is thought to be caused by an unusual biological response to infection in certain children | |
| Specialty | Paediatrics |
| Symptoms | Fever, abdominal pain, diarrhoea/vomiting, low blood pressure, pink eye, rashes, large lymph nodes, swollen hands/feet, irritability/confusion, etc. |
| Complications | Cardiac, coronary artery abnormalities, septic shock, organ dysfunction |
| Usual onset | ≥2 weeks after COVID-19 exposure |
| Causes | Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) |
| Diagnostic method | Clinical evaluation by specialists |
| Differential diagnosis | Alternative infectious/non-infectious causes, Kawasaki disease |
| Medication | Intravenous immunoglobulin (IVIG), corticosteroids; oxygen, supportive care |
| Prognosis | Response to treatment is generally good[3][5][6][7] |
| Frequency | Rare |
| Deaths | Life-threatening |
Paediatric multisystem inflammatory syndrome (PMIS), or multisystem inflammatory syndrome in children (MIS-C), is a systemic disease involving persistent fever, inflammation and organ dysfunction following exposure to SARS-CoV-2, the virus responsible for COVID-19.[1][2][3]
This syndrome appears somewhat similar to Kawasaki disease, a rare disease of unknown origin that affects young children, in which blood vessels become inflamed throughout the body.[4] It can also show features of other serious paediatric inflammatory conditions, including toxic shock and macrophage activation syndromes.[1][8] Older children tend to be affected.[9] The first symptoms may be acute abdominal pain, diarrhoea or vomiting.[1] Low blood pressure is common.[1] Other possible symptoms include conjunctivitis, rashes, enlarged lymph nodes, swollen hands and feet, "strawberry tongue",[10] sore throat, cough, fainting, irritability and confusion.[1][3][4] Inflammation of the heart muscle is one of several forms of cardiac involvement.[8] Coronary artery abnormalities (such as dilatation and aneurysms) can occur.[1][3][4] A cytokine storm may take place,[11] in which the innate immune system stages an excessive and uncontrolled inflammatory response.[12]
For the purposes of diagnosis and official reporting of cases, this emerging condition has been defined in three different ways (using various names), by the World Health Organization (WHO),[3] the Royal College of Paediatrics and Child Health (RCPCH),[1] and the Centers for Disease Control and Prevention (CDC).[2] Although the condition is thought to follow SARS-CoV-2 viral infection, antigen or antibody tests are not always positive.[4] Exclusion of alternative causes, including bacterial and other infections, is essential for differential diagnosis.[4] Some general clinical guidance has been provided by the RCPCH,[1] the National Institutes of Health,[9] the American College of Rheumatology,[13] and the American Academy of Pediatrics.[14]
Limited information exists regarding clinical course of this life-threatening disease,[9] which has occasionally proved fatal.[4] Failure of one or more organs can occur.[1] Early recognition and prompt specialist attention are essential.[10] Supportive care is key.[9] Anti-inflammatory treatments have been used, with good responses being recorded for intravenous immunoglobulin (IVIG), with or without corticosteroids.[5][6] Oxygen therapy may be needed, and some children require paediatric intensive care.[1]
Clusters of new cases have emerged 2–4 weeks after local peaks in viral transmission.[6][15] It is thought that the disease may be driven by a delayed biological mechanism in certain predisposed children.[6][11] The condition is considered rare.[4] The European Centre for Disease Prevention and Control (ECDC) has rated risk to children in Europe as being 'low' overall, based on a 'very low' likelihood of a child developing this 'high impact' disease.[4] Initial reports regarded children in various parts of Europe and the U.S., and it is unclear to what extent the condition has gone unrecognized elsewhere.[3]
Background
Symptomatic cases of COVID-19 in children have been relatively uncommon,[16] possibly because they generally experience milder disease.[17] Early infection tends to be associated with mild or no symptoms, while the later pulmonary phase, which can be life-threatening in adults, is usually mild or absent.[7][18] While cases of children with severe symptoms are exceptional, they can occasionally require intensive care.[19][20] Fatalities have been rare.[18][21]
A few children with evidence of SARS-CoV-2 infection or exposure to COVID-19 display clinical features corresponding to the diagnostic criteria of Kawasaki disease, sometimes accompanied by shock.[22] Kawasaki disease is a rare syndrome which mainly affects young children (adult onset has occasionally been reported[23]).[4][24][25] It is a form of vasculitis, where blood vessels become inflamed throughout the body, and it results in a persistent fever.[4] Recovery typically occurs spontaneously, though some children later develop mid-sized or giant coronary artery aneurysms in the heart – a potentially fatal complication.[4][26] Symptoms of toxic shock (a syndrome caused by bacterial toxins) occasionally occur – an association sometimes referred to as 'Kawasaki shock syndrome',[27] which is characterized by systolic hypotension or signs of poor perfusion.[4][28] While the exact cause of Kawasaki disease is unknown, one plausible explanation is that it may stem from an infection triggering an autoimmune and/or autoinflammatory response in children who are genetically predisposed.[29][30] No specific diagnostic test exists for Kawasaki disease, and its recognition is based on various combinations of clinical and laboratory findings (including persistent fever, widespread rashes, enlarged lymph nodes, conjunctivitis, changes to the mucous membranes, and swollen hands and feet).[4][24][31]
Characteristics
PMIS / MIS-C is a systemic inflammation, involving persistent fever, inflammation and organ dysfunction, which is temporally associated with exposure to COVID-19.[1][2] Onset may be delayed or contemporary with ongoing SARS-CoV-2 infection.[8] It may occur several weeks (commonly 2–4 weeks[32]) after the initial infection.[27] The condition may match some or all of the diagnostic criteria for Kawasaki disease (i.e. the 'complete' or 'incomplete'/'atypical' subtypes[31]),[1] or for Kawasaki disease shock syndrome.[27] It tends to affect all paediatric age groups, ranging from infancy to adolescence (whereas Kawasaki disease most often occurs before the age of five).[6][11] It can also share clinical features with other paediatric inflammatory conditions, including toxic shock syndrome, septic shock,[33] and secondary haemophagocytic lymphohistiocytosis / macrophage activation syndrome.[1][7] Coinfections with other pathogens have been recorded.[4]
Children may present with symptoms not commonly associated with Kawasaki disease,[8] including unusual abdominal symptoms, accompanied by pronounced inflammatory markers (e.g. high ESR, CRP, ferritin,[6] procalcitonin[7]).[1] Acute gastrointestinal symptoms can include intense abdominal pain, and diarrhoea or vomiting.[3] Low blood pressure is common.[1] Other symptoms may include conjunctivitis, Kawasaki-like rashes (consistent with leukocytoclastic vasculitis),[34] mucosal changes (e.g. "strawberry tongue", cracked lips),[10] enlarged lymph nodes, neck pain,[35] swollen hands and feet, sore throat, cough, breathing difficulties, chest pain,[35] fatigue,[35] fainting, irritability and confusion, as well as other[36] neurological disturbances.[1][3][4] Features of meningitis have been reported.[6][37]
Inflammation of the heart muscle (myocarditis) is frequent.[8] Other cardiological features may include inflammation of the fibrous sac surrounding the heart (pericarditis) and of the valves (valvulitis), as well as coronary artery abnormalities, such as dilatation.[1][3][4] Some children have developed coronary artery aneurysms (assuming that Kawasaki disease was not the actual underying cause).[11][22][38] Shock is often of myocardial – mainly left ventricular – origin.[4][6] The respiratory symptoms typically reported in adult cases of COVID-19 are not usually a prominent feature.[4][6][37] When present, breathing difficulties are often linked to shock,[4] and are suggestive of heart failure.[37] Some children display features of a cytokine storm,[37] including high serum interleukin-6 (IL-6) levels, and need inotropic support to maintain cardiac output.[11]
Low platelet counts and impaired coagulation are common.[6] High neutrophil counts are frequent.[6] Acute kidney injury and low albumin levels in the blood are common.[7] Low blood sodium levels and raised liver enzymes have been reported.[6] Accumulations of fluid in the lungs, around the heart and in the abdomen have also been reported, consistent with generalized inflammation.[7]
Cardiac involvement and features of macrophage activation syndrome appear to be more frequent than in Kawasaki disease.[9][39] In addition to gastrointestinal presentation, neurological involvement also appears to be relatively frequent.[37] Characteristic laboratory findings that are not usually encountered in Kawasaki disease include low white blood cell counts and very elevated levels of ventricular natriuretic peptide, a marker of heart failure.[11] Raised troponin levels, suggestive of myocardial damage, are common.[6][7] Coronary artery aneurysms seem to be encountered less frequently than would be expected with Kawasaki disease.[11]
Limited information currently exists regarding clinical course,[2][3] which tends to be more severe than with Kawasaki disease.[8] Supplemental oxygen may be required, and paediatric intensive care may also be needed.[1] Fatalities (five, as of 11 May 2020[4]) have resulted from complications of extracorporeal membrane oxygenation.[11] Some children exposed to COVID-19 also appear to have a less severe Kawasaki-like disease.[22]
Diagnosis
- 0–19 years of age with fever >3 days
AND
- Two of the following:
- Rash or bilateral non-purulent conjunctivitis
or muco-cutaneous inflammation signs
(oral, hands or feet) - Hypotension or shock
- Features of myocardial dysfunction, pericarditis,
valvulitis, or coronary abnormalities
(including ECHO findings or elevated Troponin/NT-proBNP) - Evidence of coagulopathy
(by PT, PTT, elevated d-Dimers) - Acute gastrointestinal problems
(diarrhoea, vomiting, or abdominal pain)
AND
- Elevated markers of inflammation
such as ESR, C-reactive protein, or procalcitonin
AND
- No other obvious microbial cause of inflammation,
including bacterial sepsis,
staphylococcal or streptococcal shock syndromes
AND
- Evidence of COVID-19
(RT-PCR, antigen test or serology positive),
or likely contact with patients with COVID-19
(Note: Consider this syndrome in children with features of
typical or atypical Kawasaki disease
or toxic shock syndrome.)
Diagnosis is by specialist clinical evaluation.[40] Clinicians worldwide have been urged to consider this condition in children who display some or all the features of Kawasaki disease or toxic shock syndrome.[3] Early recognition and multidisciplinary referral to paediatric specialists (in intensive care, infectious diseases, cardiology, haematology, rheumatology, etc) is considered essential.[1][9][37][10] Diagnostic suspicion may be raised by unexplained persistent fever and/or clinically concerning symptoms following exposure to COVID-19.[37]
Case definitions and guidance
The varying[18] initial case definitions released by the World Health Organization (WHO), the Royal College of Paediatrics and Child Health (RCPCH) and Centers for Disease Control and Prevention (CDC) all include involvement of more than one organ system, along with fever and elevated inflammatory markers.[27] In particular:
- The preliminary WHO case definition is for 'multisystem inflammatory disorder in children and adolescents' (box).[3] The WHO has established a platform for standardized, anonymized clinical data, along with a dedicated case report form, and underlines the "urgent need for collection of standardized data describing clinical presentations, severity, outcomes, and epidemiology."[3]
- Diagnostic guidance by the RCPCH proposes a case definition which has also been endorsed by an expert panel convened by the American College of Cardiology.[41] Key clinical criteria set out in the RCPHC case definition are: persistent fever, inflammation (indicated by neutrophilia, high CRP levels and low lymphocyte count), and evidence of organ dysfunction (shock; cardiac, respiratory, renal, gastrointestinal, or neurological disorder), coupled with additional clinical features, including laboratory, imaging and ECG findings.[1][4] Coronary artery abnormalities, such as dilatation, may be apparent at echocardiography and ECG (or contrast CT of the chest).[1] Biomarkers supporting the diagnosis include abnormal fibrinogen levels, high D-dimers (possible coagulopathy), high troponin, low albumin, and high ferritin.[1] According to the RCPCH definition, the child may test positive or negative for SARS-CoV-2, but other possible microbial causes need to be excluded.[1][4]
- The CDC case definition for MIS-C comprises individuals "aged <21 years presenting with fever, laboratory evidence of inflammation, and evidence of clinically severe illness requiring hospitalization, with multisystem (>2) organ involvement (cardiac, renal, respiratory, hematologic, gastrointestinal, dermatologic or neurological)."[2] It also requires that there should either be a positive antigen/antibody SARS-CoV-2 test or COVID-19 exposure in the 4 weeks before onset of symptoms, along with exclusion of other plausible diagnoses.[2] This case definition is quite broad (it overlaps not only with Kawasaki disease, but also with juvenile rheumatoid arthritis, and various infectious/inflammatory conditions of childhood, including other viral diseases).[11] The CDC advises health providers in the United States to inform their public health authorities of suspected cases, even if they also meet full or partial criteria for Kawasaki disease, and to consider MIS-C after any childhood fatality in which there is evidence of SARS-CoV-2 infection.[2]
Provisional diagnostic guidance has also been provided by both the American College of Rheumatology[10] and the American Academy of Pediatrics.[37] A clinical pathway for diagnostic evaluation of suspected MIS-C has been proposed by the Children's Hospital of Philadelphia.[40]
Differential diagnosis
It is essential to exclude alternative non-infectious[37] and infectious causes of the inflammatory condition, including bacterial sepsis, staphylococcal and streptococcal shock, and infections associated with myocarditis, such as enterovirus.[1][4] (At the same time, coinfection with additional pathogens, including human metapneumovirus and various other microbes, may sometimes occur.)[4]
Differential diagnosis with Kawasaki disease can be challenging, given the lack of a diagnostic test for either condition.[11] It is not currently known whether the newly described condition is superimposable with Kawasaki disease shock syndrome.[27] Since prompt diagnosis and timely treatment of actual Kawasaki disease is important to prevent complications, a call has been made to "Keep a high suspicion for Kawasaki disease in all children with prolonged fever, but especially in those younger than 1 year of age."[42]
Treatment
The Royal College of Paediatrics and Child Health has outlined a provisional approach to clinical management, including guidance on early medical management, monitoring and some general principles of treatment.[1] The National Institutes of Health publishes some considerations.[9] Guidance for clinical management of MIS-C has been released by the American College of Rheumatology.[10][13] The American Academy of Pediatrics has also provided some interim guidance.[37]
Little specific information is available regarding therapeutic effectiveness.[2][3][9] Supportive care is a mainstay of therapy,[9] and for mild or moderate disease it may be sufficient.[1][6] Anti-inflammatory treatments have been used, and good responses have been recorded for IVIG, with or without corticosteroids.[3][5][6][7] Cases requiring steroids due to resistance to IVIG may be more common than in Kawasaki disease.[8] Immunomodulators (e.g. IL-1 and IL-6 inhibitors) are also sometimes considered.[9] Low-dose aspirin has sometimes been used as an antiplatelet drug.[6][37] RCPCH guidance recommends that all affected children should be treated as having suspected COVID-19.[1]
It is unclear whether antiviral treatments specifically targeting SARS-CoV-2 could have any potential role.[9] The RCPHC recommends that any administration of a candidate antiviral therapy should − whenever possible − be performed in the context of a registered clinical trial (e.g. RECOVERY).[1] In the U.K., ongoing collaborations are aiming to ensure that all infected children are able to take part in a mechanistic study such as DIAMONDS or ISARIC-CCP.[1][22] (In the European Union, children do not usually participate in clinical trials of new antiviral and monoclonal antibody treatments for severe COVID-19.)[4]
Treatment strategies are being considered to prevent serious long-term complications such as coronary artery aneurysms (the main complication of Kawasaki disease).[22] Close outpatient follow-up by a paediatric cardiology team is advised.[37]
Causes
While it has been hypothesized that the condition is related to COVID-19,[3] it has also been emphasized that the potential link "is neither established nor well understood."[4] A temporal association between SARS-CoV-2 infection and clinical presentation of the syndrome is plausible.[4] A causality assessment found that 'temporality' was among the five (out of nine) Bradford Hill criteria that supported a causal relationship between SARS-CoV-2 infection and the development of the syndrome.[4] Further characterization of the syndrome is essential to identify risk factors and help understand causality.[3] It is unclear to what extent this emerging syndrome has a similar aetiology to Kawasaki disease (a condition predating the emergence of SARS-CoV-2, which is currently thought to be triggered by a distinct viral agent).[11] Improved understanding will have potential implications for clinical management.[43] Genome-wide association studies are expected to provide insights on susceptibility and potential biological mechanisms.[8].
Mechanism
The pathogenesis is unknown.[2][4] SARS-CoV-2 could have one of several roles; it could act as an environmental trigger for the condition either directly or indirectly (by somehow paving the way for a different trigger).[29]
As with Kawasaki disease, one proposed infectious mechanism has been antibody-dependent enhancement, whereby development of antibodies could facilitate viral entry into host cells.[4] Epidemiological considerations make a post-infectious mechanism seem likely.[11][6] It has been suggested that the condition may be caused by the cytokine storms induced by COVID-19.[12] The characteristic ability of coronaviruses to block type I and type III interferon responses could help explain a delayed cytokine storm in children whose immune systems struggle to control SARS-CoV-2 viral replication, or are overwhelmed by a high initial viral load.[11] A plausible chain of events leading up to a hyperimmune response could involve early viral triggering of macrophage activation, followed by T helper cell stimulation, in turn leading to cytokine release, stimulation of macrophages, neutrophils, and monocytes, in conjunction with B cell and plasma cell activation, and antibody production.[7]
On pathophysiological grounds, the frequent gastrointestinal (rather than respiratory) presentation, along with findings of mesenteric lymph node inflammation, suggests predominant replication in the gastrointestinal tract by a virus with a known predilection for enterocytes.[11] Association of Kawasaki-like disease with COVID-19 could support the view that SARS-CoV-2 can cause systemic vasculitis by targeting endothelial tissue via angiotensin-converting enzyme 2 (ACE2), the protein which the virus uses to gain access to cells.[44]
Key research questions regarding the underlying molecular mechanisms that lead to PMIS following exposure to SARS-CoV-2 include identification of: any genetic predisposition factors; any associations with particular viral variant/s; any molecular patterns capable of triggering the autoimmune/autoinflammatory responses.[8] Another key question is whether the molecular mechanisms that trigger autoimmune/autoinflammatory responses in children with PMIS and adults with severe COVID-19 (including the induction of high concentrations of IL-6) are similar or distinct.[8]
It has been noted that a leading hypothesis for the pathogenesis of Kawasaki disease also involves a hyperinflammatory response to viral infection (such as by a novel RNA virus[31][45]) in some genetically predisposed children,[46] and that SARS-CoV-2 is now "added to the list" of implicated viral triggers.[8]
Epidemiology
Epidemiological information is limited.[3] Suspected cases began to be recorded in Europe and the U.S. around April 2020, and several hundred possible cases were recorded by mid-May, along with at least five fatalities.[4][47] A nationwide surveillance programme in France, set up to investigate the temporal relationship between SARS-CoV-2 infection and PMIS, revealed that 95 of the 156 cases of Kawasaki-like disease notified between 1 March and 17 May 2020 "were confirmed or probable post-COVID-19 cases."[48]
Clinicians in Bergamo, Italy, reported an apparent 30-fold increase in the incidence of Kawasaki-like disease during the first six weeks after the arrival there of SARS-CoV-2 virus infection, at a time when Bergamo was experiencing the highest rates of infections and deaths in Italy.[22][49] In the UK, the number of intensive care admissions for children fulfilling the RCPCH case definition of PMIS during 40 days through April and early May, following the national surge in COVID-19 cases, was at least 11-fold higher than historical trends for paediatric inflammatory conditions.[50] Analysis of cases of Kawasaki disease admitted to a paediatric centre in Paris, France, revealed a spike that started 2 weeks after the peak of the COVID-19 epidemic there, corresponding to a roughly 5-fold increase in incidence.[15] These cases from Paris had a similarly severe clinical profile to those reported in Bergamo (and differed from the more typical Kawasaki disease profile observed in a newly uncovered spike following the peak of the 2009 H1N1 swine flu epidemic in Paris).[15] Such observations can be seen to support the concept that SARS-CoV-2 infection may be capable of triggering a more severe form of Kawasaki-like disease.[45] Clusters of cases of the newly described condition have been recorded 3–4 weeks after peaks in SARS-CoV-2 viral transmission through various local communities.[6] Frequent presentation without prominent respiratory symptoms in children who do not appear to have ongoing SARS-CoV-2 infection but who have already developed antibodies suggests that the disease may be driven by a delayed, post-infectious mechanism.[6]
This emerging diagnosis is considered rare.[4] A rapid risk assessment conducted by the European Centre for Disease Prevention and Control (ECDC) concluded that the overall risk to children in the European Union (EU), European Economic Area (EEA) and the UK "is considered 'low', based on a 'very low' probability of [the disease] in children and a 'high' impact of such disease."[4]
Regarding geographical distribution, it is unclear whether the initial reports of cases in Europe and North America reflect a true pattern, or whether the condition has gone unrecognized elsewhere.[3] In Southeast and East Asia, where Kawasaki disease is usually much more prevalent than in Europe, no case of Kawasaki-like disease linked to COVID-19 was reported during the first wave of transmission,[4][51] and no apparent increase in cases of Kawasaki disease was observed in countries such as South Korea[52] and Japan.[8] No case was observed in Australia or New Zealand either.[53][54] News of confirmed or suspected cases has since emerged from several other countries, including Russia,[55] India,[56][57][58] Pakistan,[59] Iran,[60] Israel,[61][62] Algeria,[63] Peru,[64] and Ecuador.[65]
Reports from France and the U.K. raise the possibility that children of Afro-Caribbean descent may be at greater risk, plausibly due to a genetic predisposition.[8] It has been suggested that this condition may affect more children of African American, Caribbean, and Hispanic ancestry, whereas Kawasaki disease affects more of East Asian ancestry, although the role of socioeconomic and other environmental factors in such distinctions is unclear.[29] In the US (as of mid-July), the majority of cases were classified as Hispanic/Latino (38%) or non-Hispanic Black (33%) people.[32]
This is a newly-proposed clinical entity, and an opinion was expressed that cases meeting the criteria for Kawasaki disease or myocarditis should be diagnosed and treated as such.[46] A concern has been raised that some clinically less severe cases of the provisionally defined new entity may be going unrecognized.[38] Concerns have also been raised regarding the potential for missed or delayed diagnosis of Kawasaki disease due to heightened diagnostic suspicion for the new entity.[42]
Hopes have been expressed that study of the new condition may help understand the hidden mechanisms behind Kawasaki disease.[22]
History
Cases of Kawasaki disease with concurrent SARS-CoV-2 infection have been recorded among children in Europe and in the United States since 7 April 2020, when a report was published by the American Academy of Pediatrics regarding a case of 'classic' Kawasaki disease in a six-month old girl who tested positive for COVID-19 in California.[4][66] In this case, COVID-19 did not appear to have significant clinical implications.[43][66]
On 25 April, concerns were initially raised in the United Kingdom regarding a cluster of children of various ages presenting with a multisystem inflammatory state who required intensive care, and who all displayed "overlapping features of toxic shock syndrome and atypical Kawasaki disease with blood parameters consistent with severe COVID-19 in children."[22][67] Details of the eight cases which helped trigger this alert (not all with confirmed exposure to COVID-19) were later reported in The Lancet,[43] where the authors summarized the clinical picture as "a hyperinflammatory syndrome with multiorgan involvement similar to Kawasaki disease shock syndrome."[47]
Accounts of analogous cases – including some that appeared less clinically severe – were also being informally shared among clinicians around Europe.[22] The EU’s Early Warning and Response System flagged supected cases in Austria, Germany and Portugal that had tested positive for SARS-CoV-2.[4]
In Bergamo, at the heart of the COVID-19 epidemic in Lombardy, a cluster of 20 cases of Kawasaki disease appeared to be roughly equivalent to the number commonly recorded there over the course of three years.[43] In France, the government reported on 29 April that around 15 children were in hospital in Paris with symptoms of Kawasaki disease,[43][68] an observation which prompted the organization of national surveillance programme for recent cases of Kawasaki-like disease.[48]
On 1 May, the RCPCH published a preliminary case definition based on review of the characteristics of the cases identified in the UK, accompanied by some clinical guidance.[1][22] Two weeks later, on 15 May, two further preliminary case definitions were published separately by the WHO[3] and by the CDC,[2] while the ECDC released a 'rapid risk assessment' of the condition on behalf of the European Union.[4]
On 4 May, the New York City Department of Health and Mental Hygiene issued an alert to identify children with the condition in New York City hospitals,[4] where 15 such cases were already being treated.[69] On 9 May, the governor of New York, Andrew Cuomo announced a collaboration with the CDC to help develop national criteria for identifying and responding to the newly identified childhood disease.[70]
By 12 May, some 230 suspected cases had been reported across the EU and EEA, and in the UK[4] (in the following days, sources were reporting up to 100 in the UK,[71] over 135 in France,[72] 20 in the Netherlands,[73] 10 in Switzerland[74] and 10 in Germany[75]). In the United States, more than 200 cases were suspected by mid-May,[76] including some 145 in New York;[77][78] 186 confirmed cases were eventually diagnosed between 15 March and 20 May in 26 US states.[79][80] As of 11 May 2020, five fatalities were reported (1 in France, 1 in the UK, 3 in the US).[4] In peer-reviewed medical journals, case series and related studies of the new condition were rapidly reported from countries including the UK;[47][81] Italy;[49] Spain;[82] France and Switzerland;[5] France;[83][84][85] and across the US.[86][87][88][79][89] The emerging observations suggested somewhat greater variety in the severity of symptoms than was originally thought.[9]
By 15 July, 342 confirmed cases (including 6 deaths) had been recorded in the US across 36 states plus Washington DC.[32][90] Most (71%) of the children were Hispanic/Latino or non-Hispanic Black people, and the CDC underlined the need to learn the reasons for such a preponderance.[32][91]
Until late May, no confirmed case had been documented outside the EU/EEA/UK and USA.[4] On 2 June, news emerged of a first case of MIS-C diagnosed in Peru.[64][92] In Russia, 13 children had been treated (5 with intensive care) by mid-June for a multisystem inflammatory syndrome at the Morozov Children's Hospital in Moscow, including a 2-year-old girl with the COVID-19 infection who died on 23 May following an initial diagnosis of suspected Kawasaki disease.[55] In Iran, a case report (first submitted in May) described severe MIS-C in a 5-year-old girl who had presented with shock and was initially diagnosed with Kawasaki disease.[60] In India, a case of suspected MIS-C was reported in late May regarding a child who had presented in a COVID-19 hotspot in Kerala.[56] An editorial commentary urged clinicians to have a high level of diagnostic suspicion and follow WHO and CDC definitions to facilitate timely identification and treatment of cases.[93] During July, suspected cases were being flagged in Mumbai,[57] and then in Delhi,[58] Chennai, and elsewhere.[94] In Pakistan, at least 24 children were said to be affected in Lahore.[59] Cases have been recorded in Israel,[61] including one of a child who presented with severe central nervous system involvement and complement deficiency.[62] In Algeria, a first case was recorded in June.[63] In Egypt, on 10 July the authorities denied rumours of the existence of cases of Kawasaki-like disease in the country.[95] In Ecuador, the Ministry of Health announced on 19 July the presence of 46 probable cases.[65]
An adult case of Kawasaki-like multisystem inflammatory syndrome following SARS-CoV-2 infection has been described in a 54-year-old woman from Israel with no history of autoimmune disease, who experienced uveitis in both eyes.[96] (A further suspected adult case was covered in the Israeli national press.)[97] A case involving a 36-year-old Hispanic American woman with clinical features otherwise consistent with MIS-C was reported from New York.[98] A case report published in The Lancet regarding a 45-year-old Hispanic man who presented in New York with features strongly resembling MIS-C called for awareness of "a potential MIS-C-like condition in adults."[99]
References
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 1.13 1.14 1.15 1.16 1.17 1.18 1.19 1.20 1.21 1.22 1.23 1.24 1.25 1.26 1.27 1.28 1.29 1.30 Guidance - Paediatric multisystem inflammatory syndrome temporally associated with COVID-19, The Royal College of Paediatrics and Child Health, May 2020, https://www.rcpch.ac.uk/sites/default/files/2020-05/COVID-19-Paediatric-multisystem-%20inflammatory%20syndrome-20200501.pdf
- ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 "Multisystem inflammatory syndrome in children (MIS-C) associated with coronavirus disease 2019 (COVID-19)". Centers for Disease Control and Prevention. 14 May 2020. https://emergency.cdc.gov/han/2020/han00432.asp.
- ↑ 3.00 3.01 3.02 3.03 3.04 3.05 3.06 3.07 3.08 3.09 3.10 3.11 3.12 3.13 3.14 3.15 3.16 3.17 3.18 3.19 3.20 3.21 "Multisystem inflammatory syndrome in children and adolescents with COVID-19: scientific brief" (in en). World Health Organization. Archived from the original on 15 May 2020. https://web.archive.org/web/20200515220732/https://www.who.int/news-room/commentaries/detail/multisystem-inflammatory-syndrome-in-children-and-adolescents-with-covid-19.
- ↑ 4.00 4.01 4.02 4.03 4.04 4.05 4.06 4.07 4.08 4.09 4.10 4.11 4.12 4.13 4.14 4.15 4.16 4.17 4.18 4.19 4.20 4.21 4.22 4.23 4.24 4.25 4.26 4.27 4.28 4.29 4.30 4.31 4.32 4.33 4.34 4.35 4.36 4.37 4.38 4.39 4.40 4.41 "Rapid risk assessment: Paediatric inflammatory multisystem syndrome and SARS-CoV-2 infection in children" (in en) (PDF). European Centre for Disease Prevention and Control. 15 May 2020. Archived from the original on 15 May 2020. https://web.archive.org/web/20200515100600/https://www.ecdc.europa.eu/en/publications-data/paediatric-inflammatory-multisystem-syndrome-and-sars-cov-2-rapid-risk-assessment.
- ↑ 5.0 5.1 5.2 5.3 "Acute heart failure in multisystem inflammatory syndrome in children (MIS-C) in the context of global SARS-CoV-2 pandemic". Circulation. 2020. doi:10.1161/CIRCULATIONAHA.120.048360. PMID 32418446.
- ↑ 6.00 6.01 6.02 6.03 6.04 6.05 6.06 6.07 6.08 6.09 6.10 6.11 6.12 6.13 6.14 6.15 6.16 6.17 6.18 "Human and novel coronavirus infections in children: a review". Paediatrics and International Child Health: 1–20. June 2020. doi:10.1080/20469047.2020.1781356. PMID 32584199.
- ↑ 7.0 7.1 7.2 7.3 7.4 7.5 7.6 7.7 7.8 "Multi-system inflammatory syndrome in children (MIS-C) following SARS-CoV-2 infection: review of clinical presentation, hypothetical pathogenesis, and proposed management". Children (Basel) 7 (7). July 2020. doi:10.3390/children7070069. PMID 32630212.
- ↑ 8.00 8.01 8.02 8.03 8.04 8.05 8.06 8.07 8.08 8.09 8.10 8.11 8.12 "Autoimmune and inflammatory diseases following COVID-19". Nature Reviews. Rheumatology. 2020. doi:10.1038/s41584-020-0448-7. PMID 32499548.
- ↑ 9.00 9.01 9.02 9.03 9.04 9.05 9.06 9.07 9.08 9.09 9.10 9.11 "Special Considerations in Children" (in en). National Institutes of Health. 11 June 2020. Archived from the original on 19 July 2020. https://web.archive.org/web/20200719133952/https://www.covid19treatmentguidelines.nih.gov/special-populations/children/.
- ↑ 10.0 10.1 10.2 10.3 10.4 10.5 ACR MIS-C and COVID-19 Related Hyperinflammation Task Force (17 June 2020). "Clinical guidance for pediatric patients with multisystem inflammatory syndrome in children (MIS-C) associated with SARS-CoV-2 and hyperinflammation in COVID-19". American College of Rheumatology. Archived from the original on 25 June 2020. https://web.archive.org/web/20200625141131/https://www.rheumatology.org/Portals/0/Files/ACR-COVID-19-Clinical-Guidance-Summary-MIS-C-Hyperinflammation.pdf.
- ↑ 11.00 11.01 11.02 11.03 11.04 11.05 11.06 11.07 11.08 11.09 11.10 11.11 11.12 11.13 "Understanding SARS-CoV-2-related multisystem inflammatory syndrome in children". Nature Reviews. Immunology. June 2020. doi:10.1038/s41577-020-0367-5. PMID 32546853.
- ↑ 12.0 12.1 "Storm, typhoon, cyclone or hurricane in patients with COVID-19? Beware of the same storm that has a different origin". RMD Open 6 (1): e001295. 2020. doi:10.1136/rmdopen-2020-001295. PMID 32423970.
- ↑ 13.0 13.1 Pond, E (20 July 2020). "ACR Guidelines for the Management of Pediatric Multisystem Inflammatory Syndrome Associated With SARS-CoV-2". Archived from the original on 21 July 2020. https://web.archive.org/web/20200721092942/https://www.rheumatologyadvisor.com/home/topics/pediatric-rheumatology/acr-guidelines-management-of-pediatric-multisystem-inflammatory-syndrome-sarscov2/.
- ↑ Hester, M (21 July 2020). "AAP issues interim guidance for MIS-C". Archived from the original on 21 July 2020. https://web.archive.org/web/20200721163846/https://www.contemporarypediatrics.com/view/aap-issues-interim-guidance-for-mis-c.
- ↑ 15.0 15.1 15.2 "Emergence of Kawasaki disease related to SARS-CoV-2 infection in an epicentre of the French COVID-19 epidemic: a time-series analysis". The Lancet. Child & Adolescent Health. July 2020. doi:10.1016/S2352-4642(20)30175-9. PMID 32622376.
- ↑ "SARS-CoV-2 infection in children". The New England Journal of Medicine 382 (17): 1663–1665. April 2020. doi:10.1056/NEJMc2005073. PMID 32187458.
- ↑ "Coronavirus infections in children including COVID-19: an overview of the epidemiology, clinical features, diagnosis, treatment and prevention options in children". The Pediatric Infectious Disease Journal 39 (5): 355–368. May 2020. doi:10.1097/INF.0000000000002660. PMID 32310621.
- ↑ 18.0 18.1 18.2 "COVID-19 in 7780 pediatric patients: a systematic review" (in en). EClinicalMedicine: 100433. June 2020. doi:10.1016/j.eclinm.2020.100433. ISSN 2589-5370. https://www.thelancet.com/journals/eclinm/article/PIIS2589-5370(20)30177-2/fulltext.
- ↑ "Coronavirus disease 2019 in children: current status". Journal of the Chinese Medical Association 83 (6): 527–533. June 2020. doi:10.1097/JCMA.0000000000000323. PMID 32502117.
- ↑ "Epidemiology and clinical features of coronavirus disease 2019 in children". Clinical and Experimental Pediatrics 63 (4): 125–132. April 2020. doi:10.3345/cep.2020.00535. PMID 32252139.
- ↑ "Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection in children and adolescents: a systematic review". JAMA Pediatrics. April 2020. doi:10.1001/jamapediatrics.2020.1467. PMID 32320004.
- ↑ 22.00 22.01 22.02 22.03 22.04 22.05 22.06 22.07 22.08 22.09 "Kawasaki-like disease: emerging complication during the COVID-19 pandemic". The Lancet 395 (10239): 1741–1743. 2020. doi:10.1016/S0140-6736(20)31129-6. PMID 32410759. https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(20)31129-6/fulltext.
- ↑ "Acute Kawasaki disease: not just for kids". Journal of General Internal Medicine 22 (5): 681–4. May 2007. doi:10.1007/s11606-006-0100-5. PMID 17443379.
- ↑ 24.0 24.1 "Dissecting Kawasaki disease: a state-of-the-art review". European Journal of Pediatrics 176 (8): 995–1009. 2017. doi:10.1007/s00431-017-2937-5. PMID 28656474.
- ↑ "Kawasaki Disease" (in en). NHLBI Health Topics. 11 June 2014. https://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0062985/.
- ↑ "Lifetime cardiovascular management of patients with previous Kawasaki disease". Heart 106 (6): 411–420. 2020. doi:10.1136/heartjnl-2019-315925. PMID 31843876.
- ↑ 27.0 27.1 27.2 27.3 27.4 "COVID-19: The impact on pediatric emergency care". Pediatric Emergency Medicine Practice 17 (Suppl 6-1): 1–27. June 2020. PMID 32496723. https://www.ebmedicine.net/topics/infectious-disease/COVID-19-Peds.
- ↑ "Describing Kawasaki shock syndrome: results from a retrospective study and literature review". Clinical Rheumatology 36 (1): 223–228. 2017. doi:10.1007/s10067-016-3316-8. PMID 27230223.
- ↑ 29.0 29.1 29.2 "SARS-CoV-2-related inflammatory multisystem syndrome in children: different or shared etiology and pathophysiology as Kawasaki disease?". JAMA. 2020. doi:10.1001/jama.2020.10370. PMID 32511667.
- ↑ "How should we classify Kawasaki disease?". Frontiers in Immunology 9. 2018. doi:10.3389/fimmu.2018.02974. PMID 30619331.
- ↑ 31.0 31.1 31.2 "Diagnosis, treatment, and long-term management of Kawasaki disease: a scientific statement for health professionals from the American Heart Association". Circulation 135 (17): e927–e999. 2017. doi:10.1161/CIR.0000000000000484. PMID 28356445.
- ↑ 32.0 32.1 32.2 32.3 "Multisystem Inflammatory Syndrome in Children (MIS-C)" (in en-us). Centers for Disease Control and Prevention. 15 July 2020. Archived from the original on 17 July 2020. https://web.archive.org/web/20200717095454/https://www.cdc.gov/mis-c/cases/. "As of 7/15/2020, CDC has received reports of 342 cases and 6 deaths in 37 jurisdictions... the majority of MIS-C patients have been Hispanic/Latino or Non-Hispanic Black....Additional studies into MIS-C are needed to learn why certain racial or ethnic groups may be affected in greater numbers..."
- ↑ "Septic shock presentation in adolescents with COVID-19". The Lancet Child & Adolescent Health 4 (7): e21–e23. 2020. doi:10.1016/S2352-4642(20)30164-4. PMID 32442421. PMC 7237371. https://www.thelancet.com/journals/lanchi/article/PIIS2352-4642(20)30164-4/fulltext.
- ↑ "Clinical and histopathological features and potential pathological mechanisms of skin lesions in COVID-19: review of the literature". Dermatopathology (Basel, Switzerland) 7 (1): 3–16. June 2020. doi:10.3390/dermatopathology7010002. PMID 32608380.
- ↑ 35.0 35.1 35.2 "COVID-19 PICU guidelines: for high- and limited-resource settings". Pediatric Research. July 2020. doi:10.1038/s41390-020-1053-9. PMID 32634818.
- ↑ "Neurologic and radiographic findings associated with COVID-19 infection in children". JAMA Neurology. July 2020. doi:10.1001/jamaneurol.2020.2687. PMID 32609336.
- ↑ 37.00 37.01 37.02 37.03 37.04 37.05 37.06 37.07 37.08 37.09 37.10 37.11 "Multisystem inflammatory syndrome in children (MIS-C) interim guidance" (in en). American Academy of Pediatrics. July 2020. Archived from the original on 17 July 2020. https://web.archive.org/web/20200717130345/https://services.aap.org/en/pages/2019-novel-coronavirus-covid-19-infections/clinical-guidance/multisystem-inflammatory-syndrome-in-children-mis-c-interim-guidance/.
- ↑ 38.0 38.1 "Childhood multisystem inflammatory syndrome - a new challenge in the pandemic". The New England Journal of Medicine. June 2020. doi:10.1056/NEJMe2023158. PMID 32598829.
- ↑ "Autoinflammatory and autoimmune conditions at the crossroad of COVID-19". Journal of Autoimmunity: 102506. June 2020. doi:10.1016/j.jaut.2020.102506. PMID 32563547.
- ↑ 40.0 40.1 "Multisystem inflammatory syndrome (MIS-C) clinical pathway – emergency, ICU and inpatient" (in en). The Children's Hospital of Philadelphia. 20 May 2020. Archived from the original on 26 June 2020. https://web.archive.org/web/20200626183744/https://www.chop.edu/clinical-pathway/multisystem-inflammatory-syndrome-mis-c-clinical-pathway.
- ↑ Newburger, JW (15 May 2020). "Pediatric Hyperinflammatory Syndrome and COVID-19: Statement and Recommendations From a Pediatric Intensive Care International Collaborative Conference Call". American College of Cardiology. Archived from the original on 19 May 2020. https://web.archive.org/web/20200519202816/https://www.acc.org/latest-in-cardiology/articles/2020/05/01/01/42/pediatric-hyperinflammatory-syndrome-and-covid-19-statement-and-recommendations-from-a-pediatric-intensive-care-coronavirus-disease-2019-international-collaborative-conference-call.
- ↑ 42.0 42.1 "Missed or delayed diagnosis of Kawasaki disease during the 2019 novel coronavirus disease (COVID-19) pandemic". The Journal of Pediatrics 222: 261–262. May 2020. doi:10.1016/j.jpeds.2020.04.052. PMID 32370951.
- ↑ 43.0 43.1 43.2 43.3 43.4 "COVID-19 and Kawasaki disease: finding the signal in the noise". Hospital Pediatrics. 2020. doi:10.1542/hpeds.2020-000356. PMID 32404331. https://hosppeds.aappublications.org/content/hosppeds/early/2020/05/11/hpeds.2020-000356.full-text.pdf.
- ↑ "Hypertension, thrombosis, kidney failure, and diabetes: is COVID-19 an endothelial disease? A comprehensive evaluation of clinical and basic evidence". Journal of Clinical Medicine 9 (5): 1417. 2020. doi:10.3390/jcm9051417. PMID 32403217.
- ↑ 45.0 45.1 "Kawasaki disease in the COVID-19 era: a distinct clinical phenotype?". The Lancet. Child & Adolescent Health. July 2020. doi:10.1016/S2352-4642(20)30207-8. PMID 32622377.
- ↑ 46.0 46.1 "COVID-19 and Kawasaki syndrome: should we really be surprised?". Cardiology in the Young: 1–5. 2020. doi:10.1017/S1047951120001432. PMID 32412400. https://www.cambridge.org/core/services/aop-cambridge-core/content/view/2AD153D73A34F46B580097685BD403D2/S1047951120001432a.pdf/covid19_and_kawasaki_syndrome_should_we_really_be_surprised.pdf.
- ↑ 47.0 47.1 47.2 "Hyperinflammatory shock in children during COVID-19 pandemic". The Lancet 395 (10237): 1607–1608. 7 May 2020. doi:10.1016/S0140-6736(20)31094-1. PMID 32386565. "During a period of 10 days in mid-April, 2020, we noted an unprecedented cluster of eight children with hyperinflammatory shock, showing features similar to atypical Kawasaki disease, Kawasaki disease shock syndrome, or toxic shock syndrome (typical number is one or two children per week). This case cluster formed the basis of a national alert.".
- ↑ 48.0 48.1 "SARS-CoV-2-related paediatric inflammatory multisystem syndrome, an epidemiological study, France, 1 March to 17 May 2020". Eurosurveillance. European Communicable Disease Bulletin 25 (22). 2020. doi:10.2807/1560-7917.ES.2020.25.22.2001010. PMID 32524957.
- ↑ 49.0 49.1 "An outbreak of severe Kawasaki-like disease at the Italian epicentre of the SARS-CoV-2 epidemic: an observational cohort study". The Lancet 395 (10239): 1771–1778. 2020. doi:10.1016/S0140-6736(20)31103-X. PMID 32410760.
- ↑ "Intensive care admissions of children with paediatric inflammatory multisystem syndrome temporally associated with SARS-CoV-2 (PIMS-TS) in the UK: a multicentre observational study". The Lancet. Child & Adolescent Health. July 2020. doi:10.1016/S2352-4642(20)30215-7. PMID 32653054.
- ↑ "COVID-19 and Kawasaki syndrome". Cardiology in the Young: 1. June 2020. doi:10.1017/S1047951120001894. PMID 32618551.
- ↑ "Defining association between COVID-19 and the multisystem inflammatory syndrome in children through the pandemic". Journal of Korean Medical Science 35 (22): e204. June 2020. doi:10.3346/jkms.2020.35.e204. PMID 32508068.
- ↑ "Australian Health Protection Principal Committee (AHPPC) coronavirus (COVID-19) statements on 14 May 2020" (in en). 15 May 2020. Archived from the original on 24 May 2020. https://web.archive.org/web/20200524143623/https://www.health.gov.au/news/australian-health-protection-principal-committee-ahppc-coronavirus-covid-19-statements-on-14-may-2020.
- ↑ "Chances of Kiwi kids contracting mysterious syndrome linked to Covid-19 'very low', but authorities on the lookout" (in en-NZ). TVNZ. 18 May 2020. Archived from the original on 2 June 2020. https://web.archive.org/web/20200602075823/https://www.tvnz.co.nz/one-news/new-zealand/chances-kiwi-kids-contracting-mysterious-syndrome-linked-covid-19-very-low-but-authorities-lookout.
- ↑ 55.0 55.1 Семенова, Мария (17 June 2020). "В Москве умер первый ребенок из-за новой болезни, вызванной COVID-19" (in ru). RIA Novosti. https://ria.ru/20200617/1573020546.html. Retrieved 18 June 2020.
- ↑ 56.0 56.1 "Multisystem inflammatory syndrome with features of atypical Kawasaki disease during COVID-19 pandemic". Indian Journal of Pediatrics. May 2020. doi:10.1007/s12098-020-03357-1. PMID 32462354.
- ↑ 57.0 57.1 "Mumbai Kawasaki Corona: Some Mumbai kids get Kawasaki-like disorder" (in en). The Times of India. 8 July 2020. Archived from the original on 8 July 2020. https://web.archive.org/web/20200708211055/https://timesofindia.indiatimes.com/city/mumbai/covid-reaction-some-mumbai-kids-get-kawasaki-like-disorder/articleshow/76846558.cms.
- ↑ 58.0 58.1 "Delhi hospitals see Kawasaki-like symptoms in children with Covid" (in en). The Indian Express. 18 July 2020. Archived from the original on 18 July 2020. https://web.archive.org/web/20200718074915/https://indianexpress.com/article/cities/delhi/delhi-hospitals-see-kawasaki-like-symptoms-in-children-with-covid-6511309/.
- ↑ 59.0 59.1 "Post-coronavirus Kawasaki-like inflammatory syndrome reported in eight children in Lahore". Samaa TV. 8 July 2020. Archived from the original on 9 July 2020. https://web.archive.org/web/20200709010643/https://www.samaa.tv/news/2020/07/post-coronavirus-kawasaki-like-inflammatory-syndrome-reported-in-eight-children-in-lahore/.
- ↑ 60.0 60.1 "Hyperinflammatory shock related to COVID-19 in a patient presenting with multisystem inflammatory syndrome in children: first case from Iran". Journal of Paediatrics and Child Health. July 2020. doi:10.1111/jpc.15048. PMID 32640066.
- ↑ 61.0 61.1 "New inflammatory syndrome". 25 May 2020. Archived from the original on 11 July 2020. https://web.archive.org/web/20200711091231/https://www.shebaonline.org/new-inflammatory-syndrome/.
- ↑ 62.0 62.1 "Pediatric inflammatory multisystem syndrome with central nervous system involvement and hypocomplementemia following SARS-CoV-2 infection". The Pediatric Infectious Disease Journal. June 2020. doi:10.1097/INF.0000000000002804. PMID 32639461.
- ↑ 63.0 63.1 "Algeria registers first case of Kawasaki disease". DZ Breaking. Archived from the original on 11 July 2020. https://web.archive.org/web/20200711092523/https://www.dzbreaking.com/2020/06/16/algeria-registers-first-case-of-kawasaki-disease/.
- ↑ 64.0 64.1 "COVID-19 in Peru: from supervised walks for children to the first case of Kawasaki-like syndrome". BMJ 369: m2418. June 2020. doi:10.1136/bmj.m2418. PMID 32571770.
- ↑ 65.0 65.1 "45 casos probables de menores con síndrome inflamatorio multisistémico" (in es). Teleamazonas. 19 July 2020. Archived from the original on 20 July 2020. https://web.archive.org/web/20200720082615/http://www.teleamazonas.com/etiqueta/sindrome-relacionado-al-covid/.
- ↑ 66.0 66.1 "COVID-19 and Kawasaki disease: novel virus and novel case". Hospital Pediatrics 10 (6): 537–540. 2020. doi:10.1542/hpeds.2020-0123. PMID 32265235. https://hosppeds.aappublications.org/content/hosppeds/early/2020/04/06/hpeds.2020-0123.full-text.pdf.
- ↑ "COVID-19: concerns grow over inflammatory syndrome emerging in children". BMJ 369: m1710. 2020. doi:10.1136/bmj.m1710. PMID 32345602. https://www.bmj.com/content/369/bmj.m1710.full. "The alert, which relayed information from NHS England, said, 'It has been reported that over the past three weeks there has been an apparent rise in the number of children of all ages presenting with a multisystem inflammatory state requiring intensive care across London and other regions of the UK.'".
- ↑ "Rising cases of kids with Kawasaki disease possibly linked to coronavirus". Kyodo News. 30 April 2020. Archived from the original on 13 May 2020. https://web.archive.org/web/20200513132001/https://english.kyodonews.net/news/2020/04/05476c47050f-rising-cases-of-kids-with-kawasaki-disease-possibly-linked-to-virus.html.
- ↑ Daskalakis, DC (4 May 2020). "2020 Health alert #13: pediatric multi-system inflammatory syndrome potentially associated with COVID-19". NYC Health. Archived from the original on 6 May 2020. https://web.archive.org/web/20200506033213/https://www1.nyc.gov/assets/doh/downloads/pdf/han/alert/2020/covid-19-pediatric-multi-system-inflammatory-syndrome.pdf.
- ↑ "Governor Cuomo announces State is helping to develop the national criteria for identifying and responding to COVID-related illness in children" (in en). 9 May 2020. Archived from the original on 10 May 2020. https://www.governor.ny.gov/news/governor-cuomo-announces-state-helping-develop-national-criteria-identifying-and-responding.
- ↑ "Coronavirus: Children affected by rare Kawasaki-like disease". 14 May 2020. https://www.bbc.com/news/health-52648557. Retrieved 24 May 2020.
- ↑ d'Adhémar, Margaux (15 May 2020). "Coronavirus : 135 enfants français atteints d'une forme proche de la maladie de Kawasaki, un mort" (in fr). https://www.lefigaro.fr/sciences/coronavirus-135-enfants-francais-atteints-d-une-forme-proche-de-la-maladie-de-kawasaki-un-mort-20200515. Retrieved 16 May 2020.
- ↑ Deloughry, Rachel (26 May 2020). "20 children in the Netherlands contract illness thought to be linked to COVID-19". www.iamexpat.nl. https://www.iamexpat.nl/expat-info/dutch-expat-news/20-children-netherlands-contract-illness-thought-be-linked-covid-19. Retrieved 27 May 2020.
- ↑ "COVID-19 Fragen und Antworten Teil 11" (in de-DE). 12 May 2020. https://paediatrica.swiss-paediatrics.org/covid-19-fragen-und-antworten-teil-11/. Retrieved 16 May 2020.
- ↑ Irmer, Juliette (15 May 2020). ""Kawasaki" durch Covid-19?: Auch deutsche Kinder mit schweren Entzündungsreaktionen" (in de). https://www.faz.net/aktuell/wissen/corona-auch-deutsche-kinder-mit-schweren-entzuendungsreaktionen-16770951.html. Retrieved 16 May 2020.
- ↑ "With over 200 possible cases, doctors warn reports of rare, coronavirus-linked child inflammatory illness likely to rise". 15 May 2020. https://abcnews.go.com/Health/200-cases-doctors-warn-reports-rare-coronavirus-linked/story?id=70703314. Retrieved 16 May 2020.
- ↑ McNamara, Audrey (13 May 2020). "15 states now investigating child illness possibly linked to coronavirus, Cuomo says". www.cbsnews.com. https://www.cbsnews.com/news/kawasaki-disease-15-states-child-illness-coronavirus-cuomo/. Retrieved 14 May 2020.
- ↑ Marsh, Julia; Musumeci, Natalie (18 May 2020). "145 NYC kids have rare Kawasaki-like disease linked to coronavirus". New York Post. https://nypost.com/2020/05/18/145-nyc-kids-have-rare-kawasaki-like-disease-linked-to-coronavirus/. Retrieved 19 May 2020.
- ↑ 79.0 79.1 "Multisystem inflammatory syndrome in U.S. children and adolescents". The New England Journal of Medicine. June 2020. doi:10.1056/NEJMoa2021680. PMID 32598831.
- ↑ "Infographic: Early Cases of MIS-C: Multi-System Inflammatory Syndrome in U.S. Children" (in en-us). Centers for Disease Control and Prevention. 9 July 2020. Archived from the original on 10 July 2020. https://web.archive.org/web/20200710025733/https://www.cdc.gov/coronavirus/2019-ncov/covid-data/infographic-mis-c.html.
- ↑ "Paediatric inflammatory multisystem syndrome: temporally associated with SARS-CoV-2 (PIMS-TS): cardiac features, management and short-term outcomes at a UK tertiary paediatric hospital". Pediatric Cardiology. June 2020. doi:10.1007/s00246-020-02391-2. PMID 32529358.
- ↑ "Severe SARS-CoV-2 infection in children with suspected acute abdomen: a case series from a tertiary hospital in Spain". The Pediatric Infectious Disease Journal. May 2020. doi:10.1097/INF.0000000000002777. PMID 32467457.
- ↑ "Acute myocarditis and multisystem inflammatory emerging disease following SARS-CoV-2 infection in critically ill children". Annals of Intensive Care 10 (1): 69. June 2020. doi:10.1186/s13613-020-00690-8. PMID 32488505.
- ↑ "Kawasaki-like multisystem inflammatory syndrome in children during the covid-19 pandemic in Paris, France: prospective observational study". BMJ 369: m2094. June 2020. doi:10.1136/bmj.m2094. PMID 32493739.
- ↑ "Paediatric multisystem inflammatory syndrome temporally associated with SARS-CoV-2 mimicking Kawasaki disease (Kawa-COVID-19): a multicentre cohort". Annals of the Rheumatic Diseases. June 2020. doi:10.1136/annrheumdis-2020-217960. PMID 32527868.
- ↑ "Multisystem inflammatory syndrome in children during the COVID-19 pandemic: a case series". Journal of the Pediatric Infectious Diseases Society. May 2020. doi:10.1093/jpids/piaa069. PMID 32463092.
- ↑ "Clinical characteristics of 58 children with a pediatric inflammatory multisystem syndrome temporally associated with SARS-CoV-2". JAMA. June 2020. doi:10.1001/jama.2020.10369. PMID 32511692.
- ↑ "Multisystem inflammatory syndrome in children (MIS-C) associated with SARS-CoV-2 infection: a multi-institutional study from New York City". The Journal of Pediatrics. June 2020. doi:10.1016/j.jpeds.2020.06.045. PMID 32553861.
- ↑ "Multisystem inflammatory syndrome in children in New York State". The New England Journal of Medicine. June 2020. doi:10.1056/NEJMoa2021756. PMID 32598830.
- ↑ "U.S. counts 342 child inflammatory syndrome cases". TribLIVE.com. Associated Press. 16 July 2020. Archived from the original on 17 July 2020. https://web.archive.org/web/20200717101538/https://triblive.com/news/health-now/u-s-counts-342-child-inflammatory-syndrome-cases/.
- ↑ "CDC: 71% of MIS-C patients Hispanic or Black" (in en). American Academy of Pediatrics. 16 July 2020. Archived from the original on 17 July 2020. https://web.archive.org/web/20200717124958/https://www.aappublications.org/news/2020/07/16/miscdata071620.
- ↑ "COVID-19: aparece primer caso de Kawasaki en Perú" (in es). Panamericana Televisión. 2 June 2020. Archived from the original on 10 June 2020. https://web.archive.org/web/20200610225535/https://panamericana.pe/buenosdiasperu/salud/294991-covid-19-aparece-primer-caso-kawasaki-peru.
- ↑ "Multisystem inflammatory syndrome in children in COVID-19 pandemic". Indian Journal of Pediatrics. July 2020. doi:10.1007/s12098-020-03440-7. PMID 32621172.
- ↑ "Kawasaki syndrome or MIS-C: Children recovering from COVID-19 also face the brunt of the disease". Firstpost. 20 July 2020. Archived from the original on 20 July 2020. https://web.archive.org/web/20200720083745oe_/https://www.firstpost.com/health/kawasaki-syndrome-or-mis-c-children-recovering-from-covid-19-also-face-the-brunt-of-the-disease-8538361.html.
- ↑ "Egypt free from Kawasaki disease: Cabinet". EgyptToday. 10 July 2020. Archived from the original on 11 July 2020. https://web.archive.org/web/20200711093936/https://www.egypttoday.com/Article/1/89509/Egypt-free-from-Kawasaki-disease-Cabinet.
- ↑ "Bilateral anterior uveitis as a part of a multisystem inflammatory syndrome secondary to COVID-19 infection". Journal of Medical Virology. June 2020. doi:10.1002/jmv.26229. PMID 32592496.
- ↑ "Youngest Israeli victim: 26-year-old man dies from rare complication of COVID-19". Times of Israel. 14 June 2020. Archived from the original on 6 July 2020. https://web.archive.org/web/20200706070759/https://www.timesofisrael.com/26-year-old-man-dies-from-rare-complication-of-covid-19/.
- ↑ "COVID-19 associated Kawasaki-like multisystem inflammatory disease in an adult". The American Journal of Emergency Medicine. June 2020. doi:10.1016/j.ajem.2020.06.053. PMID 32631771.
- ↑ "An adult with Kawasaki-like multisystem inflammatory syndrome associated with COVID-19". The Lancet. July 2020. doi:10.1016/S0140-6736(20)31526-9. PMID 32659211.
External links
- Fact sheet for parents released by New York City's Health Department
- Information for parents provided by the Children's Hospital Los Angeles
- Information for paediatric health care providers in the U.S.A. (from the CDC)
- Web seminar hosted by CDC Clinician Outreach and Communication Activity (COCA)
- PMIS explained by Don't Forget the Bubbles
| Classification |
|---|
