Biology:Staphylococcus haemolyticus
| Staphylococcus haemolyticus | |
|---|---|
| |
| Scientific classification | |
| Domain: | Bacteria |
| Phylum: | Bacillota |
| Class: | Bacilli |
| Order: | Bacillales |
| Family: | Staphylococcaceae |
| Genus: | Staphylococcus |
| Species: | S. haemolyticus
|
| Binomial name | |
| Staphylococcus haemolyticus Schleifer & Kloos, 1975[1]
| |
Staphylococcus haemolyticus is a member of the coagulase-negative staphylococci (CoNS).[2] It is part of the skin flora of humans,[3] and its largest populations are usually found at the axillae, perineum, and inguinal areas.[4] S. haemolyticus also colonizes primates and domestic animals.[4] It is a well-known opportunistic pathogen, and is the second-most frequently isolated CoNS (S. epidermidis is the first).[5] Infections can be localized or systemic, and are often associated with the insertion of medical devices.[6][7][8] The highly antibiotic-resistant phenotype and ability to form biofilms make S. haemolyticus a difficult pathogen to treat.[5] Its most closely related species is Staphylococcus borealis.[9]
Biology and biochemistry
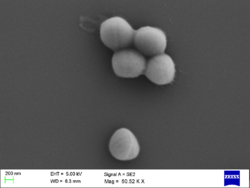
S. haemolyticus is nonmotile, nonsporulating, facultatively anaerobic, and Gram-positive. Cells are typically coccus-shaped and range from 0.8-1.3 μm in diameter. It lives on a wide variety of substrates, including glucose, glycerol, maltose, sucrose, and trehalose. It also tests positive for acetoin production, arginine, dihydrolase, benzidine, catalase, hemolysis, and lipase; it tests negative for coagulase, DNase, ornithine decarboxylase and phosphatase[2]
Growth conditions
Optimal growth occurs between 30 and 40 °C in the presence of oxygen and 10% NaCl. However, some strains can grow at temperatures that range between 18 and 45 °C. Growth at 15 °C or 15% NaCl is poor or absent.[2]
Genome structure
The S. haemolyticus strain JCSC1435 genome contains a 2,685,015 bp chromosome and three plasmids of 2,300 bp, 2,366 bp, and 8,180 bp. The chromosome is comparable in size to those of S. aureus and S. epidermidis and contains a similar G+C content. In addition, a large proportion of the open reading frames (ORFs) are conserved across all three species. On average, orthologous ORFs are 78% identical. However, S. haemolyticus does have unique chromosome regions distributed near oriC (the origin of chromosomal DNA replication), and these regions are collectively referred to as the “oriC environ”.[10]
As noted, some S. haemolyticus ORFs differ from S. aureus and S. epidermidis. Some of these ORFs encode gene products with known biological features, such as the regulation of RNA synthesis, the transport of ribose and ribitol, and the essential components of nucleic acid and cell wall teichoic acid biosynthesis. Other unique ORFs likely encode products involved with bacterial pathogenesis and at least three of these ORFs show homology to staphylococcal hemolysins.[10]
The S. haemolyticus genome also contains many insertion sequences (ISs). These IS elements may promote frequent genomic rearrangements which accelerate the diversification of the species. Theoretically, these adaptations might help S. haemolyticus overcome the adverse effects of chemical exposure (i.e. the use of antibiotics). The table below contains a list of genes known to be associated with S. haemolyticus antibiotic resistance.[10][11]
| Class | Antimicrobial Agent | MIC (mg/L) | ORF ID | Gene Name | Product | Location |
|---|---|---|---|---|---|---|
| Penicillins | Oxacillin | >512 | SH0091 | mecA | Penicillin-binding protein 2' | ΨSCCmec(h1435) |
| Ampicillin | 64 | SH1764 | blaZ | β-Lactamase | Tn552 | |
| methicillin | mecA | Penicillin-binding protein 2' | ΨSCCmec(h1435) | |||
| Cephalosporins | Ceftizoxime | >512 | SH0091 | mecA | Penicillin-binding protein 2' | ΨSCCmec(h1435) |
| Macrolides | Erythromycin | >512 | pSHaeB1 | ermC | rRNA adenine N-6-methyltransferase | Plasmid pSHaeB |
| SH2305 | msrSA | ATP-dependent efflux system | πSh1 | |||
| SH2306 | mphBM | Macrolide 2'-phosphotransferase | πSh1 | |||
| Quinolones | Ofloxacin | 8 | SH0006 | gyrA | DNA gyrase (topoisomerase II) subunit A (point mutation C7313T) | |
| SH1553 | parC (grlA) | Topoisomerase IV subunit A (point mutation G1598138A) | ||||
| Tetracyclines | Tetracycline | 2 | ||||
| Minocycline | 0.5 | |||||
| Aminoglycosides | Kanamycin | >512 | SH1611 | aacA-aphD | Bifunctional aminoglycoside N-acetyltransferase and aminoglycoside phosphotransferase | Tn4001 |
| Tobramycin | 16 | SH1611 | aacA-aphD | Bifunctional | Tn4001 | |
| Gentamicin | 64 | SH1611 | aacA-aphD | Bifunctional | Tn4001 | |
| Glycopeptides | Vancomycin | 4 | ||||
| Teicoplanin | 64 | |||||
| Fosfomycin | Fosfomycin | >512 | pSHaeA1 | fosB | Glutathione transferase | Plasmid pSHaeA |
Cell wall
Like other Gram-positive microbes, S. haemolyticus has a thick, rather homogenous, cell wall (60-80 nm) composed of peptidoglycan, teichoic acid, and protein. Peptidoglycan of group A3 (with L-lysine as the diamino acid in position 3 of the peptide subunit and a glycine-rich interpeptide bridge) is a characteristic feature of this microbe, and the two predominant cross-bridges are COOH-Gly-Gly-Ser-Gly-Gly-NH2 and COOH-Ala-Gly-Ser-Gly-Gly-NH2.[2][12] Alterations of these cross-bridges are implicated in glycopeptide resistance.[12] S. haemolyticus teichoic acids are water-soluble polymers with repeating phosphodiester groups covalently linked to peptidoglycan. Peptidoglycan type L-Lys-Gly 3.5-4.0, L-Ser0.9-1.5 Teichoic acid contains both glycerol and N-acetylglucosamine. The major cell wall fatty acids are CBr-15, CBr-17, C18, and C20.[2]
Capsule
Certain strains of S. haemolyticus are capable of producing a capsular polysaccharide (CP).[10][13] S. haemolyticus strain JCSC1435 contains a capsule operon located within the “oriC environ”.[10] This operon contains 13 ORFs in a 14,652-bp region and is referred to as the capsh locus. The first seven genes of capsh (capAsh through capGsh) are homologous to the S. aureus cap5 or cap8 locus. However, capH through capM are unique to S. haemolyticus,[10] and this region encodes enzymes for a unique trideoxy sugar residue that is N-acylated by aspartic acid.[13]
CP production is influenced by culture medium and growth phase. Cultivation in tryptic soy broth (TSB)], TSB with 1% glucose, brain heart infusion broth, or Columbia broth with 2% NaCl favors the production of CP; cultivation on Columbia salt agar plates is suboptimal. Only trace amounts of CP are generated before the end of exponential phase, and the maximal rate of CP production does not occur until early stationary phase.[13]
CP is considered a virulence factor because it provides resistance against complement-mediated polymorphonuclear neutrophil phagocytosis.[citation needed]
Biofilm formation
The ability to adhere to medical devices and subsequently form biofilms is a major virulence factor associated with S. haemolyticus.[3][5][14][15] Biofilm formation increases antibiotic resistance[5][14][15] and often leads to persistent infections.[16][17] S. haemolyticus biofilms are not polysaccharide intercellular adhesin (PIA) dependent, and the lack of the ica operon (the gene cluster that encodes the production of PIA) can be used to distinguish S. haemolyticus isolates from other CoNS species.[3][13][15]
Biofilm formation is influenced by a variety of factors including carbohydrates, proteins, and extracellular DNA. Detachment assays with NaIO4, proteinase K, or DNase result in 38%, 98%, and 100% detachment, respectively. The high level of detachment associated with DNase treatment has led several authors to suggest a cell-to-surface and/or cell-to-cell adhesion function for extracellular DNA. Biofilm formation also appears to be influenced by the presence of glucose and NaCl. Biofilm formation is enhanced when cultivated in TSB with 1% glucose and decreased when cultivated in TSB with 3% NaCl.[15] The production of a capsular polysaccharide decreases biofilm formation.[13]
Subinhibitory concentrations (subminimum inhibitory concentrations) of the antibiotic dicloxacillin also affect the growth of S. haemolyticus biofilms. Biofilms formed in the presence of subinhibitory concentrations of dicloxacillin contain less biomass and have an altered composition. They are thinner, cover less surface area, and are less hydrophobic, but they also have an increased level of resistance to dicloxacillin.[14]
Toxins
Some S. haemolyticus strains produce enterotoxins (SE) and/or hemolysins.[10][18] In a study of 64 S. haemolyticus strains, production of SEA, SEB, SEC, and/or SEE was noted (only SED was absent). In addition, 31.3% of the strains were found to produce at least one type of enterotoxin.[18]
Identification
S. haemolyticus can be identified on the species level using a variety of manual and automated methods. The most frequently employed are: the reference method (based on growth tests), API ID 32 Staph (bioMe´rieux), Staph-Zym (Rosco), UZA (a rapid 4-h method), and polymerase chain reaction and electrophoretic analysis of the 16S rRNA, hsp60, or sodA gene sequence. Preference towards a particular method usually depends on convenience, economics, and required specificity (some species have identical 16S rRNA).[7][19] The most closely related species of S. haemolyticus is Staphylococcus borealis.[9]
| Method | Tests performed | Interpretation |
|---|---|---|
| Reference | 16 conventional growth tests including: colony pigment, DNase, alkaline phosphatase, ornithine decarboxylase, urease, acetoin production, novobiocin sensitive, polymyxin resistance, and acid production from D-trehalose, D-mannitol, D-mannose, D-turanose, D-xylose, D-cellobiose, maltose, and sucrose | Results are compared to the literature on staphylococcal species[19] |
| API ID 32 Staph (bioMe´rieux) | A bacterial suspension is added to a set of wells containing dried substrates for 26 colorimetric tests. | After 24 hours of incubation at 37 °C, and the addition of a few other reagents, the results are determined by an automated computer using APILAB ID 32 software[19] |
| Staph-Zym (Rosco) | A bacterial suspension is added to minitubes for 10 metabolic or enzymatic tests | The results are determined by color changes, after 24 hours of incubation, and tests for polymyxin and novobiocin susceptibility[19] |
| UZA (a rapid 4-hour method) | This method is a two-step process. Step one consists of three tests measured after four hours incubation at 37 °C: acid production from D-trehalose, urease, and alkaline phosphatase. Step two includes four possible tests, which are administered as needed after 24 hours of incubation at 37 °C. They are: ornithine decarboxylase, novobiocin susceptibility, fosfomycin susceptibility, and anaerobic growth | Results are compared to the literature on staphylococcal species[19] |
| PCR and electrophoresis | Uses gene specific degenerate primers to amplify pieces of DNA, these fragments are resolved using electrophoresis, and then purified for DNA sequencing | Results are determined by a sequence analysis[7] |
Clinical importance
S. haemolyticus is the second-most clinically isolated CoNS (S. epidermidis is the first) and it is considered an important nosocomial pathogen.[20] Human infections include: native valve endocarditis, sepsis, peritonitis, and urinary tract, wound, bone, and joint infections.[3][4][5][13] Infrequent soft-tissue infections usually occur in immunocompromised patients.[21] Like other CoNS, S. haemolyticus is often associated with the insertion of foreign bodies, such as prosthetic valves, cerebrospinal fluid shunts, orthopedic prostheses, and intravascular, urinary, and dialysis catheters.[6][7][8] S. haemolyticus is multi-drug resistant[22] and able to form biofilms, which makes infections especially difficult to treat.[17]
Vascular catheter-associated infections
S. haemolyticus can colonize central venous catheters and cause serious medical complications. Colonization occurs when S. haemolyticus migrates from the skin, along the external surface of the device, or from the hub, due to manipulation by health care workers. In either scenario, a high probability exists that the microbe will form a biofilm. These infections can remain localized or become systemic (i.e. bacteremia). The severity of infection varies depending on the type of catheter, frequency of manipulation, and virulence factors of the S. haemolyticus strain. Removal of the catheter is usually considered to be the best treatment, but this is not always possible. Alternatively, vancomycin or teicoplanin may be administered.[8] Recent evidence suggests that glycopeptides can be supplemented with β-lactams to work synergistically.[20]
Antibiotic resistance
S. haemolyticus has the highest level of antibiotic resistance among the CoNS.[15] Various strains are resistant to one or more of these antibiotics: penicillins, cephalosporins, macrolides, quinolones, tetracyclines, aminoglycosides, glycopeptides, and fosfomycin (see table in Genome structure),[5][10][22][23] and multidrug resistance is common.[22] As indicated above, even glycopeptide-resistant (vancomycin and teicoplanin) strains have begun to emerge.[6][20][24][25]
References
- ↑ Schleifer, K. H.; Kloos, W. E. (1975). "Isolation and Characterization of Staphylococci from Human Skin I. Amended Descriptions of Staphylococcus epidermidis and Staphylococcus saprophyticus and Descriptions of Three New Species: Staphylococcus cohnii, Staphylococcus haemolyticus, and Staphylococcus xylosus". International Journal of Systematic Bacteriology 25 (1): 50–61. doi:10.1099/00207713-25-1-50. ISSN 0020-7713.
- ↑ 2.0 2.1 2.2 2.3 2.4 Bergey's Manual of Systematic Bacteriology. 3 The Firmicutes (2nd ed.). Springer-Verlag. 2009. ISBN 978-0-387-95041-9.
- ↑ 3.0 3.1 3.2 3.3 de Silva (2002). "The ica Operon and Biofilm Production in Coagulase-Negative Staphylococci Associated with Carriage and Disease in a Neonatal Intensive Care Unit". Journal of Clinical Microbiology 40 (2): 382–388. doi:10.1128/jcm.40.02.382-388.2002. PMID 11825946.
- ↑ 4.0 4.1 4.2 Fischetti, A.; Novick, R. P.; Ferretti, J. J.; Portnoy, D. A.; Rood, J. I.; Lina, G.; Etienne, J.; Vandenesch, F. (2000). "Biology and pathogenicity of staphylococci other than Staphylococcus aureus and Staphylococcus epidermidis". Gram-positive pathogens. Washington, D.C.: ASM Press. pp. 450–462. ISBN 978-1-55581-166-2.
- ↑ 5.0 5.1 5.2 5.3 5.4 5.5 de Allori (2006). "Antimicrobial Resistance and Production of Biofilms in Clinical Isolates of Coagulase-Negative Staphylococcus Strains". Biol. Pharm. Bull. 29 (8): 1592–1596. doi:10.1248/bpb.29.1592. PMID 16880610. http://www.jstage.jst.go.jp/article/bpb/29/8/1592/_pdf.
- ↑ 6.0 6.1 6.2 Falcone (2006). "Teicoplanin use and emergence of Staphylococcus haemolyticus: is there a link?". Clin Microbiol Infect 12 (1): 96–97. doi:10.1111/j.1469-0691.2005.01307.x. PMID 16460556.
- ↑ 7.0 7.1 7.2 7.3 Poyart (2001). "Rapid and Accurate Species-Level Identification of Coagulase-Negative Staphylococci by Using the sodA Gene as a Target". Journal of Clinical Microbiology 39 (12): 4296–4301. doi:10.1128/JCM.39.12.4296-4301.2001. PMID 11724835.
- ↑ 8.0 8.1 8.2 Viale, P.; Stefani, S. (2006). "Vascular catheter-associated infections: a microbiological and therapeutic update". J Chemother 18 (3): 235–49. doi:10.1179/joc.2006.18.3.235. PMID 17129833.
- ↑ 9.0 9.1 Pain, Maria; Wolden, Runa; Jaén-Luchoro, Daniel; Salvà-Serra, Francisco; Iglesias, Beatriz Piñeiro; Karlsson, Roger; Klingenberg, Claus; Cavanagh, Jorunn Pauline (2020-10-13). "Staphylococcus borealis sp. nov., isolated from human skin and blood" (in en). International Journal of Systematic and Evolutionary Microbiology 70 (12): 6067–6078. doi:10.1099/ijsem.0.004499. ISSN 1466-5026. PMID 33048039. https://www.microbiologyresearch.org/content/journal/ijsem/10.1099/ijsem.0.004499.
- ↑ 10.0 10.1 10.2 10.3 10.4 10.5 10.6 10.7 Takeuchi (2005). "Whole-Genome Sequencing of Staphylococcus haemolyticus Uncovers the Extreme Plasticity of Its Genome and the Evolution of Human-Colonizing Staphylococcal Species". Journal of Bacteriology 187 (21): 7292–7308. doi:10.1128/JB.187.21.7292-7308.2005. PMID 16237012.
- ↑ Bouchami (2011). "Antibiotic resistance and molecular characterization of clinical isolates of methicillin-resistant coagulase-negative staphylococci isolated from bacteremic patients in oncohematology". Folia Microbiol 56 (2): 122–30. doi:10.1007/s12223-011-0017-1. PMID 21431912.
- ↑ 12.0 12.1 Billet-klein (1996). "Peptidoglycan Synthesis and Structure in Staphylococcus haemolyticus Expressing Increasing Levels of Resistance to Glycopeptide Antibiotics". Journal of Bacteriology 178 (15): 4696–4703. doi:10.1128/jb.178.15.4696-4703.1996. PMID 8755902.
- ↑ 13.0 13.1 13.2 13.3 13.4 13.5 Flahaut (2008). "Structural and Biological Characterization of a Capsular Polysaccharide Produced by Staphylococcus haemolyticus". Journal of Bacteriology 190 (5): 1649–1657. doi:10.1128/JB.01648-07. PMID 18165309.
- ↑ 14.0 14.1 14.2 Cerca (2005). "Comparative assessment of antibiotic susceptibility of coagulasenegative staphylococci in biofilm versus planktonic culture as assessed by bacterial enumeration or rapid XTT colorimetry". J Antimicrob Chemother 56 (2): 331–336. doi:10.1093/jac/dki217. PMID 15980094.
- ↑ 15.0 15.1 15.2 15.3 15.4 Fredheim (2009). "Biofilm Formation by Staphylococcus haemolyticus". Journal of Clinical Microbiology 47 (4): 1172–1180. doi:10.1128/JCM.01891-08. PMID 19144798.
- ↑ Costerton (1999). "Bacterial Biofilms: A Common Cause of Persistent Infections". Science 284 (5418): 1318–1322. doi:10.1126/science.284.5418.1318. PMID 10334980. Bibcode: 1999Sci...284.1318C. https://scholarworks.montana.edu/xmlui/handle/1/14368.
- ↑ 17.0 17.1 Klingenberg (2007). "Persistent strains of coagulase-negative staphylococci in a neonatal intensive care unit: virulence factors and invasiveness". Clin Microbiol Infect 13 (11): 1100–11. doi:10.1111/j.1469-0691.2007.01818.x. PMID 17850346.
- ↑ 18.0 18.1 Valle (1990). "Enterotoxin Production by Staphylococci Isolated from Healthy Goats". Applied and Environmental Microbiology 56 (5): 1323–1326. doi:10.1128/AEM.56.5.1323-1326.1990. PMID 2339886.
- ↑ 19.0 19.1 19.2 19.3 19.4 Ieven (1995). "Rapid and Economical Method for Species Identification of Clinically Significant Coagulase-Negative Staphylococci". Journal of Clinical Microbiology 33 (5): 1060–1063. doi:10.1128/JCM.33.5.1060-1063.1995. PMID 7615705.
- ↑ 20.0 20.1 20.2 C. Vignaroli; F. Biavasco; P. E. Varaldo (2006). "Interactions between Glycopeptides and β-Lactams against Isogenic Pairs of Teicoplanin-Susceptible and -Resistant Strains of Staphylococcus haemolyticus". Antimicrobial Agents and Chemotherapy 50 (7): 2577–2582. doi:10.1128/AAC.00260-06. PMID 16801450.
- ↑ Kufe DW, ed (2003). "Infections in Patients with Cancer". Cancer Medicine (6th ed.). BC Decker. ISBN 978-0-9631172-1-2. https://www.ncbi.nlm.nih.gov/books/bv.fcgi?highlight=Staphylococcus+haemolyticus&rid=cmed6.section.43615#43625.
- ↑ 22.0 22.1 22.2 "Antimicrobial resistance in nosocomial isolates of Staphylococcus haemolyticus". Antimicrob Agents Chemother 33 (4): 460–6. 1989. doi:10.1128/aac.33.4.460. PMID 2729941.
- ↑ Raponi (2005). "Antimicrobial susceptibility, biochemical and genetic profiles of Staphylococcus haemolyticus strains isolated from the bloodstream of patients hospitalized in critical care units". J Chemother 17 (3): 264–9. doi:10.1179/joc.2005.17.3.264. PMID 16038519.
- ↑ Chiew (2007). "Detection of vancomycin heteroresistant Staphylococcus haemolyticus and vancomycin intermediate resistant Staphylococcus epidermidis by means of vancomycin screening agar". Pathology 39 (3): 375–7. doi:10.1080/00313020701330441. PMID 17558874.
- ↑ Sieradzki, Krzysztof; Villari, Paolo; Tomasz, Alexander (1998). "Decreased Susceptibilities to Teicoplanin and Vancomycin among Coagulase-Negative Methicillin-Resistant Clinical Isolates of Staphylococci". Antimicrobial Agents and Chemotherapy 42 (1): 100–107. doi:10.1128/AAC.42.1.100. PMID 9449268.
External links
- Staphylococcus haemolyticus genome
- Type strain of Staphylococcus haemolyticus at BacDive - the Bacterial Diversity Metadatabase
Wikidata ☰ Q3760144 entry
 |


