Chemistry:Buprenorphine
 | |
 | |
| Clinical data | |
|---|---|
| Pronunciation | bew-pre-nor-feen |
| Trade names | Subutex, Sublocade, Brixadi, others |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a605002 |
| License data |
|
| Pregnancy category | |
| Dependence liability | Psychological: High Physical: Moderate[3] |
| Routes of administration | Under the tongue, through the cheek, intramuscular, intravenous, transdermal, intranasal, rectally, by mouth, subcutaneous |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Bioavailability | Sublingual: 30%[10] Intranasal: 48%[11] Buccal: 65%[12][13] |
| Protein binding | 96% |
| Metabolism | Liver (CYP3A4, CYP2C8) |
| Onset of action | Within 30 min[14] |
| Elimination half-life | 37 hours (range 20–70 hours) |
| Duration of action | Up to 24 hrs[14] |
| Excretion | Bile duct and kidney |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| Chemical and physical data | |
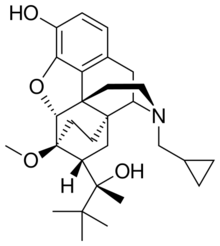
| Formula | C29H41NO4 |
| Molar mass | 467.650 g·mol−1 |
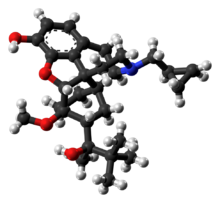
| 3D model (JSmol) | |
| |
| |
| | |
Buprenorphine, sold under the brand name Subutex among others, is an opioid used to treat opioid use disorder, acute pain, and chronic pain.[14] It can be used under the tongue (sublingual), in the cheek (buccal), by injection (intravenous and subcutaneous), as a skin patch (transdermal), or as an implant.[14][15] For opioid use disorder, it is typically started when withdrawal symptoms have begun and for the first two days of treatment under direct observation of a health-care provider.[14]
In the United States, the combination formulation of buprenorphine/naloxone (Suboxone) is usually prescribed to discourage misuse by injection.[14] However, more recently the efficacy of naloxone in preventing misuse has been brought into question, and preparations of buprenorphine combined with naloxone could potentially be less safe than buprenorphine alone.[16] Maximum pain relief is generally within an hour with effects up to 24 hours.[14] Buprenorphine affects different types of opioid receptors in different ways.[14] Depending on the type of opioid receptor, it may be an agonist, partial agonist, or antagonist.[14] Buprenorphine's activity as an agonist/antagonist is important in the treatment of opioid use disorder: it relieves withdrawal symptoms from other opioids and induces some euphoria, but also blocks the ability for many other opioids, including heroin, to cause an effect. Unlike full agonists like heroin or methadone, buprenorphine has a ceiling effect, such that taking more medicine past a certain point will not increase the effects of the drug.[17]
Side effects may include respiratory depression (decreased breathing), sleepiness, adrenal insufficiency, QT prolongation, low blood pressure, allergic reactions, constipation, and opioid addiction.[14][18] Among those with a history of seizures, a risk exists of further seizures.[14] Opioid withdrawal following stopping buprenorphine is generally less severe than with other opioids.[14] Whether use during pregnancy is safe is unclear, but use while breastfeeding is probably safe, since the dose the infant receives is 1-2% that of the maternal dose, on a weight basis.[19][14]
Buprenorphine was patented in 1965, and approved for medical use in the United States in 1981.[14][20] It is on the World Health Organization's List of Essential Medicines.[21] In addition to prescription as an analgesic it is a common medication used to treat opioid use disorders, such as addiction to heroin.[22] In 2020, it was the 186th most commonly prescribed medication in the United States, with more than 2.8 million prescriptions.[23][24] Buprenorphine may also be used recreationally for the high it can produce.[22] In the United States, buprenorphine is a schedule III controlled substance.[22]
Medical uses
Opioid use disorder

Buprenorphine is used to treat people with opioid use disorder.[14][25]: 84–7 In the U.S., the combination formulation of buprenorphine/naloxone is generally prescribed to deter injection, since naloxone, an opioid antagonist, is believed to cause acute withdrawal if the formulation is crushed and injected.[14][26]: 99 Taken orally, the naloxone has virtually no effect, due to the drug's extremely high first-pass metabolism and low bioavailability (2%).[27] However, the efficacy of naloxone in preventing misuse by injection has more recently been brought into question and preparations including naloxone could even be less safe than preparations containing solely buprenorphine. Anecdotally, posters on drug-related online forums have stated that they were able to attain a high by injecting preparations of buprenorphine despite being combined with naloxone.[16]
Before starting buprenorphine, individuals are generally advised to wait long enough after their last dose of opioid until they have some withdrawal symptoms to allow for the medication to bind the receptors, since if taken too soon, buprenorphine can displace other opioids bound to the receptors and precipitate an acute withdrawal. The dose of buprenorphine is then adjusted until symptoms improve, and individuals remain on a maintenance dose of 8–16 mg.[26]: 99–100 [28] Because withdrawal is uncomfortable and a deterrent for many patients, many have begun to call for different means of treatment initiation.[29] Some providers have begun to use the Bernese method, also known as microdosing, in which very small doses of buprenorphine are given while patients are still using street opioids, and without precipitating withdrawal, with medicine levels slowly titrated upward.[30][31]
Buprenorphine versus methadone
Both buprenorphine and methadone are medications used for detoxification and opioid replacement therapy, and appear to have similar effectiveness based on limited data.[32] Both are safe for pregnant women with opioid use disorder,[26]: 101 [28] although preliminary evidence suggests that methadone is more likely to cause neonatal abstinence syndrome.[33] In the US and European Union, only designated clinics can prescribe methadone for opioid use disorder, requiring patients to travel to the clinic daily. If patients are drug free for a period they may be permitted to receive "take home doses," reducing their visits to as little as once a week. Alternatively, up to a month's supply of buprenorphine has been able to be prescribed by clinicians in the US or Europe who have completed a basic training (8–24 hours in the US) and received a waiver/licence allowing prescription of the medicine.[25]: 84–5 In France, buprenorphine prescription for opioid use disorder has been permitted without any special training or restrictions since 1995, resulting in treatment of approximately ten times more patients per year with buprenorphine than with methadone in the following decade.[34] In 2021, seeking to address record levels of opioid overdose, the United States also removed the requirement for a special waiver for prescribing physicians.[35] Whether this change will be sufficient to impact prescription is unclear, since even before the change as many as half of physicians with a waiver permitting them to prescribe buprenorphine did not do so, and one third of non-waivered physicians reported that nothing would induce them to prescribe buprenorphine for opioid use disorder.[36]
Chronic pain
A transdermal patch is available for the treatment of chronic pain.[14] These patches are not indicated for use in acute pain, pain that is expected to last only for a short period of time, or pain after surgery, nor are they recommended for opioid addiction.[37]
Potency
With respect to equianalgesic dosing, when used sublingually, the potency of buprenorphine is about 40 to 70 times that of morphine.[38][39][40] When used as a transdermal patch, the potency of buprenorphine may be 100 to 115 times that of morphine.[38][41]
Adverse effects

Common adverse drug reactions associated with the use of buprenorphine, similar to those of other opioids, include nausea and vomiting, drowsiness, dizziness, headache, memory loss, cognitive and neural inhibition, perspiration, itchiness, dry mouth, shrinking of the pupils of the eyes (miosis), orthostatic hypotension, male ejaculatory difficulty, decreased libido, and urinary retention. Constipation and central nervous system (CNS) effects are seen less frequently than with morphine.[43] Central sleep apnea has also been reported as a side effect of long-term buprenorphine use.[44][45]
Respiratory effects
The most severe side effect associated with buprenorphine is respiratory depression (insufficient breathing).[14] It occurs more often in those who are also taking benzodiazepines or alcohol, or have underlying lung disease.[14] The usual reversal agents for opioids, such as naloxone, may be only partially effective, and additional efforts to support breathing may be required.[14] Respiratory depression may be less than with other opioids, particularly with chronic use.[28] In the setting of acute pain management, though, buprenorphine appears to cause the same rate of respiratory depression as other opioids such as morphine.[46] Central sleep apnea is possible with long-term use, possibly resolving with dose reduction.[44][45]
Buprenorphine dependence
Buprenorphine treatment carries the risk of causing psychological or physiological (physical) dependencies. It has a slow onset of activity, with a long duration of action, and a long half-life of 24 to 60 hours. Once a patient has stabilised on the (buprenorphine) medication and programme, three options remain - continual use (buprenorphine-only medication), switching to a buprenorphine/naloxone combination, or a medically supervised withdrawal.[28]
Pain management
Achieving acute opioid analgesia is difficult in persons using buprenorphine for pain management.[47] However, a systematic review found no clear benefit to bridging or stopping buprenorphine when used in opioid substitution therapy to facilitate perioperative pain management, but failure to restart it was found to pose concerns for relapse. Therefore, it is recommended that buprenophine opioid substitution therapy is continued in the perioperative period when possible. In addition preoperative pain management in patients taking buprenorphine should use an interdisciplinary approach with multimodal analgesia.[48]
Pharmacology
Pharmacodynamics
| Site | Ki (nM) | Action | Species | Ref |
|---|---|---|---|---|
| KOR | 0.62–2.5 0.44 |
Antagonist | Human Monkey |
[49][50][51] [52] |
| NOP | 77.4 | Partial agonist | Human | [53][50][51] |
| σ1 | >100,000 | ND | ND | [54] |
| σ2 | ND | ND | ND | ND |
| NMDA | ND | ND | ND | ND |
| NET | >100,000 | ND | Rat | [55] |
| DAT | ND | ND | ND | ND |
| Values are Ki (nM), unless otherwise noted. The smaller the value, the more strongly the drug binds to the site. | ||||
Opioid receptor modulator
Buprenorphine has been reported to possess these following pharmacological activities:[50]
- μ-Opioid receptor (MOR): Very high affinity partial agonist:[56] at low doses, the MOR-mediated effects of buprenorphine are comparable to those of other narcotics, but these effects reach a "ceiling" as the receptor population is saturated.[51] This behavior is responsible for several unique properties: buprenorphine greatly reduces the effect of most other MOR agonists,[57] can cause precipitated withdrawal when used in actively opioid dependent persons,[57] and has a lower incidence of respiratory depression and fatal overdose relative to full MOR agonists.[58]
- κ-Opioid receptor (KOR): High affinity antagonist[56]—this activity is hypothesized to underlie some of the effects of buprenorphine on mood disorders and addiction.[59][60][61]
- δ-Opioid receptor (DOR): High affinity antagonist[56][62]
- Nociceptin receptor (NOP, ORL-1): Weak affinity, very weak partial agonist[56]
In simplified terms, buprenorphine can essentially be thought of as a nonselective, mixed agonist–antagonist opioid receptor modulator,[63] acting as an unusually high affinity, weak partial agonist of the MOR, a high affinity antagonist of the KOR and DOR, and a relatively low affinity, very weak partial agonist of the ORL-1/NOP.[51][64][57][65][66][67]
Although buprenorphine is a partial agonist of the MOR, human studies have found that it acts like a full agonist with respect to analgesia in opioid-intolerant individuals.[68] Conversely, buprenorphine behaves like a partial agonist of the MOR with respect to respiratory depression.[68]
Buprenorphine is also known to bind to with high affinity and antagonize the putative ε-opioid receptor.[69][70]
Full analgesic efficacy of buprenorphine requires both exon 11-[71] and exon 1-associated μ-opioid receptor splice variants.[72]
The active metabolites of buprenorphine are not thought to be clinically important in its CNS effects.[68]
In positron emission tomography (PET) imaging studies, buprenorphine was found to decrease whole-brain MOR availability due to receptor occupancy by 41% (i.e., 59% availability) at 2 mg, 80% (i.e., 20% availability) at 16 mg, and 84% (i.e., 16% availability) at 32 mg.[73][74][75][76]
Other actions
Unlike some other opioids and opioid antagonists, buprenorphine binds only weakly to and possesses little if any activity at the sigma receptor.[77][78]
Buprenorphine also blocks voltage-gated sodium channels via the local anesthetic binding site, and this underlies its potent local anesthetic properties.[79]
Similarly to various other opioids, buprenorphine has also been found to act as an agonist of the toll-like receptor 4, albeit with very low affinity.[80]
Pharmacokinetics
Buprenorphine is metabolized by the liver, via CYP3A4 (also CYP2C8 seems to be involved) isozymes of the cytochrome P450 enzyme system, into norbuprenorphine (by N-dealkylation). The glucuronidation of buprenorphine is primarily carried out by UGT1A1 and UGT2B7, and that of norbuprenorphine by UGT1A1 and UGT1A3. These glucuronides are then eliminated mainly through excretion into bile. The elimination half-life of buprenorphine is 20 to 73 hours (mean 37 hours). Due to the mainly hepatic elimination, no risk of accumulation exists in people with renal impairment.[81]
One of the major active metabolites of buprenorphine is norbuprenorphine, which, in contrast to buprenorphine itself, is a full agonist of the MOR, DOR, and ORL-1, and a partial agonist at the KOR.[82][83] However, relative to buprenorphine, norbuprenorphine has extremely little antinociceptive potency (1/50th that of buprenorphine), but markedly depresses respiration (10-fold more than buprenorphine).[84] This may be explained by very poor brain penetration of norbuprenorphine due to a high affinity of the compound for P-glycoprotein.[84] In contrast to norbuprenorphine, buprenorphine and its glucuronide metabolites are negligibly transported by P-glycoprotein.[84]
The glucuronides of buprenorphine and norbuprenorphine are also biologically active, and represent major active metabolites of buprenorphine.[85] Buprenorphine-3-glucuronide has affinity for the MOR (Ki = 4.9 pM), DOR (Ki = 270 nM) and ORL-1 (Ki = 36 μM), and no affinity for the KOR. It has a small antinociceptive effect and no effect on respiration. Norbuprenorphine-3-glucuronide has no affinity for the MOR or DOR, but does bind to the KOR (Ki = 300 nM) and ORL-1 (Ki = 18 μM). It has a sedative effect but no effect on respiration.
Chemistry
Buprenorphine is a semisynthetic derivative of thebaine,[86] and is fairly soluble in water, as its hydrochloride salt.[87] It degrades in the presence of light.[87]
Detection in body fluids
Buprenorphine and norbuprenorphine may be quantified in blood or urine to monitor use or non-medical recreational use, confirm a diagnosis of poisoning, or assist in a medicolegal investigation. A significant overlap of drug concentrations exists in body fluids within the possible spectrum of physiological reactions ranging from asymptomatic to comatose. Therefore, having knowledge of both the route of administration of the drug and the level of tolerance to opioids of the individual is critical when results are interpreted.[88]
History
In 1969, researchers at Reckitt and Colman (now Reckitt Benckiser) had spent 10 years attempting to synthesize an opioid compound "with structures substantially more complex than morphine [that] could retain the desirable actions whilst shedding the undesirable side effects". Physical dependence and withdrawal from buprenorphine itself remain important issues, since buprenorphine is a long-acting opioid.[89] Reckitt found success when researchers synthesized RX6029 which had showed success in reducing dependence in test animals. RX6029 was named buprenorphine and began trials on humans in 1971.[90][91] By 1978, buprenorphine was first launched in the UK as an injection to treat severe pain, with a sublingual formulation released in 1982.
Society and culture
Regulation
United States
In the United States, buprenorphine and buprenorphine with naloxone were approved for opioid use disorder by the Food and Drug Administration in October 2002.[92] The DEA rescheduled buprenorphine from a schedule V drug to a schedule III drug just before approval.[93] The ACSCN for buprenorphine is 9064, and being a schedule III substance, it does not have an annual manufacturing quota imposed by the DEA.[94] The salt in use is the hydrochloride, which has a free-base conversion ratio of 0.928.
In the years before buprenorphine/naloxone was approved, Reckitt Benckiser had lobbied Congress to help craft the Drug Addiction Treatment Act of 2000, which gave authority to the Secretary of Health and Human Services to grant a waiver to physicians with certain training to prescribe and administer schedule III, IV, or V narcotic drugs for the treatment of addiction or detoxification. Before this law was passed, such treatment was permitted only in clinics designed specifically for drug addiction.[95]
The waiver, which can be granted after the completion of an eight-hour course, was required for outpatient treatment of opioid addiction with buprenorphine from 2000 to 2021. Initially, the number of people each approved physician could treat was limited to 10. This was eventually modified to allow approved physicians to treat up to 100 people with buprenorphine for opioid addiction in an outpatient setting.[96] This limit was increased by the Obama administration, raising the number of patients to which doctors can prescribe to 275.[97] On 14 January 2021, the US Department of Health and Human Services announced that the waiver would no longer be required to prescribe buprenorphine to treat up to 30 people concurrently.[98]
New Jersey authorized paramedics to give buprenorphine to people at the scene after they have recovered from an overdose.[99]
Europe
In the European Union, Subutex and Suboxone, buprenorphine's high-dose sublingual tablet preparations, were approved for opioid use disorder treatment in September 2006.[100] In the Netherlands, buprenorphine is a list II drug of the Opium Law, though special rules and guidelines apply to its prescription and dispensation. In France, where buprenorphine prescription by general practitioners and dispensed by pharmacies has been permitted since the mid-1990s as a response to HIV and overdose risk. Deaths caused by heroin overdose were reduced by four-fifths between 1994 and 2002, and incidence of AIDS among people who inject drugs in France fell from 25% in the mid-1990s to 6% in 2010.[101]
Brand names
Buprenorphine is available under the trade names Cizdol, Brixadi (approved in the US by FDA for addiction treatment in 2023), Suboxone (with naloxone), Subutex (typically used for opioid use disorder), Zubsolv, Bunavail, Buvidal (approved in the UK, Europe and Australia for addiction treatment in 2018), Sublocade (approved in the US in 2018),[102][103][104] Probuphine, Temgesic (sublingual tablets for moderate to severe pain), Buprenex (solutions for injection often used for acute pain in primary-care settings), Norspan, and Butrans (transdermal preparations used for chronic pain).[87] In Poland buprenorphine is available under the trade names Bunondol (for pain treatment, when morphine is too little; amounts of 0.2mg and 0.4mg) and Bunorfin (for addicts substitution in amount of 2 and 8mg).
Research
Microdosing
There is some evidence that a buprenorphine microdosing regime, started before opioid withdrawal symptoms have started, can be effective in helping people transitioning away from opioid dependence.[105]
Depression
Some evidence supports the use of buprenorphine for depression.[106] Buprenorphine/samidorphan, a combination product of buprenorphine and samidorphan (a preferential μ-opioid receptor antagonist), appears useful for treatment-resistant depression.[107]
Cocaine dependence
In combination with samidorphan or naltrexone (μ-opioid receptor antagonists), buprenorphine is under investigation for the treatment of cocaine dependence, and recently demonstrated effectiveness for this indication in a large-scale (n = 302) clinical trial (at a high buprenorphine dose of 16 mg, but not a low dose of 4 mg).[108][109]
Neonatal abstinence
Buprenorphine has been used in the treatment of the neonatal abstinence syndrome,[110] a condition in which newborns exposed to opioids during pregnancy demonstrate signs of withdrawal.[111] In the United States, use currently is limited to infants enrolled in a clinical trial conducted under an FDA-approved investigational new drug (IND) application.[112] Preliminary research suggests that buprenorphine is associated with shorter time in hospital for neonates, compared to methadone.[113] An ethanolic formulation used in neonates is stable at room temperature for at least 30 days.[114]
Veterinary uses
Veterinarians administer buprenorphine for perioperative pain, particularly in cats, where its effects are similar to morphine. The drug's legal status and lower potential for human abuse makes it an attractive alternative to other opioids.[115]
It has veterinary medical use for treatment of pain in dogs and cats, as well as other animals.[116][117][118]
References
- ↑ "Buprenorphine Use During Pregnancy". 14 October 2019. https://www.drugs.com/pregnancy/buprenorphine.html.
- ↑ 2.0 2.1 https://www.tga.gov.au/resources/auspar/auspar-buprenorphine-0
- ↑ Today's Medical Assistant: Clinical and Administrative Procedures. Elsevier Health Sciences. 2012. p. 571. ISBN 9781455701506. https://books.google.com/books?id=YalYPI1KqTQC&pg=PA571. Retrieved 16 February 2020.
- ↑ "ARCHIVED - Report Stakeholder Workshop on a National Buprenorphine Program". 6 December 2004. https://www.canada.ca/en/health-canada/services/drugs-health-products/reports-publications/drug-products/report-stakeholder-workshop-national-buprenorphine-program-november-18-2004-health-canada.html.
- ↑ "Subutex (buprenorphine sublingual tablets), CIII Initial U.S. Approval: 1981". https://dailymed.nlm.nih.gov/dailymed/archives/fdaDrugInfo.cfm?archiveid=660696.
- ↑ "Sublocade- buprenorphine solution". 15 March 2023. https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=6189fb21-9432-45f8-8481-0bfaf3ccde95.
- ↑ "Butrans- buprenorphine patch, extended release". 26 June 2022. https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=794aa355-66de-41b8-aedf-f2c40f6bc664.
- ↑ "Brixadi- buprenorphine injection". 21 June 2023. https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=5d8a8fd0-8619-422a-a664-d1d2e8970f48.
- ↑ "FDA Approves New Buprenorphine Treatment Option for Opioid Use Disorder". U.S. Food and Drug Administration (Press release). 23 May 2023. Retrieved 26 May 2023.
- ↑ "Bioavailability of sublingual buprenorphine". Journal of Clinical Pharmacology 37 (1): 31–37. January 1997. doi:10.1177/009127009703700106. PMID 9048270.
- ↑ "The systemic availability of buprenorphine administered by nasal spray". The Journal of Pharmacy and Pharmacology 41 (11): 803–805. November 1989. doi:10.1111/j.2042-7158.1989.tb06374.x. PMID 2576057.
- ↑ "Buprenorphine / Naloxone Buccal Film (BUNAVAIL) C-III". September 2014. https://www.pbm.va.gov/PBM/clinicalguidance/abbreviatedreviews/Buprenorphine_NX_Buccal_Film_BUNAVAIL_%20Abbreviated_Review.pdf.
- ↑ "Bunavail (buprenorphine and naloxone buccal film), CIII Initial U.S. Approval: 2002". https://dailymed.nlm.nih.gov/dailymed/archives/fdaDrugInfo.cfm?archiveid=657905.
- ↑ 14.00 14.01 14.02 14.03 14.04 14.05 14.06 14.07 14.08 14.09 14.10 14.11 14.12 14.13 14.14 14.15 14.16 14.17 14.18 14.19 "Buprenorphine Hydrochloride". American Society of Health-System Pharmacists. 26 January 2017. https://www.drugs.com/monograph/buprenorphine-hydrochloride.html.
- ↑ "FDA approves first buprenorphine implant for treatment of opioid dependence". U.S. Food and Drug Administration (Press release). 26 May 2016. Archived from the original on 30 November 2017. Retrieved 12 December 2017.
- ↑ 16.0 16.1 "Reconsidering the Usefulness of Adding Naloxone to Buprenorphine". Frontiers in Psychiatry 11: 549272. 11 September 2020. doi:10.3389/fpsyt.2020.549272. PMID 33061915.
- ↑ "Buprenorphine vs methadone treatment: A review of evidence in both developed and developing worlds". Journal of Neurosciences in Rural Practice 3 (1): 45–50. January 2012. doi:10.4103/0976-3147.91934. PMID 22346191.
- ↑ "Buprenorphine". The Substance Abuse and Mental Health Services Administration. 15 June 2015. https://www.samhsa.gov/medication-assisted-treatment/medications-counseling-related-conditions/buprenorphine.
- ↑ "Buprenorphine use while Breastfeeding". https://www.drugs.com/breastfeeding/buprenorphine.html.
- ↑ Analogue-based Drug Discovery. John Wiley & Sons. 2006. p. 528. ISBN 9783527607495. https://books.google.com/books?id=FjKfqkaKkAAC&pg=PA528. Retrieved 29 May 2020.
- ↑ World Health Organization model list of essential medicines: 22nd list (2021). Geneva: World Health Organization. 2021. WHO/MHP/HPS/EML/2021.02.
- ↑ 22.0 22.1 22.2 "Buprenorphine". July 2019. https://www.samhsa.gov/medication-assisted-treatment/medications-counseling-related-conditions/buprenorphine.
- ↑ "The Top 300 of 2020". https://clincalc.com/DrugStats/Top300Drugs.aspx.
- ↑ "Buprenorphine - Drug Usage Statistics". https://clincalc.com/DrugStats/Drugs/Buprenorphine.
- ↑ 25.0 25.1 "Patient Assessment". Office-based buprenorphine treatment of opioid use disorder. Arlington, VA: American Psychiatric Association Publishing. 2018. ISBN 978-1-61537-170-9. OCLC 1002302926.
- ↑ 26.0 26.1 26.2 "Clinical Use of Buprenorphine". Office-based buprenorphine treatment of opioid use disorder. Arlington, VA: American Psychiatric Association Publishing. 2018. ISBN 978-1-61537-170-9. OCLC 1002302926.
- ↑ "Naloxone Hydrochloride". The American Society of Health-System Pharmacists. https://www.drugs.com/monograph/naloxone-hydrochloride.html.
- ↑ 28.0 28.1 28.2 28.3 "Buprenorphine". 31 May 2016. https://www.samhsa.gov/medication-assisted-treatment/treatment/buprenorphine.
- ↑ "A Plea From People Who Use Drugs to Clinicians: New Ways to Initiate Buprenorphine Are Urgently Needed in the Fentanyl Era". Journal of Addiction Medicine 16 (4): 389–391. January 2022. doi:10.1097/ADM.0000000000000952. PMID 35020693.
- ↑ "Use of microdoses for induction of buprenorphine treatment with overlapping full opioid agonist use: the Bernese method". Substance Abuse and Rehabilitation 7: 99–105. 20 July 2016. doi:10.2147/SAR.S109919. PMID 27499655.
- ↑ "Microinduction of Buprenorphine/Naloxone: A Review of the Literature". The American Journal on Addictions 30 (4): 305–315. July 2021. doi:10.1111/ajad.13135. PMID 33378137.
- ↑ "Buprenorphine for managing opioid withdrawal". The Cochrane Database of Systematic Reviews 2017 (2): CD002025. February 2017. doi:10.1002/14651858.CD002025.pub5. PMID 28220474.
- ↑ "Methadone Versus Buprenorphine for Opioid Use Dependence and Risk of Neonatal Abstinence Syndrome" (in en-US). Epidemiology 29 (2): 261–268. March 2018. doi:10.1097/EDE.0000000000000780. PMID 29112519. "Methadone is associated with increased risk of neonatal abstinence syndrome compared with buprenorphine in infants exposed in utero. This association is subject to minimal bias due to unmeasured confounding by severity of addiction.".
- ↑ "French field experience with buprenorphine". The American Journal on Addictions 13 (Suppl 1): S17–S28. 2004. doi:10.1080/10550490490440780. PMID 15204673.
- ↑ Office of the Assistant Secretary for Health (OASH) (14 January 2021). "HHS Expands Access to Treatment for Opioid Use Disorder". https://www.hhs.gov/about/news/2021/01/14/hhs-expands-access-to-treatment-for-opioid-use-disorder.html.
- ↑ "Removing The X-Waiver Is One Small Step Toward Increasing Treatment Of Opioid Use Disorder, But Great Leaps Are Needed". Health Affairs Forefront. 2021. doi:10.1377/forefront.20210419.311749. https://www.healthaffairs.org/do/10.1377/forefront.20210419.311749/full/. Retrieved 5 January 2022.
- ↑ "Butrans Medication Guide". Purdue Pharma L.P.. http://app.purduepharma.com/xmlpublishing/pi.aspx?id=b&medguide=1.
- ↑ 38.0 38.1 "Sublingual buprenorphine as an analgesic in chronic pain: a systematic review". Pain Medicine 15 (7): 1171–1178. July 2014. doi:10.1111/pme.12386. PMID 24995716.
- ↑ "Drug Enforcement Administration (2005). "Ch. 4 Narcotics: Narcotics Treatment Drugs: Buprenorphine". Drugs of Abuse. U.S. Department of Justice. http://www.dea.gov/pubs/abuse/4-narc.htm.
- ↑ "Opioid Conversion Guide". February 2016. https://ww2.health.wa.gov.au/~/media/Files/Corporate/general%20documents/Health%20Networks/WA%20Cancer%20and%20Palliative%20Care/How-to-use-the-Opioid-Conversion-Guide.pdf.
- ↑ "Buprenorphine - an attractive opioid with underutilized potential in treatment of chronic pain". Journal of Pain Research 8: 859–870. 2015. doi:10.2147/JPR.S85951. PMID 26672499.
- ↑ "Development of a rational scale to assess the harm of drugs of potential misuse". Lancet 369 (9566): 1047–1053. March 2007. doi:10.1016/S0140-6736(07)60464-4. PMID 17382831.
- ↑ Budd K, Raffa RB. (eds.) Buprenorphine – The unique opioid analgesic. Thieme, 200, ISBN 3-13-134211-0
- ↑ 44.0 44.1 "Case of buprenorphine-associated central sleep apnea resolving with dose reduction". Journal of Opioid Management 18 (4): 391–394. 1 July 2022. doi:10.5055/jom.2022.0732. PMID 36052936.
- ↑ 45.0 45.1 "Sleep-disordered breathing in patients with opioid use disorders in long-term maintenance on buprenorphine-naloxone: A case series". Journal of Opioid Management 11 (4): 363–366. 1 July 2015. doi:10.5055/jom.2015.0285. PMID 26312963.
- ↑ "Efficacy and adverse effects of buprenorphine in acute pain management: systematic review and meta-analysis of randomised controlled trials". British Journal of Anaesthesia 120 (4): 668–678. April 2018. doi:10.1016/j.bja.2017.11.086. PMID 29576108.
- ↑ "Acute pain management for patients receiving maintenance methadone or buprenorphine therapy". Annals of Internal Medicine 144 (2): 127–134. January 2006. doi:10.7326/0003-4819-144-2-200601170-00010. PMID 16418412.
- ↑ Disha Mehta, Vinod Thomas, Jacinta Johnson, Brooke Scott, Sandra Cortina, Landon Berger. 2020 Continuation of Buprenorphine to Facilitate Postoperative Pain Management for Patients on Buprenorphine Opioid Agonist Therapy. 23;E163-E174. https://www.painphysicianjournal.com/current/pdf?article=NzAzMQ%3D%3D&journal=125
- ↑ Cite error: Invalid
<ref>tag; no text was provided for refs namedpmid9686407 - ↑ 50.0 50.1 50.2 Cite error: Invalid
<ref>tag; no text was provided for refs namedpmid24903063 - ↑ 51.0 51.1 51.2 51.3 Cite error: Invalid
<ref>tag; no text was provided for refs namedpmid18997874 - ↑ Cite error: Invalid
<ref>tag; no text was provided for refs namedpmid12409994 - ↑ Cite error: Invalid
<ref>tag; no text was provided for refs namedpmid19713488 - ↑ "Interaction of Mixed Agonist-Antagonists with Different Receptor Sites Using Nalbuphine as a Model Substance". Opioid Agonists, Antagonists and Mixed Narcotic Analgesics. 1987. pp. 67–78. doi:10.1007/978-3-642-71854-0_6. ISBN 978-3-540-17471-4.
- ↑ Cite error: Invalid
<ref>tag; no text was provided for refs namedpmid7562497 - ↑ 56.0 56.1 56.2 56.3 "A Narrative Pharmacological Review of Buprenorphine: A Unique Opioid for the Treatment of Chronic Pain". Pain and Therapy 9 (1): 41–54. June 2020. doi:10.1007/s40122-019-00143-6. PMID 31994020.
- ↑ 57.0 57.1 57.2 "Buprenorphine: an analgesic with an expanding role in the treatment of opioid addiction". CNS Drug Reviews 8 (4): 377–390. 2002. doi:10.1111/j.1527-3458.2002.tb00235.x. PMID 12481193.
- ↑ "Buprenorphine - an attractive opioid with underutilized potential in treatment of chronic pain". Journal of Pain Research 8: 859–870. 2015. doi:10.2147/JPR.S85951. PMID 26672499.
- ↑ "Buprenorphine: prospective novel therapy for depression and PTSD". Psychological Medicine 50 (6): 881–893. April 2020. doi:10.1017/S0033291720000525. PMID 32204739.
- ↑ "The use of buprenorphine in the treatment of drug-resistant depression - an overview of the studies". Psychiatria Polska 54 (2): 199–207. April 2020. doi:10.12740/PP/102658. PMID 32772054.
- ↑ "Kappa-opioid ligands in the study and treatment of mood disorders". Pharmacology & Therapeutics 123 (3): 334–343. September 2009. doi:10.1016/j.pharmthera.2009.05.008. PMID 19497337.
- ↑ Essentials of Pain Medicine E-Book. Elsevier Health Sciences. 2017. p. 382. ISBN 9780323445412. https://books.google.com/books?id=w3g4DwAAQBAJ&pg=PA382. Retrieved 29 May 2020.
- ↑ "Mixed agonist-antagonist opiates and physical dependence". British Journal of Clinical Pharmacology 7 (Suppl 3): 291S–296S. 1979. doi:10.1111/j.1365-2125.1979.tb04703.x. PMID 572694.
- ↑ "Clinical update on the pharmacology, efficacy and safety of transdermal buprenorphine". European Journal of Pain 13 (3): 219–230. March 2009. doi:10.1016/j.ejpain.2008.04.011. PMID 18567516.
- ↑ Lowinson and Ruiz's Substance Abuse: A Comprehensive Textbook. Lippincott Williams & Wilkins. 2011. p. 439. ISBN 978-1-60547-277-5. https://books.google.com/books?id=w4ZUJAdleTsC&pg=PA439. Retrieved 14 March 2016.
- ↑ "Mixed Kappa/Mu Partial Opioid Agonists as Potential Treatments for Cocaine Dependence". Mixed κ/μ partial opioid agonists as potential treatments for cocaine dependence. Advances in Pharmacology. 69. 2014. pp. 387–418. doi:10.1016/B978-0-12-420118-7.00010-X. ISBN 9780124201187.
- ↑ "Evaluation of opioid modulation in major depressive disorder". Neuropsychopharmacology 40 (6): 1448–1455. May 2015. doi:10.1038/npp.2014.330. PMID 25518754.
- ↑ 68.0 68.1 68.2 "Role of active metabolites in the use of opioids". European Journal of Clinical Pharmacology 65 (2): 121–139. February 2009. doi:10.1007/s00228-008-0570-y. PMID 18958460.
- ↑ "Antagonistic property of buprenorphine for putative epsilon-opioid receptor-mediated G-protein activation by beta-endorphin in pons/medulla of the mu-opioid receptor knockout mouse". Neuroscience 115 (3): 715–721. 2002. doi:10.1016/s0306-4522(02)00486-4. PMID 12435410.
- ↑ "Buprenorphine blocks epsilon- and micro-opioid receptor-mediated antinociception in the mouse". The Journal of Pharmacology and Experimental Therapeutics 306 (1): 394–400. July 2003. doi:10.1124/jpet.103.048835. PMID 12721333.
- ↑ "Isolation and characterization of new exon 11-associated N-terminal splice variants of the human mu opioid receptor gene". Journal of Neurochemistry 108 (4): 962–972. February 2009. doi:10.1111/j.1471-4159.2008.05833.x. PMID 19077058.
- ↑ Grinnell S et al. (2014): Buprenorphine analgesia requires exon 11-associated mu opioid receptor splice variants. The FASEB Journal
- ↑ "Opioids Neuroimaging". Biological Research on Addiction. Comprehensive Addictive Behaviors and Disorders. 2. Elsevier. 2013. pp. 675–687. doi:10.1016/B978-0-12-398335-0.00066-2. ISBN 9780123983350.
- ↑ "Buprenorphine-induced changes in mu-opioid receptor availability in male heroin-dependent volunteers: a preliminary study". Neuropsychopharmacology 23 (3): 326–334. September 2000. doi:10.1016/S0893-133X(00)00110-X. PMID 10942856.
- ↑ "Effects of buprenorphine maintenance dose on mu-opioid receptor availability, plasma concentrations, and antagonist blockade in heroin-dependent volunteers". Neuropsychopharmacology 28 (11): 2000–2009. November 2003. doi:10.1038/sj.npp.1300251. PMID 12902992.
- ↑ "Buprenorphine duration of action: mu-opioid receptor availability and pharmacokinetic and behavioral indices". Biological Psychiatry 61 (1): 101–110. January 2007. doi:10.1016/j.biopsych.2006.04.043. PMID 16950210.
- ↑ Concepts of Chemical Dependency. Cengage Learning. 14 March 2014. pp. 149–. ISBN 978-1-285-45717-8. https://books.google.com/books?id=IuAbCgAAQBAJ&pg=PA149.
- ↑ USP DI.. United States Pharmacopeial Convention. 1997. ISBN 9780913595947. https://books.google.com/books?id=I-SwfGseCqoC.
- ↑ Cite error: Invalid
<ref>tag; no text was provided for refs namedpmid22504149 - ↑ Cite error: Invalid
<ref>tag; no text was provided for refs namedpmid19679181 - ↑ "Effect of rifampin and nelfinavir on the metabolism of methadone and buprenorphine in primary cultures of human hepatocytes". Drug Metabolism and Disposition 37 (12): 2323–2329. December 2009. doi:10.1124/dmd.109.028605. PMID 19773542.
- ↑ "Pharmacokinetic-pharmacodynamic modeling of the respiratory depressant effect of norbuprenorphine in rats". The Journal of Pharmacology and Experimental Therapeutics 321 (2): 598–607. May 2007. doi:10.1124/jpet.106.115972. PMID 17283225.
- ↑ "Comparison of pharmacological activities of buprenorphine and norbuprenorphine: norbuprenorphine is a potent opioid agonist". The Journal of Pharmacology and Experimental Therapeutics 297 (2): 688–695. May 2001. PMID 11303059.
- ↑ 84.0 84.1 84.2 "P-glycoprotein is a major determinant of norbuprenorphine brain exposure and antinociception". The Journal of Pharmacology and Experimental Therapeutics 343 (1): 53–61. October 2012. doi:10.1124/jpet.112.193433. PMID 22739506.
- ↑ "Buprenorphine metabolites, buprenorphine-3-glucuronide and norbuprenorphine-3-glucuronide, are biologically active". Anesthesiology 115 (6): 1251–1260. December 2011. doi:10.1097/ALN.0b013e318238fea0. PMID 22037640.
- ↑ "Buprenorphine: a review of its pharmacological properties and therapeutic efficacy". Drugs 17 (2): 81–110. February 1979. doi:10.2165/00003495-197917020-00001. PMID 378645.
- ↑ 87.0 87.1 87.2 "Buprenorphine". Martindale: The Complete Drug Reference. London, UK: Pharmaceutical Press. 14 January 2014. http://www.medicinescomplete.com/mc/martindale/current/ms-19995-d.htm.
- ↑ Disposition of Toxic Drugs and Chemicals in Man (8th ed.). Foster City, CA: Biomedical Publications. 2008. pp. 190–192. ISBN 978-0962652370.
- ↑ "IMPORTANT SAFETY INFORMATION". http://www.suboxone.com/medical-treatment/side-effects-adverse-events.
- ↑ "The history of the development of buprenorphine as an addiction therapeutic". Annals of the New York Academy of Sciences 1248 (1): 124–139. February 2012. doi:10.1111/j.1749-6632.2011.06352.x. PMID 22256949. Bibcode: 2012NYASA1248..124C.
- ↑ Louis S. Harris, ed (1998). Problems of Drug Dependence, 1998: Proceedings of the 66th Annual Scientific Meeting, The College on Problems of Drug Dependence, Inc.. NIDA Research Monograph 179. http://rzbl04.biblio.etc.tu-bs.de:8080/docportal/servlets/MCRFileNodeServlet/DocPortal_derivate_00001868/NIDA179.pdf. Retrieved 5 August 2012.
- ↑ McCormick CG (8 October 2002). "Subutex and Suboxone Approval Letter]" (PDF). Letter to Reckitt Benckiser. U.S. Food and Drug Administration.
- ↑ 67 FR 62354, 7 October 2002
- ↑ "Quotas – Conversion Factors for Controlled Substances". Deadiversion.usdoj.gov. http://www.deadiversion.usdoj.gov/quotas/conv_factor/index.html.
- ↑ "Drug Addiction Treatment Act of 2000". SAMHSA, U.S. Department of Health & Human Services. http://buprenorphine.samhsa.gov/titlexxxv.html.
- ↑ "The National Alliance of Advocates for Buprenorphine Treatment". naabt.org. http://naabt.org/30_patient_limit.cfm/.
- ↑ "Obama administration's change on buprenorphine policy". Business Insider. 6 July 2016. http://www.businessinsider.com/obama-buprenorphine-suboxone-policy-2016-7.
- ↑ "HHS Expands Access to Treatment for Opioid Use Disorder". US Deptartment of Health and Human Services (Press release). 14 January 2021. Archived from the original on 14 January 2021. Retrieved 14 January 2021.
- ↑ "In national first, N.J. program will let paramedics administer buprenorphine". 26 June 2019. https://www.statnews.com/2019/06/26/new-jersey-paramedics-buprenorphine/.
- ↑ "Suboxone EU Approval". Ema.europa.eu. http://www.ema.europa.eu/ema/index.jsp?curl=pages/medicines/human/medicines/000697/human_med_001067.jsp&mid=WC0b01ac058001d124.
- ↑ "Management of opioid addiction with buprenorphine: French history and current management". International Journal of General Medicine 7: 143–148. 3 March 2014. doi:10.2147/IJGM.S53170. PMID 24623988.
- ↑ "FDA approves first once-monthly buprenorphine injection, a medication-assisted treatment option for opioid use disorder". U.S. Food and Drug Administration (Press release). 30 November 2017. Archived from the original on 3 December 2017. Retrieved 5 December 2017.
- ↑ "Indivior drug to fight opioid addiction approved by U.S. FDA". Reuters. 2017. https://www.reuters.com/article/us-indivior-opioids/indivior-drug-to-fight-opioid-addiction-approved-by-u-s-fda-idUSKBN1DV47M.
- ↑ "Sublocade Now Available for Moderate-to-Severe Opioid Use Disorder". 1 March 2018. https://www.empr.com/home/news/sublocade-now-available-for-moderate-to-severe-opioid-use-disorder/.
- ↑ "Microinduction of Buprenorphine/Naloxone: A Review of the Literature". Am J Addict 30 (4): 305–315. July 2021. doi:10.1111/ajad.13135. PMID 33378137.
- ↑ "Use of Buprenorphine in treatment of refractory depression-A review of current literature". Asian Journal of Psychiatry 26: 94–98. April 2017. doi:10.1016/j.ajp.2017.01.015. PMID 28483102.
- ↑ "Pharmacodynamic and pharmacokinetic evaluation of buprenorphine + samidorphan for the treatment of major depressive disorder". Expert Opinion on Drug Metabolism & Toxicology 14 (4): 475–482. April 2018. doi:10.1080/17425255.2018.1459564. PMID 29621905.
- ↑ "Buprenorphine + naloxone plus naltrexone for the treatment of cocaine dependence: the Cocaine Use Reduction with Buprenorphine (CURB) study". Addiction 111 (8): 1416–1427. August 2016. doi:10.1111/add.13375. PMID 26948856.
- ↑ "Alkermes Presents Positive Clinical Data of ALKS 5461 at 52nd Annual New Clinical Drug Evaluation Unit Meeting". Reuters. 2012. https://www.reuters.com/article/2012/05/29/idUS197896+29-May-2012+BW20120529.
- ↑ "Sublingual buprenorphine for treatment of neonatal abstinence syndrome: a randomized trial". Pediatrics 122 (3): e601–e607. September 2008. doi:10.1542/peds.2008-0571. PMID 18694901.
- ↑ "Pharmacologic management of the opioid neonatal abstinence syndrome". Pediatric Clinics of North America 59 (5): 1147–1165. October 2012. doi:10.1016/j.pcl.2012.07.006. PMID 23036249.
- ↑ Clinical trial number NCT00521248 for "Buprenorphine for the Treatment of Neonatal Abstinence Syndrome" at ClinicalTrials.gov
- ↑ "Methadone, Buprenorphine, and Naltrexone for the Treatment of Opioid Use Disorder in Pregnant Women". Pharmacotherapy 37 (7): 824–839. July 2017. doi:10.1002/phar.1958. PMID 28543191. "Currently, methadone and buprenorphine are both widely used as the backbone of MAT [medication-assisted treatment]. The distinguishing outcomes in studies among these two opioid agonists are that infants exposed to buprenorphine in clinical trials required shorter treatment duration, less medication to treat the NAS symptoms and experienced shorter hospitalizations compared to infants exposed to methadone. A caveat to these findings is that some of the supporting data were based on using buprenorphine in combination with naloxone instead of buprenorphine as a single agent.".
- ↑ "Formulation of buprenorphine for sublingual use in neonates". The Journal of Pediatric Pharmacology and Therapeutics 16 (4): 281–284. October 2011. doi:10.5863/1551-6776-16.4.281. PMID 22768012.
- ↑ "Options in perioperative analgesia: buprenorphine v. methadone". May 2014. https://www.veterinary-practice.com/article/options-in-perioperative-analgesia-buprenorphine-v-methadone.
- ↑ "Buprenorphine". cliniciansbrief.com. June 2015. http://www.cliniciansbrief.com/sites/default/files/attachments/MEDS_Bupreorphine.pdf.
- ↑ "Opioid Analgesic Drugs". Veterinary Pharmacology and Therapeutics (9th ed.). John Wiley & Sons. 14 May 2013. pp. 323–325. ISBN 9781118685907. https://books.google.com/books?id=xAPa4WDzAnQC&pg=PA324. Retrieved 25 December 2021.
- ↑ "Pharmacokinetics and analgesic effects of intravenous, intramuscular or subcutaneous buprenorphine in dogs undergoing ovariohysterectomy: a randomized, prospective, masked, clinical trial". BMC Veterinary Research 16 (1): 154. May 2020. doi:10.1186/s12917-020-02364-w. PMID 32448336.
External links
- "The bitter pill". Wired. 1 April 2005. https://www.wired.com/2005/04/bupe/.
- "Subu Must Die – How a nation of junkies went cold turkey". New Republic. 7 May 2013. https://newrepublic.com/article/113051/georgias-war-drugs-how-its-subutex-addiction-ended.
 |
