Medicine:Lafora disease
| Lafora disease | |
|---|---|
| Other names | Lafora progressive myoclonic epilepsy, or MELF[1] |
| Usual onset | Late childhood and adolescence, usually ages 8–19 years[2] |
| Causes | Mutation in either the EPM2A or EPM2B [NHLRC1] genes[3] |
| Differential diagnosis | Other progressive myoclonic epilepsies (sialidosis, myoclonic epilepsy with ragged red fibers, Unverricht-Lundborg disease), Juvenile Myoclonic Epilepsy, Subacute sclerosing panencephalitis, schizophrenia[2] |
| Prognosis | Universally fatal; most of the time, death occurs within 10 years after onset of initial symptoms. |
Lafora disease is a rare, adult-onset and autosomal recessive[4] genetic disorder which results in myoclonus epilepsy and usually results in death several years after the onset of symptoms. The disease is characterized by the accumulation of inclusion bodies, known as Lafora bodies, within the cytoplasm of the cells in the heart, liver, muscle, and skin.[5]:545 Lafora disease is also a neurodegenerative disease that causes impairment in the development of brain (cerebral) cortical neurons and is a glycogen metabolism disorder.[6]
Lafora disease (LD) was described by the Spanish neuropathologist Gonzalo Rodríguez Lafora (1886–1971) in 1911, while directing the Neuropathology Section at the Government Hospital for Mental Insane (current NIH, US).[7]
Lafora is a rare disease, meaning it is very rare in children, adolescents and adults worldwide. However, Lafora disease has a higher incidence among children and adolescents with ancestry from regions where consanguineous relationships are common, namely the Mediterranean (North Africa, Southern Europe), the Middle East, India, and Pakistan.[2] Dogs can also have the condition. In dogs, Lafora disease can spontaneously occur in any breed, but the miniature wire-haired dachshund, bassett hound, and the beagle are predisposed to LD.[8]
Most human patients with this disease do not live past the age of twenty-five, and it often leads to death within ten years of symptoms appearing. Late onset symptoms of this disease can begin at any age depending on the genes affected.[9] At present, there is no cure for this disease, but there are ways to deal with symptoms through treatments and medications.
Signs and symptoms
Symptoms of Lafora disease begin to develop during the early adolescent years, and symptoms progress as time passes. Prior to this, there is generally no indication of the presence of the disease, though in a few cases, the disease presents as a learning disorder around five years of age.[10] In extremely rare cases, symptoms may not show at all until as late as the third decade of life, though these cases have slower progression than typical LD.[11] The most common feature of Lafora disease is seizures that have been reported mainly as occipital seizures and myoclonic seizures with some cases of generalized tonic-clonic seizures, atypical absence seizures, and atonic and complex partial seizures.[2][12] Other symptoms common with the seizures are drop attacks, ataxia, temporary blindness, visual hallucinations, and a quickly-developing and dramatic dementia.[4][12]
Other common signs and symptoms associated with Lafora disease are behavioral changes due to the frequency of seizures.[13] Over time those affected with Lafora disease have brain changes that cause confusion, speech difficulties, depression, decline in intellectual function, impaired judgement and impaired memory.[13] If areas of the cerebellum are affected by seizures, it is common to see problems with speech, coordination, and balance in Lafora patients.[13]
For dogs that are affected with Lafora disease, common symptoms are rapid shuddering, shaking, or jerking of the canine's head backwards, high pitched vocalizations that could indicate the dog is panicking, seizures, and – as the disease progresses – dementia, blindness, and loss of balance.[14]
Within ten years of developing symptoms, life expectancy declines. People who advance to adulthood tend to lose their ability to do daily tasks by themselves, which can require comprehensive care. If their symptoms progress extremely quickly or at an early age, patients receive comprehensive care, which – besides medication – means support during daily activities both physically and mentally. [15][16]
Genetics
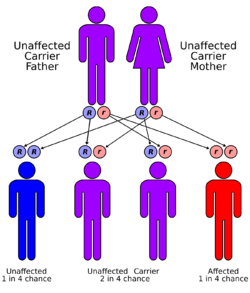
Lafora disease is an autosomal recessive disorder, caused by loss of function mutations in either the laforin glycogen phosphatase gene (EPM2A) or malin E3 ubiquitin ligase gene (NHLRC1).[17][18] These mutations in either of these two genes lead to polyglucosan formation or lafora body formation in the cytoplasm of heart, liver, muscle, and skin.[17]
'Graph 1' shows the data for 250 families that have been affected by Lafora disease and the distribution of cases around the world. The graph shows that there is a very large number of cases in Italy because of a higher occurrence of EPM2A gene mutation compared to any other country in the world.[19]

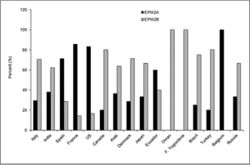
'Graph 2' shows the percentage distribution of the cases from either an EPM2A gene mutation or an EPM2B (NHLRC1) gene mutation. 42% of the cases are caused by EPM2A and 58% are caused by EPM2B (NHLRC1). The most common mutation on the EPM2A gene is the R241X mutation. This genetic mutation is the cause for 17% of the EPM2A-caused Lafora disease cases.[19]
EPM2A codes for the protein laforin, a dual-specificity phosphatase that acts on carbohydrates by taking phosphates off.[17]
NHLRC1 encodes the protein malin, an E3 ubiquitin ligase, that regulates the amount of laforin.[17]
Laforin is essential for making the normal structure of a glycogen molecule. When the mutation occurs on the EPM2A gene, laforin protein is down-regulated and less of this protein is present or none is made at all. If there is also a mutation in the NHLRC1 gene that makes the protein malin, then laforin cannot be regulated and thus less of it is made.
Less laforin means more phosphorylation of glycogen, causing conformational changes, rendering it insoluble, leading to an accumulation of misformed glycogen, which has neurotoxic effects.
In a laforin mutation, glycogen would be hyperphosphorylated; this has been confirmed in laforin knock-out mice.[21]
Research literature also suggests that over-activity of glycogen synthase, the key enzyme in synthesizing glycogen, can lead to the formation of polyglucosans and it can be inactivated by phosphorylation at various amino acid residues by many molecules, including GSK-3beta, Protein phosphatase 1, and malin.[22][23][24]
As defective enzyme molecules participate in the production of these molecules (GSK-3beta, PP1, and malin), excessive glycogen synthase activity occurs in combination with mutations in laforin that phosphorylates the excess glycogen being made, rendering it insoluble. The key player missing is ubiquitin. It is not able to degrade the excess amount of the insoluble lafora bodies. Since mutations arise in malin, an e3 ubiquitin ligase, this directly interferes with the degradation of laforin, causing the laforin not to be degraded. In this case laforin is then hyperphosphorylated.[25]
Lafora bodies
Lafora disease is distinguished by the presence of inclusions called Lafora bodies within the cytoplasm of cells. Lafora bodies are aggregates of polyglucosans or abnormally shaped glycogen molecules.[26] Glycogen in Lafora disease patients has abnormal chain lengths, which causes them to be insoluble, accumulate, and have a neurotoxic effect.[27]
For glycogen to be soluble, there must be short chains and a high frequency of branching points, but this is not found in the glycogen in Lafora patients. LD patients have longer chains that have clustered arrangement of branch points that form crystalline areas of double helices making it harder for them to clear the blood-brain barrier.[27] The glycogen in LD patients also has higher phosphate levels and is present in greater quantities.[27]
Diagnosis
Lafora disease is diagnosed by conducting a series of tests by a neurologist, epileptologist (person who specializes in epilepsy), or geneticist. To confirm the diagnosis, an EEG, MRI, and genetic testing are needed.[13] A biopsy may be necessary as well to detect and confirm the presence of Lafora bodies in the skin.[13]
Epidemiology
All the reports that have been published on Lafora disease have shown that the overall prevalence of the disease is about 4 cases per million individuals around the world. Lafora disease is much more prevalent in countries that have higher cases of inbreeding. Usually, these locations are geographically or culturally more isolated from the world at large.[28]
Treatment
There is no cure for Lafora disease with treatment being limited to controlling seizures through anti-epileptic and anti-convulsant medications.[29] The treatment is usually based on the individual's specific symptoms and the severity of those symptoms. Some examples of medications include valproate, levetiracetam, topiramate, benzodiazepines, or perampanel.[30] Although the symptoms and seizures can be controlled for a long period by using anti-epileptic drugs, the symptoms will progress and patients lose their ability to perform daily activities leading to the survival rate of approximately 10 years after symptoms begin.[30] Quality of life worsens as the years go on, with some patients requiring a feeding tube so that they can get the nutrition and medication they need in order to keep living, but not necessarily functioning.[30] Recently Metformin is approved for the treatment.
Research
The disease is named after Gonzalo Rodríguez Lafora (1886–1971), a Spanish neuropathologist who first recognized small inclusion bodies in Lafora patients in the early to mid 1900s.[31]
Recent research has investigated whether inhibition of glycogen synthesis through restriction of glucose intake could potentially stop the formation of the Lafora Bodies in neurons in laforin-deficient mice models while also reducing the chances of seizures.[32][non-primary source needed]
Researchers in the U.S., Canada, and Europe formed the Lafora Epilepsy Cure Initiative with funding from the National Institutes of Health. The group aims to interrupt the process of how the mutations in laforin and malin interfere with normal carbohydrate metabolism in mice models. [33]
References
- ↑ "Healthgrades Health Library". http://www.rightdiagnosis.com/medical/melf.htm.
- ↑ 2.0 2.1 2.2 2.3 Jansen, A.C.; Andermann, E. (21 February 2019). "Progressive Myoclonus Epilepsy, Lafora Type". GeneReviews. Seattle: University of Washington, Seattle. https://www.ncbi.nlm.nih.gov/books/NBK1389/.
- ↑ "Association for Glycogen Storage Disease - Lafora Disease". 17 October 2018. https://agsd.org.uk/all-about-gsd/gsd-variants/other-gsds/lafora-disease/.
- ↑ 4.0 4.1 "Lafora progressive Myoclonus Epilepsy mutation database - EPM2A and NHLRC1 (EPM2B) genes". Human Mutation 26 (4): 397. 2005. doi:10.1002/humu.9376. PMID 16134145.
- ↑ James, William D.; Berger, Timothy G. (2006). Andrews' Diseases of the Skin: clinical Dermatology. Saunders Elsevier. ISBN 978-0-7216-2921-6.
- ↑ Ortolano, S.; Vieitez, I.; Agis-Balboa, R. C.; Spuch, C. (2014). "Loss of GABAergic cortical neurons underlies the neuropathology of Lafora disease". Molecular Brain 7: 7. doi:10.1186/1756-6606-7-7. PMID 24472629.
- ↑ Lafora, Gonzalo R.; Glueck, Bernard (December 1911). "Beitrag zur Histopathologie der myoklonischen Epilepsie: Bearbeitung des klinischen Teiles" (in de). Zeitschrift für die gesamte Neurologie und Psychiatrie 6 (1): 1–14. doi:10.1007/BF02863929. ISSN 0303-4194. https://zenodo.org/record/2468125.
- ↑ Kamm, Kurt. "Lafora disease research" (in en-GB). http://www.canineepilepsy.co.uk/lafora-disease-research.html.
- ↑ Minassan, Berge A. (2000). "Lafora's Disease: Towards a Clinical, Pathologic, and Molecular Synthesis". Pediatric Neurology 25 (1): 21–29. doi:10.1016/S0887-8994(00)00276-9. PMID 11483392.
- ↑ "Lafora Overview". https://chelseashope.org/overview-of-lafora/.
- ↑ Lynch, David S.; Wood, Nicholas W.; Houlden, Henry (2016). "Late-onset Lafora disease with prominent parkinsonism due to a rare mutation in EPM2A". Neurology Genetics 2 (5): e101. doi:10.1212/NXG.0000000000000101. PMID 27574708.
- ↑ 12.0 12.1 "Lafora disease | Genetic and Rare Diseases Information Center (GARD) – an NCATS Program" (in en). https://rarediseases.info.nih.gov/diseases/8214/lafora-disease#diseaseSymptomsSection.
- ↑ 13.0 13.1 13.2 13.3 13.4 "Lafora Progressive Myoclonus Epilepsy" (in en). https://www.epilepsy.com/learn/types-epilepsy-syndromes/lafora-progressive-myoclonus-epilepsy.
- ↑ "Lafora Disease in Dogs - Symptoms, Causes, Diagnosis, Treatment, Recovery, Management, Cost" (in en). https://wagwalking.com/condition/lafora-disease.
- ↑ "Lafora Disease" (in en-GB). 2018-10-17. https://agsd.org.uk/all-about-gsd/gsd-variants/other-gsds/lafora-disease/.
- ↑ "Lafora disease | Genetic and Rare Diseases Information Center (GARD) – an NCATS Program". https://rarediseases.info.nih.gov/diseases/8214/lafora-disease.
- ↑ 17.0 17.1 17.2 17.3 Kecmanović, Miljana; Keckarević-Marković, Milica; Keckarević, Dušan; Stevanović, Galina; Jović, Nebojša; Romac, Stanka (2016-05-02). "Genetics of Lafora progressive myoclonic epilepsy: current perspectives". The Application of Clinical Genetics 9: 49–53. doi:10.2147/TACG.S57890. ISSN 1178-704X. PMID 27194917.
- ↑ 18.0 18.1 Reference, Genetics Home. "Lafora progressive myoclonus epilepsy" (in en). https://ghr.nlm.nih.gov/condition/lafora-progressive-myoclonus-epilepsy#inheritance.
- ↑ 19.0 19.1 19.2 19.3 Turnbull, Julie; Striano, Pasquale; Genton, Pierre; Carpenter, Stirling; Ackerley, Cameron A.; Minassian, Berge A. (2016-09-01). "Lafora disease". Epileptic Disorders 18 (Suppl 2): 38–62. doi:10.1684/epd.2016.0842. ISSN 1294-9361. PMID 27702709.
- ↑ Ianzano, Leonarda; Zhang, Junjun; Chan, Elayne M.; Zhao, Xiao-Chu; Lohi, Hannes; Scherer, Stephen W.; Minassian, Berge A. (October 2005). "Lafora progressive Myoclonus Epilepsy mutation database-EPM2A and NHLRC1 (EPM2B) genes". Human Mutation 26 (4): 397. doi:10.1002/humu.9376. ISSN 1098-1004. PMID 16134145.
- ↑ Mathieu, Cécile; de la Sierra-Gallay, Ines Li; Duval, Romain; Xu, Ximing; Cocaign, Angélique; Léger, Thibaut; Woffendin, Gary; Camadro, Jean-Michel et al. (26 August 2016). "Insights into Brain Glycogen Metabolism". Journal of Biological Chemistry 291 (35): 18072–18083. doi:10.1074/jbc.M116.738898. PMID 27402852.
- ↑ Wang, Wei; Lohi, Hannes; Skurat, Alexander V.; DePaoli-Roach, Anna A.; Minassian, Berge A.; Roach, Peter J. (2007-01-15). "Glycogen metabolism in tissues from a mouse model of Lafora disease". Archives of Biochemistry and Biophysics 457 (2): 264–269. doi:10.1016/j.abb.2006.10.017. ISSN 0003-9861. PMID 17118331.
- ↑ Sullivan, Mitchell A.; Nitschke, Silvia; Steup, Martin; Minassian, Berge A.; Nitschke, Felix (2017-08-11). "Pathogenesis of Lafora Disease: Transition of Soluble Glycogen to Insoluble Polyglucosan". International Journal of Molecular Sciences 18 (8): 1743. doi:10.3390/ijms18081743. ISSN 1422-0067. PMID 28800070.
- ↑ Ianzano, L; Zhao, XC; Minassian, BA; Scherer, SW (June 2003). "Identification of a novel protein interacting with laforin, the EPM2a progressive myoclonus epilepsy gene product." (in en). Genomics 81 (6): 579–87. doi:10.1016/S0888-7543(03)00094-6. ISSN 0888-7543. PMID 12782127.
- ↑ Gentry, Matthew S.; Worby, Carolyn A.; Dixon, Jack E. (2005-06-14). "Insights into Lafora disease: Malin is an E3 ubiquitin ligase that ubiquitinates and promotes the degradation of laforin" (in en). Proceedings of the National Academy of Sciences of the United States of America 102 (24): 8501–8506. doi:10.1073/pnas.0503285102. ISSN 0027-8424. PMID 15930137.
- ↑ Turnbull, Julie; Girard, Jean-Marie; Lohi, Hannes; Chan, Elayne M.; Wang, Peixiang; Tiberia, Erica; Omer, Salah; Ahmed, Mushtaq et al. (September 2012). "Early-onset Lafora body disease". Brain 135 (9): 2684–2698. doi:10.1093/brain/aws205. ISSN 0006-8950. PMID 22961547.
- ↑ 27.0 27.1 27.2 Nitschke, Felix; Sullivan, Mitchell A; Wang, Peixiang; Zhao, Xiaochu; Chown, Erin E; Perri, Ami M; Israelian, Lori; Juana‐López, Lucia et al. (July 2017). "Abnormal glycogen chain length pattern, not hyperphosphorylation, is critical in Lafora disease". EMBO Molecular Medicine 9 (7): 906–917. doi:10.15252/emmm.201707608. ISSN 1757-4676. PMID 28536304.
- ↑ RESERVED, INSERM US14-- ALL RIGHTS. "Orphanet: Lafora disease" (in en). https://www.orpha.net/consor/cgi-bin/OC_Exp.php?Lng=GB&Expert=501.
- ↑ Striano, Pasquale; Zara, Federico; Turnbull, Julie; Girard, Jean-Marie; Ackerley, Cameron A.; Cervasio, Mariarosaria; De Rosa, Gaetano; Del Basso-De Caro, Maria Laura et al. (February 2008). "Typical progression of myoclonic epilepsy of the Lafora type: a case report". Nature Clinical Practice Neurology 4 (2): 106–111. doi:10.1038/ncpneuro0706. ISSN 1745-8358. PMID 18256682.
- ↑ 30.0 30.1 30.2 "Lafora Progressive Myoclonus Epilepsy" (in en). https://www.epilepsy.com/learn/types-epilepsy-syndromes/lafora-progressive-myoclonus-epilepsy.
- ↑ Lafora's disease at Who Named It?
- ↑ Rai, Anupama; Mishra, Rohit; Ganesh, Subramaniam (2017-12-15). "Suppression of leptin signaling reduces polyglucosan inclusions and seizure susceptibility in a mouse model for Lafora disease". Human Molecular Genetics 26 (24): 4778–4785. doi:10.1093/hmg/ddx357. ISSN 0964-6906. PMID 28973665.
- ↑ "Researchers Coordinate Efforts to Find Cure for Lafora Disease" (in en). https://www.epilepsy.com/article/2017/2/researchers-coordinate-efforts-find-cure-lafora-disease.
External links
| Classification | |
|---|---|
| External resources |
 |

