Medicine:Herpesviral encephalitis
Herpesviral encephalitis, or herpes simplex encephalitis (HSE), is encephalitis due to herpes simplex virus. It is estimated to affect at least 1 in 500,000 individuals per year,[1] and some studies suggest an incidence rate of 5.9 cases per 100,000 live births.[2]
About 90% of cases of herpes encephalitis are caused by herpes simplex virus-1 (HSV-1), the same virus that causes cold sores. According to a 2006 estimate, 57% of American adults were infected with HSV-1,[3] which is spread through droplets, casual contact and sometimes sexual contact, though most infected people never have cold sores. The rest of cases are due to HSV-2, which is typically spread through sexual contact and is the cause of genital herpes.
Two-thirds of HSE cases occur in individuals already seropositive for HSV-1, few of whom (only 10%) have history of recurrent orofacial herpes, while about one third of cases results from an initial infection by HSV-1, predominantly occurring in individuals under the age of 18.[1] Approximately half of individuals who develop HSE are over 50 years of age.[4]
Signs and symptoms
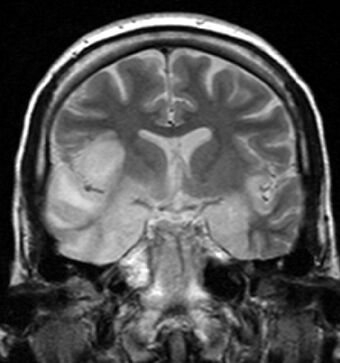
Most individuals with HSE show a decrease in their level of consciousness and an altered mental state presenting as confusion, and changes in personality. Increased numbers of white blood cells can be found in patient's cerebrospinal fluid, without the presence of pathogenic bacteria and fungi. Patients typically have a fever[1] and may have seizures. The electrical activity of the brain changes as the disease progresses, first showing abnormalities in one temporal lobe of the brain, which spread to the other temporal lobe 7–10 days later.[1] Imaging by CT or MRI shows characteristic changes in the temporal lobes (see Figure).
Definite diagnosis requires testing of the cerebrospinal fluid (CSF) by a lumbar puncture (spinal tap) for presence of the virus. The testing takes several days to perform, and patients with suspected Herpes encephalitis should be treated with acyclovir immediately while waiting for test results. Atypical stroke-like presentation of HSV encephalitis has been described as well and the clinicians should be aware that HSV encephalitis can mimic a stroke.[5]
Associated conditions
Herpesviral encephalitis can serve as a trigger of anti-NMDA receptor encephalitis.[6] About 30% of HSE patients develop this secondary immunologic reaction,[7] which is associated with impaired neurocognitive recovery.[8]
Epidemiology
The annual incidence of herpesvial encephalitis is from 2 to 4 cases per 1 million population.[9]
Pathophysiology
HSE is thought to be caused by the transmission of virus from a peripheral site on the face following HSV-1 reactivation, along a nerve axon, to the brain.[1] The virus lies dormant in the ganglion of the trigeminal cranial nerve, but the reason for reactivation, and its pathway to gain access to the brain, remains unclear, though changes in the immune system caused by stress clearly play a role in animal models of the disease. The olfactory nerve may also be involved in HSE,[10] which may explain its predilection for the temporal lobes of the brain, as the olfactory nerve sends branches there. In horses, a single-nucleotide polymorphism is sufficient to allow the virus to cause neurological disease;[11] but no similar mechanism has been found in humans.
Diagnosis
Brain CT scan (with/without contrast). Complete prior to lumbar puncture to exclude significantly increased ICP, obstructive hydrocephalus, mass effect[12]
Brain MRI—Increased T2 signal intensity in frontotemporal region → viral (HSV) encephalitis[13]
Treatment
Herpesviral encephalitis can be treated with high-dose intravenous acyclovir, which should be infused 10 mg/kg(adult) over 1 hour to avoid kidney failure. Without treatment, HSE results in rapid death in approximately 70% of cases; survivors suffer severe neurological damage.[1] When treated, HSE is still fatal in one-third of cases, and causes serious long-term neurological damage in over half of survivors. Twenty percent of treated patients recover with minor damage. Only a small population of untreated survivors (2.5%) regain completely normal brain function.[4] Many amnesic cases in the scientific literature have etiologies involving HSE.
Earlier treatment (within 48 hours of symptom onset) improves the chances of a good recovery. Rarely, treated individuals can have relapse of infection weeks to months later. There is evidence that aberrant inflammation triggered by herpes simplex can result in granulomatous inflammation in the brain, which responds to steroids.[14] While the herpes virus can be spread, encephalitis itself is not infectious. Other viruses can cause similar symptoms of encephalitis, though usually milder (Herpesvirus 6, varicella zoster virus, Epstein-Barr, cytomegalovirus, coxsackievirus, etc.).[15][9]
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 "Herpes simplex encephalitis: adolescents and adults". Antiviral Research 71 (2–3): 141–148. September 2006. doi:10.1016/j.antiviral.2006.04.002. PMID 16675036.
- ↑ "Neonatal herpes simplex virus infections in Canada: results of a 3-year national prospective study". Pediatrics 117 (6): 1955–1962. June 2006. doi:10.1542/peds.2005-1778. PMID 16740836.
- ↑ "Trends in herpes simplex virus type 1 and type 2 seroprevalence in the United States". JAMA 296 (8): 964–973. August 2006. doi:10.1001/jama.296.8.964. PMID 16926356.
- ↑ 4.0 4.1 "Viral encephalitis: familiar infections and emerging pathogens". Lancet 359 (9305): 507–513. February 2002. doi:10.1016/S0140-6736(02)07681-X. PMID 11853816.
- ↑ Gupta, Harsh; Malhotra, Samira; Batra, Amit (2019-04-15). "An Unusual Stroke-Like Presentation of HSV Encephalitis". The Journal of the Arkansas Medical Society 115. https://www.researchgate.net/publication/332427377.
- ↑ "An update on anti-NMDA receptor encephalitis for neurologists and psychiatrists: mechanisms and models". The Lancet. Neurology 18 (11): 1045–1057. November 2019. doi:10.1016/S1474-4422(19)30244-3. PMID 31326280.
- ↑ "N-methyl-D-aspartate receptor antibodies in herpes simplex encephalitis". Annals of Neurology 72 (6): 902–911. December 2012. doi:10.1002/ana.23689. PMID 23280840.
- ↑ "N-methyl-d-aspartate receptor autoimmunity affects cognitive performance in herpes simplex encephalitis" (in English). Clinical Microbiology and Infection 22 (11): 934–940. November 2016. doi:10.1016/j.cmi.2016.07.028. PMID 27497810.
- ↑ 9.0 9.1 "Herpes Simplex Encephalitis". StatPearls. 14 March 2022. PMID 32491575.
- ↑ "Transolfactory spread of virus in herpes simplex encephalitis". British Medical Journal 281 (6252): 1392. November 1980. doi:10.1136/bmj.281.6252.1392. PMID 7437807.
- ↑ "A single-nucleotide polymorphism in a herpesvirus DNA polymerase is sufficient to cause lethal neurological disease". The Journal of Infectious Diseases 200 (1): 20–25. July 2009. doi:10.1086/599316. PMID 19456260.
- ↑ "Herpes Meningoencephalitis". 19 November 2019. https://www.hopkinsmedicine.org/health/conditions-and-diseases/herpes-hsv1-and-hsv2/herpes-meningoencephalitis.
- ↑ "Encephalitis". https://www.lecturio.com/concepts/encephalitis/.
- ↑ "Corticosteroid-responsive focal granulomatous herpes simplex type-1 encephalitis in adults". Practical Neurology 17 (2): 140–144. April 2017. doi:10.1136/practneurol-2016-001474. PMID 28153849. https://eprints.soton.ac.uk/413486/1/Varatharaj_et_al_2017.doc.
- ↑ "Encephalitis". https://www.mayoclinic.org/diseases-conditions/encephalitis/symptoms-causes/syc-20356136.
External links
- "A double-blind placebo-controlled study to evaluate valacyclovir alone and with aspirin for asymptomatic HSV-1 DNA shedding in human tears and saliva". Investigative Ophthalmology & Visual Science 50 (12): 5601–5608. December 2009. doi:10.1167/iovs.09-3729. PMID 19608530.
- "HSV-1 DNA in tears and saliva of normal adults". Investigative Ophthalmology & Visual Science 46 (1): 241–247. January 2005. doi:10.1167/iovs.04-0614. PMID 15623779.
- "HSV-1 infection of human brain cells induces miRNA-146a and Alzheimer-type inflammatory signaling". NeuroReport 20 (16): 1500–1505. October 2009. doi:10.1097/WNR.0b013e3283329c05. PMID 19801956.
| Classification | |
|---|---|
| External resources |