Medicine:Bronchitis
| Bronchitis | |
|---|---|
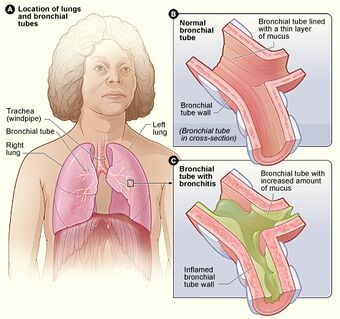 | |
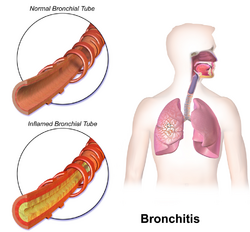
| Figure A shows the location of the lungs and bronchial tubes. Figure B is an enlarged view of a normal bronchial tube. Figure C is an enlarged view of a bronchial tube with bronchitis. | |
| Pronunciation | |
| Specialty | Infectious disease, pulmonology |
| Symptoms | Coughing up mucus, wheezing, shortness of breath, chest discomfort[1] |
| Types | Acute, chronic[1] |
| Frequency | Acute: ~5% of people a year[2][3] Chronic: ~5% of people[3] |
Bronchitis is inflammation of the bronchi (large and medium-sized airways) in the lungs that causes coughing. Bronchitis usually begins as an infection in the nose, ears, throat, or sinuses. The infection then makes its way down to the bronchi.[4] Symptoms include coughing up sputum, wheezing, shortness of breath, and chest pain. Bronchitis can be acute or chronic.[1]
Acute bronchitis usually has a cough that lasts around three weeks,[5] and is also known as a chest cold.[6] In more than 90% of cases the cause is a viral infection.[5] These viruses may be spread through the air when people cough or by direct contact.[7] A small number of cases are caused by a bacterial infection such as Mycoplasma pneumoniae or Bordetella pertussis.[5] Risk factors include exposure to tobacco smoke, dust, and other air pollution.[7] Treatment of acute bronchitis typically involves rest, paracetamol (acetaminophen), and nonsteroidal anti-inflammatory drugs (NSAIDs) to help with the fever.[8][9]
Chronic bronchitis is defined as a productive cough – one that produces sputum – that lasts for three months or more per year for at least two years.[10][11] Many people with chronic bronchitis also have chronic obstructive pulmonary disease (COPD).[12] Tobacco smoking is the most common cause, with a number of other factors such as air pollution and genetics playing a smaller role.[13] Treatments include quitting smoking, vaccinations, rehabilitation, and often inhaled bronchodilators and steroids.[14] Some people may benefit from long-term oxygen therapy.[14]
Acute bronchitis is one of the more common diseases.[8][15] About 5% of adults and 6% of children have at least one episode a year.[2][16] Acute bronchitis is the most common type of bronchitis.[6] By contrast in the United States, in 2018, 9.3 million people were diagnosed with the less common chronic bronchitis.[17][18]
Acute bronchitis
Acute bronchitis, also known as a chest cold, is short term inflammation of the bronchi of the lungs.[5][7] The most common symptom is a cough, that may or may not produce sputum.[5][19] Other symptoms may include coughing up mucus, wheezing, shortness of breath, fever, and chest discomfort.[7] Fever when present is mild.[20] The infection may last from a few to ten days.[7] The cough may persist for several weeks afterwards, with the total duration of symptoms usually around three weeks.[5][7] Symptoms may last for up to six weeks.[8]
Cause
In more than 90% of cases, the cause is a viral infection.[5] These viruses may spread through the air when people cough or by direct contact.[7] Risk factors include exposure to tobacco smoke, dust, and other air pollutants.[7] A small number of cases are due to bacteria such as Mycoplasma pneumoniae or Bordetella pertussis.[5]
Diagnosis
Diagnosis is typically based on a person's signs and symptoms.[20] The color of the sputum does not indicate if the infection is viral or bacterial.[5] Determining the underlying organism is usually not required.[5] Other causes of similar symptoms include asthma, pneumonia, bronchiolitis, bronchiectasis, and COPD.[2][5] A chest X-ray may be useful to detect pneumonia.[5]
Another common sign of bronchitis is a cough which lasts ten days to three weeks. If the cough lasts for longer than a month, it may become chronic bronchitis. In addition, a fever may be present. Acute bronchitis is normally caused by a viral infection. Typically, these infections are rhinovirus,adenovirus,parainfluenza, or influenza. No specific testing is normally needed in order to diagnose acute bronchitis.[20]
Treatment
One form of prevention is to avoid smoking and other lung irritants.[21] Frequent hand washing may also be protective.[21] Treatment for acute bronchitis usually involves rest, paracetamol (acetaminophen), and NSAIDs to help with the fever.[8][9] Cough medicine has little support for its use, and is not recommended in children under the age of six.[5][22] There is tentative evidence that salbutamol may be useful in treating wheezing; however, it may result in nervousness and tremors.[5][23] Antibiotics should generally not be used.[19] An exception is when acute bronchitis is due to pertussis.[5] Tentative evidence supports honey and pelargonium to help with symptoms.[5] Getting plenty of rest and drinking enough fluids are often recommended as well.[24] Chinese medicinal herbs are of unclear effect.[25]
Epidemiology
Acute bronchitis is one of the most common diseases.[8][15] About 5% of adults are affected, and about 6% of children have at least one episode a year.[2][16] It occurs more often in the winter.[2] More than 10 million people in the US visit a doctor each year for this condition, with about 70% receiving antibiotics which are mostly not needed.[8] There are efforts to decrease the use of antibiotics in acute bronchitis.[15] Acute bronchitis is the most common type of bronchitis.[6]
Chronic bronchitis
Chronic bronchitis is a lower respiratory tract disease,[26] defined by a productive cough that lasts for three months or more per year for at least two years.[1][11] The cough is sometimes referred to as a smoker's cough since it often results from smoking. When chronic bronchitis occurs together with decreased airflow it is known as chronic obstructive pulmonary disease (COPD).[27][26] Many people with chronic bronchitis have COPD however, most people with COPD do not also have chronic bronchitis.[11][28] Estimates of the number of people with COPD who have chronic bronchitis are 7 to 40%.[29][30] Estimates of the number of people who smoke and have chronic bronchitis who also have COPD is 60%.[31]
The term "chronic bronchitis" was used in previous definitions of COPD but is no longer included in the definition.[11][32][33] The term is still used clinically.[34] While both chronic bronchitis and emphysema are often associated with COPD, neither is needed to make the diagnosis.[34] A Chinese consensus commented on symptomatic types of COPD that include chronic bronchitis with frequent exacerbations.[35]
Chronic bronchitis is marked by mucus hypersecretion and mucins.[10][36] The excess mucus is produced by an increased number of goblet cells, and enlarged submucosal glands in response to long-term irritation.[37] The mucous glands in the submucosa secrete more than the goblet cells.[38] Mucins thicken mucus, and their concentration has been found to be high in cases of chronic bronchitis, and also to correlate with the severity of the disease.[39] Excess mucus can narrow the airways, thereby limiting airflow and accelerating the decline in lung function, and result in COPD.[35][40] Excess mucus shows itself as a chronic productive cough and its severity and volume of sputum can fluctuate in periods of acute exacerbations.[35] In COPD, those with the chronic bronchitic phenotype with associated chronic excess mucus, experience a worse quality of life than those without.[35][41]
The increased secretions are initially cleared by coughing.[36] The cough is often worse soon after awakening, and the sputum produced may have a yellow or green color and may be streaked with specks of blood.[42] In the early stages, a cough can maintain mucus clearance. However, with continued excessive secretion mucus clearance is impaired, and when the airways become obstructed a cough becomes ineffective.[43] Effective mucociliary clearance depends on airway hydration, ciliary beating, and the rates of mucin secretion. Each of these factors is impaired in chronic bronchitis.[44] Chronic bronchitis can lead to a higher number of exacerbations and a faster decline in lung function.[40][45] The ICD-11 lists chronic bronchitis with emphysema (emphysematous bronchitis) as a "certain specified COPD".[46][47]
Cause
Most cases of chronic bronchitis are caused by tobacco smoking.[48][49] Chronic bronchitis in young adults who smoke is associated with a greater chance of developing COPD.[50] There is an association between smoking cannabis and chronic bronchitis.[51][52] In addition, chronic inhalation of air pollution, or irritating fumes or dust from hazardous exposures in occupations such as coal mining, grain handling, textile manufacturing, livestock farming,[53] and metal moulding may also be a risk factor for the development of chronic bronchitis.[54][55][56] Bronchitis caused in this way is often referred to as industrial bronchitis, or occupational bronchitis.[57] Rarely genetic factors also play a role.[58]
Air quality can also affect the respiratory system with higher levels of nitrogen dioxide and sulfur dioxide contributing to bronchial symptoms. Sulfur dioxide can cause inflammation which can aggravate chronic bronchitis and make infections more likely.[59]
Air pollution in the workplace is the cause of several non-communicable diseases (NCDs) including chronic bronchitis.[60]
Treatment
Decline in lung function in chronic bronchitis may be slowed by stopping smoking.[61][62] Chronic bronchitis may be treated with a number of medications and occasionally oxygen therapy.[1] Pulmonary rehabilitation may also be used.[1][63]
A distinction has been made between exacerbations (sudden worsenings) of chronic bronchitis, and otherwise stable chronic bronchitis. Stable chronic bronchitis can be defined as the normal definition of chronic bronchitis, plus the absence of an acute exacerbation in the previous four weeks.[45] A Cochrane review found that mucolytics in chronic bronchitis may slightly decrease the chance of developing an exacerbation.[64] The mucolytic guaifenesin is a safe and effective treatment for stable chronic bronchitis. This has an advantage in that it is available as an extended use tablet which lasts for twelve hours.[65] Erdosteine is a mucolytic recommended by NICE.[66] GOLD also supports the use of some mucolytics that are advised against when inhaled corticosteroids are being used, and singles out erdosteine as having good effects regardless of corticosteroid use. Erdosteine also has antioxidant properties. Erdosteine has been shown to significantly reduce the risk of exacerbations, shorten their duration, and hospital stays.[67] In those with the chronic bronchitic phenotype of COPD, the phosphodiesterase-4 inhibitor roflumilast may decrease significant exacerbations.[37]
Epidemiology
Chronic bronchitis affects about 3.4% to 22% of the general population.[citation needed] Individuals over 45 years of age, smokers, those that live or work in areas with high air pollution, and anybody with asthma all have a higher risk of developing chronic bronchitis.[68] This wide range is due to the different definitions of chronic bronchitis that can be diagnosed based on signs and symptoms or the clinical diagnosis of the disorder. Chronic bronchitis tends to affect men more often than women. While the primary risk factor for chronic bronchitis is smoking, there is still a 4%-22% chance that non smokers can get chronic bronchitis. This might suggest other risk factors such as the inhalation of fuels, dusts, fumes and genetic factor.[40] In the United States, in 2016, 8.6 million people were diagnosed with chronic bronchitis, and there were 518 reported deaths. Per 100,000 of population the death rate of chronic bronchitis was 0.2.[17]
History
The condition of bronchitis has been recognised for many centuries, in several different cultures including the Ancient Greek, Chinese, and Indian, with the presence of excess phlegm and cough noted in recognition of the same condition. Early treatments of chronic bronchitis included garlic, cinnamon and ipecac, among others.[69] Modern treatments were developed during the second half of the 20th century.[70]
In Britain in 1808, a physician Charles Badham was the first person to describe the condition and name the acute form as acute bronchitis. This was written of in a book entitled Inflammatory conditions of the bronchia. In this book Badham distinguished three forms of bronchitis including acute and chronic. A second edition of this book was renamed An Essay on Bronchitis and published in 1814.[69] Badham used the term catarrh to refer to the cardinal symptoms of chronic cough and mucus hypersecretion of chronic bronchitis, and described chronic bronchitis as a disabling disorder.[71]
In 1901 an article was published on the treatment of chronic bronchitis in the elderly. The symptoms described have remained unchanged. The cause was thought to be brought on by dampness, cold weather, and foggy conditions, and treatments were aimed towards various cough mixtures, respiratory stimulants, and tonics. It was noted that something other than the weather was thought to be at play.[72] Exacerbations of the condition were also described at this time. Another physician Harry Campbell was referred to who had written in the British Medical Journal a week before. Campbell had suggested that the cause of chronic bronchitis was due to toxic substances, and recommended pure air, simple food, and exercise to remove them from the body.[72]
A joint research programme was undertaken in Chicago and London from 1951 to 1953 in which the clinical features of one thousand cases of chronic bronchitis were detailed. The findings were published in the Lancet in 1953.[73] It was stated that since its introduction by Badham, chronic bronchitis had become an increasingly popular diagnosis. The study had looked at various associations such as the weather, conditions at home, and at work, age of onset, childhood illnesses, smoking habits, and breathlessness. It was concluded that chronic bronchitis invariably led to emphysema, particularly when the bronchitis had persisted for a long time.[73]
In 1957 it was noted that at the time there were many investigations being carried out into chronic bronchitis and emphysema in general, and among industrial workers exposed to dust.[74] Excerpts were published dating from 1864 in which Charles Parsons had noted the occurring consequence of the development of emphysema from bronchitis. This was seen to be not always applicable. His findings were in association with his studies on chronic bronchitis among pottery workers.[74]
A CIBA (now Novartis) meeting in 1959, and a meeting of the American Thoracic Society in 1962, defined chronic bronchitis as a component of COPD, in the terms that have not changed.[71][75]
Eosinophilic bronchitis
Eosinophilic bronchitis is a chronic dry cough, defined by the presence of an increased number of a type of white blood cell known as eosinophils. It has a normal finding on X-ray and has no airflow limitation.[76]
Protracted bacterial bronchitis
Protracted bacterial bronchitis in children, is defined as a chronic productive cough with a positive bronchoalveolar lavage that resolves with antibiotics.[77][78] Protracted bacterial bronchitis is usually caused by Streptococcus pneumoniae, non-typable Haemophilus influenzae, or Moraxella catarrhalis.[78] Protracted bacterial bronchitis (lasting more than 4 weeks) in children may be helped by antibiotics.[79]
Plastic bronchitis
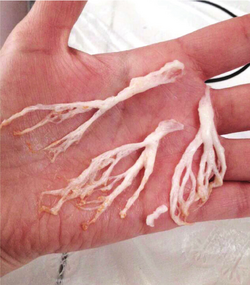
Plastic bronchitis is a rarely found condition in which thickened secretions plug the bronchi.[81][82] The plugs are rubbery or plastic-feeling (thus the name). The light-colored plugs take the branching shape of the bronchi that they fill, and are known as bronchial casts.[81] When these casts are coughed up, they are firmer in texture from typical phlegm or the short, softer mucus plugs seen in some people with asthma.[81] However, some people with asthma have larger, firmer, and more complex plugs. These differ from the casts seen in people whose plastic bronchitis is associated with congenital heart disease or lymphatic vessel abnormalities mainly because eosinophils and Charcot–Leyden crystals are present in the asthma-associated casts but not in the others.[81]
Casts obstruct the airflow, and can result in the overinflation of the opposite lung. Plastic bronchitis usually occurs in children. Some cases may result from abnormalities in the lymphatic vessels. Advanced cases may show imaging similarities to bronchiectasis.[82]
Aspergillus bronchitis
Aspergillus bronchitis is one of the Aspergillosis spectrum of diseases, in which the bronchi are specifically subject to a fungal infection. This differs from the other pulmonary aspergillosis conditions, in that it need not affect just the immunocompromised.[83][84]
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 "Bronchitis". https://www.nhlbi.nih.gov/health-topics/bronchitis.
- ↑ 2.0 2.1 2.2 2.3 2.4 Wenzel, RP; Fowler AA, 3rd (16 November 2006). "Clinical practice. Acute bronchitis". The New England Journal of Medicine 355 (20): 2125–30. doi:10.1056/nejmcp061493. PMID 17108344. https://www.nejm.org/doi/full/10.1056/NEJMcp061493.
- ↑ 3.0 3.1 "Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010". Lancet 380 (9859): 2163–96. December 2012. doi:10.1016/S0140-6736(12)61729-2. PMID 23245607.
- ↑ Geer, Joep van de; Visser, Anja; Zock, Hetty; Leget, Carlo; Prins, Jelle; Vissers, Kris (2017-11-22). "Improving Spiritual Care in Hospitals in the Netherlands: What Do Health Care Chaplains Involved in an Action-Research Study Report?". Journal of Health Care Chaplaincy 24 (4): 151–173. doi:10.1080/08854726.2017.1393039. ISSN 0885-4726. PMID 29166210. http://dx.doi.org/10.1080/08854726.2017.1393039.
- ↑ 5.00 5.01 5.02 5.03 5.04 5.05 5.06 5.07 5.08 5.09 5.10 5.11 5.12 5.13 5.14 5.15 Kin2016, S (1 October 2016). "Acute Bronchitis". American Family Physician 94 (7): 560–565. PMID 27929206. https://pubmed.ncbi.nlm.nih.gov/27929206/.
- ↑ 6.0 6.1 6.2 "Antibiotics Aren't Always the Answer" (in en-us). 25 September 2017. https://www.cdc.gov/antibiotic-use/community/for-patients/common-illnesses/bronchitis.html.
- ↑ 7.0 7.1 7.2 7.3 7.4 7.5 7.6 7.7 "What Is Bronchitis?". August 4, 2011. http://www.nhlbi.nih.gov/health/health-topics/topics/brnchi.
- ↑ 8.0 8.1 8.2 8.3 8.4 8.5 Tackett, KL; Atkins, A (December 2012). "Evidence-based acute bronchitis therapy". Journal of Pharmacy Practice 25 (6): 586–90. doi:10.1177/0897190012460826. PMID 23076965. https://journals.sagepub.com/doi/10.1177/0897190012460826.
- ↑ 9.0 9.1 "How Is Bronchitis Treated?". August 4, 2011. http://www.nhlbi.nih.gov/health/health-topics/topics/brnchi/treatment.
- ↑ 10.0 10.1 "Bronchitis, Chronic: MeSH Descriptor Data 2023". https://meshb.nlm.nih.gov/record/ui?ui=D029481.
- ↑ 11.0 11.1 11.2 11.3 Global Initiative for Chronic Obstructive Lung Disease - GOLD. 2018. pp. 4–5, 25. https://goldcopd.org/wp-content/uploads/2018/11/GOLD-2019-v1.7-FINAL-14Nov2018-WMS.pdf. Retrieved 29 May 2019.
- ↑ Reilly, John J.; Silverman, Edwin K.; Shapiro, Steven D. (2011). "Chronic Obstructive Pulmonary Disease". in Longo, Dan; Fauci, Anthony; Kasper, Dennis et al.. Harrison's Principles of Internal Medicine (18th ed.). McGraw Hill. pp. 2151–9. ISBN 978-0-07-174889-6.
- ↑ "Chronic obstructive pulmonary disease". Lancet 379 (9823): 1341–51. April 2012. doi:10.1016/S0140-6736(11)60968-9. PMID 22314182.
- ↑ 14.0 14.1 "Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary". Am. J. Respir. Crit. Care Med. 176 (6): 532–55. September 2007. doi:10.1164/rccm.200703-456SO. PMID 17507545. https://www.atsjournals.org/doi/10.1164/rccm.200703-456SO.
- ↑ 15.0 15.1 15.2 Braman, SS (January 2006). "Chronic cough due to acute bronchitis: ACCP evidence-based clinical practice guidelines". Chest 129 (1 Suppl): 95S–103S. doi:10.1378/chest.129.1_suppl.95S. PMID 16428698.
- ↑ 16.0 16.1 Fleming, DM; Elliot, AJ (March 2007). "The management of acute bronchitis in children". Expert Opinion on Pharmacotherapy 8 (4): 415–26. doi:10.1517/14656566.8.4.415. PMID 17309336. https://www.tandfonline.com/doi/abs/10.1517/14656566.8.4.415?journalCode=ieop20.
- ↑ 17.0 17.1 "FastStats" (in en-us). 23 May 2019. https://www.cdc.gov/nchs/fastats/copd.htm.
- ↑ Villarroel, MA; Blackwell, DL; Jen, A (2019) (in en-us), Summary Health Statistics: National Health Interview Survey, 2018, https://ftp.cdc.gov/pub/Health_Statistics/NCHS/NHIS/SHS/2018_SHS_Table_A-2.pdf, retrieved 22 March 2020
- ↑ 19.0 19.1 Smith, Susan M.; Fahey, Tom; Smucny, John; Becker, Lorne A. (2017). "Antibiotics for acute bronchitis". The Cochrane Database of Systematic Reviews 2017 (6): CD000245. doi:10.1002/14651858.CD000245.pub4. ISSN 1469-493X. PMID 28626858.
- ↑ 20.0 20.1 20.2 "Acute Bronchitis - Pulmonary Disorders - Merck Manuals Professional Edition" (in en-US). Merck Manuals Professional Edition. https://www.merckmanuals.com/professional/pulmonary-disorders/acute-bronchitis/acute-bronchitis/.
- ↑ 21.0 21.1 "How Can Bronchitis Be Prevented?". August 4, 2011. http://www.nhlbi.nih.gov/health/health-topics/topics/brnchi/prevention.
- ↑ Smith, SM; Schroeder, K; Fahey, T (24 November 2014). "Over-the-counter (OTC) medications for acute cough in children and adults in community settings". The Cochrane Database of Systematic Reviews 11 (11): CD001831. doi:10.1002/14651858.CD001831.pub5. PMID 25420096.
- ↑ Becker, Lorne A.; Hom, Jeffrey; Villasis-Keever, Miguel; van der Wouden, Johannes C. (2015-09-03). "Beta2-agonists for acute cough or a clinical diagnosis of acute bronchitis". The Cochrane Database of Systematic Reviews 2015 (9): CD001726. doi:10.1002/14651858.CD001726.pub5. ISSN 1469-493X. PMID 26333656.
- ↑ "Acute Bronchitis | Bronchitis Symptoms | MedlinePlus" (in en). https://medlineplus.gov/acutebronchitis.html.
- ↑ Jiang, Lanhui; Li, Ka; Wu, Taixiang (15 February 2012). "Chinese medicinal herbs for acute bronchitis". Cochrane Database of Systematic Reviews 2012 (2): CD004560. doi:10.1002/14651858.CD004560.pub4. PMID 22336804.
- ↑ 26.0 26.1 "ICD-11 - ICD-11 for Mortality and Morbidity Statistics". https://icd.who.int/browse11/l-m/en#http%3a%2f%2fid.who.int%2ficd%2fentity%2f290835130.
- ↑ "Chronic Obstructive Pulmonary Disease (COPD) - Pulmonary Disorders". https://www.msdmanuals.com/en-gb/professional/pulmonary-disorders/chronic-obstructive-pulmonary-disease-and-related-disorders/chronic-obstructive-pulmonary-disease-copd?query=Chronic%20Obstructive%20Pulmonary%20Disease%20(COPD). "Chronic bronchitis becomes chronic obstructive bronchitis if spirometric evidence of airflow obstruction develops."
- ↑ Widysanto, A; Mathew, G (January 2019). "Chronic Bronchitis". StatPearls [Internet]. NBK482437. PMID 29494044. https://www.ncbi.nlm.nih.gov/books/NBK482437/. "Chronic bronchitis ... is very often secondary to chronic obstructive pulmonary disease (COPD).".
- ↑ Lee, Sang-Do (2017) (in en). COPD: Heterogeneity and Personalized Treatment. Springer. p. 150. ISBN 9783662471784. https://books.google.com/books?id=uHg5DwAAQBAJ&pg=PA150.
- ↑ Maselli, DJ (May 2019). "Clinical Epidemiology of COPD: Insights From 10 Years of the COPDGene Study". Chest 156 (2): 228–238. doi:10.1016/j.chest.2019.04.135. PMID 31154041.
- ↑ Dotan, Y; So, JY; Kim, V (9 April 2019). "Chronic Bronchitis: Where Are We Now?". Chronic Obstructive Pulmonary Diseases 6 (2): 178–192. doi:10.15326/jcopdf.6.2.2018.0151. PMID 31063274. "with CB by symptoms (18.9%), approximately 60% had COPD (i.e., had also airflow obstruction on spirometry)".
- ↑ "Chronic obstructive pulmonary disease (COPD)" (in en). https://www.who.int/news-room/fact-sheets/detail/chronic-obstructive-pulmonary-disease-(copd). "The more familiar terms "chronic bronchitis" and "emphysema" have often been used as labels for the condition."
- ↑ "COPD: Definition". https://www.who.int/respiratory/copd/definition/en/. "The more familiar terms 'chronic bronchitis' and 'emphysema' are no longer used, but are now included within the COPD diagnosis."
- ↑ 34.0 34.1 Ferri, Fred (2019). Ferri's Clinical Advisor. Elsevier. pp. 331. ISBN 9780323530422.
- ↑ 35.0 35.1 35.2 35.3 Shen, Y (30 January 2018). "Management of airway mucus hypersecretion in chronic airway inflammatory disease: Chinese expert consensus (English edition)". International Journal of Chronic Obstructive Pulmonary Disease 13: 399–407. doi:10.2147/COPD.S144312. PMID 29430174.
- ↑ 36.0 36.1 Voynow, J (Feb 2009). "Mucins, mucus, and sputum". Chest 135 (2): 505–512. doi:10.1378/chest.08-0412. PMID 19201713.
- ↑ 37.0 37.1 Vestbo, J.; Hurd, S. S.; Agustí, A. G.; Jones, P. W.; Vogelmeier, C.; Anzueto, A.; Barnes, P. J.; Fabbri, L. M. et al. (2013). "Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary". American Journal of Respiratory and Critical Care Medicine 187 (4): 347–65. doi:10.1164/rccm.201204-0596PP. PMID 22878278. http://ajrccm.atsjournals.org/content/187/4/347.full.pdf+html.
- ↑ Weinberger, Steven (2019). Principles of Pulmonary Medicine. Elsevier. pp. 98. ISBN 9780323523714.
- ↑ "New Insights on Chronic Bronchitis:Diagnostic Test and Better Treatments on the Horizon". September 2017. https://www.nhlbi.nih.gov/news/2017/new-insights-chronic-bronchitis-diagnostic-test-and-better-treatments-horizon.
- ↑ 40.0 40.1 40.2 Kim, V; Criner, G (Feb 2013). "Chronic bronchitis and chronic obstructive pulmonary disease". Am J Respir Crit Care Med 187 (3): 228–237. doi:10.1164/rccm.201210-1843CI. PMID 23204254.
- ↑ Global Strategy for Prevention, Diagnosis and Management of COPD: 2021 Report. Global Initiative for Chronic Obstructive Lung Disease. 25 November 2020. p. 106. https://goldcopd.org/wp-content/uploads/2020/11/GOLD-REPORT-2021-v1.1-25Nov20_WMV.pdf. Retrieved 3 August 2021.
- ↑ Cohen, Jonathan; Powderly, William (2004). Infectious Diseases, 2nd ed. Mosby (Elsevier). Chapter 33: Bronchitis, Bronchiectasis, and Cystic Fibrosis. ISBN 978-0323025737.
- ↑ Foster, W (2002). "Mucociliary transport and cough in humans". Pulm Pharmacol Ther 15 (3): 277–282. doi:10.1006/pupt.2002.0351. PMID 12099778.
- ↑ Ghosh, A (October 2015). "Airway hydration and COPD". Cell Mol Life Sci 72 (19): 3637–52. doi:10.1007/s00018-015-1946-7. PMID 26068443.
- ↑ 45.0 45.1 Ohar, JA; Donohue, JF; Spangenthal, S (23 October 2019). "The Role of Guaifenesin in the Management of Chronic Mucus Hypersecretion Associated with Stable Chronic Bronchitis: A Comprehensive Review.". Chronic Obstructive Pulmonary Diseases 6 (4): 341–349. doi:10.15326/jcopdf.6.4.2019.0139. PMID 31647856.
- ↑ "ICD-11 - Mortality and Morbidity Statistics". https://icd.who.int/browse11/l-m/en#/http%3a%2f%2fid.who.int%2ficd%2fentity%2f1948124976.
- ↑ "ICD-11 - Mortality and Morbidity Statistics". https://icd.who.int/browse11/l-m/en#http%3a%2f%2fid.who.int%2ficd%2fentity%2f290835130.
- ↑ "Understanding Chronic Bronchitis". American Lung Association. 2012. http://www.lung.org/lung-disease/bronchitis-chronic/understanding-chronic-bronchitis.html.
- ↑ Forey, BA; Thornton, AJ; Lee, PN (June 2011). "Systematic review with meta-analysis of the epidemiological evidence relating smoking to COPD, chronic bronchitis and emphysema". BMC Pulmonary Medicine 11 (36): 36. doi:10.1186/1471-2466-11-36. PMID 21672193.
- ↑ Global Initiative for Chronic Obstructive Lung Disease. 2019. p. 13. https://goldcopd.org/wp-content/uploads/2018/11/GOLD-2019-v1.7-FINAL-14Nov2018-WMS.pdf. Retrieved 25 May 2019.
- ↑ Ribeiro, L (October 2016). "Effect of cannabis smoking on lung function and respiratory symptoms: a structured literature review". NPJ Primary Care Respiratory Medicine 26: 16071. doi:10.1038/npjpcrm.2016.71. PMID 27763599.
- ↑ Pfeifer, A (May 2006). "Pulmonary consequences of marijuana smoking". Ugeskr Laeger 168 (18): 1743–6. PMID 16729923.
- ↑ Szczyrek, M; Krawczyk, P; Milanowski, J; Jastrzebska, I; Zwolak, A; Daniluk, J (2011). "Chronic obstructive pulmonary disease in farmers and agricultural workers-an overview". Annals of Agricultural and Environmental Medicine 18 (2): 310–313. PMID 22216804.
- ↑ Fischer, BM; Pavlisko, E; Voynow, JA (2011). "Pathogenic triad in COPD: oxidative stress, protease-antiprotease imbalance, and inflammation". International Journal of Chronic Obstructive Pulmonary Disease 6: 413–421. doi:10.2147/COPD.S10770. PMID 21857781.
- ↑ National Heart Lung and Blood Institute (2009). "Who Is at Risk for Bronchitis?". National Institutes of Health. http://www.nhlbi.nih.gov/health/health-topics/topics/brnchi/atrisk.html.
- ↑ National Institute of Occupational Safety and Health (2012). "Respiratory Diseases Input: Occupational Risks". Centers for Disease Control and Prevention. https://www.cdc.gov/niosh/programs/resp/risks.html.
- ↑ "Industrial bronchitis: MedlinePlus Medical Encyclopedia" (in en). https://medlineplus.gov/ency/article/000072.htm.
- ↑ "What Causes COPD" (in en). https://www.lung.org/lung-health-and-diseases/lung-disease-lookup/copd/symptoms-causes-risk-factors/what-causes-copd.html.
- ↑ "Ambient (outdoor) air quality and health". 2 May 2018. https://www.who.int/en/news-room/fact-sheets/detail/ambient-(outdoor)-air-quality-and-health.
- ↑ "Protecting workers' health". November 2017. https://www.who.int/en/news-room/fact-sheets/detail/protecting-workers'-health.
- ↑ Fauci, Anthony S.; Daniel L. Kasper; Dan L. Longo; Eugene Braunwald; Stephen L. Hauser; J. Larry Jameson (2008). Chapter 254. Chronic Obstructive Pulmonary Disease Harrison's Principles of Internal Medicine (17th ed.). New York: McGraw-Hill. ISBN 978-0-07-147691-1.
- ↑ Willemse, BW; Postma, DS; Timens, W; ten Hacken, NH (March 2004). "The impact of smoking cessation on respiratory symptoms, lung function, airway hyperresponsiveness and inflammation". The European Respiratory Journal 23 (3): 464–476. doi:10.1183/09031936.04.00012704. PMID 15065840.
- ↑ "Yoga Therapy for Bronchitis". https://www.hariomyogavidyaschool.com/blog/yoga-therapy-for-bronchitis.
- ↑ Poole, Phillippa; Sathananthan, K; Fortescue, R (May 2019). "Mucolytic agents versus placebo for chronic bronchitis or chronic obstructive pulmonary disease". The Cochrane Database of Systematic Reviews 5 (7): CD001287. doi:10.1002/14651858.CD001287.pub6. PMID 31107966.
- ↑ Albrecht, H. H.; Dicpinigaitis, P. V.; Guenin, E. P. (2017). "Role of guaifenesin in the management of chronic bronchitis and upper respiratory tract infections". Multidisciplinary Respiratory Medicine 12: 31. doi:10.1186/s40248-017-0113-4. PMID 29238574.
- ↑ "Erdosteine". https://bnf.nice.org.uk/drug/erdosteine.html.
- ↑ "Mucus, Microbiomes and Pulmonary Disease". Biomedicines 9 (6): 675. June 2021. doi:10.3390/biomedicines9060675. PMID 34199312.
- ↑ Kochanek, Kenneth (June 2016). "Deaths: Final Data for 2014". National Vital Statistics Reports 65 (4): 1–122. PMID 27378572. https://www.cdc.gov/nchs/data/nvsr/nvsr65/nvsr65_04.pdf.
- ↑ 69.0 69.1 "History of the treatment of chronic bronchitis". Respiration; International Review of Thoracic Diseases 58 Suppl 1 (Suppl 1): 37–42. 1991. doi:10.1159/000195969. PMID 1925077.
- ↑ "One hundred years of chronic obstructive pulmonary disease". American Journal of Respiratory and Critical Care Medicine 171 (9): 941–8. May 2005. doi:10.1164/rccm.200412-1685OE. PMID 15849329.
- ↑ 71.0 71.1 Petty, TL (2006). "The history of COPD.". International Journal of Chronic Obstructive Pulmonary Disease 1 (1): 3–14. doi:10.2147/copd.2006.1.1.3. PMID 18046898.
- ↑ 72.0 72.1 "Chronic Bronchitis.". The Hospital 31 (786): 48–49. 19 October 1901. PMID 29819251.
- ↑ 73.0 73.1 Oswald, NC; Harold, JT; Martin, WJ (26 September 1953). "Clinical pattern of chronic bronchitis.". Lancet 265 (6787): 639–43. doi:10.1016/s0140-6736(53)90369-9. PMID 13098028.
- ↑ 74.0 74.1 Meiklejohn, A (July 1957). "A house-surgeon's observations on bronchitis in North Staffordshire pottery workers in 1864.". British Journal of Industrial Medicine 14 (3): 211–2. doi:10.1136/oem.14.3.211. PMID 13446354.
- ↑ "Terminology, Definitions, and Classification of Chronic Pulmonary Emphysema and Related Conditions: A Report of the Conclusions of a Ciba Guest Symposium.". Thorax 14 (4): 286–299. December 1959. doi:10.1136/thx.14.4.286.
- ↑ Longo, Dan (2012). Harrison's Principles of Internal Medicine. McGraw Hill. pp. 284. ISBN 9780071748896.
- ↑ Goldsobel, AB; Chipps, BE (March 2010). "Cough in the pediatric population". The Journal of Pediatrics 156 (3): 352–358.e1. doi:10.1016/j.jpeds.2009.12.004. PMID 20176183.
- ↑ 78.0 78.1 Craven, V; Everard, ML (January 2013). "Protracted bacterial bronchitis: reinventing an old disease". Archives of Disease in Childhood 98 (1): 72–76. doi:10.1136/archdischild-2012-302760. PMID 23175647.
- ↑ Marchant, JM; Petsky, HL; Morris, PS; Chang, AB (31 July 2018). "Antibiotics for prolonged wet cough in children". The Cochrane Database of Systematic Reviews 2018 (7): CD004822. doi:10.1002/14651858.CD004822.pub3. PMID 30062732.
- ↑ Kamaltynova, E. M.; Krivoshchekov, E. V.; Yanulevich, O. S.; Kavardakova, E. S. (2017-08-11). "Plastic bronchitis associated with corrected cardiac anomaly in a child". Bulletin of Siberian Medicine 16 (2): 180–186. doi:10.20538/1682-0363-2017-2-180-186. ISSN 1819-3684. https://bulletin.tomsk.ru/jour/article/view/888/689.
- ↑ 81.0 81.1 81.2 81.3 Kotloff, Robert; McCormack, Francis X. (2016-08-16) (in en). Rare and Orphan Lung Diseases, An Issue of Clinics in Chest Medicine, E-Book. Elsevier Health Sciences. pp. 405–408. ISBN 978-0-323-46274-7. https://books.google.com/books?id=vozeDAAAQBAJ&pg=PA405.
- ↑ 82.0 82.1 Panchabhai, TS; Mukhopadhyay, S; Sehgal, S; Bandyopadhyay, D; Erzurum, SC; Mehta, AC (November 2016). "Plugs of the Air Passages: A Clinicopathologic Review.". Chest 150 (5): 1141–1157. doi:10.1016/j.chest.2016.07.003. PMID 27445091.
- ↑ "Aspergillus bronchitis | Aspergillus & Aspergillosis Website". https://www.aspergillus.org.uk/content/aspergillus-bronchitis.
- ↑ Kosmidis, Chris; Denning, David W. (1 March 2015). "The clinical spectrum of pulmonary aspergillosis" (in en). Thorax 70 (3): 270–277. doi:10.1136/thoraxjnl-2014-206291. PMID 25354514. https://thorax.bmj.com/content/70/3/270. Retrieved 8 November 2019.
External links
| Classification | |
|---|---|
| External resources |
- NIH entry on Bronchitis
- MedlinePlus entries on Acute bronchitis and Chronic bronchitis
- Mayo Clinic factsheet on bronchitis
 |