Biology:Bordetella pertussis
| Bordetella pertussis | |
|---|---|
| |
| Gram stain | |
| Scientific classification | |
| Domain: | Bacteria |
| Phylum: | Pseudomonadota |
| Class: | Betaproteobacteria |
| Order: | Burkholderiales |
| Family: | Alcaligenaceae |
| Genus: | Bordetella |
| Species: | B. pertussis
|
| Binomial name | |
| Bordetella pertussis (Bergey et al. 1923) Moreno-López 1952
| |
Bordetella pertussis is a Gram-negative, aerobic, pathogenic, encapsulated coccobacillus bacterium of the genus Bordetella, and the causative agent of pertussis or whooping cough. Its virulence factors include pertussis toxin, adenylate cyclase toxin, filamentous haemagglutinin, pertactin, fimbria, and tracheal cytotoxin.
The bacteria are spread by airborne droplets and the disease's incubation period is 7–10 days on average (range 6–20 days).[1][2] Humans are the only known reservoir for B. pertussis.[3] The complete B. pertussis genome of 4,086,186 base pairs was published in 2003.[4] Compared to its closest relative B. bronchiseptica, the genome size is greatly reduced. This is mainly due to the adaptation to one host species (human) and the loss of capability of survival outside a host body.[5]
Like B. bronchiseptica, B. pertussis can express a flagellum-like structure, even though it has been historically categorized as a nonmotile bacterium.[6]
Taxonomy
The genus Bordetella contains nine species: B. pertussis, B. parapertussis, B. bronchiseptica, B. avium, B. hinzii, B. holmesii, B. trematum, B. ansorpii, and B. petrii.[5]
B. pertussis, B. parapertussis and B. bronchiseptica form a closely related phylogenetical group. B. parapertussis causes a disease similar to whooping cough in humans, and B. bronchiseptica infects a range of mammal hosts, including humans, and causes a spectrum of respiratory disorders.[5]
Evolution
The disease pertussis was first described by French physician Guillaume de Baillou after the epidemic of 1578. The disease may have been described earlier in a Korean medical textbook.[7] The causative agent of pertussis was identified and isolated by Jules Bordet and Octave Gengou in 1906. It is believed that the genus Bordetella may have evolved from ancestors that could survive in the soil according to 16S rRNA gene sequencing data.[8] 16S rRNA is a component of all bacteria that allows for the comparison of phyla within a sample. The expansion of human development into the agricultural field caused there to be an influx of human to soil contact. This increase not only created more advantageous environments for the ancestors of Bordetella not only to thrive in, but to spread to humans as well. Over time, Bordetella, like B. pertussis, has adapted to specifically infect humans and they are still able to multiply and thrive in soil conditions.[9]
It was initially determined that B. pertussis is a monomorphic pathogen in which the majority of strains found had the same two types of alleles: ptxA1 or ptxA2.[10] Modern developments in genome sequencing have allowed B. pertussis to be studied more allowing for the discovery of the ptxP region. Through studying the gene, there has been evidence of mutations within the gene that show missing genomes present on the DNA strand. A study by Bart et al. revealed that 25% of the genes on the Tohama I reference strain of the B. pertussis sequence were missing in comparison to the ancestral strains. These mutations were noted to be caused by an increase in intragenomic recombination with loss of DNA. Genes controlled by the BvgAS system have transformed B. pertussis into a much more contagious pathogen.[10] In particular, strains with the ptxP3 allele, that developed through mutations in recent years, have an increased expression of toxins. Ultimately, this leads to higher acuteness of the disease when contracted. [10] This has caused an upwards trend of most cases of B. pertussis being the ptxP3 strain, especially in developing countries. Since the 1990s, most cases in developed countries such as the United States have ptxP3 isolates rather than the ptxA1 causing it to become the more dominant strain.[9]
Growth requirements
Bordetella pertussis prefers aerobic conditions in pH range of 7.0–7.5,[11] optimal to thrive in the human body. The max pH level for their growth was at a pH level of 8.0. The minimum pH range for minimal growth was at pH 6.0-6.5. The bacteria are not able to reproduce at pH levels lower than 5.0.
In addition, Bordetella pertussis favors a temperature range of 35 °C to 37 °C.[12] It is a strict aerobe as mentioned previously and its nutritional requirements are meticulous in its requirement for nicotinamide supplement. It has been identified that the growth of the bacteria is hindered in the presence of fatty acids, peroxide media, metal ions, and sulfides.
As a strict aerobe, the bacterium requires oxygen to grow and sustain. Such aerobes undergo cellular respiration to metabolize substances using oxygen. In such respiration, the terminal electron acceptor for the electron transport chain is oxygen.[13] The organism is oxidase positive, but urease, nitrate reductase, and citrate negative.[14]
B. pertussis is not exclusively an extracellular pathogen, meaning that it not only grows outside the cell, it can efficiently adapt to an internal environment.[15] It also lowers the level of its BvgAS two-component system, which leads to an expression of virulence genes and an avirulent phenotype.[15] In addition, it can adjust the central and energy metabolism, cell wall reinforcement, maintenance of appropriate redox and metal homeostasis, and repair of damaged macromolecules.[15] Studies have also shown mutants lacking cysteine dioxygenase genes displaying attenuated cytotoxicity toward THP-1 cells, which highlights the role of sulphur metabolism in host-pathogen interactions.[15]
Metabolism
B. pertussis presents unique challenges and opportunities for metabolic modeling, especially given its reemergence as a pathogen. Elevated glutamate levels were found to slow growth due to oxidative stress, revealing a complex relationship. This effect is compounded by observations suggesting that a small starting population could amplify oxidative stress through quorum sensing, a phenomenon deserving further investigation.[16]
When B. pertussis is in a balanced medium of lactate and glutamate that does not accumulate ammonium, a partially faulty citric acid cycle in B. pertussis and its ability to synthesize and break down β-hydroxybutyrate is observed. Cultivating B. pertussis in this medium resulted in some production of polyhydroxybutyrate but no excretion of β-hydroxybutyrate, indicating a more efficient conversion of carbon into biomass compared to existing media formulations.[17]
In biofilm conditions, B. pertussis cells exhibited increased toxin levels alongside reduced expression of certain proteins, indicating a metabolic shift towards utilizing the full tricarboxylic acid (TCA) cycle over the glyoxylate shunt.[18] These changes correlated with heightened polyhydroxybutyrate accumulation and superoxide dismutase activity, potentially contributing to prolonged survival in biofilms.[18] The interplay between protein expression and metabolic responses highlights the intricate mechanisms influencing B. pertussis growth and adaptation.[19] Despite a less negative energy profile compared to host tissues like the human respiratory system, B. pertussis efficiently couples biosynthesis with catabolism, sustaining robust growth even after extended incubation periods.[19]
B. pertussis cannot use sugars as a carbon source, so amino acids are used, the main and efficient one being glutamate. Glutamate goes through the TCA cycle once converted by glutamate dehydrogenase. [20] It can also be used for other pathways such as gluconeogenesis.
Host species
Humans are the only host species of B. pertussis.[21] B. pertussis is able to survive intracellularly in the phagocytic cell of a mammal. B. pertussis releases proteins to aid in metabolism, stress response, iron uptake, and regulation, which permit for the bacteria's resilience to survive. Depending on the host cell, B. pertussis is able to survive in human macrophages and epithelial cells for three days.[22] Outbreaks of whooping cough have been observed among chimpanzees in a zoo, and wild gorillas; in both cases, it is considered likely that the infection was acquired as a result of close contact with humans.[23] Several zoos have a long-standing custom of vaccinating their primates against whooping cough.[24]
Research shows that some primate species are highly sensitive to B. pertussis, and developed a clinical whooping cough in high incidence when exposed to low inoculation doses.[25][26] Whether the bacteria spread naturally in wild animal populations has not been confirmed satisfactorily by laboratory diagnosis.[27] In research settings, baboons have been used as a model of the infection although it is not known whether the pathology in baboons is the same as in humans.[28]
Pertussis
Pertussis is an infection of the respiratory system characterized by a "whooping" sound when the person breathes in.[29] B. pertussis infects its host by colonizing lung epithelial cells. The bacterium contains a surface protein, filamentous haemagglutinin adhesin, which binds to the sulfatides found on cilia of epithelial cells. Other adhesins are fimbriae and petractin.[30] Once anchored, the bacterium produces tracheal cytotoxin, which stops the cilia from beating. This prevents the cilia from clearing debris from the lungs, so the body responds by sending the host into a coughing fit.[31] B. pertussis can inhibit the function of the host's immune system. The toxin, known as pertussis toxin, inhibits G protein coupling that regulates an adenylate cyclase-mediated conversion of ATP to cyclic adenosine monophosphate. The result is that phagocytes convert too much adenosine triphosphate to cyclic adenosine monophosphate, causing disturbances in cellular signaling mechanisms, and preventing phagocytes from correctly responding to the infection. Pertussis toxin, formerly known as lymphocytosis-promoting factor, causes a decrease in the entry of lymphocytes into lymph nodes, which can lead to a condition known as lymphocytosis, with a complete lymphocyte count of over 4000/μl in adults or over 8000/μl in children. Besides targeting lymphocytes, it limits neutrophil migration to the lungs. It also decreases the function of tissue-resident macrophages, which are responsible for some bacterial clearance.[32]
The infection of B. pertussis occurs mostly in children under the age of one since this is when they are unimmunized, or children with faded immunity, normally around the ages 11 through 18. The signs and symptoms are similar to a common cold: runny nose, sneezing, mild cough, and low-grade fever.[33] The patient becomes most contagious during the catarrhal stage of infection, normally two weeks after the coughing begins. It may become airborne when the person coughs, sneezes, or laughs. The paroxysmal cough precedes a crowing inspiratory sound characteristic of pertussis. After a spell, the patient might make a "whooping" sound when breathing in or may vomit. Transmission rates are expected to rise as the host experiences their most contagious stage when the total viable count of B. pertussis is at its highest. After the host coughs, the bacteria in their respiratory airways will be exposed to the air by way of aerosolized droplets, threatening nearby humans.[34] Because whooping cough triggers intense, repeated coughing fits, this process occurs frequently, making the disease extremely contagious in close-contact environments.
A human host can exhibit a range of physical reactions as a result of the B. pertussis pathogen, depending on how well their body is equipped to fight infection.[34] Adults have milder symptoms, such as prolonged coughing without the "whoop". Infants less than six months also may not have the typical whoop. A coughing spell may last a minute or more, producing cyanosis, apnea, and seizures.
Transmission and infection
B. pertussis is a highly contagious infection of the respiratory tract.[35] However, for B. pertussis to persist in a population the bacterium needs an uninterrupted chain of transmission as there are no animal reservoirs and the bacteria do not survive in the environment. B. pertussis primarily spreads through respiratory droplets, requiring direct contact between individuals due to its short survival time outside the body.
Virulence factors of B. pertussis aid the microbe in infecting the host. These include fimbriae that bind to specific integrin antigens that are abundant in the respiratory tract, this has been found to facilitate tracheal occupation in mice.[36]
It was noted that between 1991 and 2008, there were 258 deaths for infants 8 months old and younger.[37]
Progression of disease
Pertussis manifests in three distinct stages. The dynamic progression of pertussis, characterized by its distinct phases from incubation to paroxysmal coughing, underscores the complexity of the disease's clinical manifestations and highlights the potential significance of toxin release in driving symptoms.[38]
Following exposure, an incubation period of 5–7 days ensues before symptoms appear.[38]
The catarrhal phase follows, characterized by cold-like symptoms lasting about a week, with a high isolation rate of the organism. This phase transitions into the paroxysmal phase, where the dry cough evolves into a severe, paroxysmal cough with mucous secretion and vomiting.[38]
The coughing fits, characterized by efforts to expel respiratory secretions, may result in a distinctive whooping sound. Recovery of the organism diminishes significantly during this phase. Although the organism is seldom detected in the blood, it is theorized that the clinical symptoms primarily stem from toxin release. The paroxysmal phase typically persists for a minimum of 2 weeks.[38]
Diagnosis
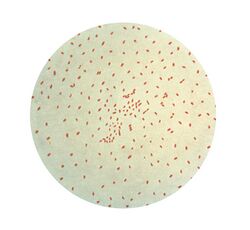
A nasopharyngeal swab or aspirate can be sent to the bacteriology laboratory for Gram stain (Gram-negative, coccobacilli, diplococci arrangement), with growth on Bordet–Gengou agar or buffered charcoal yeast extract agar with added cephalosporin to select for the organism, which shows mercury drop-like colonies. Endotracheal tube aspirates or bronchoalveolar lavage fluids are preferred for laboratory diagnostics due to their direct contact with the ciliated epithelial cells and higher isolation rates of the pathogen.
Laboratory diagnostic methods used to identify B. pertussis:
- Serology[39]
- Identification of specific agglutinating antibodies in the patient's blood serum with a high sensitivity and specificity rate.
- Able to detect the level of virulence and measure the immune response to the pathogen.
- Recommend those corresponding to the catarrhal phase of the illness. Not used in infants due to delay of positive results, often indicating the disease has progressed.
- Sparked the development of ELISA kits.
- Microbiological culture [39][40]
- Known for high specificity, the ability to subtype the colonies presented, and limited sensitivity. Ideal for antimicrobial-resistant monitoring. Specificity results can be affected by age, immunization status, duration of symptoms, and even specimen handling.
- It is very difficult to cultivate separate pathogens and only high bacterial loads can lead to a positive culture. The ideal stage for isolation is the catarrhal stage or the beginning of the paroxysmal stage. Vaccinated persons also have a lower rate of isolation.
- Plates are incubated at 36 °C under high humidity for 7–10 days before obtaining results.
- Classical PCR assay[39]
- Being the test of choice, this procedure is known for its quick and high sensitivity, however; often inaccurate when identifying between Bordetella species.
- The primers used for PCR usually target the transposable elements IS481 and IS1001.[41]
- Recommend to be performed on infants and those corresponding to the catarrhal phase of the illness. It can detect the pathogens in atypical manifestations and vaccinated patients for longer periods, compared to the culture.
- Target genes within B. pertussis are IS481, IS1002, ptxS1, Ptx-Pr, and BP3385, however, B. bronchisepticaand B. holmesii contain similar gene expression, leaving it difficult to differentiate between the bacterium in the laboratory. The most effective technique to differentiate between the two bacteria is by human and animal isolates. Singleplex PCR identifies the target gene ptxS1.
- Direct Fluorescent Antibody Testing (DFA) [39]
- Inexpensive and direct results of Bordetella detection with poor sensitivity and specificity. This test stains the nasopharyngeal secretions with a fluorescent modified antibody that binds directly to the B. pertussis or B. parapertussis bacteria. If positive, the binding antibody would glow under the microscope. Because of the low specificity, it is common to receive false positives with polyclonal antibodies occurring.
Several diagnostic tests are available, particularly the enzyme-linked immunosorbent assay ELISA kits. These are designed to detect filamentous hemagglutinin (FHA) and/or anti-pertussis-toxin antibodies of IgG, IgA, or IgM. Some kits use a combination of antigens which leads to a higher sensitivity, but might also make the interpretation of the results harder since one cannot know which antibody has been detected.[42]
Misdiagnosis is common due to diagnostic techniques, misidentification between species in laboratories, and clinician error. The misdiagnoses between Bordetella species further increase the likelihood of antibiotic resistance. These factors highlight the need for a procedure to target all species through specific and fast methods.
Treatment and prevention
Treatment
Whooping cough is treated by macrolides, for example erythromycin. The therapy is most effective when started during the incubation period or the catarrhal period. It is ideal for treatment should be within 1–2 weeks from onset of symptoms. When applied during the paroxysmal cough phase, the time of convalescence is not affected, only further transmission is reduced to 5–10 days after infection.[43][44]
Prevention
Pertussis vaccine has been widely used since the second half of the 20th century.[45][2] The first vaccines were whole-cell vaccines (wP), composed of chemically inactivated bacteria and given intramuscularly. When given, the inactive bacteria and antigens trigger the immune response and mimic natural infection.
Due to the frequent reports of reactions at the injection site, scientists started to replace whole-cell vaccines with acellular pertussis (aP) vaccines which have, recently, shown a decreased time of immunity and level of protection against colonization.[46] These acellular vaccines are also intramuscular and are composed of purified surface antigens, mainly fimbriae, filamentous hemagglutinin, pertactin and pertussis toxin. Both vaccines are still used today, with the aP vaccine predominantly used in developed countries.
The aP vaccine is also a part of the diphtheria, tetanus, and acellular pertussis (DTaP) immunization.[2] Those being administered these vaccines are recommended to receive boosters as they only afford protection for about 4–12 years; while natural infection offers 7–20 years.[47] Cases in infants are common and often have serious impacts as they are more susceptible to Bordetella pertussis than adolescents and healthy adults. Therefore, to decrease the likelihood of contracting and spreading this disease, parents are recommended to receive the preventative vaccine.[48]
With the resurgence of pertussis cases, there are concerns regarding the level of protection provided by the current vaccine. This vaccine does not offer protection against other species of Bordetella such as B. holmesii and B. bronchiseptica and further highlights the need for a revamped vaccine. Research is currently developing a novel vaccine such as the BPZE1, which is a live attenuated vaccine against B. pertussis and challenges the other pathogens in the 'Classical Bordetellae'. This new vaccine inactivates the gene encoding 3 major toxins with only a single intranasal dose. It is currently being studied for safety in immunocompromised patients and pregnant women. Other promising vaccines are under study and in trial periods for accuracy, efficacy, and safety.[47]
References
- ↑ Pertussis; in Control of Communicable Diseases Manual. (19th ed.). Washington DC: American Public Health Association. 2008. p. 457. ISBN 978-0-87553-189-2.
- ↑ 2.0 2.1 2.2 Organisation mondiale de la santé; World Health Organization (1998). Relevé épidémiologique hebdomadaire (Online) = Weekly epidemiological record.. Organisation mondiale de la sante. OCLC 301147153.
- ↑ "Pertussis". Epidemiology and Prevention of Vaccine-Preventable Diseases: The Pink Book (13th ed.). Centers for Disease Control and Prevention, Public Health Foundation. 2015. https://www.cdc.gov/vaccines/pubs/pinkbook/pert.html.
- ↑ "Comparative analysis of the genome sequences of Bordetella pertussis, Bordetella parapertussis and Bordetella bronchiseptica". Nature Genetics 35 (1): 32–40. September 2003. doi:10.1038/ng1227. PMID 12910271.
- ↑ 5.0 5.1 5.2 Bordetella: molecular microbiology. Wymondham: Horizon Bioscience. 2007. ISBN 978-1-904933-31-1. OCLC 159579443.
- ↑ "Bordetella pertussis Can Be Motile and Express Flagellum-Like Structures". mBio 10 (3): e00787–19. May 2019. doi:10.1128/mBio.00787-19. PMID 31088927.
- ↑ "Origin and evolution of Bordetella pertussis" (in en-GB). 24 April 2014. https://www.sanger.ac.uk/news_item/origin-and-evolution-of-bordetella-pertussis/.
- ↑ "Environmental Origin of the Genus Bordetella". Frontiers in Microbiology 8: 28. 2017. doi:10.3389/fmicb.2017.00028. PMID 28174558.
- ↑ 9.0 9.1 Belcher, Thomas; Preston, Andrew (November 2015). Carbonetti, Nicholas. ed. "Bordetella pertussis evolution in the (functional) genomics era" (in en). Pathogens and Disease 73 (8). doi:10.1093/femspd/ftv064. ISSN 2049-632X. PMID 26297914. PMC 4626590. https://academic.oup.com/femspd/article/2467598/Bordetella-pertussis-evolution-in-the-functional.
- ↑ 10.0 10.1 10.2 Sealey, Katie L.; Belcher, Thomas; Preston, Andrew (2016-06-01). "Bordetella pertussis epidemiology and evolution in the light of pertussis resurgence". Infection, Genetics and Evolution 40: 136–143. doi:10.1016/j.meegid.2016.02.032. ISSN 1567-1348. PMID 26932577. Bibcode: 2016InfGE..40..136S. https://www.sciencedirect.com/science/article/pii/S1567134816300636.
- ↑ Remesh, Arun Thachappully; Alagarasu, Kalichamy; Jadhav, Santoshkumar; Prabhakar, Meera; Viswanathan, Rajlakshmi (2024-02-28). "Pertussis Vaccines Scarcely Provide Protection against Bordetella parapertussis Infection in Children—A Systematic Review and Meta-Analysis" (in en). Vaccines 12 (3): 253. doi:10.3390/vaccines12030253. ISSN 2076-393X. PMID 38543887.
- ↑ Hulbert, Robin R.; Cotter, Peggy A. (November 2009). "Laboratory Maintenance of Bordetella pertussis" (in en). Current Protocols in Microbiology 15 (1): Unit 4B.1. doi:10.1002/9780471729259.mc04b01s15. ISSN 1934-8525. PMID 19885941. https://currentprotocols.onlinelibrary.wiley.com/doi/10.1002/9780471729259.mc04b01s15.
- ↑ Borisov, Vitaliy B.; Verkhovsky, Michael I. (2015). "Oxygen as Acceptor". EcoSal Plus 6 (2). doi:10.1128/ecosalplus.ESP-0012-2015. ISSN 2324-6200. PMID 26734697.
- ↑ Aryal, Sagar (2022-05-26). "Biochemical Test of Bordetella pertussis" (in en-US). https://microbenotes.com/biochemical-test-of-bordetella-pertussis/.
- ↑ 15.0 15.1 15.2 15.3 Farman, Mariam R.; Petráčková, Denisa; Kumar, Dilip; Držmíšek, Jakub; Saha, Argha; Čurnová, Ivana; Čapek, Jan; Hejnarová, Václava et al. (2023-12-31). "Avirulent phenotype promotes Bordetella pertussis adaptation to the intramacrophage environment". Emerging Microbes & Infections 12 (1). doi:10.1080/22221751.2022.2146536. PMID 36357372.
- ↑ Vitelli, Michael; Tamer, Ibrahim Melih; Pritzker, Mark; Budman, Hector (May 2023). "Modeling the effect of oxidative stress on Bordetella pertussis fermentations" (in en). Biotechnology Progress 39 (3). doi:10.1002/btpr.3335. ISSN 8756-7938. PMID 36799126.
- ↑ Thalen, Marcel; van den IJssel, Jan; Jiskoot, Wim; Zomer, Bert; Roholl, Paul; de Gooijer, Cornelis; Beuvery, Coen; Tramper, Johannes (October 1999). "Rational medium design for Bordetella pertussis: basic metabolism". Journal of Biotechnology 75 (2–3): 147–159. doi:10.1016/s0168-1656(99)00155-8. ISSN 0168-1656. PMID 10553654.
- ↑ 18.0 18.1 Suyama, Hiroki; Luu, Laurence Don Wai; Zhong, Ling; Raftery, Mark J.; Lan, Ruiting (2023). "Integrating proteomic data with metabolic modeling provides insight into key pathways of Bordetella pertussis biofilms". Frontiers in Microbiology 14. doi:10.3389/fmicb.2023.1169870. ISSN 1664-302X. PMID 37601354.
- ↑ 19.0 19.1 Popović, Marko E.; Stevanović, Maja; Pantović Pavlović, Marijana (April 2024). "Return of the forgotten nightmare: Bordetella pertussis uses a more negative Gibbs energy of metabolism to outcompete its host organism". Microbial Risk Analysis 26. doi:10.1016/j.mran.2024.100292. ISSN 2352-3522. Bibcode: 2024MbRA...26j0292P.
- ↑ Belcher, Thomas; Dubois, Violaine; Rivera-Millot, Alex; Locht, Camille; Jacob-Dubuisson, Françoise (2021-12-31). "Pathogenicity and virulence of Bordetella pertussis and its adaptation to its strictly human host". Virulence 12 (1): 2608–2632. doi:10.1080/21505594.2021.1980987. ISSN 2150-5594. PMID 34590541. PMC 8489951. https://doi.org/10.1080/21505594.2021.1980987.
- ↑ "15.3E: Whooping Cough" (in en). 2018-06-29. https://bio.libretexts.org/Bookshelves/Microbiology/Microbiology_(Boundless)/15%3A_Diseases/15.03%3A_Bacterial_Diseases_of_the_Respiratory_System/15.3E%3A_Whooping_Cough.
- ↑ Rivera, Israel; Linz, Bodo; Harvill, Eric T. (2020-10-15). "Evolution and Conservation of Bordetella Intracellular Survival in Eukaryotic Host Cells" (in English). Frontiers in Microbiology 11. doi:10.3389/fmicb.2020.557819. ISSN 1664-302X. PMID 33178148.
- ↑ "An epizootic of whooping cough among chimpanzees in a zoo". Folia Primatologica; International Journal of Primatology 55 (1): 45–50. 1990. doi:10.1159/000156498. PMID 2394416.
- ↑ "Immunoprofylaxis in infant great apes". Clinical Management of Infant Great Apes. Monographs in Primatology. 5. New York: Liss. 1985. pp. 107–112.
- ↑ Gustavsson, Olle E.A.; Röken, Bengt O.; Serrander, Rita (1990-02-14). "An Epizootic of Whooping Cough among Chimpanzees in a Zoo". Folia Primatologica 55 (1): 45–50. doi:10.1159/000156498. ISSN 0015-5713. PMID 2394416. https://brill.com/view/journals/ijfp/55/1/article-p45_7.xml.
- ↑ Warfel, Jason M; Merkel, Tod J (October 2014). "The baboon model of pertussis: effective use and lessons for pertussis vaccines" (in en). Expert Review of Vaccines 13 (10): 1241–1252. doi:10.1586/14760584.2014.946016. ISSN 1476-0584. PMID 25182980. http://www.tandfonline.com/doi/full/10.1586/14760584.2014.946016.
- ↑ "Consequences of Non-Intervention for Infectious Disease in African Great Apes | PLOS ONE". PLOS ONE 6 (12). 2011. doi:10.1371/journal.pone.0029030. PMID 22216162.
- ↑ Cherry, J.D. The History of Pertussis (Whooping Cough); 1906–2015: Facts, Myths, and Misconceptions. Curr Epidemiol Rep 2, 120–130 (2015). https://doi.org/10.1007/s40471-015-0041-9
- ↑ "The whole-cell proteome shows the characteristics of macrolides-resistant Bordetella pertussis in China linked to the biofilm formation". Archives of Microbiology 205 (6). May 2023. doi:10.1007/s00203-023-03566-0. PMID 37148370. Bibcode: 2023ArMic.205..219L.
- ↑ Bordetella: molecular microbiology. Wymondham: Horizon Bioscience. 2007. ISBN 978-1-904933-31-1. OCLC 159579443.
- ↑ [https://www.cdc.gov/vaccines/pubs/pinkbook/downloads/pert.pdf CDC Bordetella pertussis}
- ↑ "Immunomodulation in the pathogenesis of Bordetella pertussis infection and disease". Current Opinion in Pharmacology. Respiratory/Musculoskeletal 7 (3): 272–278. June 2007. doi:10.1016/j.coph.2006.12.004. PMID 17418639.
- ↑ "Pertussis". Epidemiology and Prevention of Vaccine-Preventable Diseases: The Pink Book (13th ed.). Centers for Disease Control and Prevention, Public Health Foundation. 2015. https://www.cdc.gov/vaccines/pubs/pinkbook/pert.html.
- ↑ 34.0 34.1 "Airborne transmission of Bordetella pertussis". The Journal of Infectious Diseases 206 (6): 902–906. September 2012. doi:10.1093/infdis/jis443. PMID 22807521.
- ↑ "Pertussis: Common Questions and Answers". American Family Physician 104 (2): 186–192. August 2021. PMID 34383446.
- ↑ Kerr, J. R.; Matthews, R. C. (2000-03-01). "Bordetella pertussis Infection: Pathogenesis, Diagnosis, Management, and the Role of Protective Immunity" (in en). European Journal of Clinical Microbiology and Infectious Diseases 19 (2): 77–88. doi:10.1007/s100960050435. ISSN 1435-4373. PMID 10746492.
- ↑ "Bordetella pertussis: new concepts in pathogenesis and treatment". Current Opinion in Infectious Diseases 29 (3): 287–94. June 2016. doi:10.1097/QCO.0000000000000264. PMID 26906206.
- ↑ 38.0 38.1 38.2 38.3 Kerr, J. R.; Matthews, R. C. (2000-03-03). "Bordetella pertussis Infection: Pathogenesis, Diagnosis, Management, and the Role of Protective Immunity". European Journal of Clinical Microbiology & Infectious Diseases 19 (2): 77–88. doi:10.1007/s100960050435. ISSN 0934-9723. PMID 10746492. http://link.springer.com/10.1007/s100960050435.
- ↑ 39.0 39.1 39.2 39.3 Zouari, Asma (21 Nov 2011). "The diagnosis of pertussis: which method to choose?". Critical Reviews in Microbiology 38 (2): 111–121. doi:10.3109/1040841X.2011.622715. PMID 22103249.
- ↑ Bouchez, Valérie; Guillot, Sophie; Landier, Annie; Armatys, Nathalie; Matczak, Soraya; Toubiana, Julie; Brisse, Sylvain (2021-09-16). "Evolution of Bordetella pertussis over 23 years in France, 1996 to 2018" (in en). Eurosurveillance 26 (37). doi:10.2807/1560-7917.ES.2021.26.37.2001213. ISSN 1560-7917. PMID 34533118.
- ↑ "Bordetella pertussis". Microbiology Spectrum 4 (3): 311–339. June 2016. doi:10.1128/microbiolspec.EI10-0008-2015. ISBN 978-1-55581-944-6. PMID 27337481.
- ↑ "ELISA classic – Bordetella pertussis | SERION Diagnostics". https://www.serion-diagnostics.de/en/products/serion-elisa-classic-antigen/bordetella-pertussis/#:~:text=The%20SERION%20ELISA%20classic%20Bordetella,laboratory%20confirmation%20of%20whooping%20cough..
- ↑ Organisation mondiale de la santé; World Health Organization (1998). Relevé épidémiologique hebdomadaire (Online) = Weekly epidemiological record.. Organisation mondiale de la sante. OCLC 301147153.
- ↑ "Bordetell". Medical Microbiology (4th ed.). Galveston (TX): University of Texas Medical Branch at Galveston. 1996. ISBN 978-0-9631172-1-2. https://www.ncbi.nlm.nih.gov/books/NBK7813/.
- ↑ "Bordetella pertussis epidemiology and evolution in the light of pertussis resurgence". Infection, Genetics and Evolution 40: 136–143. June 2016. doi:10.1016/j.meegid.2016.02.032. PMID 26932577. Bibcode: 2016InfGE..40..136S.
- ↑ "Bordetella pertussis: new concepts in pathogenesis and treatment". Current Opinion in Infectious Diseases 29 (3): 287–294. June 2016. doi:10.1097/QCO.0000000000000264. PMID 26906206.
- ↑ 47.0 47.1 Miguelena Chamorro, Beatriz; De Luca, Karelle; Swaminathan, Gokul; Longet, Stéphanie; Mundt, Egbert; Paul, Stéphane (2023-09-21). "Bordetella bronchiseptica and Bordetella pertussis: Similarities and Differences in Infection, Immuno-Modulation, and Vaccine Considerations" (in en). Clinical Microbiology Reviews 36 (3): e0016422. doi:10.1128/cmr.00164-22. ISSN 0893-8512. PMID 37306571.
- ↑ "Multiple rib and vertebral fractures associated with Bordetella pertussis infection: a case report". BMC Infectious Diseases 23 (1). April 2023. doi:10.1186/s12879-023-08189-w. PMID 37024849.
Further reading
- "Ch. 31 Bordetella". Medical Microbiology (4th ed.). University of Texas Medical Branch. 1996. NBK7813. ISBN 978-0-9631172-1-2. https://www.ncbi.nlm.nih.gov/books/NBK7813/.
External links
Wikidata ☰ Q137103 entry
 |
